Abstract
Background
Immunosuppressant nonadherence (INA) has been shown to affect outcomes after solid organ transplantation. The aim of the present study was to determine the prevalence of INA in heart transplant recipients and the associated risk factors of INA.
Methods
Adult heart transplant recipients who firstly received heart transplantation (discharged for at least 3 months) were consecutively enrolled. Immunosuppressant adherence was assessed using the Basel Assessment of Adherence with Immunosuppressive Medication Scale (BAASIS). INA was categorized into five domains of contributing factors (socio-demographic factors, transplant-related factors, healthcare system access factors, post-transplant treatment-related factors, and patient-related psychosocial factors). These factors were compared between adherent and nonadherent patients. The risk factors of INA were investigated by logistic regression analysis.
Results
A total of 168 heart recipients were ultimately included. Among them, 69 (41.1%) recipients were revealed to be nonadherent. Logistic regression analysis indicated that INA was associated with monthly income<3000 Chinese Yuan (CNY) (OR, 3.11; 95% CI, 1.58–6.12; p=0.001), number of prescribed concomitant drugs (OR, 1.23; 95% CI, 1.12–1.50; p=0.003) and concerns about immunosuppressants (OR, 1.09; 95% CI, 1.01–1.18; p=0.031).
Conclusions
Heart recipients had a high prevalence of INA. Lower income, greater number of prescribed concomitant drugs, and more concerns about immunosuppressants correlated most with timing nonadherence and taking nonadherence among heart recipients. These findings will be helpful to intervene on and prevent future INA of heart recipients.
Keywords: heart transplantation, immunosuppressants, adherence, risk factors, interventions
Introduction
Heart transplantation is the gold-standard treatment for refractory end-stage heart failure.1 Heart transplant recipients require numerous medications with complex treatment regimens, including immunosuppressants.2,3 Life-long immunosuppression is often critical for solid organ recipients to prevent graft rejection from an immune response.4,5 Near-perfect adherence to immunosuppressants is crucial to achieving optimal long-term graft survival.2,6 However, many studies have revealed that immunosuppressant nonadherence (INA) has become a persistent problem among solid organ recipients.3,7
INA is defined as “deviation from the prescribed medication regimen sufficient to influence adversely the regimen’s intended effect”.8 The prevalence of INA varies from 2% to 67% (see reviews of Denhaerynck et al9 and Belaiche et al10) in transplant recipients. Meanwhile, the incidence of INA varies by type of transplant, with the highest incidence in kidney transplant recipients (36 cases per 100 patients per year), and the lowest in liver transplant recipients (7 cases per 100 patients per year).11
INA has been associated with high variability in drug blood levels, graft rejection, graft loss, retransplantation and even death.2,12–14 Moreover, the financial cost of INA increases more than $12,000 US dollars per patient over a 3-year time period.15 Despite the clinical impact of INA, there is no effective approach to improving immunosuppressant adherence (IA) in solid organ recipients.16
Identification of risk factors for INA has been helpful in guiding the development of interventional and preventive efforts. To date, factors related to INA can be divided into five aspects: socio-demographic factors, transplant-related factors, healthcare system access factors, post-transplant treatment-related factors, and patient-related psychosocial factors.10,17 The available literature suggests that INA is associated with male gender,10 younger age,6,10 living alone,18 generally negative beliefs about immunosuppressants,6,18 poorer social support,6,10 depression and anxiety,10 and lower mental, but higher physical health-related quality of life.6 However, these findings are mainly from kidney transplant recipients. Therefore, the results are difficult to extrapolate to heart transplant recipients. A multi-center study on INA was conducted in heart transplant recipients, but data from the Far East were not included.19 The prevalence of INA in Chinese heart recipients is not clear, and the related factors have not been investigated.
Therefore, the present study aimed to investigate the prevalence of INA in Chinese heart transplant recipients and to explore the risk factors related to INA, which would be helpful to find out interventions to improve adherence after heart transplantation.
Materials and Methods
Participants
This cross-sectional study was conducted at Union Hospital, Tongji Medical College, Huazhong University of Science and Technology. Eligible patients that were available for follow-up were consecutively enrolled between April 24, 2018 and January 16, 2019. Inclusion criteria were: (1) adult patients (≥18 years old); (2) patients who underwent the first isolated orthotopic heart transplantation and discharged for at least 3 months; (3) patients agreed to participate in the study. Exclusion criteria were: (1) patients that had received a heart transplant in combination with an additional organ, including heart-liver transplantation, combined heart-lung transplantation, etc.; (2) patients unable to understand and communicate in Chinese; (3) patients whose heart transplant procedure did not meet the guidelines set out in the Declaration of Istanbul; (4) and patients with severe mental illness.20 Oral and written informed consent were given to all patients. All organs were donated voluntarily with written informed consent in accordance with the Declaration of Istanbul. This study was carried out in accordance with the principles of the Declaration of Helsinki and approved by the institutional ethics committee of Tongji Medical College, Huazhong University of Science and Technology (IORG No: IORG0003571).
Medication regimens for heart transplant recipients included immunosuppressants to prevent allograft rejection and other concomitant drugs to prevent or treat comorbidities. An initial triple immunosuppressive regimen that included tacrolimus (Prograf®; Astellas Pharma Co., Dublin, Ireland), mycophenolate mofetil (CellCept®; Roche, Shanghai, China) and prednisone acetate (Prednisone®; Huazhong Pharmaceutical Co., Ltd, HuBei, China) was given to all recipients after heart transplantation.21 Oral prednisone was started 3 days after transplantation with an initial dose of 1 mg/kg/d (twice daily) and decreased 5 mg every 3 days to a maintenance dose of 10 mg/d. Patients received steroids-sparing therapy if the occurrence of severe adverse reactions such as osteonecrosis of the femoral head. Sirolimus (Rapamune®; Wyeth Pharmaceuticals Australia Pty Ltd, Baulkham Hills, NSW, Australia) was given concomitantly with the triple immunosuppressive regimen to help relief tacrolimus-related nephrotoxicity. When sirolimus was added to triple immunosuppressive regimen, the dose of tacrolimus was reduced according to the blood concentrations (maintained trough concentration: 4–6 ng/mL). The dose of sirolimus was added according to the blood concentrations (maintained trough concentration: 4–6 ng/mL). Meanwhile, appropriate concomitant drugs were utilized for hypertension, hypercholesterolemia, and other comorbidities.
Data Collection
Data were collected from their electronic medical records and patient interviews in outpatient clinic visits at Union Hospital, Tongji Medical College, Huazhong University of Science and Technology from April 24, 2018 and January 16, 2019. All the interviews were completed by a pharmacist using a patient-centered, non-judgmental and non-threatening approach. Collected data were categorized into five domains of hypothesized factors contributing to INA: (1) Socio-demographic factors; (2) Transplant-related factors; (3) Healthcare system access factors; (4) Post-transplant treatment-related factors; and (5) Patient-related psychosocial factors. Further detail can be found in Table S1.
Five questionnaires were used in this study. All instruments were translated into Chinese and back into English following a standard translation protocol.18 Content validity was checked by two eminent doctors and three pharmacists who worked with the heart transplant recipients.
BAASIS for Measuring Adherence to Immunosuppressants
IA was assessed using the Basel Assessment of Adherence with Immunosuppressive Medication Scale (BAASIS) - a validated and reliable tool to detect self-reported IA among adult transplant recipients.22 Permission to use the BAASIS was obtained from the author and the BAASIS interview version was used in the present study. BAASIS has been developed according to the most recent taxonomy on medication adherence, with the fact that only the implementation aspect of nonadherence is being assessed.23 BAASIS contains four dimensions that contribute to IA: taking adherence (missing≥1 dose), drug holidays (skipping≥1 consecutive doses), timing adherence (taking medication≥2 hrs before or after the prescribed time) and dose alteration (taking more or fewer pills than prescribed or changing dosages without a physician’s order). INA was defined as any positive answer to the 4 BAASIS dimensions. IA was defined as answering “NO” to all four BAASIS instrument dimensions.24,25
BMQ for Measuring Beliefs About Medication
Belief in the necessity of and concerns about immunosuppressants was measured by the Belief Medication Questionnaire (BMQ),13 which has previously been used in transplant recipients.12,26 In our sample, Cronbach’s α was 0.85 for necessity and 0.61 for concerns. The necessity subscale and concerns subscale each contain five items. Each item is scored on a 5-point scale (1=strongly disagree, 5=strongly agree) and is summed resulting in a score for each subscale. High scores indicate a strong belief in the necessity and low concern for the use of immunosuppressants.27
HADS for Anxiety and Depression
Anxiety and depression were assessed by Hospital Anxiety and Depression Scale (HADS), which has been demonstrated to be valid and reliable in solid organ recipients.6 Cronbach’s α in our sample was 0.76 for anxiety and 0.70 for depression. Anxiety and depression were separately measured by seven questions with summed scores ranging from 0 to 21. Higher scores were associated with more anxiety or depression. Scores>10 indicate clinically relevant depression and anxiety; scores lower than seven are considered as clinically not relevant, scores from 8 to 10 are considered “borderline”.6
ISEL-12 for Social Support
Social support was measured by the Interpersonal Support Evaluation List-12 (ISEL-12), which was widely used in solid organ recipients and has been shown to be reliable in this population.28 Cronbach’s α in our sample was 0.91. The ISEL-12 had 12 items that could assess the level of perceived social support on a 4-point scale ranging from 0 (totally false) to 3 (totally true). All items were summed to give a total score ranging from 0 to 36. Higher scores indicate more perceived social support.
SF-12 for Health-Related Quality of Life
Health-related quality of life was assessed with the 12-Item Short-Form Health Survey (SF-12), which was previously used in solid organ recipients.6 Cronbach’s α in our sample was 0.92 for physical health-related quality of life and 0.94 for mental health-related quality of life. Physical Component Summary (PCS) and Mental Component Summary (MCS) scores (summed scores ranging from 0 to100) were calculated using standard methodology.29 Higher values were associated with higher health-related quality of life.6
Statistical Analysis
The overall study population was divided into “Adherent” and “Nonadherent” groups according to the BAASIS results. Different dimensions of BAASIS were described using frequencies and percentages. All characteristics were described with mean and standard deviation (SD) or medians and interquartile range (IQR) for continuous variables, and frequency and percentage for discrete variables. Differences between groups were analyzed by t-tests for normally distributed continuous variables, Mann–Whitney U-tests for non-normally distributed continuous variables, and χ2 tests for dichotomous variables. Further, a logistic model was developed with variables whose p-value<0.05 in comparing the difference between the two groups. All P values were two-tailed, and factors with p-value<0.05 were considered statistically significant. All statistical analyses were performed using the statistical software SPSS Statistics (Version 19.0, SPSS Inc. Chicago, IL, USA).
Results
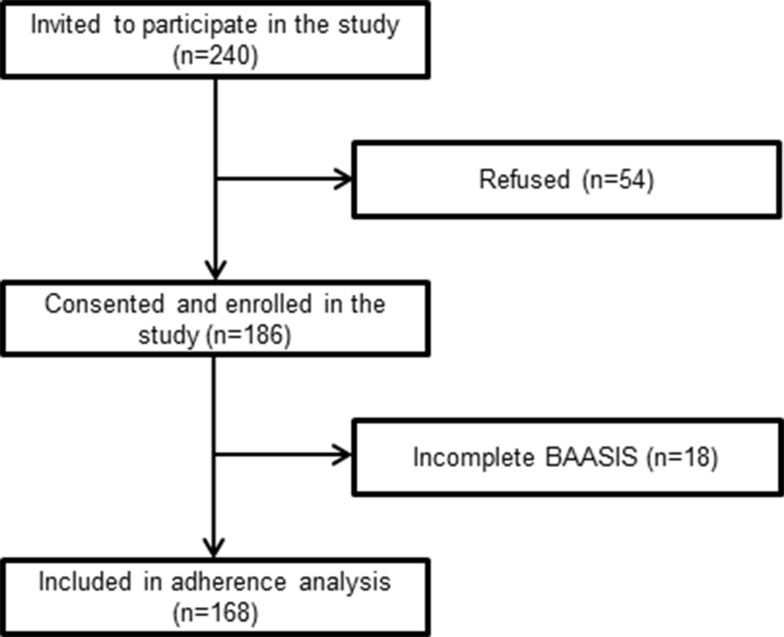
A total of 240 heart recipients came to the hospital for follow-up and were approached. Among them, 168 patients who received a heart transplant between December 18, 2008 and July 11, 2018 (83.9% male; median age, 51.5 years) finished questionnaires and were included into the final analysis. The response rate was 70.0% (The process of patient enrollment and exclusion during patient recruitment was showed in Figure 1.) Different dimensions of IA are shown in Table 1. Generally, 69 (41.1%) patients were identified as nonadherent. A 35.1% of the patients were categorized under timing nonadherence (>2 hrs deviation from dosing schedule) and 14.0% of the patients were categorized undertaking nonadherence (missing doses).
Figure 1.
The process of patient enrollment and exclusion during patient recruitment.
Table 1.
Adherence to Immunosuppressants Measured by BAASIS-Written Questionnaire (N=168)
| Dimension | BAASIS Items | Response | n (%) |
|---|---|---|---|
| Taking adherence | 1: Do you remember missing a dose of your anti-rejection medications in the last 4 weeks? | Once | 19 (11.3) |
| Twice | 4 (2.4) | ||
| Three times | 0 (0.0) | ||
| Four times | 0 (0.0) | ||
| More than 4 times | 0 (0.0) | ||
| 23 (14.0) | |||
| Drug holiday | 2a: Do you remember having skipped two or more doses of your anti-rejection medications in a row in the last 4 weeks? | Once | 8 (4.8) |
| Twice | 0 (0.0) | ||
| Three times | 0 (0.0) | ||
| Four times | 0 (0.0) | ||
| More than 4 times | 0 (0.0) | ||
| 8 (4.8) | |||
| Timing adherence | 3: Do you remember having taken your anti-rejection medications more than 2 hrs before or after the recommended dosing time in the last 4 weeks? | Once | 23 (14.0) |
| 2–3 times | 14 (8.3) | ||
| 4–5 times | 12 (7.1) | ||
| Every 2–3 days | 8 (4.8) | ||
| Almost every day | 2 (1.2) | ||
| 59 (35.1) | |||
| Dose alteration | 4: Have you altered the prescribed amount (for example, taken more or fewer pills or changed your dose) of your anti-rejection medications during the last 4 weeks, without your doctor telling you to do so? | Yes | 7 (4.2) |
| 7 (4.2) | |||
| Overall nonadherence | 69 (41.1) | ||
Notes: aFor patients who answered “yes” to 1; Bold values of the table were the sums of patients have positive answers to the dimensions.
Abbreviation: BAASIS, basel assessment of adherence to immunosuppressive medication scale.
As seen in Table 2, a significantly higher proportion of nonadherent patients had less than a high school level education (53.6% vs. 37.4%, p=0.037), monthly income less than 3000 CNY (59.4% vs. 31.3%, p<0.001) and living in a rural area (36.2% vs. 20.2%, p=0.021) compared with adherent patients. Moreover, nonadherent patients were prescribed a greater median number of concomitant drugs than adherent patients (median 6.0 vs. median 5.0, p=0.004).
Table 2.
Differences Between Adherent and Nonadherent Patients About Socio-Demographic, Transplant-Related, Healthcare System Access and Post-Transplant Treatment-Related Factors
| Characteristics | Total Sample (n=168) | Adherent (n=99) | Nonadherent (n=69) | P |
|---|---|---|---|---|
| Socio-demographic factors | ||||
| Age, years (IQR) | 51.5 (41.0–58.0) | 51.0 (41.0–58.0) | 52.0 (41.0–59.0) | 0.768 |
| Male sex (%) | 141 (83.9) | 81 (81.8) | 60 (87.0) | 0.372 |
| Education level: less than high school (%) | 74 (44.0) | 37 (37.4) | 37 (53.6) | 0.037 |
| Monthly income < 3000 CNY (%) | 72 (42.9) | 31 (31.3) | 41 (59.4) | <0.001 |
| Marital status: single/divorced/widowed (%) | 27 (16.1) | 15 (15.2) | 12 (17.4) | 0.697 |
| Living alone (%) | 19 (11.3) | 8 (8.1) | 11 (15.9) | 0.139 |
| Transplant-related factors | ||||
| Years after transplantation (SD) | 2.9 (2.0) | 2.9 (2.1) | 3.1 (1.7) | 0.498 |
| Age at the time of transplantation (IQR) | 46.1 (12.5) | 45.9 (12.7) | 46.4 (12.3) | 0.804 |
| Healthcare system access factors | ||||
| Living in rural (lack of transportation) (%) | 45 (26.8) | 20 (20.2) | 25 (36.2) | 0.021 |
| Type of insurance (%) | 0.165 | |||
| Medical insurance for urban and rural residents | 94 (56.0) | 51 (51.5) | 43 (62.3) | |
| Employee basic medical insurance | 74 (44.0) | 48 (48.5) | 26 (37.7) | |
| Post-transplant treatment-related factors | ||||
| Immunosuppressive medication (%) | ||||
| Prednisone | 154 (91.7) | 89 (89.9) | 65 (94.2) | 0.402 |
| Sirolimus | 8 (4.8) | 4 (4.0) | 4 (5.8) | 0.718 |
| Daily dose of tacrolimus (IQR) | 2.8 (2.0–4.0) | 3.0 (2.0–4.0) | 2.8 (2.0–4.0) | 0.710 |
| Comorbidities | ||||
| Diabetes | 61 (36.3) | 36 (36.4) | 25 (36.2) | 0.986 |
| Hypertension | 131 (78.0) | 76 (76.8) | 55 (79.7) | 0.651 |
| Hyperlipemia | 100 (59.5) | 61 (61.6) | 39 (56.5) | 0.508 |
| Hyperuricemia | 60 (35.7) | 34 (34.3) | 26 (37.7) | 0.657 |
| Number of prescribed concomitant drugs (IQR) | 5.5 (4.0–7.0) | 5.0 (3.0–7.0) | 6.0 (5.0–8.0) | 0.004 |
Note: The bold values indicate these variables that were statistically significant (p<0.05).
Abbreviations: CNY, Chinese Yuan; IQR, interquartile range; SD, standard deviation.
Nonadherent patients were significantly different from adherent patients in psychosocial factors (Table 3). Specifically, nonadherent patients had more concerns about immunosuppressants compared to adherent patients (19.3 vs. 17.3, p=0.003). Nonadherent patients also had lower median anxiety scores (10.0 vs. 12.0, p=0.041), a poorer PCS score (44.6 vs. 48.0, p=0.002) and lower MCS score (44.4 vs. 49.1, p=0.001). The details of differences between nonadherent and adherent patients were shown in Tables 2 and 3.
Table 3.
Differences Between Adherent and Nonadherent Patients About Patient-Related Psychosocial Factors
| Characteristic | Total Sample (n=168) | Adherent (n=99) | Nonadherent (n=69) | P |
|---|---|---|---|---|
| Necessity (IQR) | 20.0 (18.3–23.0) | 20.0 (19.0–23.0) | 20.0 (18.0–23.0) | 0.439 |
| Concerns (SD) | 18.1 (4.5) | 17.3 (4.2) | 19.3 (4.6) | 0.003 |
| Anxiety score (IQR) | 11.0 (9.0–14.0) | 12.0 (10.0–14.0) | 10.0 (9.0–13.0) | 0.041 |
| Depression score (IQR) | 9.0 (8.0–11.0) | 10.0 (8.0–12.0) | 9.0 (7.5–11.0) | 0.290 |
| Social support (IQR) | 24.0 (23.0–29.0) | 24.0 (23.0–29.0) | 24.0 (23.0–28.5) | 0.981 |
| PCS score (SD) | 46.6 (7.0) | 48.0 (6.9) | 44.6 (6.7) | 0.002 |
| MCS score (IQR) | 47.8 (42.2–50.9) | 49.1 (44.6–51.2) | 44.4 (40.5–48.9) | 0.001 |
Note: The bold values indicate these variables that were statistically significant (p<0.05).
Abbreviations: IQR, interquartile range; SD, standard deviation; PCS, Physical Component Summary; MCS, Mental Component Summary.
As shown in Table 4, the logistic model demonstrated that risk factors associated with INA were a monthly income<3000 CNY (OR, 3.11; 95% CI, 1.58–6.12; p=0.001), number of prescribed concomitant drugs (OR, 1.23; 95% CI, 1.12–1.50; p=0.003) and concerns about immunosuppressants (OR, 1.09; 95% CI, 1.01–1.18; p=0.031). However, education level, living in rural, anxiety, PCS score and MCS score were not statistically significant in the final model.
Table 4.
Logistic Regression Model for the Risk Factors of NonAdherence
| Regression Coefficient B | Wald | Odds Ratio | 95% Confidence Interval | P (Single Risk Factors) | P (Whole Model) | |
|---|---|---|---|---|---|---|
| Monthly income< 3000 CNY | 1.14 | 10.78 | 3.11 | 1.58–6.12 | 0.001 | < 0.001 |
| Number of prescribed concomitant drugs | 0.20 | 8.83 | 1.23 | 1.12–1.50 | 0.003 | |
| Concerns | 0.09 | 4.67 | 1.09 | 1.01–1.18 | 0.031 |
Abbreviation: CNY, Chinese Yuan.
Discussion
This study appears to be the first to evaluate the IA in Chinese heart transplant recipients. The present study found that more than one-third of heart recipients were nonadherent to immunosuppressants. INA was mainly caused by missing doses of immunosuppressants and taking medication≥2 hrs before or after the prescribed time. The incidence of INA was found to be associated with lower income, a greater number of prescribed concomitant drugs, and more concerns about immunosuppressants.
Prevalence of INA in this study (41.1%) was higher than Denhaerynck et al19 observed in their study. The 4-continent, 11-country cross-sectional Building Research Initiative Group: Chronic Illness Management and Adherence in Transplantation (BRIGHT) study assessed INA of heart transplant recipients using BAASIS and found the overall prevalence of INA was 34.1%.19 The observed discrepancy in INA prevalence might be partly explained by the limited sample size in the present study. Another possible explanation is that this discrepancy might arise from regional differences. The majority of participants in the BRIGHT study were from Europe, North America, South America, or Australia and 85.9% of patients were white.19 In this study, the heart recipients were Chinese. Our results were similar to a study conducted among Chinese using BAASIS, in which 39.4% of liver transplant recipients were nonadherent.25 Additionally, a possibility of the higher nonadherence could be related to the setting. The present center lacks routine care related to the management of medication adherence (such as routine assessment of medication adherence, adherence support programs, and provider training), which should be taken into consideration in the future. In line with previous studies,19,25 timing nonadherence dimension (missing≥1 dose) and taking nonadherence dimension (skipping≥1 consecutive dose) characterized most of the nonadherent recipients.
The relationship between INA and low income from this study support previous findings in kidney recipients that being short on money or residing in a lower economic status was associated with nonadherence.26,30 Furthermore, low-income transplant patients had difficulty in affording the long-term immunosuppressant costs, which may have resulted in intentional or unintentional INA.2
The association of nonadherence with the number of prescribed concomitant drugs was consistent with earlier findings from kidney transplant recipients which demonstrated a strong association between greater pill burden and nonadherence to Calcineurin Inhibitors (CNIs).31 Another study conducted among patients with end-stage liver disease also supported our observation of more prescribed medications and greater regimen complexity strongly correlating with INA.32
Moreover, concerns about the potential adverse effects of immunosuppressants were associated with nonadherence in this study, which correlates with prior studies of kidney transplant recipients where more medication concerns indicated poorer adherence.27,33 However, other studies of kidney recipients found adherence was not associated with concerns about immunosuppressants (as measured by the BMQ).6,26 One possible explanation for the discrepancy is that recipients had different perceptions about immunosuppressants.34 Nonadherent recipients in the present study may have had more concerns about the potential for adverse effects of immunosuppressants compared with adherent recipients. Findings from this study suggested increased efforts should be made by health care providers to promote the necessity of immunosuppressants and address the concerns patients have with long-term use of immunosuppressants.
This study did not find a significant association between INA and anxiety or depression, which differed from earlier studies of renal transplant recipients.10,35 However, close attention should be paid to the emotional state of heart transplant recipients. In the present study, 59.5% of recipients had clinically relevant anxiety (HADS anxiety score>10), which is comparable to the proportion found in the study of Scheel et al6 (63.9% with HADS anxiety score>10). Moreover, 32.7% recipients in the present study exhibited clinically relevant depression symptoms (HADS depression score>10), which is higher than the findings of Scheel et al6 (16.7% with HADS depression score>10). Also, the prevalence of clinically relevant anxiety and depression symptoms was much higher than the findings of Weng et al36 (6.0% with HADS anxiety score>10 and 2.0% with a HADS depression score>10). Therefore, efforts should be made to improve the emotional state of heart transplant recipients in the future.
These risk factors found in the present study had important implications for developing evidence-based interventions to improve immunosuppressant adherence after heart transplantation. There were some interventions that have been tested and found efficacious, including education, cognitive/behavioral interventions (behavioral contracts, pharmacist counseling, motivational interviewing, etc.).37 However, these interventions varied among different centers with diverse patient populations, and resources for adherence monitoring.37 Thus, the interventions may need to be tailored to meet the transplant recipients in different ways. For the heart recipients in the present study, lower income, a greater number of prescribed concomitant drugs, and more concerns about immunosuppressants might be the focus of intervention in order to improve immunosuppressants adherence in the present center. However, our findings were preliminary, further research should be warranted to investigate the intervention fits the present center.
There were some limitations to the present study. First, this was a single-center cross-sectional study with a small sample size. The sample size was limited by the small population of heart transplant recipients. Second, adherence was assessed using only a BAASIS questionnaire, which might underestimate the incidence of INA.38 Electronic monitoring systems are the gold standard for assessing adherence because of their reliance on objective measures rather than the subjective measures in this study.6 Despite these limitations, this study demonstrates the prevalence and associated risk factors of INA in heart transplant recipients. We anticipate the findings from this study will be able to be drawn upon in future efforts to intervene on and prevent future INA.
Conclusion
In conclusion, the prevalence of INA (majoritively associated with timing and taking nonadherence) in Chinese heart transplant recipients was 41.1%. Recipients with lower income, greater number of prescribed concomitant drugs and more concerns with using immunosuppressants were the most likely to demonstrate INA. Greater attention to these indicative INA risk factors in heart transplant recipients may be useful for clinicians to assist in detecting where greater efforts in preventing and intervening on INA may be necessary.
Funding
This study was supported by National Natural Science Foundation of China (81703630, 81673456) and the National Key R&D Program of China (2017YFC0909900).
Disclosure
There are no conflicts of interest.
References
- 1.Dhital KK, Iyer A, Connellan M, et al. Adult heart transplantation with distant procurement and ex-vivo preservation of donor hearts after circulatory death: a case series. Lancet. 2015;385(9987):2585–2591. doi: 10.1016/S0140-6736(15)60038-1 [DOI] [PubMed] [Google Scholar]
- 2.Doyle IC, Maldonado AQ, Heldenbrand S, Tichy EM, Trofe-Clark J. Nonadherence to therapy after adult solid organ transplantation: a focus on risks and mitigation strategies. Am J Health Syst Pharm. 2016;73(12):378–389. doi: 10.2146/ajhp150650 [DOI] [PubMed] [Google Scholar]
- 3.Helmy R, Scalso de Almeida S, Denhaerynck K, et al. Prevalence of medication nonadherence to co-medication compared to immunosuppressants in heart transplant recipients: findings from the international cross-sectional BRIGHT study. Clin Ther. 2019;41(1):130–136. doi: 10.1016/j.clinthera.2018.11.007 [DOI] [PubMed] [Google Scholar]
- 4.Scheel J, Reber S, Stoessel L, et al. Patient-reported non-adherence and immunosuppressant trough levels are associated with rejection after renal transplantation. BMC Nephrol. 2017;18(1):107. doi: 10.1186/s12882-017-0517-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Senft Y, Kirsch M, Denhaerynck K, et al. Practice patterns to improve pre and post-transplant medication adherence in heart transplant centres: a secondary data analysis of the international BRIGHT study. Eur J Cardiovasc Nurs. 2017;17(4):356–367. doi: 10.1177/1474515117747577 [DOI] [PubMed] [Google Scholar]
- 6.Scheel JF, Schieber K, Reber S, et al. Psychosocial variables associated with immunosuppressive medication non-adherence after renal transplantation. Front Psychiatry. 2018;9:23. doi: 10.3389/fpsyt.2018.00023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castleberry AW, Bishawi M, Worni M, et al. Medication nonadherence after lung transplantation in adult recipients. Ann Thorac Surg. 2017;103(1):274–280. doi: 10.1016/j.athoracsur.2016.06.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fine RN, Becker Y, De Geest S, et al. Nonadherence consensus conference summary report. Am J Transplant. 2009;9(1):35–41. doi: 10.1111/j.1600-6143.2008.02495.x [DOI] [PubMed] [Google Scholar]
- 9.Denhaerynck K, Dobbels F, Cleemput I, et al. Prevalence, consequences, and determinants of nonadherence in adult renal transplant patients: a literature review. Transpl Int. 2005;18(10):1121–1133. doi: 10.1111/tri.2005.18.issue-10 [DOI] [PubMed] [Google Scholar]
- 10.Belaiche S, Décaudin B, Dharancy S, et al. Factors relevant to medication non-adherence in kidney transplant: a systematic review. Int J Clin Pharm. 2017;39(3):582–593. doi: 10.1007/s11096-017-0436-4 [DOI] [PubMed] [Google Scholar]
- 11.Dew MA, DiMartini AF, De Vito Dabbs A, et al. Rates and risk factors for nonadherence to the medical regimen after adult solid organ transplantation. Transplantation. 2007;83(7):858–873. doi: 10.1097/01.tp.0000258599.65257.a6 [DOI] [PubMed] [Google Scholar]
- 12.Belaiche S, Décaudin B, Dharancy S, et al. Factors associated with the variability of calcineurin inhibitor blood levels in kidney recipients grafted for more than 1 year. Fundam Clin Pharmacol. 2017;32(1):88–97. doi: 10.1111/fcp.12328 [DOI] [PubMed] [Google Scholar]
- 13.Massey EK, Tielen M, Laging M, et al. Discrepancies between beliefs and behavior: a prospective study into immunosuppressive medication adherence after kidney transplantation. Transplantation. 2015;99(2):375–380. doi: 10.1097/TP.0000000000000608 [DOI] [PubMed] [Google Scholar]
- 14.Killian MO, Schuman DL, Mayersohn GS, Triplett KN. Psychosocial predictors of medication non-adherence in pediatric organ transplantation: a systematic review. Pediatr Transplant. 2018;22(4):e13188. doi: 10.1111/petr.2018.22.issue-4 [DOI] [PubMed] [Google Scholar]
- 15.Pinsky BW, Takemoto SK, Lentine KL, Burroughs TE, Schnitzler MA, Salvalaggio PR. Transplant outcomes and economic costs associated with patient noncompliance to immunosuppression. Am J Transplant. 2009;9(11):2597–2606. doi: 10.1111/ajt.2009.9.issue-11 [DOI] [PubMed] [Google Scholar]
- 16.Shneider C, Dunphy C, Shemesh E, Annunziato RA. Assessment and treatment of nonadherence in transplant recipients. Gastroenterol Clin North Am. 2018;47(4):939–948. doi: 10.1016/j.gtc.2018.07.015 [DOI] [PubMed] [Google Scholar]
- 17.Sabaté E. Adherence to long-term therapies: evidence for action [Internet]. Geneva: World Health Organization; 2003. Available from: http://apps.who.int/medicinedocs/en/d/Js4883e/.18. [Google Scholar]
- 18.Hugon A, Roustit M, Lehmann A, et al. Influence of intention to adhere, beliefs and satisfaction about medicines on adherence in solid organ transplant recipients. Transplantation. 2014;98(2):222–228. doi: 10.1097/TP.0000000000000221 [DOI] [PubMed] [Google Scholar]
- 19.Denhaerynck K, Berben L, Dobbels F, et al. Multi-level factors are associated with immunosuppressant nonadherence in heart transplant recipients: the international BRIGHT study. Am J Transplant. 2017;18(6):1447–1460. doi: 10.1111/ajt.14611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruggeri M, Leese M, Thornicroft G, et al. Definition and prevalence of severe and persistent mental illness. Br J Psychiatry. 2000;177(2):149–155. doi: 10.1192/bjp.177.2.149 [DOI] [PubMed] [Google Scholar]
- 21.Zhang M, Han Y, Yuan Y, et al. Risk factors for new-onset diabetes mellitus after heart transplantation in Chinese patients: a single center experience. Ann Nutr Metab. 2019;74(4):331–338. doi: 10.1159/000500138 [DOI] [PubMed] [Google Scholar]
- 22.Dobbels F, Berben L, De Geest S, et al. The psychometric properties and practicability of self-report instruments to identify medication nonadherence in adult transplant patients: a systematic review. Transplantation. 2010;90(2):205–219. doi: 10.1097/TP.0b013e3181e346cd [DOI] [PubMed] [Google Scholar]
- 23.De Geest S, Zullig LL, Dunbar-Jacob J, et al. ESPACOMP medication adherence reporting guideline (EMERGE). Ann Intern Med. 2018;169(1):30–35. doi: 10.7326/M18-0543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fellström B, Holmdahl J, Sundvall N, et al. Adherence of renal transplant recipients to once-daily, prolonged-release and twice-daily, immediate-release tacrolimus-based regimens in a real-life setting in Sweden. Transplant Proc. 2018;50(10):3275–3282. doi: 10.1016/j.transproceed.2018.06.027 [DOI] [PubMed] [Google Scholar]
- 25.Wang C, Wang G, Yi H, et al. Symptom experienced three years after liver transplantation under immunosuppression in adults. PLoS One. 2013;8(11):e80584. doi: 10.1371/journal.pone.0080584 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 26.Cossart AR, Staatz CE, Campbell SB, Isbel NM, Cottrell WN. Investigating barriers to immunosuppressant medication adherence in renal transplant patients. Nephrology (Carlton). 2017;24(1):102–110. doi: 10.1111/nep.13214 [DOI] [PubMed] [Google Scholar]
- 27.Griva K, Neo HLM, Vathsala A. Unintentional and intentional non-adherence to immunosuppressive medications in renal transplant recipients. Int J Clin Pharm. 2018;40(5):1234–1241. doi: 10.1007/s11096-018-0652-6 [DOI] [PubMed] [Google Scholar]
- 28.Sacco P, Sultan S, Tuten M, et al. Substance use and psychosocial functioning in a sample of liver transplant recipients with alcohol-related liver disease. Transplant Proc. 2018;50(10):3689–3693. doi: 10.1016/j.transproceed.2018.07.003 [DOI] [PubMed] [Google Scholar]
- 29.Ware J, Kosinski M, Turner-Bowker D, Gandek B. SF-12v2: How to Score Version 2 of the SF-12 Health Survey. Lincoln, RI, USA: Quality Metric Incorporated; 2002:29–38. [Google Scholar]
- 30.Adhikari UR, Taraphder A, Hazra A, Das T. Medication adherence in kidney transplant recipients in an urban Indian setting. Indian J Nephrol. 2017;27(4):294–300. doi: 10.4103/0971-4065.202835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sabbatini M, Garofalo G, Borrelli S, et al. Efficacy of a reduced pill burden on therapeutic adherence to calcineurin inhibitors in renal transplant recipients: an observational study. Patient Prefer Adherence. 2014;8:73–81. doi: 10.2147/PPA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuo SZ, Haftek M, Lai JC. Factors associated with medication non-adherence in patients with end-stage liver disease. Dig Dis Sci. 2017;62(2):1–7. doi: 10.1007/s10620-016-4391-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weng LC, Yang YC, Huang HL, Chiang YJ, Tsai YH. Factors that determine self-reported immunosuppressant adherence in kidney transplant recipients: a correlational study. J Adv Nurs. 2016;73(1):228–239. doi: 10.1111/jan.13106 [DOI] [PubMed] [Google Scholar]
- 34.Constantiner M, Rosenthal-Asher D, Tedla F, et al. Differences in attitudes toward immunosuppressant therapy in a multi-ethnic sample of kidney transplant recipients. J Clin Psychol Med Settings. 2018;25(1):11–19. doi: 10.1007/s10880-017-9524-9 [DOI] [PubMed] [Google Scholar]
- 35.Cukor D, Rosenthal DS, Jindal RM, Brown CD, Kimmel PL. Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients. Kidney Int. 2009;75(11):1223–1229. doi: 10.1038/ki.2009.51 [DOI] [PubMed] [Google Scholar]
- 36.Weng FL, Chandwani S, Kurtyka KM, Zacker C, Chisholm-Burns MA, Demissie K. Prevalence and correlates of medication non-adherence among kidney transplant recipients more than 6 months post-transplant: a cross-sectional study. BMC Nephrol. 2013;14(1):261. doi: 10.1186/1471-2369-14-261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Myaskovsky L, Jesse MT, Kuntz K, et al. Report from the American society of transplantation psychosocial community of practice adherence task force: real-world options for promoting adherence in adult recipients. Clin Transplant. 2018;32(9):e13353. doi: 10.1111/ctr.13353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Obi Y, Ichimaru N, Kato T, et al. A single daily dose enhances the adherence to immunosuppressive treatment in kidney transplant recipients: a cross-sectional study. Clin Exp Nephrol. 2013;17(2):310–315. doi: 10.1007/s10157-012-0713-4 [DOI] [PubMed] [Google Scholar]