Abstract
Background:
End-of-life hospitalizations in nursing home residents are common, although they are often burdensome and potentially avoidable.
Aim:
We aimed to summarize the existing evidence on end-of-life hospitalizations in nursing home residents.
Design:
Systematic review (PROSPERO registration number CRD42017072276).
Data sources:
A systematic literature search was carried out in PubMed, CINAHL, and Scopus (date of search 9 April 2019). Studies were included if they reported proportions of in-hospital deaths or hospitalizations of nursing home residents in the last month of life. Two authors independently selected studies, extracted data, and assessed the quality of studies. Median with interquartile range was used to summarize proportions.
Results:
A total of 35 studies were identified, more than half of which were from the United States (n = 18). While 29 studies reported in-hospital deaths, 12 studies examined hospitalizations during the last month of life. The proportion of in-hospital deaths varied markedly between 5.9% and 77.1%, with an overall median of 22.6% (interquartile range: 16.3%–29.5%). The proportion of residents being hospitalized during the last month of life ranged from 25.5% to 69.7%, and the median was 33.2% (interquartile range: 30.8%–38.4%). Most studies investigating the influence of age found that younger age was associated with a higher likelihood of end-of-life hospitalization. Four studies assessed trends over time, showing heterogeneous findings.
Conclusion:
There is a wide variation in end-of-life hospitalizations, even between studies from the same country. Overall, such hospitalizations are common among nursing home residents, which indicates that interventions tailored to each specific health care system are needed to improve end-of-life care.
Keywords: Hospitalization, in-hospital death, nursing home, end of life, systematic review
What is already known about the topic?
Nursing homes play an important role in end-of-life care as an increasing number of people spend their last days in this setting.
End-of-life hospitalizations in nursing home residents are common, although they often result in aggressive treatment, inconsistent with the residents’ preferences.
The proportion of in-hospital deaths is often considered as an indicator for potentially inappropriate care at the end of life.
What this paper adds?
Our systematic review found a wide variation in the proportion of in-hospital deaths between countries but also between studies from the same country, ranging between 5.9% and 77.1%.
More than half of all studies were conducted in the United States, and the majority of studies were limited to the place of death.
The few studies examining age and sex differences indicate that males were more often hospitalized at the end of life or died in hospital than female residents, as were younger residents compared to residents of higher age.
Implications for practice, theory, or policy
Countries or regions with low proportions of end-of-life hospitalizations should serve as examples to those with high proportions to improve end-of-life care in nursing homes by adopting targeted interventions, such as advance care planning or palliative approaches.
Future studies should not only focus on the site of death but also examine patterns of end-of-life care.
Introduction
Even though palliative care, hospice care, and advance care planning have become more common in nursing homes in recent years to improve end-of-life care, these are not yet routinely available in this setting.1,2 Most people wish not to die in hospital,3–5 but do-not-hospitalize orders in nursing homes are rare, often not interpreted literally or even unknown in many countries.6
Although in some situations, hospital admissions at the end of life might be considered appropriate and unavoidable,7,8 it is often critically discussed whether the benefit of hospitalization outweighs potential burdens. Prior research has shown that emergency department and hospital admissions often result in various health complications like gastrointestinal or respiratory tract infection, delirium, functional decline, pressure ulcers, or antibiotic-resistant bacteria in nursing home residents.9 The psychologic burden is also immense, which translates to higher emotional distress as well as a decreased quality of end-of-life care.10,11 Despite this, mortality is high during hospitalizations of nursing home residents12,13 and end-of-life hospitalizations within this population are often considered to measure potentially inappropriate admissions.14,15
Overall, large variations in hospital deaths among the general population were found between European countries.16 This also seems to be the case among nursing home residents. For instance, the percentage of in-hospital deaths of nursing home residents varies widely not only internationally (e.g. Scotland with 11%17 vs the United States with about 32%)18 but also between neighboring countries or even within countries.14,19,20 Previous studies also analyzed different years or measured hospitalizations during different periods before death.21–23 Nevertheless, hospitalization rates of nursing home residents steadily increase as death approaches, especially during the last month of life.24,25 End-of-life hospitalizations of nursing home residents and differences between studies have not yet been systematically evaluated, however.
Therefore, the aim of our systematic review is to summarize the literature on the proportion of deceased nursing home residents with end-of-life hospitalizations. We also focused on the influence of age and sex as well as on differences across countries and time periods.
Methods
A protocol was registered in the PROSPERO database (CRD42017072276). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement for reporting this systematic review.26
Data sources and searches
The literature search was performed using PubMed, CINAHL, and Scopus, which were searched from inception until 24 October 2017 (see Table A1 in the supplemental appendix for the search strategy). The search was rerun on 9 April 2019 to identify any relevant studies published since the original search date. We used an adapted version of the search strategy of a previous systematic review on hospitalization in nursing home residents27 and added search terms for end of life. In addition, we scanned the reference lists of included studies.
Eligibility criteria
We included studies reporting on the proportion of end-of-life hospitalizations of deceased nursing home residents due to all causes. End of life was defined as the last month before death. Therefore, studies had to provide information on the proportion of deceased nursing home residents who had been in hospital during any period in the last month of life (e.g. the last 30, 14, 7 days) or on the proportion of deceased residents who had died in hospital (i.e. in-hospital death). Published observational and interventional studies were eligible for inclusion. We also included studies from countries using other terms for nursing homes (e.g. long-term care facilities in the United States, care homes with nursing in the United Kingdom, or residential care facilities in Australia). We excluded studies on other kinds of institutions, such as assisted living facilities or long-term care hospitals. We also excluded studies limited to residents from skilled nursing facilities, as these might be quite different compared to long-term care residents. Interventional studies that neither reported baseline data nor had a control group and studies with a sample size smaller than 100 deceased nursing home residents were also excluded, as they are not considered to ensure robust and generalizable results. Furthermore, studies limited to specific groups of nursing home residents, such as residents with cognitive impairment or residents who died non-suddenly, and studies referring to specific hospital admissions (e.g. specific diagnoses) were excluded. When authors published multiple reports based on the same dataset and outcome, only the report with the larger sample size was included. No language restrictions were imposed.
Study selection and data extraction
After removing duplicates, two of the authors independently screened articles based on title and abstract for inclusion or exclusion. The full text of all articles that met the inclusion criteria was independently assessed by the two reviewers, and any disagreement was resolved by discussion or by a third reviewer.
We abstracted data for study characteristics (e.g. country, data source), resident characteristics (mean age, sex, dementia), and outcome results. We used a standardized data abstraction form. Data extraction was performed by one reviewer and verified by a second. Discrepancies were resolved by discussion or by a third reviewer. When proportions were not directly specified in the publication, we calculated it, whenever possible, by dividing the number of nursing home residents being hospitalized or dying in hospital by all deceased residents. If the original publication stratified its results by different groups, such as hospice versus non-hospice residents, we reported the results for all residents. If a study examined all discharges from the nursing homes (i.e. all deaths as well as all discharges to other facilities), we used data for deceased residents only.
Quality assessment
Two reviewers independently assessed the quality of included studies using the Joanna Briggs Institute’s critical appraisal checklist for studies reporting prevalence data, which includes nine items.28 We chose this tool because of its flexibility to be used across different study designs.29 Any disagreement between the two reviewers was resolved by discussion. If necessary, a third reviewer was involved. The assessment of study quality was performed to establish the validity of studies, but it had no impact on the inclusion or exclusion of the study.
Data synthesis
We analyzed the results using a narrative synthesis and by calculating overall medians and interquartile ranges (IQR) to summarize proportions derived from individual studies. If a study reported proportions for several years, only the latest year was included. Data analyses were performed using SAS for Windows version 9.4 (SAS Institute Inc, Cary, North Carolina, USA). Given the expected heterogeneity between studies, a meta-analysis was not planned.
Furthermore, we analyzed differences between age and sex, when reported. We also reported the influence of facility characteristics on end-of-life hospitalizations that were statistically assessed in at least three studies. According to the protocol, a subgroup analysis was planned to compare end-of-life hospitalizations between nursing home residents with and without dementia. Since only few studies compared those two groups and most studies are limited to residents with dementia without a control group, which were excluded in this review, we decided to do a separate systematic review on this topic (PROSPERO CRD42018104263).
Results
Literature search
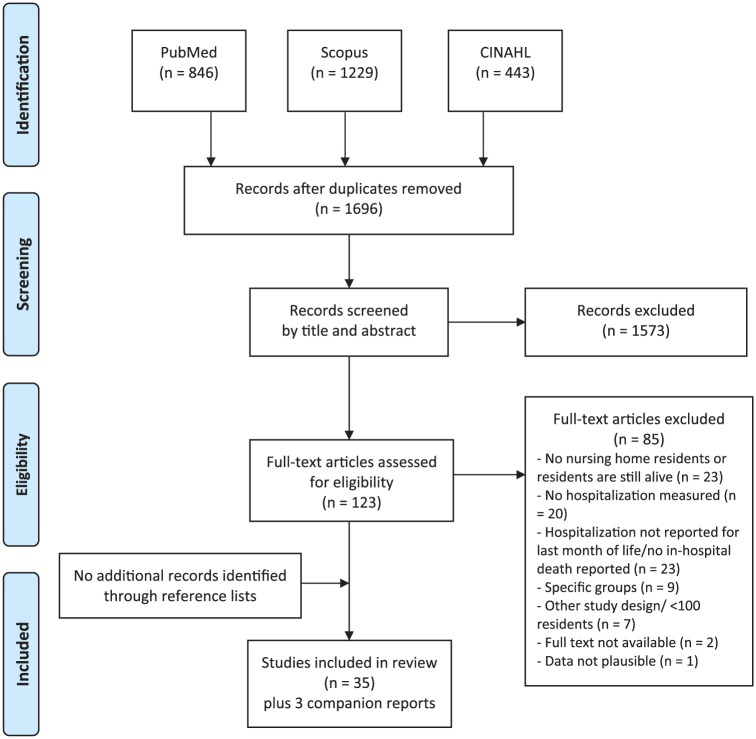
The literature search resulted in a total of 1696 articles, of which 123 were deemed potentially relevant. We excluded 85 full-text articles that did not meet the inclusion criteria. Full texts could not be retrieved for two studies. A total of 35 studies and 3 companion reports fulfilled our inclusion criteria (Figure 1).
Figure 1.
Flowchart.
Study characteristics
The characteristics of the 35 included studies are shown in Table 1. The data used were generated between 1992 and 2016. More than half of all studies are from the United States (n = 18),18,20,30–45 five from Japan,46–50 four from Canada,14,24,51,52 two from the United Kingdom,17,53 two from Australia,54,55 two from Germany,59,60 and one each from Belgium56 and France.57 The sample size ranged between 102 and 2,954,276 residents.
Table 1.
Baseline characteristics of the studies included (by country).
| Country | References | Data source | Year of dataa | Number of deceased residents | Number of included facilities | Inclusion/exclusion criteria | Age at death (% females) | Deceased residents with dementia |
|---|---|---|---|---|---|---|---|---|
| United States | Cai et al.30 | Linkage of MDS and Medicare data | July 2007–September 2010 | 394,948 | Not reported | Inclusion criteria - Residents aged ⩾65 years - Long-term residents (⩾90 days) - NH decedents defined as those who were in NH within 7 days before death |
Mean age: 85.4 yearsb,c (71.6%)c | 65.8%c |
| United States | Cai et al.31 | Linkage of MDS, Medicare claims and OSCAR | January 2000–December 2009 | 2,954,276 | 14,294 | Inclusion criteria - Residents who were in NH for the last 30 days of life - Freestanding NH with at least 8 years of data and at least 30 beds |
Not reported | Not reported |
| United States | Gozalo and Miller32 | Linkage of MDS, Medicare claims, OSCAR, hospice provider of service files, and ARF | January 1995–December 1997 | 183,742 (hospice and non-hospice) | Not reported | Inclusion criteria - Residents who were not enrolled in hospice before their NH admission |
Mean age: 85.0 yearsc (67.2%)c | 47.1%c |
| United States | Intrator et al.33 | Linkage of MDS, Medicare claims, and OSCAR | 2006 | 5379d | 202d | No patient characteristics as exclusion criteria | Not reported | Not reported |
| United States | Kelly et al.34 | Interviews with family caregivers (Sample of the Health and Retirement Study) | January 1992–December 2006 | 1817 | Not reported | Inclusion criteria - Residents aged ⩾50 years |
Mean age: 83.3 yearsb (59.1%) | Not reported |
| United States | Levy et al.35 | MDS, Veterans Affairs Vital Statistics files, Veterans Health Administration Support Services Center Datasets Library | June 2005–May 2007 | 7408 | Not reported | Inclusion criteria - Veterans living in Veterans Affairs NH |
Median age: 78 years (2.5%) | Not reported |
| United States | Li et al.36 | Linkage of MDS, Medicare beneficiary file, hospice claims, and hospital claims, LTCFocUS.org | January 2003–December 2007 | 1,261,726 (2007: 236,619) | 16,347 (2007: 15,098) |
Inclusion criteria - Residents aged ⩾ 65 years - Long-term residents (> 3 months) - Residents who died in LTC facility or in hospital within 8 days Exclusion criteria - Rehabilitation and postacute residents - Residents in coma |
2007: Mean age: 86.6 years (69.9%) |
2007: 60.9% |
| United States | Miller et al.37 | Linkage of survey data, MDS, Medicare claims, OSCAR, and ARF | July 2009–June 2010 | 58,876 | 1981 | Inclusion criteria for in-hospital death - Resident died in an acute care hospital within 7 days of transfer from the NH Exclusion criteria - Residents in coma Exclusion criteria for any hospitalization in last 30 days of life - Residents with less than a 30 day total nursing home stay |
Not reported | Not reported |
| United States | Miller et al.38 | Linkage of palliative care consult data, OSCAR, MDS, Medicare claims, and ARF | 2000–2010 | Not reported | 148 | Exclusion criteria - NH that operated for less than 3 years - Others with less than 3 years of data |
Not reported | Not reported |
| United States | Mukamel et al.39 | Linkage of MDS, Medicare enrollment files, hospital claims, and hospice claims | 2003–2007 | 1,447,926 | >16,000 | Inclusion criteria - Long-term residents (>3 months) - Residents who died in NH, or within 8 days of a NH stay Exclusion criteria - Residents in coma |
Mean age: 86.3 years (69.0%) | Not reported |
| United States | Mukamel et al.18 | Linkage of MDS and vital status data | October 2012–September 2013 | 39,590 | 626 | Inclusion criteria - All residents who died in the NH or died in the hospital within 18 days of being discharged from the NH to the hospital |
Mean age: 84.7 years (61.9%) | 56.6%c |
| United States | Sloane et al.40 | After-death interviews with staff and family respondents (Collaborative Studies of Long-Term Care (CS-LTC)) | July 2002–January 2005 | 314d | 31d | Inclusion criteria - Having spent 15 of the last 30 days of life in a study facility - Having died no more than 3 days after leaving the facility |
Not reported | 78.7%c |
| United States | Temkin-Greener et al.41 | Linkage of MDS, Medicare beneficiary file, inpatient and hospice claims | January 2005–December 2007 | 915,688 | 13,206 | Inclusion criteria - Residents aged ⩾65 years - Long-term residents (>3 months) - Decedents who died in a NH or within 8 days of discharge to a different care setting Exclusion criteria - Facilities with <20 decedents |
Not reported | Not reported |
| United States | Temkin-Greener et al.20 | Linkage of MDS, Medicare denominator file, and Medicare inpatient and hospice claims | January 2003–December 2007 | 2,530,374 | 16,872 | Inclusion criteria - Decedents who died in a NH or within 8 days of discharge to a different care setting |
Age groups <65 years: 3.6% 65–74 years: 10.8% 75–84 years: 28.3% 85+ years: 57.3% (63.8%) |
Not reported (only for Alzheimer) |
| United States | Temkin-Greener et al.42 | Linkage of MDS and vital status data | October 2012–April 2016 | 119,486e | 609e | Inclusion criteria - Residents aged ⩾65 years - Died in NH or died in acute care hospital within 18 days |
Mean age: 84.7 years (61.7%) | 57.9%c |
| United States | Teno et al.43 | MDS, Medicare enrollment and inpatient hospitalization data, OSCAR | 1999–2007 | Not reported | 15,784 | Inclusion criteria - Residents aged ⩾66 years - NH with at least 25 deaths per year - Residents residing in a NH at least 8 days prior to death |
Not reported for deceased residents | Not reported |
| United States | Zheng et al.44 | Linkage of MDS, Medicare inpatient and hospice claims | January 2005–December 2007 | 49,048 | 555 | Inclusion criteria - Residents aged ⩾ 65 years - Long-term residents (> 3 months) - Black and white NH decedents (other minority groups were not included) Exclusion criteria - Residents who were transferred to a different NH after last MDS health assessment - Residents in coma - Decedents from facilities that are: - <70 beds - With no black residents - With more than 90% of residents being black |
Mean age: 87.1 yearsb,c (70.7%)c | Not reported |
| United States | Zheng et al.45 | Linkage of MDS and Medicare Beneficiary File, Inpatient and Hospice Claims, Provider of Services File and ARF | January 2005–December 2007 | 747,641 (hospice and non-hospice) | 14,030 | Inclusion criteria - Long-term residents (>3 months) Exclusion criteria - Facilities with less than 20 decedents - Residents in coma |
Mean age: 86.7 yearsc (70.9%)c | Not reported (only for Alzheimer) |
| Japan | Hirano et al.46 | Medical records, death certificates, notes of nurses, caregivers, and counseling staff | April 1998–June 2008 | 131d | 1 | No patient characteristics as exclusion criteria | Mean age: 87.6 yearsc | 90.1%c |
| Japan | Ikegami and Ikezaki47 | NH questionnaires | 2009 | 1158 | 241 | No patient characteristics as exclusion criteria | Mean age: 88.5 years (70.5%) | Not reported |
| Japan | Nakanishi et al.48 | Survey data | 2007, 2010, 2013 | 1647 | Not reported | Exclusion criteria - Residents covered by respite care |
Mean age: 88.8 yearsc (74.7%)c | 25.8%c |
| Japan | Shinoda-Tagawa and Ikegami49 | National survey data | November 2002–December 2002 | 4175 | 835 | No patient characteristics as exclusion criteria | Mean age: 87.1 yearsc (72.3%)c | Not reported |
| Japan | Takezako et al.50 | Nursing home records (chart review) | April 1999–September 2004 | 102f | 1 | Inclusion criteria - All deceased residents who died in the NH or in hospital Exclusion criteria - Those who were predicted to have a long hospital stay (>1 month) and agreed to be discharged from the NH - Those who once were discharged and readmitted to the NH |
Mean age: 86.6 years (77%)f | 65%f |
| Canada | Krishnan et al.14 | Review of medical charts, Resident Assessment Instrument-Minimum Data Set (RAI-MDS), and review of death certificates | April 2010–March 2013 | 118 | 1 | No patient characteristics as exclusion criteria | Mean age: 88.8 years (79.7%) | Not reported |
| Canada | Krishnan et al.51 | Data from interviews with family members | May 2006–December 2008 | 119 | Not reported | No patient characteristics as exclusion criteria | Mean age: 86.7 years (58.8%) | 68.1% |
| Canada | McGrego et al.52 | Secondary administrative data from the Ministry of Health, supplemented with facility data | April 1996–August 1999 | 14,413 | Not reported | Inclusion criteria - Residents aged ⩾65 years - Freestanding publicly funded NH - Died within 30 days of hospital admission Exclusion criteria - NH attached to a hospital - Deaths occurring in mental health group homes, dedicated rehabilitation and palliative care facilities, those receiving respite or personal care |
65–74 years: 7.7%c
75–79 years: 11.8%c 80–84 years: 21.1%c 85–89 years: 26.9%c 90–94 years: 20.7%c ⩾95 years: 11.7%c (62.6%)c |
Not reported |
| Canada | Menec et al.24 | Administrative health care records | January 2003–December 2004 | 2379 | 60 | Inclusion criteria - Facilities with at least 20 deaths Exclusion criteria - Individuals who died in locations other than a hospital or LTC facility |
<74 years: 9.2%b
75–84 years: 29.5%b 85–94 years: 48.2%b ⩾95 years: 13.1%b (64.2%) |
Not reported |
| UK | Finucane et al.17 | Case note review | May 2013–January 2014 | 120 | 8 | No patient characteristics as exclusion criteria | Mean age: 86 yearsb (61.9%)c |
74% |
| UK | Kinley et al.53 | Notes and daily records from NH that were participating in the Gold Standards Framework in Care Homes (GSFCH) program | June 2008–May 2011 | 2444 | 38 | No patient characteristics as exclusion criteria | Mean age: 85 yearsb (61%) |
47.5% |
| Australia | Chapman et al.54 | Quasi-experimental study of specialist palliative care | January 2012–December 2014e | 173e | 4 | No patient characteristics as exclusion criteria | Mean age: 86.6 years (63.6%)c,e |
30.1%c,e |
| Australia | Horey et al.55 | Interviews with RACF staff and GPs, RACF manager surveys, and prospective audits of deaths and EOL care pathway use, resident records (The Good Death Project) | April 2008–April 2009 | 267e | 14e | No patient characteristics as exclusion criteria | Not reported | Not reported |
| Belgium | De Gendt et al.56 | Structured mail questionnaires | September 2006–October 2006 | 1240d | 318d | No patient characteristics as exclusion criteria | Mean age: 86 years (68.9%) |
65.2% |
| France | Morin et al.57 with companion report58 | Survey data | 2013 | 70,622 | 3705 | Inclusion criteria All deceased residents in France who died in 2012 |
Not reported | Not reported |
| Germany | Hoffmann and Allers59 with companion report25 | Health insurance claims data | January 2010–December 2014 | 67,328 | Not reported | Inclusion criteria - Residents aged ⩾65 years - Newly admitted to a NH between 2010 and 2014 |
Mean age: 85.3 years (69.8%) |
43.1% |
| Germany | Ramroth et al.60 with companion report61 | Data from examinations by the medical service of the social health insurance plans and records of the health insurance plans | 2000–2001 | 792 | 97 | Inclusion criteria - Newly admitted to a NH in 2000 |
Mean age: 84.7 yearsb (70.7%) |
Not reported |
MDS: minimum data set; NH: nursing home; OSCAR: online survey certification and reporting system; ARF: area resource file; LTC: long-term care; RACF: residential aged care facility; GP: general practitioner; EOL: end of life.
Proportions are reported with one decimal place (provided decimal places were given or could be calculated).
Month of data collection are reported whenever these were provided in the respective study.
Age/dementia not (explicitly) reported for the time of death.
Calculated by the reviewers based on data given in the publication.
Sample differs from the total study sample as we were only interested in deceased nursing home residents.
Residents included in control/baseline group or pre-implementation period.
Study inclusion criteria required that residents had not died suddenly (n = 86), we added the given number of sudden deaths (n = 16); data for age, sex, and dementia apply only to the residents who died non-suddenly.
Overall, 26 and 25 studies included in the review reported data on all deceased residents’ age and sex, respectively. The mean or median age in the studies ranged from 70 to 89 years and was measured at different points of time, for example, age at nursing home admission or at time of death. Female residents were in the majority in 24 studies, ranging from 59.1% to 79.7%. One study examined decedents from veteran nursing homes with predominantly male residents.35 The proportion of residents with dementia was reported in 15 studies and varied between 25.8% and 90.1% (median: 60.9%; IQR: 47.1%–68.1%).
Methodological quality and risk of bias
The quality assessment for each study is presented in Table A2 (supplemental appendix). In a total of 25 studies (71.4%), the sample frame was appropriate to address the target population of all nursing home residents. In the majority of studies (88.6%), study participants were sampled in an appropriate way, and the sample size was adequate in 77.1%. End-of-life hospitalizations were measured with valid methods in most studies (74.3%).
In-hospital deaths
Overall, 29 out of 35 studies reported a proportion of in-hospital deaths, which ranged from 5.9% in a Canadian study14 to 77.1% in a study from Japan46 (Table 2), with an overall median of 22.6% (IQR: 16.3%–29.5%). Comparing countries with three or more studies, the country with the highest median rate of in-hospital deaths was Japan (52.7%; IQR: 49.0%–64.1%; n = 5). The United States and Canada had a median proportion of in-hospital deaths of 17.5% (IQR: 16.0%–22.6%; n = 13) and 19.1% (IQR: 5.9%–24.6%; n = 3), respectively.
Table 2.
Results of the studies included.
| Country | References | Year of data | Proportion of residents with hospitalizations during the last month of life | Proportion of in-hospital deaths |
|---|---|---|---|---|
| United States | Cai et al.30 | 2007–2010 | Last 30 days of life: 33.0%a | – |
| United States | Cai et al.31 | 2000–2009 | Last 30 days of life 2000: 24.8% 2009: 33.3% |
– |
| United States | Gozalo and Miller32 | 1995–1997 | Last 30 days of life: 42.0%a | – |
| United States | Intrator et al.33 | 2006 | – | 17.5% |
| United States | Kelly et al.34 | 1992–2006 | – | 22.6% |
| United States | Levy et al.35 | 2005–2007 | – | 13.4% |
| United States | Li et al.36 | 2003–2007 | – | 2003: 16.5% 2004: 17.2% 2005: 17.0% 2006: 16.5% 2007: 16.3% |
| United States | Miller et al.37 | 2009–2010 | Last 30 days of life: 30.9% | 15.0% |
| United States | Miller et al.38 | 2000–2010 | Last 30 days of life: 29% | 16% |
| United States | Mukamel et al.39 | 2003–2007 | – | 20.3% |
| United States | Mukamel et al.18 | 2012–2013 | – | 31.7% |
| United States | Sloane et al.40 | 2002–2005 | Last month of life: 25.5%a | 8.4%a |
| United States | Temkin-Greener et al.41 | 2005–2007 | – | 17.4% |
| United States | Temkin-Greener et al.20 | 2003–2007 | Last 30 days of life 2003: 31.9% 2004: 33.4% 2005: 33.8% 2006: 34.1% 2007: 34.7% |
2003: 20.6% 2004: 20.5% 2005: 20.5% 2006: 20.3% 2007: 20.3% |
| United States | Temkin-Greener et al.42 | 2012–2016 | – | 31.2b |
| United States | Teno et al.43 | 1999–2007 | Last 7 days of life 1999: 15.0% 2007: 14.8% |
– |
| United States | Zheng et al.44 | 2005–2007 | – | 25.6%a |
| United States | Zheng et al.45 | 2005–2007 | Last 30 days of life: 33.0%a | – |
| Japan | Hirano et al.46 | 1998–2008 | – | 77.1% |
| Japan | Ikegami and Ikezaki47 | 2009 | – | 52.7%a |
| Japan | Nakanishi et al.48 | 2007, 2010, 2013 | – | 46.9%a |
| Japan | Shinoda-Tagawa and Ikegami49 | 2002 | – | 64.1% |
| Japan | Takezako et al.50 | 1999–2004 | – | 49.0%a |
| Canada | Krishnan et al.14 | 2010–2013 | – | 5.9% |
| Canada | Krishnan et al.51 | 2006–2008 | Last month of life: 69.7% | – |
| Canada | McGregor et al.52 | 1996–1999 | Last 30 days of life: 30.6%a | 24.6% |
| Canada | Menec et al.24 | 2003–2004 | – | 19.1% |
| UK | Finucane et al.17 | 2013–2014 | – | 10.8%a |
| UK | Kinley et al.53 | 2008–2011 | Last month of life: 34% | 27% |
| Australia | Chapman et al.54 | 2012–2014 | – | 24.9%a, b |
| Australia | Horey et al.55 | 2008–2009 | – | 14.2%b |
| Belgium | De Gendt et al.56 | 2006 | – | 19.7% |
| France | Morin et al.57 | 2013 | – | 25.3% |
| Germany | Allers and Hoffmann25,59 | 2010–2014 | Last month of life: 51.5% Last week of life: 37.4% |
29.5% |
| Germany | Ramroth et al.62 | 2000–2001 | – | 28.9% |
Proportions are reported with one decimal place (provided decimal places were given in the publication or could be calculated).
Calculated from data given in the publication.
Data refer to control group/baseline group or pre-implementation period.
Nine studies provided sex-specific proportions of in-hospital deaths, and this proportion was greater in males in all studies.14,20,24,35,47–49,52,59 Ten studies compared age distribution by place of death. Eight out of these 10 studies found that older residents died less often in hospital than younger residents,20,24,46–49,52,59 while two studies found no difference between the mean/median age of those who died in a nursing home and those who died in a hospital.14,35 Nine studies used logistic regression to determine the relationship between in-hospital death and age and sex. Male residents were significantly more likely to die in hospital in four studies,36,47,52,59 while four further studies18,24,44,49 found higher odds for male residents, but the figures were not statistically significant. In one study, female sex was associated with slightly higher odds of in-hospital death.39 Younger age was associated with a higher likelihood of in-hospital death in all nine studies (Table 3).18,24,36,39,44,47,49,52,59
Table 3.
End-of-life hospitalizations by age and sex.
| Country | References | Hospitalizations during the last month of life by age and sex |
In-hospital deaths by age and sex |
||
|---|---|---|---|---|---|
| Proportion | Model | Proportion | Model | ||
| United States | Gozalo and Miller32 | – | Last 30 days of life Age <75 years: Reference 75–80 years: OR = 1.03 (95% CI = 0.99–1.07) 80–85 years: OR = 0.99 (95% CI = 0.95–1.03) 85–90 years: OR = 0.95 (95% CI = 0.91–0.98) 90+ years: OR = 0.78 (95% CI = 0.74–0.81) Sex Male: OR = 1.07 (95% CI = 1.05–1.10) Female: Reference |
– | – |
| United States | Levy et al.35 | – | – | Median age of residents that died in Hospital: 78.6 years vs NH: 78.1 years, p = 0.26 Sex Male: 13.5%a Female: 12.0%a |
– |
| United States | Li et al.36 | – | – | – | Age (in years) OR = 0.70 (95% CI = 0.50–0.98) Sex Male: Reference Female: OR = 0.93 (95% CI = 0.90–0.95) |
| United States | Mukamel et al.39 | – | – | – | Age (in years) OR = 0.71,a p < 0.001 Sex Male: Reference Female: OR = 1.06,a p < 0.001 |
| United States | Mukamel et al.18 | – | – | – | Age (in years) OR = 0.98,a p < 0.001 Sex Male: OR = 1.06,a p ⩾ 0.05 Female: Reference |
| United States | Temkin-Greener et al.20 | – | – | Age <65 years: 28.0% 65–74 years: 25.6% 75–84 years: 23.1% 85+ years: 17.7% Sex Male: 22.4% Female: 19.3% |
– |
| United States | Zheng et al.44 | – | – | – | Age <80 years: Reference 80–90 years: OR = 0.90 (95% CI = 0.85–0.96) >90 years: OR = 0.77 (95% CI = 0.72–082) Sex Male: Reference Female: OR = 0.99 (95% CI = 0.94–1.04) |
| Japan | Hirano et al.46 | – | – | Mean age of residents that died in Hospital: 86.5 years vs NH: 91.3 years |
– |
| Japan | Ikegami and Ikezaki47 | – | – | Mean age of residents that died in Hospital: 87.9 years vs NH: 89.2 years Proportion of male residents that died in Hospital: 32.2% vs NH: 26.5% |
Association with dying in a NH Age (in years) Unadjusted OR = 1.02 (95% CI = 1.00–1.04) Sex Male: Reference Female: Unadjusted OR = 1.33 (95% CI = 1.03–1.71) |
| Japan | Nakanishi et al.48 | – | – | Mean age of residents that died in Hospital: 87.7 years vs NH: 89.8 years, p < 0.001 Sex Male: 56.6%a Female: 43.7%a |
– |
| Japan | Shinoda-Tagawa and Ikegami49 | – | – | Mean age of residents that died in Hospital: 86.4 years vs NH: 88.5 years, p < 0.001 Sex Male: 70.4%a Female: 61.6%a |
Association with dying in a NH Age (in years): OR = 1.02 (95% CI = 1.01–1.05) Sex Male: OR = 0.8 (95% CI = 0.6–1.2) Female: Reference |
| Canada | Krishnan et al.14 | – | – | Mean age of residents that died in Hospital: 88.9 years vs NH: 88.8 years, p = 0.992 Sex Male: 8.3% Female: 5.3%, p = 0.629 |
– |
| Canada | McGregor et al.52 | – | – | Age 65–74 years: 34.2% 75–79 years: 27.7% 80–84 years: 26.5% 85–89 years: 25.2% 90–94 years: 21.5% 95+ years: 15.5% Sex Male: 27.8% Female: 22.7% |
Age 65–74 years: Reference 75–79 years: OR = 0.69 (95% CI = 0.58–0.83) 80–84 years: OR = 0.63 (95% CI = 0.53–0.74) 85–89 years: OR = 0.57 (95% CI = 0.48–0.66) 90–94 years: OR = 0.45 (95% CI = 0.38–0.53) 95+ years: OR = 0.33 (95% CI = 0.27–0.40) Sex Male: OR = 1.17 (95% CI = 1.07–1.27) Female: Reference |
| Canada | Menec et al.24 | – | – | Age ⩽74 years: 29.2% 75–84 years: 24.0% 85–94 years: 16.7% 95+ years: 9.9% Sex Male: 21.7% Female: 17.6% |
Age ⩽74 years: OR = 3.308 (95% CI = 1.990–5.497) 75–84 years: OR = 2.792 (95% CI = 1.814–4.295) 85–94 years: OR = 1.839 (95% CI = 1.213–2.787) 95+ years: Reference Sex Male: OR = 1.187 (95% CI = 0.945–1.492) Female: Reference |
| Germany | Hoffmann and Allers59 | – | – | Age 65–74 years: 27.5% (26.5%–28.6%) 75–84 years: 32.1% (31.5%–32.8%) 85–94 years: 29.6% (29.1%–30.1%) 95+ years: 21.7% (20.6%–22.9%) Sex Male: 32.4% (31.8%–33.1%) Female: 28.3% (27.9%–28.7%) |
Age 65–74 years: OR = 1.50 (95% CI = 1.37–1.64) 75–84 years: OR = 1.77 (95% CI = 1.64–1.91) 85–94 years: OR = 1.49 (95% CI = 1.39–1.60) 95+ years: Reference Sex Male: OR = 1.24 (95% CI = 1.19–1.28) Female: Reference |
OR: odds ratio; CI: confidence interval; NH: nursing home.
Proportions are reported with one decimal place (provided decimal places were given in the publication or could be calculated).
Calculated from data given in the publication.
Four studies assessed the time spent in hospital before death. One study from Germany reported that the terminal hospital stay lasted on average 9 days and the length of hospital stay was 1 day in 9.8%, up to 3 days in 32.6% and up to 7 days in 58.8%.60 Another study from Germany also reported that the last hospital stay lasted less than 3 days for 33.2% of residents who died in hospital,60 while another study from Scotland found that of the 13 residents who died in hospital, 7 died within 3 days of admission (53.8%).17 A study from Japan showed that 18% of those who died in hospital died within 24 h of admission.49
Hospitalizations during the last month of life
Twelve out of the 35 studies (eight from the United States, two from Canada, and one each from the United Kingdom and Germany) assessed the proportion of residents being in hospital during the last month of life and found proportions ranging from 25.5% to 69.7% (Table 2).20,25,30–32,37,38,40,45,51–53 The overall median of the 12 studies was 33.2% (IQR: 30.8%–38.4%).
Only one study examined the influence of age and sex on hospitalizations in the last month of life. Logistic regression was used in this study, and male sex was associated with a higher likelihood, whereas older age was associated with a lower likelihood of hospitalization in the last month of life (Table 3).32
Besides in-hospital deaths (n = 29) and hospitalizations during the last month of life (n = 12), only one further period was assessed. Two studies examined the hospitalizations in the last week of life, reporting a proportion of end-of-life hospitalizations of 14.8%43 and 37.4%25 (Table 2). Differences by age and sex were not assessed.
Longitudinal trends
Four studies, all from the United States, assessed trends over time.20,31,36,43 Two studies analyzed a period of 5 years,20,36 one of 9 years43 and one of 10 years31 up to the year 2009. Findings varied between studies. While in two studies, in-hospital deaths and hospitalizations during the last 7 days of life remained virtually unchanged,36,43 one study found an increase in hospitalizations during the last 30 days of life from 24.8% in 2000 to 33.3% in 2009.31 Another study found an increase in the likelihood of in-hospital death in a multivariable analysis between 2003 and 2007, as well as in the proportion with hospitalizations during the last 30 days of life.20
Influence of facility characteristics on end-of-life hospitalizations
Facility characteristics reported in at least three studies were for-profit ownership, smaller nursing home size, higher number of registered nurses, and availability of physicians (Table 4). The nine studies included were from the United States (n = 3),36,38,41 Canada (n = 3),24,51,52 and Japan (n = 3).47,49,50 The results were rather inconclusive. While two studies found that for-profit facilities had higher odds of in-hospital death,24,41 two others reported no significant differences.36,52 Four out of five studies reported no association with respect to nursing home size.36,41,49,51,52 While in some studies a higher number of registered nurses or a higher availability of physicians was associated with a decreased chance of end-of-life hospitalization,36,49,50 others reported no significant results.38,41,47,51
Table 4.
Influence of facility characteristics on end-of-life hospitalizations.
| Facility characteristics | ↑ (increase of end-of-life hospitalization) |
↔ (no significant association) |
↓ (decrease of end-of-life hospitalization) |
|---|---|---|---|
| For-profit ownership | Menec et al.24
Temkin-Greener et al.41 |
Li et al.36
McGregor et al.52 |
– |
| Small NH size | McGregor et al.52 | Temkin-Greener et al.41
Li et al.36 Shinoda-Tagawa and Ikegami49 Krishnan et al.51 |
– |
| Staffing capacity/higher number of registered nurse hours per resident per day | – | Miller et al.38
Temkin-Greener et al.41 |
Li et al.36 |
| Availability of physicians | – | Ikegami and Ikezaki47
Krishnan et al.51 |
Takezako et al.50
Shinoda-Tagawa and Ikegami49 |
NH: nursing home.
Discussion
Main findings
We systematically examined the epidemiology of hospitalizations shortly before death and found the proportions of in-hospital deaths ranging from 5.9% to 77.1% across studies, with a median of 22.6%. In studies assessing the last month of life, there was less heterogeneity, with about one-third of residents being hospitalized within the last month of life. More than half of all studies were conducted in the United States. The majority of studies reported proportions of in-hospital deaths, and only one-third of studies assessed other periods during the last month before death. Most studies indicate that males were more often transferred to hospitals at the end of life and died in hospital than female residents, as were younger residents compared to residents of higher age. However, few studies examined differences between age and sex, and only four studies assessed trends, showing mixed findings.
On one hand, we found varying prevalences of end-of-life hospitalizations across countries. Overall, the highest median proportion was reported for Japan, with more than half of residents dying in hospital.46–49 One explanation for frequent end-of-life hospitalizations in Japan compared to Western countries is that many Japanese nursing homes do not provide 24-h nursing care.47 The study with the lowest proportion of in-hospital deaths is from Canada. The authors suggest as one reason that this low proportion may be related to a full-time nurse practitioner who is available within the facility as well as the high frequency of advance care planning.14 The latter might be supported by our finding of lower proportions of in-hospital deaths in countries that already have comprehensive advance care planning programs (e.g. Australia, Belgium) compared to countries with less implementation of advance care planning (e.g. Germany, Japan). Advance care planning aims to define a person’s preferences regarding future medical treatment and care before their health deteriorates.62 In this way, unwanted transfers to hospital at the end of life can be reduced, while the use of palliative care, the quality of life, and patient satisfaction with care can be increased.1,62,63 Instead of life-prolonging treatments, palliative care approaches and quality of life seem to play a more important role in some countries like the Netherlands.16,64 For instance, the majority of residents with dementia had a palliative care goal on the day of death in a Dutch study although advance directives were rare.65 Furthermore, the availability of skilled nursing home professionals and medical resources probably explain why in some countries a greater percentage of residents die in the nursing home instead of a hospital.16,66
On the other hand, even in a given country, the proportions of in-hospital deaths varied widely, for example, ranging from 8.4% to 31.7% in the United States. Our findings are in line with those of Temkin-Greener et al.20 and Levy et al.,67 who found substantial, though much smaller, variation across different regions in the United States. This is also consistent with a French study showing major regional differences.57 Explanations for such variations discussed by the authors include different state regulation policies20 as well as differences in region-specific end-of-life practices and medical cultures as well as varying perceptions with regard to hospitalizations.57 In addition, several studies found that advance care planning or the presence of advance directives including do-not-hospitalize and do-not-resuscitate orders as well as hospice care were associated with lower proportions of end-of-life hospitalization, irrespective of the country where the study was conducted.20,32,33,45,54,56
With increasing age, residents are less likely to be transferred to hospital near end of life which suggests less aggressive treatment in older age. Although the findings on the influence of sex on end-of-life hospitalizations are less conclusive, some studies indicate that male sex was associated with higher proportions and odds of end-of-life hospitalizations, including when controlling for age. These sex differences were also found when assessing all hospitalizations of nursing home residents, not restricting to end of life,27 as well as for populations outside the nursing home.16 This suggests that men may receive more aggressive treatment compared to women. The reasons for these differences, however, are not clear.27,68
Besides the above-mentioned aspects, there might also be other relevant resident as well as facility-level characteristics predicting end-of-life hospitalizations. We assessed the influence of facility characteristics on end-of-life hospitalizations and found inconclusive results. However, we only included facility characteristics that were reported in at last three studies to be able to draw robust conclusions and hence not included all potential characteristics that might have an influence. However, a general problem is that many variables are not operationalized uniformly and results are therefore difficult to compare. For example, seven studies investigated the influence of the length of nursing home stay with different operationalization (e.g. categorical, with long-stay (⩾90 days) vs short stay (<90 days), or continuous, in mean number of days) and showed inconclusive findings.14,18,20,32,35,49,59
Furthermore, the time or period at which a study was conducted may also play a role, as, for example, advance care planning has become more common in recent years. Overall, we found only four studies investigating trends over time, which were all conducted in the United States, analyzed data only up to 2009, and showed inconclusive findings. Also, when comparing temporal trends for in-hospital deaths, no clear pattern could be observed. However, comparability is limited due to the heterogeneity of the studies. Nevertheless, studies from the United States found that an increasing number of nursing homes introduced initiatives that aim at reducing potentially avoidable hospitalization.69,70 Those initiatives show promising results, especially by integrating advanced practice registered nurses and interdisciplinary support teams.70–72 This might indicate a shift to an improvement of end-of-life care. However, more studies reporting on trends and including more recent years are needed to support this conclusion.
It is important to bear in mind that we included all studies reporting a proportion of end-of-life hospitalizations, irrespective of whether or not this was the primary outcome. Therefore, we included studies that focus on different research questions, such as racial disparities, advance care planning interventions, palliative care consultations, or the effect of hospice use on terminal hospitalization. Moreover, three studies focused on only one facility and, therefore, their generalizability might be limited. Although we included 35 studies in our review, not all of these studies used end-of-life hospitalizations as a main outcome, and only some studies assessed differences between age or sex (n = 15). Out of 35 included studies, 12 studies focused on the last month and just 2 studies on the last week of life, while the majority of studies reported in-hospital deaths only. Thus, important information about the extent and patterns of end-of-life hospitalizations may be missed.24 Furthermore, just four studies examined length of stay of the last hospitalization, finding that large proportions of residents died shortly after being admitted to hospital. Clearly, more research on hospitalizations in this vulnerable phase of life is needed.
Strengths and limitations
This is the first systematic review that summarizes the existing evidence on the frequency of end-of-life hospitalizations in nursing home residents. However, there are some limitations that must be considered. We might have missed studies that did not focus on end-of-life hospitalizations but mention such a proportion in the full text. However, we used a comprehensive search strategy and screened more than 100 full texts and the references of all included studies, resulting in 35 studies being included in this systematic review. Furthermore, we did not exclude studies based on language or time period.
While some studies compared death occurring in nursing homes to those in hospital only, other studies examined the place of death also, including death at home, at other facilities or in hospice, which might lead to small differences in the relative proportions when comparing the frequency of in-hospital deaths between those studies. However, as only very few residents die outside the nursing home or the hospital, these differences should have little effect on our findings.
To increase comparability, we excluded studies on specific subgroups, such as cognitively impaired residents or sudden deaths. However, the included studies focused on various kinds of research questions, for example, comparing hospice versus non-hospice residents or identifying racial differences. In addition, populations varied widely; for example, studies consisted of residents with different life expectancies, and one study included only veterans. Therefore, comparability is limited. In addition, differences between health care systems as well as types of long-term care facilities limit comparability between countries. Nevertheless, this review provides a comprehensive overview of the global extent of hospitalization of nursing home residents near the end of life.
Conclusion
There is a wide variation in the proportion of nursing home residents with end-of-life hospitalizations not only between countries but also between studies from the same countries. Overall, hospitalizations at the end of life are common among nursing home residents. Countries or regions with low proportions should serve as examples to those with high proportions to improve end-of-life care in nursing homes by adopting targeted interventions, such as advance care planning or palliative approaches. Future studies should not limit their focus on the location of death but also examine the patterns of care during the last weeks of life as well as time spent in hospital before death. Moreover, studies outside the United States that stratify findings by age and sex as well as studies on trends over time are warranted.
Supplemental Material
Supplemental material, Supplementary_file_1_search_strategy for Hospitalizations of nursing home residents at the end of life: A systematic review by Katharina Allers, Falk Hoffmann and Rieke Schnakenberg in Palliative Medicine
Supplemental Material
Supplemental material, Supplementary_Table_2 for Hospitalizations of nursing home residents at the end of life: A systematic review by Katharina Allers, Falk Hoffmann and Rieke Schnakenberg in Palliative Medicine
Footnotes
Author contributions: All authors were involved in the development of study concept. K.A. performed the literature search. K.A., F.H., and R.S. participated in the selection of literature, in the data extraction, in the quality assessment, in the analysis of the literature, and wrote the manuscript. All authors reviewed earlier versions of the manuscript and read and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Katharina Allers  https://orcid.org/0000-0003-3458-8124
https://orcid.org/0000-0003-3458-8124
Supplemental material: Supplemental material for this article is available online.
References
- 1. Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010; 340: c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wallace CL, Adorno G, Stewart DB. End-of-life care in nursing homes: a qualitative interpretive meta-synthesis. J Palliat Med 2018; 21(4): 503–512. [DOI] [PubMed] [Google Scholar]
- 3. Ng CWL, Cheong S, Govinda Raj A, et al. End-of-life care preferences of nursing home residents: results of a cross-sectional study. Palliat Med 2016; 30(9): 843–853. [DOI] [PubMed] [Google Scholar]
- 4. Meeussen K, Van den Block L, Bossuyt N, et al. GPs’ awareness of patients’ preference for place of death. Br J Gen Pract 2009; 59(566): 665–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gomes B, Higginson IJ, Calanzani N, et al. Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol 2012; 23(8): 2006–2015. [DOI] [PubMed] [Google Scholar]
- 6. Cohen AB, Knobf MT, Fried TR. Do-not-hospitalize orders in nursing homes: “call the family instead of calling the ambulance.” J Am Geriatr Soc 2017; 65(7): 1573–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Reyniers T, Houttekier D, Cohen J, et al. What justifies a hospital admission at the end of life? A focus group study on perspectives of family physicians and nurses. Palliat Med 2014; 28(7): 941–948. [DOI] [PubMed] [Google Scholar]
- 8. Gott M, Seymour J, Bellamy G, et al. Older people’s views about home as a place of care at the end of life. Palliat Med 2004; 18(5): 460–467. [DOI] [PubMed] [Google Scholar]
- 9. Dwyer R, Gabbe B, Stoelwinder JU, et al. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age Ageing 2014; 43: 759–766. [DOI] [PubMed] [Google Scholar]
- 10. Wright AA, Keating NL, Balboni TA, et al. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. J Clin Oncol 2010; 28(29): 4457–4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pivodic L, Smets T, Van den Noortgate N, et al. Quality of dying and quality of end-of-life care of nursing home residents in six countries: an epidemiological study. Palliat Med 2018; 32(10): 1584–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ong ACL, Sabanathan K, Potter JF, et al. High mortality of older patients admitted to hospital from care homes and insight into potential interventions to reduce hospital admissions from care homes: the Norfolk experience. Arch Gerontol Geriatr 2011; 53(3): 316–319. [DOI] [PubMed] [Google Scholar]
- 13. Ahearn DJ, Jackson TB, McIlmoyle J, et al. Improving end of life care for nursing home residents: an analysis of hospital mortality and readmission rates. Postgrad Med J 2010; 86(1013): 131–135. [DOI] [PubMed] [Google Scholar]
- 14. Krishnan P, Williams H, Maharaj I. Patterns of end-of-life care: place of death and terminal hospitalization among long-term-care residents. J Hosp Palliat Nurs 2015; 17(2): 133–142. [Google Scholar]
- 15. Cardona-Morrell M, Kim JCH, Brabrand M, et al. What is inappropriate hospital use for elderly people near the end of life? a systematic review. Eur J Intern Med 2017; 42: 39–50. [DOI] [PubMed] [Google Scholar]
- 16. Cohen J, Bilsen J, Addington-Hall J, et al. Population-based study of dying in hospital in six European countries. Palliat Med 2008; 22(6): 702–710. [DOI] [PubMed] [Google Scholar]
- 17. Finucane AM, Stevenson B, Murray SA. Gradual physical decline characterises the illness trajectories of care home residents. Int J Palliat Nurs 2017; 23(9): 457–461. [DOI] [PubMed] [Google Scholar]
- 18. Mukamel DB, Ladd H, Caprio T, et al. Prototype end-of-life quality measures based on MDS 3 data. Med Care 2016; 54(11): 1024–1032. [DOI] [PubMed] [Google Scholar]
- 19. Levy C, Morris M, Kramer A. Improving end-of-life outcomes in nursing homes by targeting residents at high risk of mortality for palliative care: program description and evaluation. J Palliat Med 2008; 11(2): 217–225. [DOI] [PubMed] [Google Scholar]
- 20. Temkin-Greener H, Zheng NT, Xing J, et al. Site of death among nursing home residents in the United States: changing patterns, 2003–2007. J Am Med Dir Assoc 2013; 14(10): 741–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mor V, Papandonatos G, Miller SC. End-of-life hospitalization for African American and non-Latino white nursing home residents: variation by race and a facility’s racial composition. J Palliat Med 2005; 8(1): 58–68. [DOI] [PubMed] [Google Scholar]
- 22. Travis SS, Loving G, McClanahan L, et al. Hospitalization patterns and palliation in the last year of life among residents in long-term care. Gerontologist 2001; 41(2): 153–160. [DOI] [PubMed] [Google Scholar]
- 23. Miller SC, Lima JC, Intrator O, et al. Palliative care consultations in nursing homes and reductions in acute care use and potentially burdensome end-of-life transitions. J Am Geriatr Soc 2016; 64(11): 2280–2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Menec VH, Nowicki S, Blandford A, et al. Hospitalizations at the end of life among long-term care residents. J Gerontol A Biol Sci Med Sci 2009; 64(3): 395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Allers K, Hoffmann F. Mortality and hospitalization at the end of life in newly admitted nursing home residents with and without dementia. Soc Psychiatry Psychiatr Epidemiol 2018; 53(8): 833–839. [DOI] [PubMed] [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62(10): 1006–1012. [DOI] [PubMed] [Google Scholar]
- 27. Hoffmann F, Allers K. Age and sex differences in hospitalisation of nursing home residents: a systematic review. BMJ Open 2016; 6(10): e011912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Munn Z, Moola S, Lisy K, et al. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 2015; 13(3): 147–153. [DOI] [PubMed] [Google Scholar]
- 29. Munn Z, Moola S, Riitano D, et al. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Heal Policy Manag 2014; 3(3): 123–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cai S, Miller SC, Mukamel DB. Racial differences in hospitalizations of dying Medicare-Medicaid dually eligible nursing home residents. J Am Geriatr Soc 2016; 64(9): 1798–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cai S, Miller SC, Gozalo PL. Nursing home–hospice collaboration and end-of-life hospitalizations among dying nursing home residents. J Am Med Dir Assoc 2018; 19(5): 439–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gozalo PL, Miller SC. Hospice enrollment and evaluation of its causal effect on hospitalization of dying nursing home patients. Health Serv Res 2007; 42(2): 587–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Intrator O, Hiris J, Berg K, et al. The residential history file: studying nursing home residents’ long-term care histories(*). Health Serv Res 2011; 46(1 Pt. 1): 120–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kelly A, Conell-Price J, Covinsky K, et al. Length of stay for older adults residing in nursing homes at the end of life. J Am Geriatr Soc 2010; 58(9): 1701–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Levy C, Hutt E, Pointer L. Site of death among veterans living in veterans affairs nursing homes. J Am Med Dir Assoc 2012; 13(3): 199–201. [DOI] [PubMed] [Google Scholar]
- 36. Li Q, Zheng NT, Temkin-Greener H. Quality of end-of-life care of long-term nursing home residents with and without dementia. J Am Geriatr Soc 2013; 61(7): 1066–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Miller SC, Lima JC, Thompson SA. End-of-life care in nursing homes with greater versus less palliative care knowledge and practice. J Palliat Med 2015; 18(6): 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Miller SC, Dahal R, Lima JC, et al. Palliative care consultations in nursing homes and end-of-life hospitalizations. J Pain Symptom Manage 2016; 52(6): 878–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mukamel DB, Caprio T, Ahn R, et al. End-of-life quality-of-care measures for nursing homes: place of death and hospice. J Palliat Med 2012; 15(4): 438–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sloane PD, Zimmerman S, Williams CS, et al. Dying with dementia in long-term care. Gerontologist 2008; 48(6): 741–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Temkin-Greener H, Zheng NT, Mukamel DB. Rural-urban differences in end-of-life nursing home care: facility and environmental factors. Gerontologist 2012; 52(3): 335–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Temkin-Greener H, Mukamel DB, Ladd H, et al. Impact of nursing home palliative care teams on end-of-life outcomes. Med Care 2018; 56(1): 11–18. [DOI] [PubMed] [Google Scholar]
- 43. Teno JM, Gozalo P, Mitchell SL, et al. Terminal hospitalizations of nursing home residents: does facility increasing the rate of do not resuscitate orders reduce them? J Pain Symptom Manage 2011; 41(6): 1040–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zheng NT, Mukamel DB, Caprio T, et al. Racial disparities in in-hospital death and hospice use among nursing home residents at the end of life. Med Care 2011; 49(11): 992–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zheng NT, Mukamel DB, Friedman B, et al. The effect of hospice on hospitalizations of nursing home residents. J Am Med Dir Assoc 2015; 16(2): 155–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hirano M, Ogiwara M, Sakamoto Y, et al. [End-of-life care in a special elderly nursing home characteristics of patients who died in nursing home facilities and current status of end-of-life decision-making]. Nihon Ronen Igakkai Zasshi 2011; 48(5): 509–515. [DOI] [PubMed] [Google Scholar]
- 47. Ikegami N, Ikezaki S. Nursing homes and end-of-life care in Japan. J Am Med Dir Assoc 2013; 14(10): 718–723. [DOI] [PubMed] [Google Scholar]
- 48. Nakanishi M, Niimura J, Endo K, et al. Regional supply of nursing home and hospital beds determine discharge destination of nursing home residents in Japan. J Am Med Dir Assoc 2016; 17(7): 672.e1–e5. [DOI] [PubMed] [Google Scholar]
- 49. Shinoda-Tagawa T, Ikegami N. Resident and facility characteristics associated with the site of death among Japanese nursing home residents. Age Ageing 2005; 34(5): 515–518. [DOI] [PubMed] [Google Scholar]
- 50. Takezako Y, Tamiya N, Kajii E. The nursing home versus the hospital as the place of dying for nursing home residents in Japan. Health Policy (New York) 2007; 81(2–3): 280–288. [DOI] [PubMed] [Google Scholar]
- 51. Krishnan P, Thompson G, McClement S. Predicting hospital transfers among nursing home residents in the last months of life. Int J Palliat Nurs 2017; 23(11): 535–542. [DOI] [PubMed] [Google Scholar]
- 52. McGregor MJ, Tate RB, Ronald LA, et al. Variation in site of death among nursing home residents in British Columbia, Canada. J Palliat Med 2007; 10(5): 1128–1136. [DOI] [PubMed] [Google Scholar]
- 53. Kinley J, Hockley J, Stone L, et al. The provision of care for residents dying in U.K. Age Ageing 2014; 43(3): 375–379. [DOI] [PubMed] [Google Scholar]
- 54. Chapman M, Johnston N, Lovell C, et al. Avoiding costly hospitalisation at end of life: findings from a specialist palliative care pilot in residential care for older adults. BMJ Support Palliat Care 2018; 8(1): 102–109. [DOI] [PubMed] [Google Scholar]
- 55. Horey DE, Street AF, Sands AF. Acceptability and feasibility of end-of-life care pathways in Australian residential aged care facilities. Med J Aust 2012; 197(2): 106–109. [DOI] [PubMed] [Google Scholar]
- 56. De Gendt C, Bilsen J, Stichele RV, et al. Advance care planning and dying in nursing homes in Flanders, Belgium: a nationwide survey. J Pain Symptom Manage 2013; 45(2): 223–234. [DOI] [PubMed] [Google Scholar]
- 57. Morin L, Johnell K, Aubry R. Variation in the place of death among nursing home residents in France. Age Ageing 2015; 44(3): 415–421. [DOI] [PubMed] [Google Scholar]
- 58. Morin L, Reynaud-Levy O, Soriano D, et al. Fin de vie en EHPAD : résultats d’une étude rétrospective nationale en France. Revue Geriatr 2014; 39: 145–157. [Google Scholar]
- 59. Hoffmann F, Allers K. Dying in hospital among nursing home residents with and without dementia in Germany. Arch Gerontol Geriatr 2019; 82: 293–298. [DOI] [PubMed] [Google Scholar]
- 60. Ramroth H, Specht-Leible N, Konig HH, et al. Hospitalizations during the last months of life of nursing home residents: a retrospective cohort study from Germany. BMC Health Serv Res 2006; 6(1): 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ramroth H, Specht-Leible N, König H, et al. Use of hospital based resources by individuals in residential care homes. Dtsch Arztebl Int 2006; 103(41): 2710–2713. [Google Scholar]
- 62. Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol 2017; 18(9): e543–e551. [DOI] [PubMed] [Google Scholar]
- 63. Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med 2014; 28(8): 1000–1025. [DOI] [PubMed] [Google Scholar]
- 64. Houttekier D, Vandervoort A, Van den Block L, et al. Hospitalizations of nursing home residents with dementia in the last month of life: results from a nationwide survey. Palliat Med 2014; 28(9): 1110–1117. [DOI] [PubMed] [Google Scholar]
- 65. Hendriks SA, Smalbrugge M, Deliens L, et al. End-of-life treatment decisions in nursing home residents dying with dementia in the Netherlands. Int J Geriatr Psychiatry 2017; 32: e43–e49. [DOI] [PubMed] [Google Scholar]
- 66. Houttekier D, Cohen J, Bilsen J, et al. Place of death of older persons with dementia. A study in five European countries. J Am Geriatr Soc 2010; 58(4): 751–756. [DOI] [PubMed] [Google Scholar]
- 67. Levy CR, Fish R, Kramer AM. Site of death in the hospital versus nursing home of Medicare skilled nursing facility residents admitted under Medicare’s Part A Benefit. J Am Geriatr Soc 2004; 52(8): 1247–1254. [DOI] [PubMed] [Google Scholar]
- 68. Dwyer R, Stoelwinder J, Gabbe B, et al. Unplanned transfer to emergency departments for frail elderly residents of aged care facilities: a review of patient and organizational factors. J Am Med Dir Assoc 2015; 16(7): 551–562. [DOI] [PubMed] [Google Scholar]
- 69. Daras LC, Wang JM, Ingber MJ, et al. What are nursing facilities doing to reduce potentially avoidable hospitalizations. J Am Med Dir Assoc 2017; 18(5): 442–444. [DOI] [PubMed] [Google Scholar]
- 70. Ingber MJ, Feng Z, Khatutsky G, et al. Initiative to reduce avoidable hospitalizations among nursing facility residents shows promising results. Health Aff (Millwood) 2017; 36(3): 441–450. [DOI] [PubMed] [Google Scholar]
- 71. Rantz MJ, Popejoy L, Vogelsmeier A, et al. Successfully reducing hospitalizations of nursing home residents: results of the Missouri quality initiative. J Am Med Dir Assoc 2017; 18(11): 960–966. [DOI] [PubMed] [Google Scholar]
- 72. Konetzka RT, Spector W, Limcangco MR. Reducing hospitalizations from long-term care settings. Med Care Res Rev 2008; 65(1): 40–66. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_file_1_search_strategy for Hospitalizations of nursing home residents at the end of life: A systematic review by Katharina Allers, Falk Hoffmann and Rieke Schnakenberg in Palliative Medicine
Supplemental material, Supplementary_Table_2 for Hospitalizations of nursing home residents at the end of life: A systematic review by Katharina Allers, Falk Hoffmann and Rieke Schnakenberg in Palliative Medicine