Abstract
Background
Although variation in physiologic pelvic tilt may affect acetabular version and coverage, postural change in pelvic tilt in patients with hip dysplasia who are candidates for hip preservation surgery has not been well characterized, and its clinical importance is unknown.
Questions/purposes
The aim of this study was to determine (1) postural changes in sagittal pelvic tilt between the supine and standing positions; (2) postural changes in the acetabular orientation and coverage of the femoral head between the supine and standing positions; and (3) patient demographic and morphologic factors associated with sagittal pelvic tilt.
Methods
Between 2009 and 2016, 102 patients underwent pelvic osteotomy to treat hip dysplasia. All patients had supine and standing AP pelvic radiographs and pelvic CT images taken during their preoperative examination. Ninety-five patients with hip dysplasia (lateral center-edge angle < 20°) younger than 60 years old were included. Patients with advanced osteoarthritis, other hip disease, prior hip or spine surgery, femoral head deformity, or inadequate imaging were excluded. Sixty-five patients (64%) were eligible for participation in this retrospective study. Two board-certified orthopaedic surgeons (TT and MF) investigated sagittal pelvic tilt, spinopelvic parameters, and acetabular version and coverage using pelvic radiographs and CT images. Intra- and interobserver reliabilities, evaluated using the intraclass correlation coefficient (0.90 to 0.98, 0.93 to 0.99, and 0.87 to 0.96, respectively), were excellent. Demographic data (age, gender, and BMI) were collected by medical record review. Sagittal pelvic tilt was quantified as the angle formed by the anterior pelvic plane and a z-axis (anterior pelvic plane angle). Using a 2D-3D matching technique, we measured the change in sagittal pelvic tilt, acetabular version, and three-dimensional coverage between the supine and standing positions. We correlated sagittal pelvic tilt with demographic and CT measurement parameters using Pearson’s or Spearman’s correlation coefficients.
Results
Although functional pelvic tilt varied widely among individuals, the pelvis of patients with hip dysplasia tilted posteriorly from the supine to the standing position (mean APP angle 8° ± 6° versus 2° ± 7°; mean difference -6°; 95% CI, -7° to -5°; range -17° to 4.1°; p < 0.001; paired t-test).The pelvis tilted more than 5° posteriorly from the supine to the standing position in 39 patients (60%), and the change was greater than 10° in 12 (18%). In the latter subgroup of patients, the mean acetabular anteversion angle increased (22° ± 5° versus 27° ±5°; mean difference 5°; 95% CI, 4°-6°; p < 0.001) and the mean anterosuperior acetabular sector angle notably deceased from the supine to the standing position (91° ± 11° versus 77° ± 14°; mean difference -14°; 95% CI, -17° to -11°; p < 0.001; paired t-test). Postural change in pelvic tilt was not associated with any of the studied demographic or morphologic parameters, including patient age, gender, BMI, and acetabular version and coverage.
Conclusions
On average, the pelvis tilted posteriorly from the supine to the standing position in patients with hip dysplasia, resulting in increased acetabular version and decreased anterosuperior acetabular coverage in the standing position. Thus, assessment with a supine AP pelvic radiograph may overlook changes in acetabular version and coverage in weightbearing positions. We recommend assessing postural change in sagittal pelvic tilt when diagnosing hip dysplasia and planning hip preservation surgery. Further studies are needed to determine how postural changes in sagittal pelvic tilt affect the biomechanical environment of the hip and the clinical results of acetabular reorientation osteotomy.
Level of Evidence
Level IV, diagnostic study.
Introduction
Hip dysplasia is a common and can predispose patients to having osteoarthritis [14]. It is characterized by reduced acetabular coverage of the femoral head, shallow acetabular concavity, and joint instability [10, 29]. These deformities lead to abnormal distribution of stress on the articular cartilage, elevated joint contact pressure, and shearing stress on the anterosuperior acetabular rim complex, resulting in early hip joint degeneration [9, 16]. Reorientation osteotomies have been developed to manage such deformities to delay or prevent the development of osteoarthritis [13, 30]. The result of these osteotomies may be affected by various factors including insufficient correction, which could lead to an unfavorable patient outcome [15, 36]. Previous studies revealed substantial individual variety in acetabular version, deficiency type, and degree of acetabular dysplasia [10, 29]. Therefore, a three-dimensional (3-D) evaluation of acetabular deformities is helpful for customizing the correction procedure according to variation in the quantity and location of acetabular deficiencies [41].
Previous studies performed 3-D evaluations of the morphology of the hip using CT, with reference to standardized pelvic positions such as the anterior pelvic plane (APP) coordinate system to minimize measurement error [10, 20, 29]. However, given the individual and postural variation in physiologic pelvic tilt and its effect on acetabular orientation [17, 19, 33, 40], the reference position of the pelvis for morphologic analysis remains controversial. Additionally, for radiographic assessment, neutral pelvic positioning while planning periacetabular osteotomy has been recommended to avoid misinterpreting acetabular deformities [18, 34, 38].
Standardizing the pelvic position may be advantageous for anatomic and epidemiologic studies. However, recent studies suggested that radiographs taken in the supine position may not show the functional position of the acetabulum in relation to the femur, and a weightbearing radiograph may be more appropriate for assessing hip deformities [17, 33, 40]. An abnormal mechanical environment in dysplastic hips, such as shearing stress forces and overload on the anterosuperior acetabulum, becomes a problem when the patient’s hip is in a weightbearing position rather than in the supine position. Therefore, we assume that characterizing the postural change in pelvic tilt and acetabular orientation may yield valuable functional information and help surgeons to diagnose hip conditions and plan for hip preservation surgery by improving acetabular reorientation and the biomechanical environment of the hip joint. Currently, little is known about postural change in pelvic tilt and its effect on acetabular orientation and 3-D coverage of the femoral head in patients with hip dysplasia who are candidates for hip preservation surgery.
The aim of this study was to determine (1) postural changes in sagittal pelvic tilt between the supine and standing positions; (2) postural changes in the acetabular orientation and coverage of the femoral head between the supine and standing positions; and (3) patient demographic and morphologic factors associated with sagittal pelvic tilt.
Patients and Methods
Patients
Our institutional review board approved this retrospective study. Between February 2009 and February 2016, 102 patients underwent pelvic osteotomy to treat hip dysplasia. During the study period, all patients had supine and standing AP pelvic radiographs and pelvic CT images taken during their preoperative examination. Two board-certified orthopaedic surgeons (TT and MF) retrospectively reviewed all pelvic radiographs and CT images. One of the observers (MF) was involved in the patients’ care.
The inclusion criteria for this study were the presence of hip dysplasia, defined as a lateral center-edge angle [47] of less than 20° on AP pelvic radiographs, and age younger than 60 years (Fig. 1). Ninety-five patients met the inclusion criteria. The exclusion criteria were advanced osteoarthritis with a Tönnis grade of 2 or greater [39] in either hip, other hip disease, prior hip surgery of either hip, history of treatment of spinal disease, prior spinal surgery, morphologic abnormalities of the femoral head, or inadequate imaging. Eight patients who had hips with advanced osteoarthritis and 12 patients with prior hip or spinal surgery were excluded from this study. Three patients with a Legg-Calvé-Perthes disease-like deformity of the femoral head were also excluded. Seven patients were excluded because of poor-quality imaging.
Fig. 1.
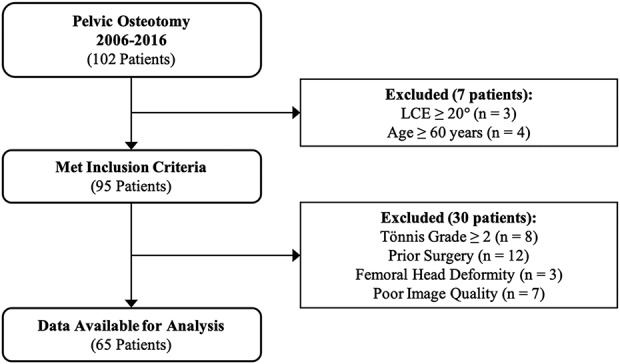
A STROBE flow diagram of this study is shown. LCE = lateral center-edge angle.
According to the criteria, 65 of the 102 potential patients (64%) were eligible for participation in this study (Table 1). There were four men and 61 women, with a median age of 45 years (range 17 to 58 years). A morphologic evaluation was performed on the operated-on side (symptom-dominant side). There were 37 right hips and 28 left hips. Seventeen patients had unilateral hip dysplasia, 48 had bilateral hip dysplasia, and 20 had bilateral hip pain. The dysplasia of all hips was classified as Type I according to the classification system of Crowe et al. [5]. Medical records were retrospectively reviewed to collect demographic data including age, gender, and BMI (kg/m2) at the time of examination.
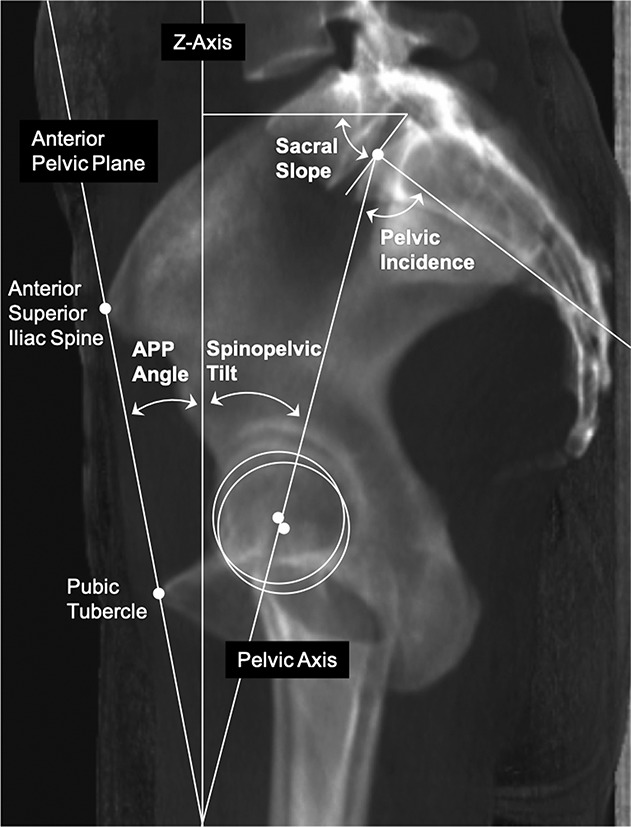
Table 1.
Patient demographic and radiographic data
CT Evaluations
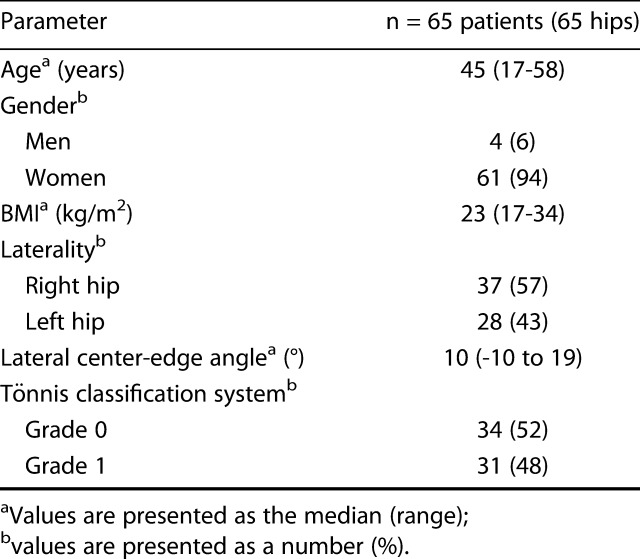
Pelvic CT was performed with the patients in the supine position, and images were obtained from the superior rim to the distal femur at 1.0-mm intervals. After downloading data from these scans in Digital Imaging and Communications in Medicine format, we (TT and MF) performed the following measurements on the digitally reconstructed radiographs and multiplanar reconstruction images using image-processing software (3-D template; Kyocera Medical Corporation, Osaka, Japan). The x- and y-axes corresponded to the transverse and sagittal axes on the axial CT slice, and the z-axis corresponded to the longitudinal scanner axis. First, the pelvic position was standardized with reference to the APP coordinate system, defined by the bilateral anterosuperior iliac spines and the midpoint between the pelvic tubercles [25]. After matching the coordinate system of the APP with that of CT scanner, we re-created sagittal pelvic tilt on the pelvic radiographs in both the supine and standing positions on the coronal digitally reconstructed radiographs by matching the vertical-to-horizontal ratio of the pelvic foramen (Fig. 2) [31, 37]. The following three pelvic positions were measured: the standardized position with reference to the APP, the supine position, and the standing position.
Fig. 2.
(A) Our methods of matching sagittal pelvic tilt using radiographs and CT images are shown. On an AP pelvic radiograph, the vertical diameter of the pelvic foramen between the bilateral sacroiliac joint and pubic symphysis (V), divided by the maximum horizontal diameter of the pelvic foramen (H), was calculated. (B) On a digitally reconstructed radiograph generated from CT images, the pelvis was rotated sagittally until the ratio of the foramen (V/H) was consistent with that on the AP pelvic radiograph.
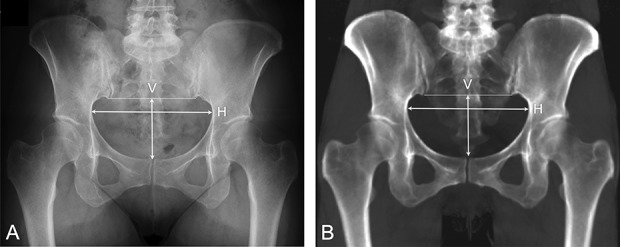
Sagittal pelvic tilt in the supine and standing positions was quantified as the angle formed by the APP and the z-axis on the sagittal digitally reconstructed radiographs (APP angle) (Fig. 3) [7]. A positive APP angle indicated anterior tilting of the pelvis and a negative angle indicated posterior tilting of the pelvis. The postural change in pelvic tilt between the supine and standing positions was calculated by subtracting the APP angle in the supine position from that in the standing position. A negative value indicated posterior change in pelvic tilt between the supine and standing positions.
Fig. 3.
Our methods of measuring sagittal pelvic tilt and spinopelvic parameters are shown. Sagittal pelvic tilt in the supine and standing positions was quantified as the angle formed by the APP and the z-axis (APP angle). The spinopelvic tilt was the angle formed by a line connecting the midpoint of the sacral plate and the midpoint of the centers of the femoral heads (pelvic axis) and the z-axis. The sacral slope was the angle formed by the cranial sacral endplate tangent and the y-axis. Pelvic incidence was quantified as the angle formed by a line perpendicular to the superior plate of the first sacral vertebra at its midpoint and the pelvic axis.
The following spinopelvic parameters were measured (Fig. 3) [22]. The spinopelvic tilt was the angle formed by a line connecting the midpoint of the sacral plate and the midpoint of the centers of the femoral heads (pelvic axis) and the z-axis. The sacral slope was the angle formed by the cranial sacral endplate tangent and the y-axis. Pelvic incidence was quantified as the angle formed by a line perpendicular to the superior plate of the first sacral vertebra at its midpoint and the pelvic axis.
The lateral center-edge angle, Tönnis angle [39], and acetabular wall index [35] were measured on the coronal digitally reconstructed radiographs. The acetabular anteversion and inclination angles were quantified at the transverse section through the femoral head’s center and at the coronal section through the femoral head’s center, respectively [10] (Fig. 4). The cranial acetabular version angle was quantified at the transverse section 5-mm distal to the acetabular roof, and we defined a hip with a negative angle as having acetabular retroversion [18]. The acetabular sector angle was measured as an indicator of radial acetabular coverage of the femoral head in five directions: anterior, anterosuperior, superior, posterosuperior, and posterior (Fig. 5) [2, 11]. The anterior and posterior acetabular sector angles were used to classify hips into four deficiency types: anterior deficiency (anterior acetabular sector angle < 50°, posterior acetabular sector angle ≥ 90°), global deficiency (anterior acetabular sector angle < 50°, posterior acetabular sector angle < 90°), mild deficiency (anterior acetabular sector angle ≥ 50°, posterior acetabular sector angle ≥ 90°), and posterior deficiency (anterior acetabular sector angle ≥ 50°, posterior acetabular sector angle < 90°) [4].
Fig. 4.
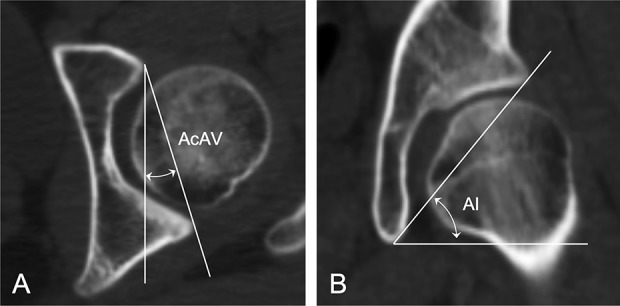
(A) The acetabular anteversion angle was quantified as the angle formed by a line connecting the anterior and posterior edges of the acetabulum and the y-axis at the transverse section through the femoral head’s center. (B) The acetabular inclination angle was quantified as the angle formed by a line connecting the superior and inferior edges of the acetabulum and the x-axis at the coronal section through the femoral head’s center. AcAV = acetabular anteversion angle; AI = acetabular inclination.
Fig. 5.
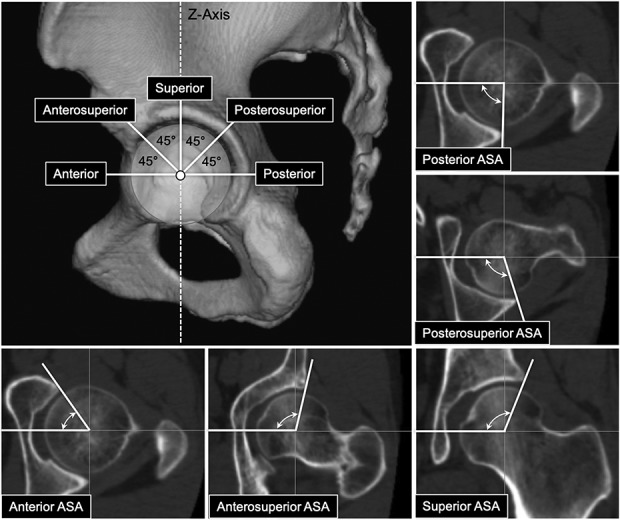
This figure shows our methods of measuring the acetabular sector angle in five radial directions. The acetabular sector angle was defined as an angle formed by a line connecting the acetabular edge and femoral head’s center and the x-axis passing through the femoral head’s center. Anterior and posterior acetabular sector angles were measured in the axial plane passing the femoral head’s center. Acetabular sector angles were also measured at 45° in the anterosuperior direction and in the superior direction, and at 45° in the posterosuperior direction. ASA = acetabular sector angle.
Using the data described above, we determined changes in sagittal pelvic tilt and spinopelvic parameter values between the supine and standing positions, changes in the acetabular version and coverage between the supine and standing positions, and the correlation between the APP angle and postural change and between patient demographic factors (age, gender, BMI, bilaterality, and Tönnis grade) and CT measurement values (spinopelvic parameters, acetabular anteversion angle, acetabular inclination angle, and acetabular sector angle) measured with reference to the APP coordinate system.
Statistical Analysis
Two board-certified orthopaedic surgeons (TT and MF) took all measurements. To test intraobserver reliability, we repeated the measurements in a blind test on 20 randomly selected hips more than 2 weeks later. A simple sampling technique through computer-generated random numbering was used to select the hips. Intraobserver reliabilities, evaluated using an intraclass coefficient, were excellent for both observers (range, 0.90 to 0.98 and 0.93 to 0.99). To test measurement reproducibility, two independent observers (TT and MF) performed measurements on 20 randomly selected hips in a blind test. Interobserver reliabilities evaluated using the intraclass correlation coefficient were excellent (range 0.87 to 0.96).
Paired t-tests or Wilcoxon signed-rank tests were used to compare continuous parameters for the supine and standing positions, depending on their distribution and homoscedasticity (Shapiro-Wilk’s test and f-test). A chi-square test or Fisher’s exact test was used to compare categorical parameters for the supine and standing positions, as appropriate. A t-test or Wilcoxon’s rank sum test was used to compare the APP angles between two groups (men versus women, unilateral versus bilateral dysplasia, and Tönnis Grade 0 versus Grade 1), as appropriate. The significance level was set at p < 0.05 for all tests. Correlations of the APP angles with continuous parameters (age, BMI, and CT measurement parameters) were calculated using Pearson’s correlation coefficients or Spearman’s rank correlation coefficients, as appropriate. We characterized the correlation coefficient values as negligible (range 0.0 to 0.3), weak (range 0.3 to 0.5), moderate (range 0.5 to 0.7), good (range 0.7 to 0.9), or excellent (range 0.9 to 1.0). Statistical analyses were performed using JMP® Version 13.0 (SAS Institute Inc., Cary, NC, USA).
Results
Postural Change in Sagittal Pelvic Tilt
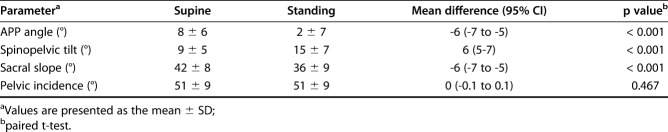
Although the APP angle in the supine and standing positions varied widely among individuals (Fig. 6), the pelvis of patients with hip dysplasia tilted posteriorly from the supine to the standing position (mean APP angle 8° ± 6° versus 2° ± 7°; mean difference -6°; 95% CI, -7° to -5°; p < 0.001) (Table 2). Larger APP angles in the supine position correlated with larger APP angles in the standing position (r = 0.784; p < 0.001). The change in the APP angle from the supine to the standing position ranged from -17° to 4°. Although the range of pelvic motion was less than 5° in 26 of the 65 patients in this study (40%), the APP angle changed by more than 5° posteriorly between the supine and standing positions in 39 patients (60%), and the posterior change was greater than 10° in 12 (18%) (Fig. 6). Spinopelvic tilt and sacral slope also changed between the supine and standing positions in a similar fashion as the APP angle, although the pelvic incidence was consistent (Table 2).
Fig. 6.
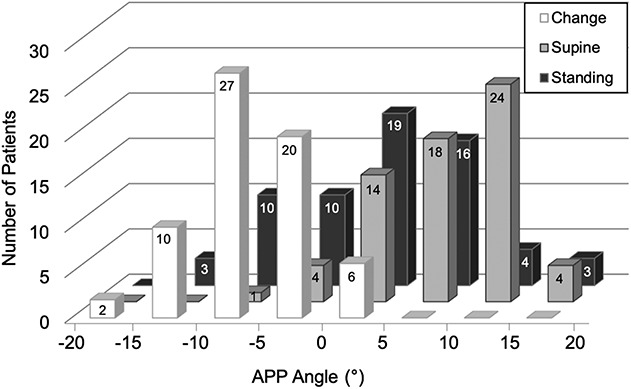
This figure shows the distributions of the APP angles in the supine and standing positions and postural change in the APP angle.
Table 2.
Comparisons of pelvic parameters between the supine and standing positions
Postural Change in Acetabular Version and Coverage
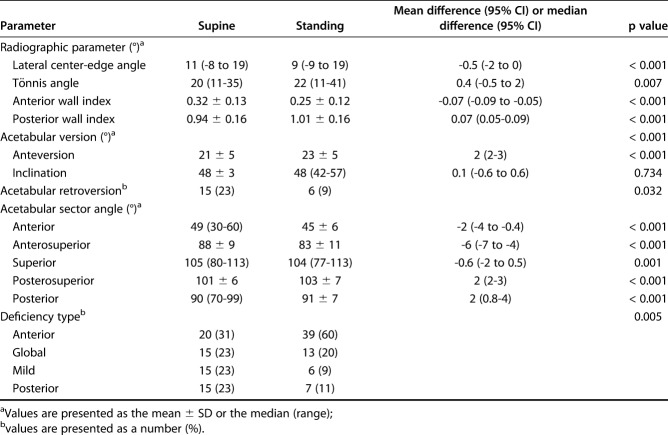
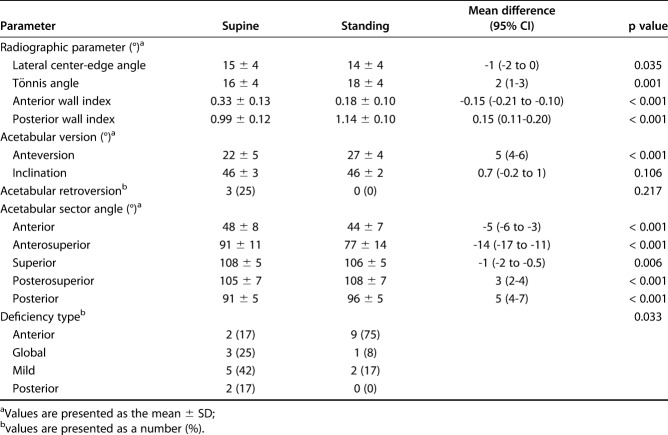
Posterior change in pelvic tilt correlated with an increase in the acetabular anteversion angle (r = -0.826; p < 0.001), a decrease in the anterior acetabular sector angle (r = 0.635; p < 0.001) and anterosuperior acetabular sector angle (r = 0.746; p < 0.001), and an increase in the posterosuperior acetabular sector angle (r = -0.357; p = 0.004) and posterior acetabular sector angle (r = -0.716; p < 0.001) (Table 3). The acetabular anteversion angle was greater in the standing position than that in the supine position (23° ± 5° versus 21° ± 5°; mean difference 2°; 95% CI, 2° to 3°; p < 0.001), but the acetabular inclination angle did not differ between the two positions (Table 4). The prevalence of acetabular retroversion decreased from 23% in the supine position to 9% in the standing position (odds ratio, 0.339; 95% CI, 0.122 to 0.939; p = 0.032). Regarding acetabular coverage, the anterior, anterosuperior, and superior acetabular sector angles decreased, while the posterosuperior and posterior acetabular sector angles increased from the supine to the standing position (Table 4). However, the overall magnitude of the observed differences was small, reflecting considerable variation in the range of pelvic motion among patients. The change in the acetabular sector angle was the largest in the anterosuperior direction (88° ± 9° in the supine position versus 83° ± 11° in the standing position; mean difference -6°; 95% CI, -7° to -4°; p < 0.001). The prevalence of anterior deficiency increased from 31% in the supine position to 60% in the standing position (p = 0.005). Regarding the radiographic parameters, the lateral center-edge angle and anterior wall index decreased, and the Tönnis angle and posterior wall index increased from the supine to the standing position (Table 4). These postural changes in acetabular version and coverage were noticeable in a subgroup of patients whose posterior change in the APP angle was greater than 10° (Table 5). In this subgroup of patients, the mean increase in the acetabular anteversion angle in the standing position was 5° (95% CI, 4° to 6°; p < 0.001). The change in the acetabular sector angle was the largest in the anterosuperior direction, with a mean value of -14° (95% CI, -17° to -11°; p < 0.001). The prevalence of anterior deficiency increased from 17% in the supine position to 75% in the standing position (p = 0.033).
Table 3.
Correlations between change in the APP angle and change in acetabular parameters
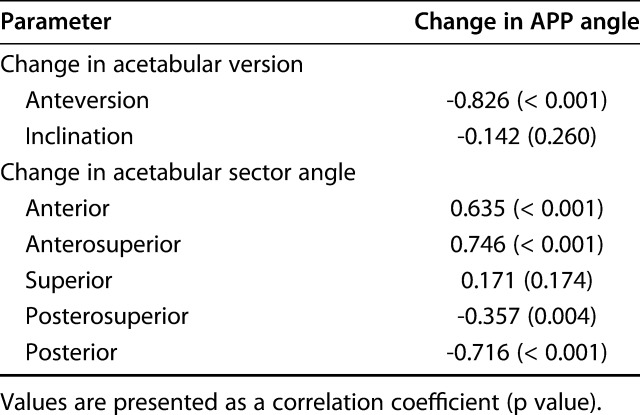
Table 4.
Comparisons of acetabular parameters between the supine and standing positions (n = 65 patients)
Table 5.
Comparisons of acetabular parameters between the supine and standing positions in patients whose posterior change in the APP angle was greater than 10° (n = 12 patients)
Factors Associated with Sagittal Pelvic Tilt
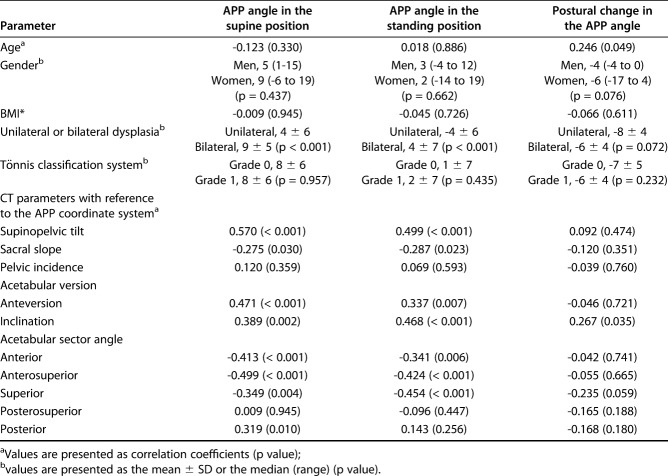
The APP angle of patients with bilateral hip dysplasia was greater than that of patients with unilateral hip dysplasia in both the supine (9° ± 5° versus 4° ± 6°; mean difference 5°; 95% CI, 2° to 8°; p < 0.001) and standing positions (4° ± 7° versus -4° ± 6°; mean difference 7°; 95% CI, 4° to 11°; p < 0.001) (Table 6). Among the pelvic parameters, spinopelvic tilt correlated positively with the APP angle in both the supine (r = 0.570; p < 0.001) and standing positions (r = 0.499; p < 0.001). The acetabular anteversion and inclination angles were positively correlated with the APP angle in both the supine and standing positions (Table 6). Regarding acetabular coverage, the anterior, anterosuperior, and superior acetabular sector angles were negatively correlated with the APP angle in both the supine and standing positions (Table 6). Postural change in the APP angle did not have a correlation with patient demographic data or CT measurement parameters (Table 6).
Table 6.
Correlation between APP angles and demographic and CT measurement parameters
Discussion
Background and Rationale
Substantial individual and postural variation in physiologic pelvic tilt may affect acetabular orientation [17, 19, 33, 40]. Considering the abnormal mechanical environment of dysplastic hips, assessment in the supine or standardized pelvic position may not show the functional orientation of the acetabulum to the femur, and a weightbearing position may be more appropriate for assessing hip deformities and planning acetabular reorientation [17, 33, 40]. To date, postural change in sagittal pelvic tilt in patients with hip dysplasia has not been well characterized, and its effect on acetabular version and coverage of the femoral head is unclear. In this study, we found that the pelvis of patients with hip dysplasia tilted posteriorly from the supine to the standing position by an average of 6°, and that the change was greater than 10° in 18% of patients. Posterior change in pelvic tilt from the supine to standing positions was associated with an increase in acetabular anteversion and a decrease in anterior-to-anterosuperior acetabular coverage of the femoral head.
Limitations
This study has several limitations. First, we did not evaluate spinal factors influencing sagittal pelvic tilt. Posterior pelvic tilt in the standing position has been reported to be associated with lumber degeneration, as found in degenerative disc diseases, degenerative spondylolisthesis, and vertebral compressive fractures in elderly patients with advanced osteoarthritis [37]. Although we excluded patients who were treated for spinal disease and those with prior spinal surgery to minimize the effect of spinal factors, a further investigation is needed to address the effect of spinal factors on our observations. Second, the study participants were symptomatic and underwent surgery, and 74% of them had bilateral hip dysplasia. Therefore, this group consisted of patients with more severe dysplasia. Our observation may apply only to people with severely dysplastic hips. Although a morphologic evaluation was performed on the operated-on side, similar results, including asymptomatic, mild dysplasia, were found in the contralateral hips. Thus, we assume that the study result applies to hip dysplasia of varying severity. Third, the study cohort was limited to Japanese patients, most of whom were women. Previous studies have demonstrated similarities between the spinopelvic parameters of white and Japanese patients, as well as between genders [21, 26], and we believe that our observations would remain unaffected by racial and gender differences. However, differences in hip morphology between races [48] and between genders [8] have been reported, and further research is warranted to address the impact of racial and gender differences on the generalizability of our observations. Lastly, exposure to radiation is a disadvantage of using a CT-based assessment. Further efforts are needed to minimize the dose of irradiation used or to develop assessment methods based on other modalities such as MRI.
Postural Change in Sagittal Pelvic Tilt
In this study, although the APP angle in both the supine and standing positions varied widely among individuals, the pelvis of patients with hip dysplasia tilted posteriorly from the supine position to the standing position. Similar to our observation, one small study [40] found that the pelvis tilted posteriorly from the supine to the weightbearing position in patients with hip dysplasia; however, the degree of the change in pelvic tilt was not directly measured. Another study [43] found that the pelvis tilted posteriorly from the supine (mean APP angle 6.2°) to the standing position (mean APP angle 0.5°) and that the mean change in the APP angle was -5.5° in 273 patients with advanced osteoarthritis secondary to hip dysplasia. These postural changes in pelvic tilt are not unique to hip dysplasia. Several studies have documented wide variation in pelvic tilt among participants and have shown that the pelvis tilts posteriorly by 4° to 5° from the supine to the standing position in normal people [6, 19, 24]. Others suggest that positioning has little or no effect on pelvic tilt [3, 27]. Anterior pelvic inclination was proposed as a feature of hip dysplasia in two studies [12, 32]. Okuda et al. [32] reported that patients with hip dysplasia tended to have a greater sacral slope angle than did healthy volunteers; however, the mean value (41.2°) was within the normal range [23, 26, 28, 45]. Although our study had no control participants, the mean values of spinopelvic parameters in the study cohort were within the reported normal range [23, 26, 28, 45]. In view of the substantial variation in physiologic pelvic tilt of normal people, that is, variation in the mean APP angle from -4° to 6.8° in the supine position and from -8° to 6.7° in the standing position in previous studies [6, 23, 24, 27, 46], we cannot conclude that patients with hip dysplasia have a distinctive pattern of pelvic tilt compared with normal people.
Postural Change in Acetabular Version and Coverage
Although a number of studies have explored the relationship between pelvic tilt and acetabular orientation [3, 17, 33, 34], few referred to patients with hip dysplasia and early-stage osteoarthritis who were candidates for hip preservation surgery. Our results showed that the posterior change in pelvic tilt correlated with an increase in the acetabular anteversion angle and a decrease in anterior and anterosuperior coverage. The latter was clearly evident in 12 patients (18%) in whom the posterior change in the APP angle was more than 10°. The prevalence of acetabular retroversion decreased from the supine (23%) to the standing position (9.2%). Similarly, Troelsen et al. [40] reported that the prevalence of acetabular retroversion decreased from 35% in the supine position to 13% in the standing position, and they warned of the risk of overestimating acetabular retroversion as seen on radiographs taken in the supine position. No studies that we know of have correlated postural change in pelvic tilt with 3-D coverage of the femoral head in dysplastic hips. The current study showed that the decrease in acetabular coverage from the supine to the standing position was the largest in the anterosuperior direction. A possible explanation for this phenomenon is that posterior tilt of the pelvis shifts the psoas valley from the anterior to the anterosuperior area, resulting in less anterosuperior coverage [44]. In dysplastic hips, shear stress forces and overload concentrate on the anterosuperior acetabulum, and the intraarticular pathology generally originates from the anterosuperior labrochondral junction [9, 16]. Therefore, decreased coverage of this area can exacerbate joint degeneration in hips with dysplasia [1].
In view of these postural changes in acetabular version and coverage, standardized pelvic radiographs taken in the supine position [34] may not show the patient-specific functional orientation of the acetabulum, and radiographs taken during weightbearing may be more appropriate when assessing abnormalities associated with hip dysplasia [17, 33, 40]. Although neutral pelvic positioning has been recommended for the preoperative planning of reorientation osteotomy to avoid misinterpreting acetabular deformities [18, 34, 38], evaluation in the supine or standardized pelvic position overlooks a possible decrease in anterosuperior acetabular coverage caused by individual and postural variation in physiologic pelvic tilt. A recent study indicated that acetabular coverage in the standing position correlated with coverage measured during gait [42]. Thus, we assume that a morphologic evaluation of a weightbearing position may yield valuable functional information and help surgeons to diagnose the hip’s condition and improve surgical reorientation and the biomechanical environment of the dysplastic hip. In patients with substantial posterior change in pelvic tilt in the standing position, anterior rotation of the acetabular fragment during osteotomy may be beneficial to correct the anterosuperior acetabular deficiency in the standing position [11].
Factors Associated with Sagittal Pelvic Tilt
Similar to previous reports in asymptomatic patients [26, 45], we observed no correlation between pelvic tilt and gender. Although we found no correlation between pelvic tilt and age, a large study [26] demonstrated that the pelvis tended to tilt slightly posteriorly with age in asymptomatic adults without spinal symptoms. Because our study cohort was small and we limited the study participants to patients under 60 years of age with hip dysplasia, we might have overlooked the association between pelvic tilt and age. Anterior rotation of the pelvis was associated with bilateral hip dysplasia, an increase in the acetabular anteversion and acetabular inclination angles, and a decrease in the anterior-to-superior acetabular sector angles, suggesting that anterior rotation of the pelvis compensated for acetabular deficiency in the anterior-to-superior acetabular region. These observations imply that patients with severe hip dysplasia tend to present with anterior rotation of the pelvis. Wassilew et al. [46] reported that the pelvis tilted more posteriorly in asymptomatic hips with acetabular retroversion than in those with anteversion. Consistent with our results, Zahn et al. [49] reported that anterior tilting of the pelvis positively correlated with the acetabular anteversion angle and inferred that pelvic tilt depends on acetabular orientation and compensates for an increased acetabular anteversion angle. Our results showed that postural change in pelvic tilt is unpredictable in terms of patient demographic and morphologic data. AP pelvic radiography while bearing weight is a convenient method to evaluate the individual patient’s range and direction of pelvic rotation and should be added to the routine assessment of hip dysplasia.
Conclusions
The results of this study showed that the pelvis tilts posteriorly from the supine to the standing position in patients with hip dysplasia. Postural change in sagittal pelvic tilt varied among individuals, and this postural change in pelvic tilt was capable of altering acetabular version and coverage of the femoral head. The change in pelvic tilt was more than 10° in 18% of patients, and these patients showed a marked increase in acetabular anteversion and a decrease in anterosuperior acetabular coverage of the femoral head in a weightbearing position. In such cases, anterior rotation of the acetabular fragment may be beneficial for correcting anterosuperior acetabular deficiency during reorientation osteotomy. We recommend assessing postural change in sagittal pelvic when diagnosing hip dysplasia and during the planning of hip preservation surgery. Further studies are needed to determine how postural changes in acetabular version and coverage affect the biomechanical environment of the hip and the clinical results of acetabular reorientation osteotomy.
Acknowledgments
We thank Toshihiko Hara MD (Department of Orthopaedic Surgery, Aso Iizuka Hospital, Iizuka Japan), Satoshi Hamai MD, PhD, Satoshi Ikemura MD, PhD, Goro Motomura MD, PhD, and Jun-ichi Fukushi MD, PhD (Department of Orthopaedic Surgery, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan) for their invaluable advice for this study.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has commercial associations that might pose a conflict of interest in connection with the submitted article. This work was supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (No. 18K09109).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedic Surgery, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan.
References
- 1.Akiho S, Yamamoto T, Kinoshita K, Matsunaga A, Ishii S, Ishimatsu T. The utility of false-profile radiographs for the detection of osteoarthritis progression in acetabular dysplasia. JB JS Open Access. 2017;2:e0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anda S, Svenningsen S, Dale L, Benum P. The acetabular sector angle of the adult hip determined by computed tomography. Acta Radiol Diagn. 1986;27:443-447. [DOI] [PubMed] [Google Scholar]
- 3.Anda S, Svenningsen S, Grontvedt T, Benum P. Pelvic inclination and spatial orientation of the acetabulum. A radiographic, computed tomographic and clinical investigation. Acta Radiol. 1990;31:389-394. [PubMed] [Google Scholar]
- 4.Anda S, Terjesen T, Kvistad KA, Svenningsen S. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr. 1991;15:115-120. [DOI] [PubMed] [Google Scholar]
- 5.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15-23. [PubMed] [Google Scholar]
- 6.Dardenne G, Dusseau S, Hamitouche C, Lefèvre C, Stindel E. Toward a dynamic approach of THA planning based on ultrasound. Clin Orthop Relat Res. 2009;467:901-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiGioia AM, Hafez MA, Jaramaz B, Levison TJ, Moody JE. Functional pelvic orientation measured from lateral standing and sitting radiographs. Clin Orthop Relat Res. 2006;453:272-276. [DOI] [PubMed] [Google Scholar]
- 8.Duncan ST, Bogunovic L, Baca G, Schoenecker PL, Clohisy JC. Are there sex-dependent differences in acetabular dysplasia characteristics? Clin Orthop Relat Res. 2015;473:1432-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fujii M, Nakashima Y, Noguchi Y, Yamamoto T, Motomura G, Hamai S, Iwamoto Y. Factors associated with severity of intra-articular lesions in patients with severe hip dysplasia. Arthroscopy. 2016;32:1581-1589. [DOI] [PubMed] [Google Scholar]
- 10.Fujii M, Nakashima Y, Sato T, Akiyama M, Iwamoto Y. Pelvic deformity influences acetabular version and coverage in hip dysplasia. Clin Orthop Relat Res. 2011;469:1735-1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujii M, Nakashima Y, Sato T, Akiyama M, Iwamoto Y. Acetabular tilt correlates with acetabular version and coverage in hip dysplasia. Clin Orthop Relat Res. 2012;470:2827-2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fukushima K. Relationship between spinal sagittal alignment and acetabular coverage: a patient-matched control study. Arch Orthop Trauma Surg. 2018;138:1495-1499. [DOI] [PubMed] [Google Scholar]
- 13.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26-36. [PubMed] [Google Scholar]
- 14.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20-33. [PubMed] [Google Scholar]
- 15.Hartig-Andreasen C, Troelsen A, Thillemann TM, Søballe K. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res. 2012;470:2978-2987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henak CR, Abraham CL, Anderson AE, Maas SA, Ellis BJ, Peters CL, Weiss JA. Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Osteoarthritis Cartilage. 2014;22:210-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henebry A, Gaskill T. The effect of pelvic tilt on radiographic markers of acetabular coverage. Am J Sports Med. 2013;41:2599-2603. [DOI] [PubMed] [Google Scholar]
- 18.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign.” J Orthop Res. 2007;25:758-765. [DOI] [PubMed] [Google Scholar]
- 19.Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph. A new computerized technique. J Bone Joint Surg Am. 1993;75:1318-1333. [DOI] [PubMed] [Google Scholar]
- 20.Larson CM, Moreau-Gaudry A, Kelly BT, Thomas Byrd JW, Tonetti J, Lavallee S, Chabanas L, Barrier G, Bedi A. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2014;473:1247-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Le Huec JC, Hasegawa K. Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur Spine J. 2016;25:3630-3637. [DOI] [PubMed] [Google Scholar]
- 22.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Legaye J. Influence of the sagittal balance of the spine on the anterior pelvic plane and on the acetabular orientation. Int Orthop. 2009;33:1695-1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517-523. [DOI] [PubMed] [Google Scholar]
- 25.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217-220. [PubMed] [Google Scholar]
- 26.Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J. 2011;20:572-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mayr E, Kessler O, Prassl A, Rachbauer F, Krismer M, Nogler M. The frontal pelvic plane provides a valid reference system for implantation of the acetabular cup: spatial orientation of the pelvis in different positions. Acta Orthop. 2005;76:848-853. [DOI] [PubMed] [Google Scholar]
- 28.Mehta VA, Amin A, Omeis I, Gokaslan ZL, Gottfried ON. Implications of spinopelvic alignment for the spine surgeon. Neurosurgery. 2012;70:707-721. [DOI] [PubMed] [Google Scholar]
- 29.Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214-223. [PubMed] [Google Scholar]
- 30.Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984;66:430-436. [PubMed] [Google Scholar]
- 31.Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop Relat Res. 2003;411:140-151. [DOI] [PubMed] [Google Scholar]
- 32.Okuda T, Fujita T, Kaneuji A, Miaki K, Yasuda Y, Matsumoto T. Stage-specific sagittal spinopelvic alignment changes in osteoarthritis of the hip secondary to developmental hip dysplasia. Spine (Phila Pa 1976). 2007;32:816-819. [DOI] [PubMed] [Google Scholar]
- 33.Pullen WM, Henebry A, Gaskill T. Variability of acetabular coverage between supine and weightbearing pelvic radiographs. Am J Sports Med. 2014;42:2643-2648. [DOI] [PubMed] [Google Scholar]
- 34.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241-248. [DOI] [PubMed] [Google Scholar]
- 35.Siebenrock KA, Kistler L, Schwab JM, Büchler L, Tannast M. The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res. 2012;470:3355-3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633-1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tamura S, Takao M, Sakai T, Nishii T, Sugano N. Spinal factors influencing change in pelvic sagittal inclination from supine position to standing position in patients before total hip arthroplasty. J Arthroplasty. 2014;29:2294-2297. [DOI] [PubMed] [Google Scholar]
- 38.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182-190. [DOI] [PubMed] [Google Scholar]
- 39.Tönnis D, Legal H. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer-Verlag; 1987:165-171. [Google Scholar]
- 40.Troelsen A, Jacobsen S, Rømer L, Søballe K. Weightbearing anteroposterior pelvic radiographs are recommended in DDH assessment. Clin Orthop Relat Res. 2008;466:813-819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Trousdale RT. Acetabular osteotomy: indications and results. Clin Orthop Relat Res. 2004;429:182-187. [PubMed] [Google Scholar]
- 42.Uemura K, Atkins PR, Maas SA, Peters CL, Anderson AE. Three-dimensional femoral head coverage in the standing position represents that measured in vivo during gait. Clin Anat. 2018;31:1177-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Uemura K, Takao M, Otake Y, Koyama K, Yokota F, Hamada H, Sakai T, Sato Y, Sugano N. Change in pelvic sagittal inclination from supine to standing position before hip arthroplasty. J Arthroplasty. 2017;32:2568-2573. [DOI] [PubMed] [Google Scholar]
- 44.Vandenbussche E, Saffarini M, Taillieu F, Mutschler C. The asymmetric profile of the acetabulum. Clin Orthop Relat Res. 2008;466:417-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87:260-267. [DOI] [PubMed] [Google Scholar]
- 46.Wassilew GI, Heller MO, Janz V, Perka C, Müller M, Renner L. High prevalence of acetabular retroversion in asymptomatic adults: a 3D CT-based study. Bone Joint J. 2017;99:1584-1589. [DOI] [PubMed] [Google Scholar]
- 47.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteo-arthritis. Acta Chir Scand. 1939:5-135. [Google Scholar]
- 48.Yoshimura N, Campbell L, Hashimoto T, Kinoshita H, Okayasu T, Wilman C, Coggon D, Croft P, Cooper C. Acetabular dysplasia and hip osteoarthritis in Britain and Japan. Br J Rheumatol . 1998;37:1193-1197. [DOI] [PubMed] [Google Scholar]
- 49.Zahn RK, Grotjohann S, Ramm H, Zachow S, Putzier M, Perka C, Tohtz S. Pelvic tilt compensates for increased acetabular anteversion. Int Orthop. 2016;40:1571-1575. [DOI] [PubMed] [Google Scholar]