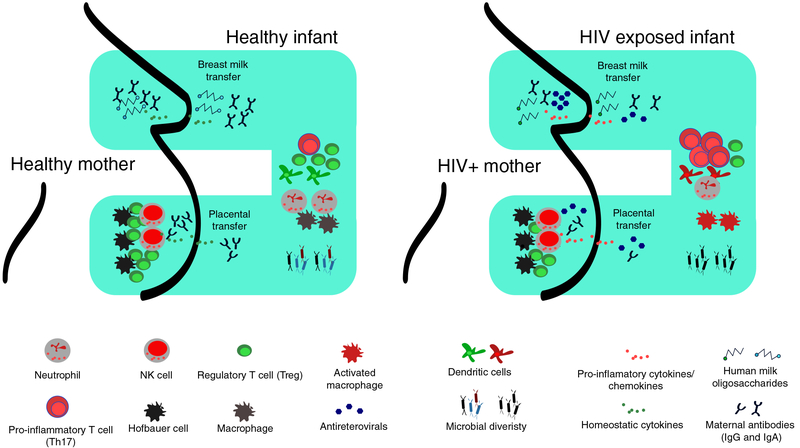
FIGURE 1. Schematic representation of the suggested model illustrating the link among in utero HIV exposure, breastfeeding, and microbiota on the developing immune system.
The left panel shows in a healthy pregnancy, the MF balance is maintained by Hofbauer cells, dNK, and Tregs in the placenta. Abs are efficiently transferred from mother to child via the placenta and breast milk provide protection against invading pathogens. Breastfeeding infants receive a plethora of bioactive compounds in breast milk including HMO that influences establishment of beneficial microbiota and promotes development of the infant’s immune system. In HIV-infected mothers, who may be invariably taking ARV drugs, chronic immune activation in the mother creates an inflammatory environment resulting in likely dysregulation of MF immune balance. Mother to child transfer of proinflammatory cytokines and chemokines occurs via placenta and/or breast milk activating innate cells in infants and promoting an expansion of inflammatory T cells (Th17 for example). Transplacental passage of maternal Abs is also impaired resulting in few protective antibodies in the infant circulation. Furthermore, less fucosylated and glycosylated HMOs are passed via maternal breast milk resulting in lower gut microbiota diversity.