Fig 8.
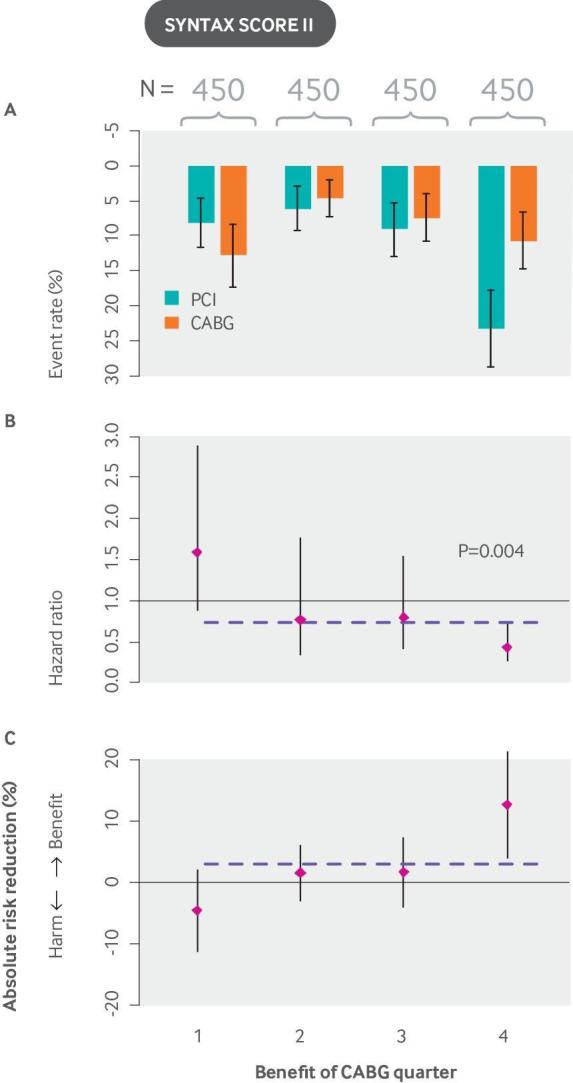
The SYNTAX score II stratifies patients with non-acute coronary artery disease on the basis of their risk of mortality with CABG versus PCI and is a useful guide to decision making. In the SYNTAX trial, rates of major adverse cardiac or cerebrovascular events at 12 months were significantly higher in the PCI group (17.8%) than in the CABG group (12.4%; P=0.002), confirming that CABG should be the preferred approach for patients with untreated three vessel or left main coronary artery disease.132 The SYNTAX score II was developed by applying a Cox proportional hazards model to the SYNTAX (Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery) trial (N=1800). It contains eight predictors: a previously developed anatomical SYNTAX score, age, creatinine clearance, left ventricular ejection fraction, presence of unprotected left main coronary artery disease, peripheral vascular disease, female sex, and COPD, plus treatment interaction terms with each of these variables. The graphs show (A) event rates, (B) hazard ratios, and (C) absolute risk reductions for CABG versus PCI. Unlike the examples shown in other figures, event rates do not increase monotonically across quarters because patients are stratified not by predicted risk but by predicted benefit (outcome risk with PCI minus outcome risk with CABG). Overall results, depicted by the horizontal dashed line, show a trend that favors CABG. However, when patients are stratified by their expected benefit, a quarter of patients who are treatment unfavorable is identified (Pinteraction=0.0037 for eight interaction terms), and benefit is largely confined to the quarter of patients at highest benefit. Although the SYNTAX score II has been validated for prediction of outcomes, it has not yet been validated for the prediction of benefit. CABG: coronary artery bypass graft surgery; COPD: chronic obstructive pulmonary disease; PCI: percutaneous coronary intervention.
