Supplemental Digital Content is available in the text.
Summary:
The CAD/CAM technology for mandibular reconstruction has improved the results in terms of outcomes in restoring mandibular complex defects. Augmented reality (AR) represents an evolution of the navigation-assisted surgery. This technology merges the images of the virtual planning with the anatomy of the patient, representing in this way an enhanced scene for the surgeon’s eye. AR can also display in a single scene additional information for the surgeon. Despite of classical navigation, this scenario can be obtained with marker-less registration method, without using reference points or fiducial markers. This technologic evolution together with the large use in our experience of CAD/CAM protocol for mandibular reconstruction we developed this feasibility study to evaluate the possibility of using a marker-less image registration system. Moreover, we tried to evaluate the overlaying of the virtual planning and its reproducibility using AR. We performed a case series of 3 consecutive patients who underwent mandibular reconstruction using AR-assisted fibular free flap harvesting applying our digital workflow. Once launched, the mobile app installed on our tablet, the registration is performed according to a shape recognition system of the leg of the patient, rendering in real time a superimposition of the anatomy of the bony, vascular, and skin of the patient and also the surgical planning of the reconstruction. AR-assisted fibular free flap harvesting was performed. We believe that AR can be a prospective improving technology for mandibular complex reconstruction.
INTRODUCTION
In complex mandibular defects, to obtain with surgery as much a similar condition to the native situation as possible, more accurate preoperative planning is needed. CAD/CAM technology has been recently introduced giving the opportunity to virtually plan the surgical procedure and reproduce it intraoperatively by using resection and fibular osteotomy cutting guides and a laser sintered titanium personalized implant supporting the fibular free flap, helping surgeons to improve the results in terms of reconstruction accuracy and morphologic outcomes.1–4
Recently, augmented reality (AR) was introduced as an evolution of the navigation-assisted surgery in cranio–maxillofacial surgery. This technology merges the virtual and real images into one single scene. This allows the direct observation of the imaging, the surgical field, and additional information, and it also smoothly enhances the perception of the physical environment.5,6 All of this can be performed without the necessity of invasive preoperative placement of fixed fiducial markers and while performing real-time marker-less image registration.
According to this technologic evolution and to the CAD/CAM protocol for mandibular reconstruction consolidation in the clinical practice, the goal of our feasibility study was to use both methods to intraoperatively reproduce the virtual planning with a marker-less image registration system.
We performed AR-assisted fibular free flap harvesting in a case series of 3 consecutive patients which underwent mandibular reconstruction applying the following workflow.
STEP 1: VIRTUAL RECONSTRUCTIVE PLANNING
The donor-site CTA scan of the patient was performed administering nonionic contrast media intravenously (Xenetix 350 Guerbet), with a slice thickness of 0.6 mm (Lightspeed VCT LS Advantage 64 slices; General Electric Medical System). The DICOM files were processed with MIMICS software (Materialise, Leuven, Belgium) to obtain the 3-dimensional (3D) virtual model of the patient. The 3D model consisted of bony, vascular, and skin 3D rendering. This process is finalized using D2P software (3D Systems Inc., Rock Hill, SC) with the help of a dedicated engineer (See Video 1 [online], which displays 3D modeling of the donor site: virtual segmentation of vessels and bone and skin of the leg).
Video 1. This video displays three-dimensional modeling of the donor site: virtual segmentation of vessels, bone and skin of the leg.
The reconstructive planning is performed on the donor-site CTA scan according to the virtual planning of the mandibular resection, performed on the Head & Neck preoperative CT scan (Lightspeed VCT LS Advantage 64 slices; General Electric Medical System). The osteotomy guides for the bony free flap were designed based on the reconstruction planning using the software TRIMATIC (Materialise, Leuven, Belgium). The cutting guides obtained were additively printed in polyamide.
STEP 2: AR REGISTRATION
The STereo Lithography interface files of the fibular cutting guide obtained according to the virtual planning of the mandibular reconstruction and the STereo Lithography interface files of the lower leg segmented anatomy are imported into the Unity 3D software (Unity Technologies, San Francisco, Calif.), installed on our mobile devices (smartphone and tablet). Once launched, the registration is performed according to a shape recognition system of the leg of the patient. The shape key-points were the knee and the malleolar region, to avoid registration errors due to the posterior leg soft tissue displacing after the skin incision (Fig. 1). The application generated “holographic” overlays, correctly rendered the anatomy of the patient and showed a superimposition of the anatomy of the bony, vascular, and skin anatomy of the patient and also the surgical planning of the reconstruction (See Video 2 [online], which displays AR registration process: surgical anatomy and planning real-time superimposition).
Fig. 1.
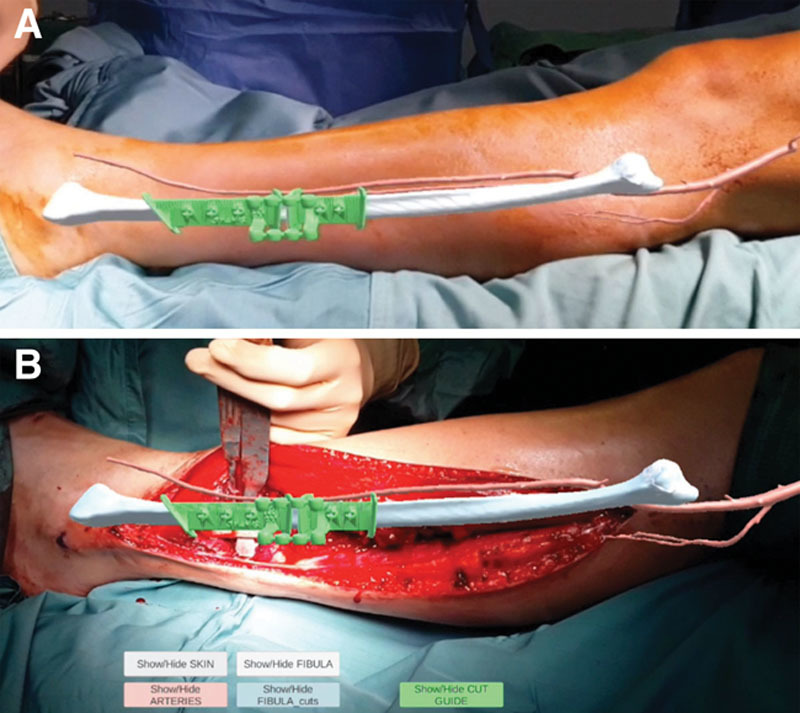
Overlay of the virtual anatomy and planning at skin (A) and bone (B) level.
Video 2. This video displays the AR registration process: surgical anatomy and planning real-time superimposition.
STEP 3: AR-ASSISTED FIBULAR FREE FLAP HARVESTING
After the registration, the fibular free flap harvesting starts comparing the fibular head and external malleolus with the virtual anatomy. The surgeon exposes the fibular bone, comparing the anatomical intraoperative findings with AR anatomy. When the bone exposure is completed, a new registration is performed. Hence, it is possible to verify the accuracy and also position the physical cutting guide according to the preoperative planning and before performing the osteotomy. (See Video 3 [online], which displays AR-assisted fibular free flap harvesting: positioning of the fibular osteotomy cutting guide.)
Video 3. This video displays the AR-assisted fibular free flap harvesting: positioning of the fibular osteotomy cutting guide.
STEP 4: FIBULAR SEGMENTATION
The fibular free flap harvesting is then completed by isolating the vascular pedicle. Then, the pedicle is detached and the segmentation can be completed by using the fibular cutting guide previously positioned. Fibular osteotomies are performed by using Piezosurgery (Mectron S.p.A., Carasco, Italy) to avoid vascular lesions of the pedicle. At this point, the insetting on the reconstructive customized plate is performed and the reconstruction is completed.
DISCUSSION
In this article, we tried to merge CAD/CAM and AR technologies to assess the possibility of using both in the intent of improving the outcomes and to possibly introduce soft tissue planning in the near future.
Very few articles in the actual literature report the possibility to either simulate or even visualize and localize 3D the vascular anatomy of the perforator vessels used for the skin paddle harvesting of the fibular composite microvascular free flap.7–9 The next step of our research will be importing on the AR software the skin paddle virtual shape and its perforator vessel, positioning the fibular cutting guide according to the perforator position. In the present article, the guide was planned and positioned taking into account the pedicle length needed to perform the vascular anastomoses.
Finally, AR for cranio–maxillofacial surgery has been developed to overcome the classical navigation limits, such as soft tissue reference marks and registration process. In our department, surgeons and biomedical engineers work together in a 3D planning laboratory. This is of course is of great help in terms of images importation time and 3D segmentation. However, nowadays the software used are more user friendly, and, after a brief learning curve, the surgeon can import the planned surgery on the AR software by himself.
The combination did not affected negatively the operative time that still benefit from the CAD/CAM method as a time-saving method in terms of fibular segmentation and insetting time and, consequently, total operating time.10
CONCLUSION
In conclusion, we believe that AR can be a prospective technology which will enable to continue the improvement of the accuracy of reproducibility of virtual planning for mandibular reconstruction in association with the well-solid CAD/CAM protocol.
Supplementary Material
Footnotes
Published online 22 November 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.van Baar GJC, Forouzanfar T, Liberton NPTJ, et al. Accuracy of computer-assisted surgery in mandibular reconstruction: a systematic review. Oral Oncol. 2018;84:52–60. [DOI] [PubMed] [Google Scholar]
- 2.van Baar GJC, Liberton NPTJ, Forouzanfar T, et al. Accuracy of computer-assisted surgery in mandibular reconstruction: a postoperative evaluation guideline. Oral Oncol. 2019;88:1–8. [DOI] [PubMed] [Google Scholar]
- 3.Tarsitano A, Battaglia S, Ricotta F, et al. Accuracy of CAD/CAM mandibular reconstruction: a three-dimensional, fully virtual outcome evaluation method. J Craniomaxillofac Surg. 2018;46:1121–1125. [DOI] [PubMed] [Google Scholar]
- 4.Tarsitano A, Ciocca L, Scotti R, et al. Morphological results of customized microvascular mandibular reconstruction: a comparative study. J Craniomaxillofac Surg. 2016;44:697–702. [DOI] [PubMed] [Google Scholar]
- 5.Badiali G, Ferrari V, Cutolo F, et al. Augmented reality as an aid in maxillofacial surgery: validation of a wearable system allowing maxillary repositioning. J Craniomaxillofac Surg. 2014;42:1970–1976. [DOI] [PubMed] [Google Scholar]
- 6.Cutolo F, Meola A, Carbone M, et al. A new head-mounted display-based augmented reality system in neurosurgical oncology: a study on phantom. Comput Assist Surg (Abingdon). 2017;22:39–53. [DOI] [PubMed] [Google Scholar]
- 7.Garvey PB, Chang EI, Selber JC, et al. A prospective study of preoperative computed tomographic angiographic mapping of free fibula osteocutaneous flaps for head and neck reconstruction. Plast Reconstr Surg. 2012;130:541e–549e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Battaglia S, Maiolo V, Savastio G, et al. Osteomyocutaneous fibular flap harvesting: computer-assisted planning of perforator vessels using computed tomographic angiography scan and cutting guide. J Craniomaxillofac Surg. 2017;45:1681–1686. [DOI] [PubMed] [Google Scholar]
- 9.Battaglia S, Ricotta F, Maiolo V, et al. Computer-assisted surgery for reconstruction of complex mandibular defects using osteomyocutaneous microvascular fibular free flaps: use of a skin paddle-outlining guide for soft-tissue reconstruction. A technical report. J Craniomaxillofac Surg. 2019;47:293–299. [DOI] [PubMed] [Google Scholar]
- 10.Tarsitano A, Battaglia S, Crimi S, et al. Is a computer-assisted design and computer-assisted manufacturing method for mandibular reconstruction economically viable? J Craniomaxillofac Surg. 2016;44:795–799. [DOI] [PubMed] [Google Scholar]


