Abstract
Cardiovascular (CV) risk factors like diabetes and hypertension are poorly controlled in both rural and urban India. This study was designed to identify the reasons for suboptimal control in a semiurban population in India. A total of 70 participants from the Study to Expand Heart Associated Treatments (SEHAT) trial, conducted in West Bengal, India. We qualitatively examined perspectives regarding CV risk factor control using focus group discussions based on the theory of reasoned action. Qualitative content analysis was used to analyze prevailing themes. Participants demonstrated a generalized knowledge of healthy lifestyle practices but lacked insight into disease-specific prevention methods. We further noticed significant gaps in the translation of existing knowledge into behavior. While personal and systemic barriers exist, factors like high patient motivation and a deep sense of trust in providers can potentially be harnessed to improve risk factor control in the community. We identified key facilitators and barriers to CV risk factor control in the community using a knowledge attitude behavior approach. Our findings provide direction for the development of community-based CV risk reduction models.
Keywords: Cardiovascular disease, facilitators and barriers, India, medication adherence
Introduction
As an Low- Middle Income country (LMIC), India is in a state of epidemiological transition from predominantly infectious diseases to noncommunicable diseases.[1] A total of 28% of all deaths in India in 2016 were attributable to cardiovascular disease (CVD).[2] Risk factor control is an important domain in CVD prevention, one that needs to be undertaken starting with the primary care physician at the Peripheral Health Center (PHC) level.[3,4] It is therefore concerning that the prevalence of hypertension has doubled and that of diabetes, tripled over the last 30 years in India.[5] A meta-analysis of hypertension control across India noted that 75% of rural hypertensive patients were not aware of their diagnosis. Only 38% of urban and 25% of rural hypertensive patients were being treated, with control being achieved in only 10--20% of this population.[6] Another South Indian study reported that 72% of patients with diabetes had suboptimal glycemic control with 46% not receiving any treatment and 15% being treated with alternative medicines.[7]
A healthy diet and lifestyle, disease awareness, medication adherence, and regular medical follow up are central to the management of CVD. Previously described barriers include a lack of knowledge about the disease and its consequences, prevalent social attitudes that deter the adoption of a healthy lifestyle, and a difficulty in giving up pleasurable behaviors. Similarly, a fear of medication side effects, multidrug therapy, and multiple dosing schedules is known to contribute to poor medication adherence.[8,9,10,11,12] Another well-recognized barrier is the lack of affordability and availability of healthcare in India, with the poorest often being most affected.[13] In the Indian scenario, the management of CV risk factors is further influenced by the use of complementary and alternative medicine as well as by the availability of multiple types of healthcare providers (medical school trained physicians, untrained healthcare practitioners (quacks) and doctors practicing alternative medicine). A South Indian study reported that 30% of their patients were concomitantly using both alternative and allopathic medications for diabetes, thereby being exposed to the risk of drug interactions.[14] For example, herbs, such as ginseng, garlic, and bitter melon are often used as adjuvants in patients with diabetes. These herbs have been shown to produce additive hypoglycemic effects in patients taking oral hypoglycemic agents or insulin.[15]
Studying knowledge, attitude, and behaviors (KAB) helps understand the community's CV health behavior to design intervention models.[16] A household survey across a general population in South India found that less than 50% of respondents recognized hypertension and 20% recognized diabetes as a risk factor for CVD.[17] Studies in other populations have identified similar themes, such as a poor knowledge of risk factors, symptoms, and complications of CVD.[18,19,20] However, there is a paucity of literature addressing the link between knowledge, attitudes, and behavior in Indian patients with hypertension and diabetes, and potential solutions to closing the gap between diagnosis and control. The current study was designed to overcome some of the limitations of prior studies by focusing on a KAB approach to identify facilitators and barriers to control in patients already diagnosed with hypertension and diabetes.
Subjects and Methods
Ethics
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Approval was obtained from Institutional Review Board (IRB) of the Society for Promotion of Ethical Clinical Trials (30th December 2015), New Delhi as well as the University Hospitals IRB, Case Western Reserve University, Cleveland, USA, Ref no 02-14-22, 2/2/2016. All participants provided written, informed consent prior to participating in the discussion.
Selection and description of participants
A total of 70 participants with hypertension and/or diabetes between 35 and 70 years of age were selected from both the intervention and control arms of Project SEHAT, a cluster randomized controlled trial designed to test the utilization of community health workers (CHWs) to manage hypertension, diabetes, and smoking in an integrated manner.[21] In the SEHAT cohort, 55% of participants with hypertension and 40% of participants with diabetes were unaware of their disease. While 36% of participants with hypertension and 58% of diabetics were on treatment, only 8% of participants with hypertension and 14% of diabetics achieved control of their disease.[22] The current study was conducted at the end of the first year of intervention at Dalkhola, West Bengal, India in 2016. Participants were stratified based on gender, medication adherence, and by whether they had seen a qualified physician for their hypertension or diabetes. Two separate groups of family members caring for patients were also interviewed.
Study design
This qualitative study consisted of 12 focus groups of five to eight participants each. To facilitate discussion, a semistructured guide based on the Theory of Reasoned Action was developed. This was formatted according to the procedures used by Friedman and Shepeard[23] and has been employed by other studies using the KAB approach.[17,24] The guide was modified based on discussions with eight CHWs. In keeping with standard focus group discussion (FGD) methodology,[25] a trained female interviewer of a similar socioeconomic background, with a college degree led the discussion in the local language, Bengali. A second person (D.B.) was in the room and took notes on nonverbal cues and important dynamics. All conversations were digitally audio recorded, transcribed into Bengali and then translated to English. At the conclusion of the discussions, subjects were given Rs. 100 (~US $2) as remuneration. All FGDs took place in a community hall at the center of town, accessible to all study participants. One to two FGDs were conducted every day for a week, to ensure participation by diverse members of the community.
Statistics
Using qualitative content analysis, two researchers (P.S. and A.K.) evaluated all of the transcripts independently to capture prevailing themes with examples.[26,27] A priori codes relevant to the study variables were developed, such as known facilitators and barriers to adherence. Responses were then categorized into existing codes where possible. Any text that could not be categorized with the initial coding scheme was given a new code. The data were then analyzed by counting the frequencies of individual codes.
Results
On average, participants were approximately 53 years old and 60% were female. Full demographic characteristics of the participants are described in Table 1.
Table 1.
Baseline demographic characteristics (n=70)
| Participant characteristics | n (%) or mean (SD) |
|---|---|
| Sex (male) | 29 (41.4) |
| Age (mean and SD) | 52.6 (11) |
| Education (years) | |
| None | 38 (54.3) |
| 1-5 | 14 (20) |
| 6-10 | 11 (15.7) |
| 11-15 | 6 (8.5) |
| 15-17 | 1 (1.4) |
| Community | |
| Bengali Hindu | 42 (60) |
| Bengali Muslim | 14 (20) |
| Marwari | 1 (1.4) |
| Others | 13 (18.5) |
| Marital status | |
| Married | 58 (82.9) |
| Nonmarried | 12 (17.1) |
| Income | |
| <25000 | 18 (25.7) |
| 26000-50000 | 13 (18.6) |
| >50000-1000001 | 13 (28.6) |
| >100000-200000 | 3 (4.2) |
| >200000 | 5 (7.1) |
| Did not disclose | 5 (8.9) |
Knowledge
Knowledge about symptoms and complications of hypertension and diabetes
Many participants were aware of the risk of kidney and eye damage, but not that of heart attacks and stroke. Nearly, half the patients in both intervention and control groups recognized that diabetes was associated with tingling or burning in their hands and feet. However, only one patient was aware that patients with such pain were at risk for developing foot ulcers from neuropathy. None of the participants recognized that hypertension and diabetes could be asymptomatic.
Recognizing the symptoms of heart attacks and stroke
While awareness of the symptoms of heart attacks and stroke was low in general, those who had suffered themselves or seen a family member suffer from these conditions were generally better informed. Only seven respondents knew that a heart attack presented with chest pain. Participants had some knowledge about the symptoms of a stroke, believing that it would present either with a fall or with paralysis. Very few participants recognized aphasia or facial droop as concerning symptoms. Other participants used nonspecific terms like “shiver in the chest,” “diffuse body pain,” or “feeling weak” to describe symptoms of both heart attacks and stroke, displaying a lack of knowledge of specific symptoms that should alert patients to these conditions. While most patients believed that heart attacks and stroke could be deadly, they often tried home remedies like pouring water on the patient's head or giving the patient oil massages before seeking modern medical help, which in itself sometimes consisted of visiting an informal (non-MBBS) medical provider.
Knowledge about CVD risk factors and prevention
A total of 77% of respondents felt that unhealthy eating habits were responsible for the increasing incidence of CVD. Other commonly identified risk factors were a sedentary lifestyle and psychological stressors. Hypertension, diabetes, substance use, and medication nonadherence were only recognized by 12--15% of respondents as important risk factors. We also identified many common myths such as avoiding food grown underground, avoiding fish, etc., Another recurrent theme was the emphasis on avoiding mental stress or “tension” in an attempt to reduce the risk of CVD. This middle aged hypertensive patient stated, “Those who have a chance of getting heart attacks, they should not worry or think they might go through it too. They should be brave.”
Attitude
Attitude toward disease
When patients were asked how they felt about their disease, over half of those who volunteered expressed a fear of dying due to the disease. Many patients felt frustrated with their illness and the burden it placed on their families. Some participants expressed ambivalence about their disease while others expressed helplessness and fatalism. For example, this hypertensive patient said, “God decides who should suffer from it. Whoever is fated to get high blood pressure will get it. That is it.”
Attitude toward behavioral change
A majority of patients interviewed reported that they would listen to their physician's advice or take medications regularly if detected to be at an increased risk for CVD. About half of those who volunteered a response said that they would improve their diet or exercise regularly. Three participants mentioned avoiding tobacco and reducing alcohol intake as being important. The remaining participants believed that they were already doing everything within their power or that it was God's will.
Facilitators and barriers to CV risk factor control
Figures 1 and 2 describe the facilitators and barriers to CV risk factor control in our population.
Figure 1.
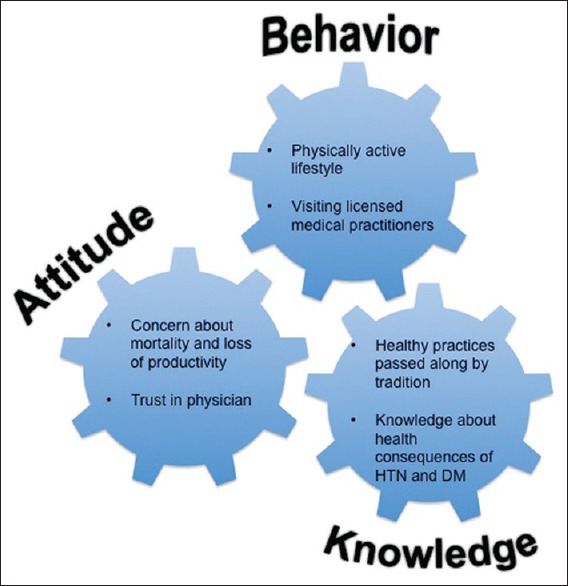
Facilitators that facilitate cardiovascular risk factor control
Figure 2.
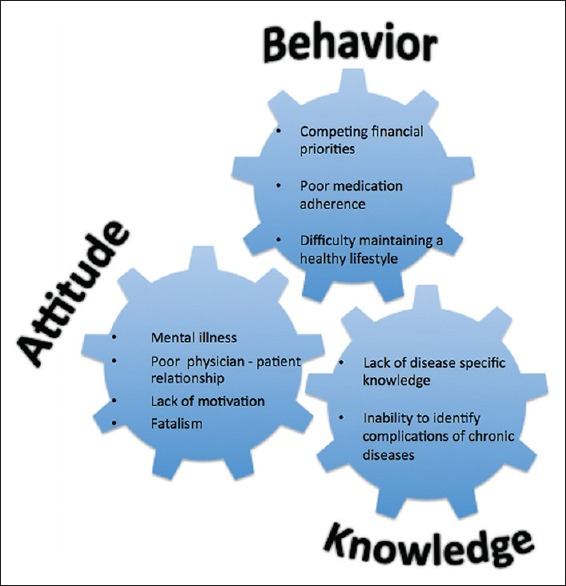
Barriers to cardiovascular risk factor control
Most respondents felt that their financial condition was the most significant barrier, rendering them incapable of visiting the doctor or purchasing medicines. This diabetic patient gave us an example. “If I take medicines, I'll have to spend INR 5000 a month (70 USD). I don't have an income of INR 5000, so I take them for five to seven days, and then stop. I take them again when my sugar rises.” There was also evidence of depressive symptoms that acted as barriers to maintaining lifestyle changes. This patient, for example, expressed frustration about his lifestyle after being diagnosed with diabetes. “Ever since my blood sugar level increased, I have thought that it would be better if I died. I am not allowed to eat anything. It'll be better if my heart fails. Many are afraid of death. I am not”. Other concerns were those of social isolation, time constraint, and the extra effort taken to maintain a healthy lifestyle. Participants did not mention taking multiple pills or side effects as barriers to medication adherence.
Behavior
Current health behavior
Table 2 shows the responses given by hypertensive and diabetic patients when asked about current measures undertaken to control their disease.
Table 2.
Current health practices for hypertension and diabetes control (Number of participants who volunteered a response=32)
| Response | No of participants with response, n (%) |
|---|---|
| Carbohydrate and fat restriction | 15 (47%) |
| Taking medications regularly | 9 (28%) |
| Exercise/walking | 7 (22%) |
| Eating at regular intervals | 5 (16%) |
| Making changes to work schedule since being diagnosed | 3 (9%) |
| Reducing salt intake | 2 (6%) |
| Quit smoking | 1 (3%) |
Healthcare preference
A majority of respondents preferred seeing a doctor with an MBBS degree (MD equivalent). A small cohort visited their local informal healthcare practitioner (Allopathic practitioner without a medical degree). “We cannot consult any renowned doctor because we do not have money. The quack doctor buys a few medicines and gives it to us. Once it (blood pressure, blood sugar) reduces, he discontinues the medicines.” Three patients used both allopathic and homoeopathic medications (Ayurveda and gooseberry) and did not seem to be concerned about interactions. Another group of patients did not visit a doctor for their chronic disease but instead trusted their local pharmacist to prescribe medications whenever symptomatic.
Discussion
Poor knowledge about disease complications and management
Our data show several important findings in this semiurban population in India. First, most participants worried about kidney and eye damage as complications of diabetes and hypertension, with a relatively low appreciation of the potential for heart attacks and stroke. Leading from this, few patients recognized the symptoms of a heart attack or stroke, and there was a concerning trend of trying home remedies for such patients, followed by visiting an informal medical provider. This could partially explain why the median time from symptom onset to hospital presentation for acute coronary syndrome (ACS) ranges from 4.5 h to greater than 24 h in some regions of the country.[28] Among other interventions, there is a need for community-wide education programs focusing on prompt identification of symptoms, followed by early consultation with a qualified medical practitioner. A study in South India showed that increasing knowledge in the community was effective in decreasing time to thrombolysis by almost an hour among ACS patients.[29]
Second, our population exhibited a generalized knowledge of healthy lifestyle habits without an in-depth understanding of disease-specific prevention measures. This was similar to other studies performed in Nepal, India, and China where participants were more cognizant of behavioral risk factors than physiological risk factors for CVD.[17,24] For example, many participants said they followed healthy dietary practices such as eating fruits and vegetables. However, they did not know to limit their salt intake as a measure to control hypertension. This is a trend common to other parts of the country as well, with a recent study estimating a mean daily salt intake between 9.45 and 10.41 g/day, almost double the WHO recommended maximum of five g/day.[30] Third, ours is a population where 14% of middle-aged adults use smoked tobacco.[22] It is, therefore, cause for concern that very few participants recognized smoking as an important CV risk factor. This indicates an urgent need for smoking cessation interventions with a focus on education about the harmful effects of smoking.
Attitude toward disease management
Most participants recognized that hypertension and diabetes needed to be controlled and expressed concern about the effect their disease had on them or their family. Fear of an adverse health outcome was a major motivating factor for patients to take medications regularly and adopt a healthy lifestyle. Most patients demonstrated a deep sense of trust in their physicians and were motivated to follow their advice. Capitalizing on this phenomenon, provider education regarding screening and management of chronic diseases has the potential to improve the quality of care received by these patients.[31,32] Further, training non-MBBS providers (informal medical practitioners and alternative medicine practitioners) with an algorithmic approach to screen for CV risk factors, provide lifestyle counseling and refer when necessary may help overcome some of the existing limitations in physician resources in many parts of India.[33]
Gaps in translation from knowledge to practice
It is well recognized in health behavior research that knowledge, while important, is not the sole driver of behavior change. This was seen in our population as well. For example, exercising regularly was perceived to be important but many patients could not translate this into practice. The lifestyle in semiurban regions like Dalkhola has shifted from labor intensive to more sedentary lifestyle patterns. Lack of public spaces such as parks and walking trails, air pollution, and the absence of a culture of exercise likely serve to impede the uptake of regular exercise in this community. Similarly, while many participants recognized that medication adherence was important, only a few reported actually being able to take their medication. Multiple factors likely contribute, and both personal and system-related barriers exist. For example, the practice of using antidiabetic agents as needed for symptom control suggests a poor understanding of the disease process as well as misinformation about the action of these drugs. It was also interesting that patients did not mention medication side effects as a barrier to adherence. Among other reasons, this could be due to a lack of awareness of specific medication side effects. In addition, system related factors like financial barriers contribute significantly to poor medication adherence. In India, most medication payments are private and out of pocket. A WHO report in 2014 showed that many of the lowest paid workers in India would be unable to routinely afford even one pill for hypertension.[13] Another group projected that 78.6% of the Indian population would be at risk of facing catastrophic payments with the purchase of the antidiabetic drug glibenclamide alone.[34] However, providing affordable healthcare alone may not be enough to increase adherence. Protocol-based approaches for providers to engage and educate patients in the control of their disease, simplifying prescriptions and medication synchronization may all provide additional benefit in this regard.
Limitations
We used a focused group discussion format with open-ended questions to allow participants to voice their thoughts according to perceived importance. This precludes an in-depth analysis of each person's views as could be achieved by individual surveys. Another limitation is that this was a single site study. Significant regional variations in beliefs and practices preclude a generalized approach to understanding health behavior in the entire Indian population.
Conclusion
This study identifies several factors influencing CV risk factor control in India using the KAB model. Significant barriers include a lack of knowledge about the disease process, existing cultural beliefs and practices, and competing financial needs. The current study provides qualitative evidence for CV risk factor control interventions in this and other similar resource-constrained communities.
Practice implications
Techniques to overcome the resource limitations include the use of community health workers and mobile technology to disseminate culturally appropriate health information[35] Educating healthcare providers (MBBS and others) may have a significant impact on identifying and managing these diseases in the community. However, improved knowledge will likely need to be coupled with other social interventions to improve lifestyle and lower financial barriers to modern medical care to effect a significant change.
Financial support and sponsorship
This work was supported by funding from the Marwari Yuva Munch, Dalkhola, India.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Prabhakaran D, Singh K, Roth GA, Banerjee A, Pagidipati NJ, Huffman MD. Cardiovascular diseases in India compared with the United States. J Am Coll Cardiol. 2018;72:79–95. doi: 10.1016/j.jacc.2018.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prabhakaran D, Jaacks LM. Reflections from India on scaling up risk factor control for cardiovascular diseases to reach 1 billion adults. Circulation. 2019;139:4–6. doi: 10.1161/CIRCULATIONAHA.118.035975. [DOI] [PubMed] [Google Scholar]
- 3.Faizi N, Khalique N, Ahmad A, Shah MS. The dire need for primary care specialization in India: Concerns and challenges. J Family Med Prim Care. 2016;5:228–33. doi: 10.4103/2249-4863.192382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varghese C, Nongkynrih B, Onakpoya I, McCall M, Barkley S, Collins TE. Better health and wellbeing for billion more people: Integrating non-communicable diseases in primary care. BMJ. 2019;364:l327. doi: 10.1136/bmj.l327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD Compare. Institute of Health Metrics and Evaluation. 2010 [Google Scholar]
- 6.Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V, et al. Increasing expenditure on health care incurred by diabetic subjects in a developing country. Diabetes Care. 2007;30:252–6. doi: 10.2337/dc06-0144. [DOI] [PubMed] [Google Scholar]
- 8.Kumaraswamy RC, Kauser MM, Jagadeesh MK, Kumar RU, Kumar SRV, Afreen A, et al. Study of determinants of nonadherence to anti-hypertensive medications in essential hypertension at a Teaching Hospital in Southern India. CHRISMED J Health Res. 2015;2:57–60. Available from: http://www.cjhr.org/text.asp?2015/2/1/57/149348 . [Google Scholar]
- 9.Rao CR, Kamath VG, Shetty A, Kamath A. Treatment compliance among patients with hypertension and type 2 diabetes mellitus in a coastal population of Southern India. Int J Prev Med. 2014;5:992–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Sweileh W, Aker O, Hamooz S. Rate of compliance among patients with diabetes mellitus and hypertension. An-Najah Univ J Res (N Sci) 2005;19:1–11. [Google Scholar]
- 11.Venkatachalam J, Abrahm SB, Singh Z, Stalin P, Sathya GR. Determinants of patient's adherence to hypertension medications in a rural population of Kancheepuram District in Tamil Nadu, South India. Indian J Community Med. 2015;40:33–7. doi: 10.4103/0970-0218.149267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aubert L, Bovet P, Gervasoni JP, Rwebogora A, Waeber B, Paccaud F. Knowledge, attitudes, and practices on hypertension in a country in epidemiological transition. Hypertension. 1998;31:1136–45. doi: 10.1161/01.hyp.31.5.1136. [DOI] [PubMed] [Google Scholar]
- 13.Mendis S. Global status report on noncommunicable diseases 2014. World Health Organization; 2014. [DOI] [PubMed] [Google Scholar]
- 14.Vishnu N, Mini GK, Thankappan KR. Complementary and alternative medicine use by diabetes patients in Kerala, India. Glob Health Epidemiol Genom. 2017;2:1–7. doi: 10.1017/gheg.2017.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kesavadev J, Saboo B, Sadikot S, Das AK, Joshi S, Chawla R, et al. Unproven therapies for diabetes and their implications. Adv Ther. 2017;34:60–77. doi: 10.1007/s12325-016-0439-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khan MS, Jafary FH, Faruqui AM, Rasool SI, Hatcher J, Chaturvedi N, et al. High prevalence of lack of knowledge of symptoms of acute myocardial infarction in Pakistan and its contribution to delayed presentationto the hospital. BMC Public Health. 2007;7:284. doi: 10.1186/1471-2458-7-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duber HC, McNellan CR, Wollum A, Phillips B, Allen K, Brown JC, et al. Public knowledge of cardiovascular disease and response to acute cardiac events in three cities in China and India. Heart. 2018;104:67–72. doi: 10.1136/heartjnl-2017-311388. [DOI] [PubMed] [Google Scholar]
- 18.Deepa M, Bhansali A, Anjana RM, Pradeepa R, Joshi SR, Joshi PP, et al. Knowledge and awareness of diabetes in urban and rural India: The Indian Council of Medical Research India diabetes study (phase I): Indian Council of Medical Research India diabetes 4. Indian J Endocrinol Metab. 2014;18:379–85. doi: 10.4103/2230-8210.131191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah S, Singh N, Qureshi W. Prevalence of complementary and alternative medicine in patients with chronic kidney disease in India. Am J Kidney Dis. 2013;61:B88. [Google Scholar]
- 20.Muninarayana C, Balachandra G, Hiremath SG, Iyengar K, Anil NS. Prevalence and awareness regarding diabetes mellitus in rural Tamaka, Kolar. Int J Diabetes Dev Ctries. 2010;30:18–21. doi: 10.4103/0973-3930.60005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khetan A, Purushothaman R, Zullo M, Gupta R, Hejjaji V, Agarwal S, et al. Rationale and design of a cluster-randomized controlled trial to evaluate the effects of a community health worker–based program for cardiovascular risk factor control in India. Am Heart J. 2017;185:161–72. doi: 10.1016/j.ahj.2016.10.027. [DOI] [PubMed] [Google Scholar]
- 22.Khetan A, Zullo M, Hejjaji V, Barbhaya D, Agarwal S, Gupta R, et al. Prevalence and pattern of cardiovascular risk factors in a population in India. Heart Asia. 2017;9:1–7. doi: 10.1136/heartasia-2017-010931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedman AL, Shepeard H. Exploring the knowledge, attitudes, beliefs, and communication preferences of the general public regarding HPV: Findings from CDC focus group research and implications for practice. Health Educ Behav. 2007;34:471–85. doi: 10.1177/1090198106292022. [DOI] [PubMed] [Google Scholar]
- 24.Vaidya A, Aryal UR, Krettek A. Cardiovascular health knowledge, attitude and practice/behaviour in an urbanising community of Nepal: A population-based cross-sectional study from Jhaukhel-Duwakot Health Demographic Surveillance Site. BMJ open. 2013;3:e002976. doi: 10.1136/bmjopen-2013-002976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morgan DL. The Focus Group Guide. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 26.Webel AR, Perazzo JD, Dawson-Rose C, Smith C, Nicholas PK, Rivero-Méndez M, et al. A multinational qualitative investigation of the perspectives and drivers of exercise and dietary behaviors in people living with HIV. Appl Nurs Res. 2017;37:13–8. doi: 10.1016/j.apnr.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 28.Guha S, Sethi R, Ray S, Bahl VK, Shanmugasundaram S, Kerkar P, et al. Cardiological Society of India: Position statement for the management of ST elevation myocardial infarction in India. Indian Heart J. 2017;69:S63–97. doi: 10.1016/j.ihj.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prabhakaran D, Jeemon P, Goenka S, Lakshmy R, Thankappan KR, Ahmed F, et al. Impact of a worksite intervention program on cardiovascular risk factors. J Am Coll Cardiol. 2009;53:1718–28. doi: 10.1016/j.jacc.2008.12.062. [DOI] [PubMed] [Google Scholar]
- 30.Johnson C, Mohan S, Rogers K, Shivashankar R, Thout SR, Gupta P, et al. Mean dietary salt intake in urban and rural areas in India: A population survey of 1395 persons. J Am Heart Assoc. 2017;6:e004547. doi: 10.1161/JAHA.116.004547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Qureshi NN, Hatcher J, Chaturvedi N, Jafar TH. Effect of general practitioner education on adherence to antihypertensive drugs: Cluster randomised controlled trial. BMJ. 2007;335:1030. doi: 10.1136/bmj.39360.617986.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anchala R, Kaptoge S, Pant H, Di Angelantonio E, Franco OH, Prabhakaran D. Evaluation of effectiveness and cost-effectiveness of a clinical decision support system in managing hypertension in resource constrained primary health care settings: Results from a cluster randomized trial. J Am Heart Assoc. 2015;4:e001213. doi: 10.1161/JAHA.114.001213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Das J, Chowdhury A, Hussam R, Banerjee AV. The impact of training informal health care providers in India: A randomized controlled trial. Science. 2016;354:aaf7384. doi: 10.1126/science.aaf7384. [DOI] [PubMed] [Google Scholar]
- 34.Niëns LM, Van de Poel E, Cameron A, Ewen M, Laing R, Brouwer WBF. Practical measurement of affordability: An application to medicines. Bull World Health Organ. 2012;90:219–27. doi: 10.2471/BLT.10.084087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feinberg L, Menon J, Smith R, Rajeev JG, Kumar RK, Banerjee A. Potential for mobile health (mHealth) prevention of cardiovascular diseases in Kerala: A population-based survey. Indian Heart J. 2017;69:182–99. doi: 10.1016/j.ihj.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


