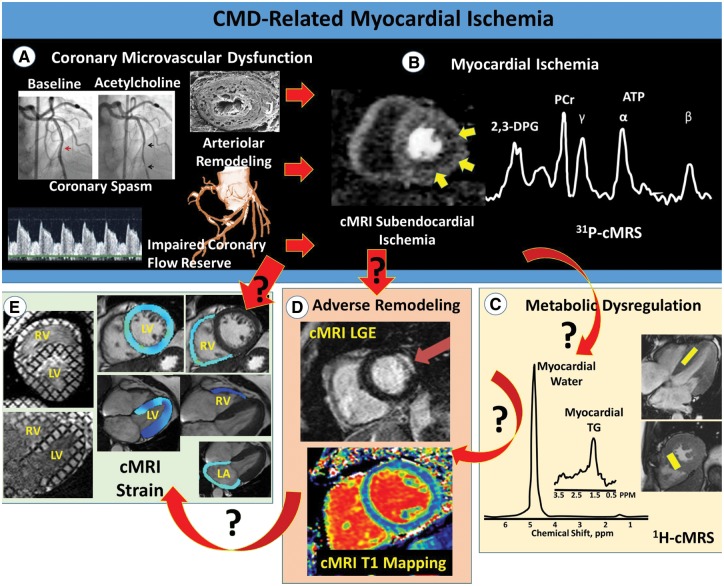
Figure 1.
Potential pathophysiological mechanisms linking CMD to HFpEF. The power of cardiac magnetic resonance imaging/magnetic resonance spectroscopy to define key pathophysiological mechanisms linking coronary microvascular dysfunction-related myocardial ischaemia to heart failure with preserved ejection fraction. Top illustrates traditional invasive measures of CMD (A), and resultant subendocardial ischaemia measured by first-pass perfusion magnetic resonance imaging and altered myocardial bioenergetics measured by 31P magnetic resonance spectroscopy (B). (C–E) illustrate three proposed mechanistic pathways linking coronary microvascular dysfunction-related ischaemia to heart failure with preserved ejection fraction, including cardiac steatosis-induced lipotoxicity (C), adverse remodeling (D), and impaired systolic and diastolic function (E). The red arrows indicate directionality (cause and effect), with black question marks highlighting knowledge gaps for investigation. Note both the simple cause–effect relationship in some cases (e.g. ischaemia-related adverse remodeling), as well as more complex relationships involving multiple pathways. Importantly, cardiac magnetic resonance imaging/magnetic resonance spectroscopy is ideally situated to address all of the proposed mechanistic pathways. 2,3-DPG: 2-3-diphosphoglycerate; ATP: adenosine triphosphate; CMD, coronary microvascular dysfunction; cardiac magnetic resonance imaging/spectroscopy, HFpEF, heart failure with preserved ejection fraction; LA, left atrium; LGE, late gadolinium enhancement; LV, left ventricle; PCr, phosphocreatine; RV, right ventricle; TG, triglyceride.