Abstract
The Achilles tendon is the largest, and most commonly torn tendon in the body. The Achilles is usually torn at a region of relative hypo-vascularity proximal to its insertion. However, partial thickness tears and other pathologies often occur at its insertion on the calcaneus. Anatomically, the insertion is a confluence of the gastrocnemius and soleus muscles that fuse to form a myotendinous unit on the posterosuperior aspect of the calcaneus. This review aims to reveal the insertional footprint as individual fascicular components attaching to facets of calcaneal tuberosity. Understanding this anatomy is essential for interpreting tear patterns and surgical implications.
Keywords: Achilles tendon, Achilles complex, Achilles insertion, Achilles rupture, Achilles tear, Calcaneal tuberosity
1. Introduction
The Achilles tendon is the largest and strongest tendon in the body. In the literature, the Achilles tendon is commonly described as a common tendon made up of the soleus and gastrocnemius muscles, which inserts as a single structure broadly on the calcaneal tuberosity. Through cadaveric dissection, however, anatomists have described its insertion as individual fascicles attaching to various calcaneal facets. As the muscular components combine to form the Achilles complex, the individual fascicles rotate in that the medial structures become superficial, and the lateral structures become deep.1, 2, 3, 4
To our knowledge, the insertional footprint has not been described radiologically in the literature. Better understanding of the various attachments from an imaging perspective may guide orthopedic surgeons to the location of specific pathologies, particularly as their related to insertional Achilles tendinopathies. The goal of this paper is to describe the anatomic footprint using cadaveric dissection and MRI to better define detailed relationships between the fascicular components and their insertions.
2. Anatomical considerations
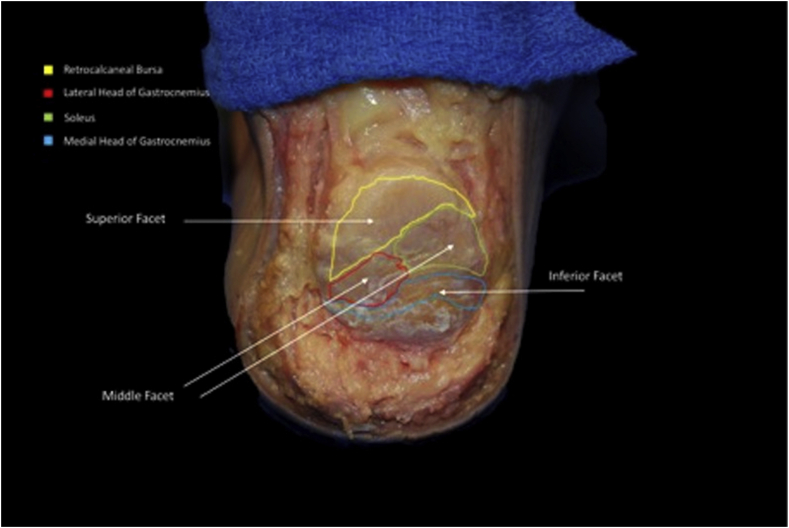
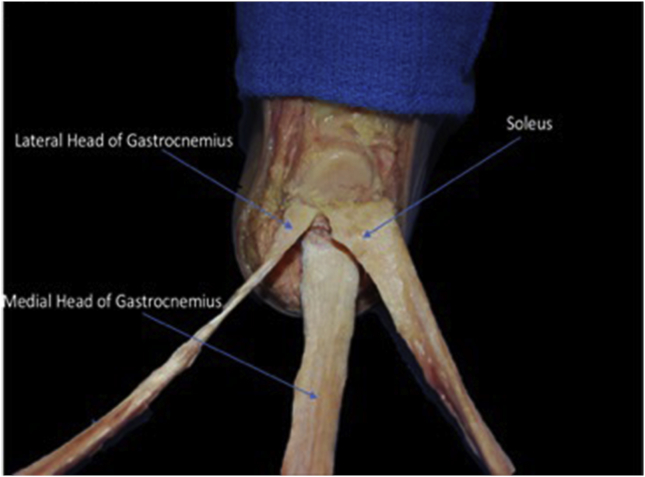
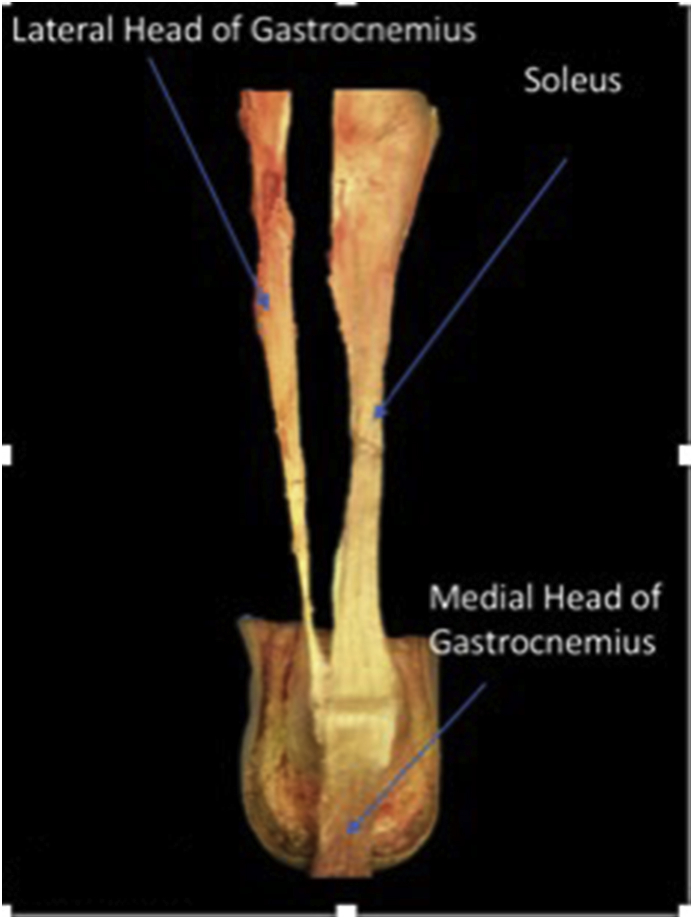
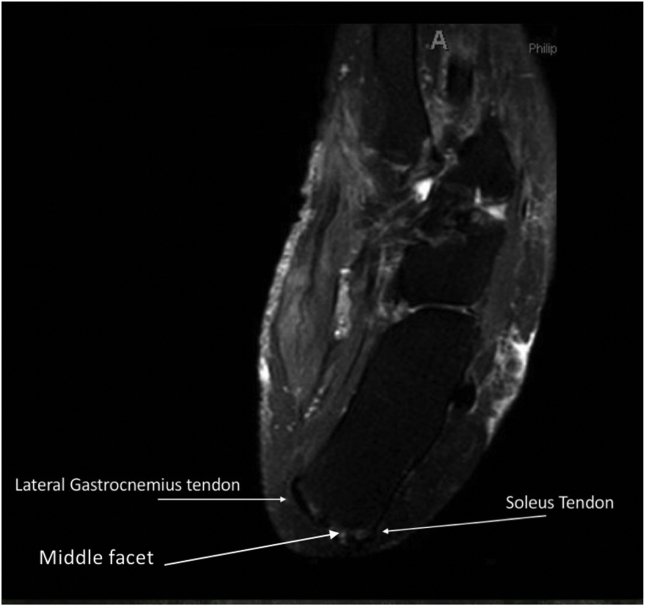
The Achilles tendon complex is derived from a fusion of the soleus, medial and lateral gastrocnemius muscles. The origin of the soleus muscle is from the posterior aspect of the upper fibula and soleal line of the tibia. The medial and lateral gastrocnemius muscles originate from the posterior aspect of the medial and lateral femoral condyles, respectively. In 65% of the population, the plantaris muscle is seen to contribute fascicles to the Achilles complex. First described by Wood Jones in 1944, as the Achilles courses inferiorly, the tendon rotates before its insertion on the calcaneus, so that the fascicles arising from the medial head of the gastrocnemius form the posterior aspect of the tendon, whereas the lateral head and soleus muscles compose the anterior part.1, 2, 3 The osseous anatomical footprint of the Achilles tendon on the calcaneus has been described as superior, middle and inferior facets (Fig. 1). The superior facet serves as the location of the retrocalcaneal bursa. The middle facet can be divided into medial and lateral components, where the soleus inserts medially, and the lateral gastrocnemius inserts laterally (Fig. 2). The inferior facet, or the superficial component of the Achilles tendon, is composed of the medial gastrocnemius muscle (Fig. 3).1,4,5 In some patients, the medial head of the gastrocnemius muscle fascicles had a continuation with the plantar fascia in the form of periosteum.1,4
Fig. 1.
Cadaveric specimen dissected so coronal view of calcaneus can be appreciated. Figure shows insertion footprints of Achilles sub-tendons, as well as location of retrocalcaneal bursa.
Fig. 2.
Cadaveric specimen dissected so coronal view of calcaneus and Achilles tendon can be appreciated. Figure shows insertions of sub-tendons of both gastrocnemius bellies and soleus muscles into their respective calcaneal facets.
Fig. 3.
Cadaveric specimen dissected so Achilles tendon can be appreciated. Figure shows the bundles of the Achilles tendon. The tendon of the medial head of the gastrocnemius is reflected back on itself to reveal the deeper sub-tendons of the Achilles footprint.
Fig. 1 demonstrates a cadaveric specimen dissected with coronal view of calcaneus visible. This demonstrates the insertion footprints of Achilles sub-tendons, as well as location of retrocalcaneal bursa. Fig. 2 also shows us a coronal view of the calcaneus. We can see the insertions of sub-tendons of both gastrocnemius bellies and soleus muscles into their respective calcaneal facets. Finally, Fig. 3 demonstrates the bundles of the Achilles tendon. The tendon of the medial head of the gastrocnemius is reflected back on itself to reveal the deeper sub-tendons of the Achilles footprint.
The course of the Achilles tendon begins proximally at the broad insertion points of both heads of the gastrocnemius muscle and the soleus muscle. However, as these muscle's sub-tendons descend they form a confluence called the triceps curae. It is at this confluence that the true Achilles tendon begins, and it is also at this proximal musculotendinous junction that most acute complete full-thickness thickness Achilles tendon tears occur.
As these sub-tendons descend, they transpose laterally towards their distal insertion, the calcaneal tuberosity. The width of this tendon's insertion footprint varies between individuals from 20 mm to 48mm.1,5, 6, 7, 8, 9, 10 Like a braided rope, the sub-tendons of the Achilles tendon spiral and intertwine as they move laterally and distally towards their insertion site. The twisting of the tendon allows for greater biomechanical strength.
The degree of twisting of the tendon is variable from individual to individual. Consequently, the level of twisting influences the arrangement that each sub-tendon inserts on the facets of the calcaneus. Several studies have attempted to scrutinize the degree of Achilles tendon spiraling in hopes that it could be relatable to predicting potential tendon injuries. One study was able to separate three types of Achilles tendon spiraling, labeled type 1, type 2, and type 3.6,11 These subsets correspond to progressively increased degree of Achilles tendon “twisting”. The majority of the population have what can be described as a “least twisted” arrangement, as already described with the insertional footprint (Fig. 1). The type 3 configuration of the Achilles tendon can be described as “most twisted,” placing the overall tendon under significantly more torsion.
3. Imaging findings
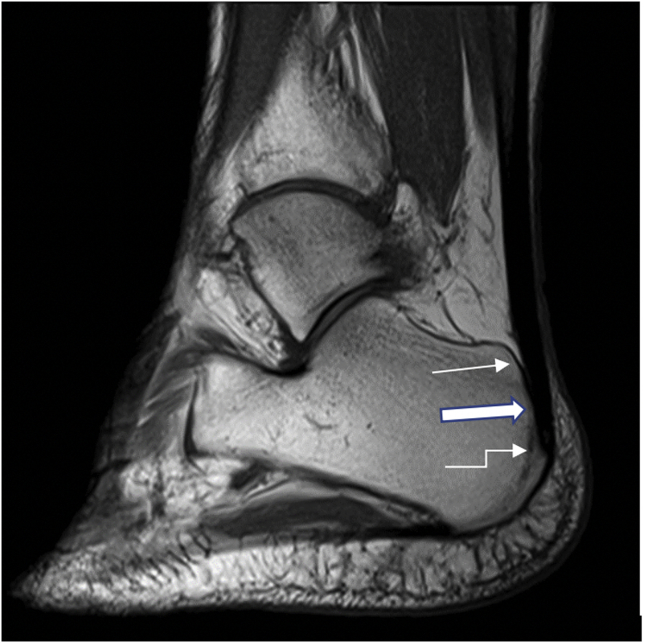
Understanding the normal imaging anatomy is essential for interpreting pathology of the Achilles insertion. On radiographic and MR imaging of the ankle, the calcaneal superior, middle, and inferior facets can be observed which correspond to the retrocalcaneal bursa, deep and superficial components of the Achilles complex, respectively (Fig. 4, Fig. 5).11 We can also see the insertional anatomy of the calcaneus with the superficial facet (thin arrow), middle facet (thick arrow), and inferior facet (bent arrow) clearly demonstrated (Fig. 4). The MRI of the ankle (Fig. 5) demonstrates the normal anatomy of the Achilles tendon in relation to the superior facet (thin arrow) corresponding to the location of the retrocalcaneal bursa, the middle facet (thick arrow) corresponding to the deep structures of the Achilles tendon complex, and the inferior facet (bent arrow) corresponding to the superficial structures of the Achilles tendon complex.
Fig. 4.
Lateral radiograph of the ankle demonstrates the insertional anatomy of the calcaneus with the superficial facet (thin arrow), middle facet (thick arrow), and inferior facet (bent arrow) clearly demonstrated.
Fig. 5.
Sagittal PD MRI of the ankle demonstrates the normal anatomy of the Achilles tendon in relation to the superior facet (thin arrow) corresponding to the location of the retrocalcaneal bursa, the middle facet (thick arrow) corresponding to the deep structures of the Achilles tendon complex, and the inferior facet (bent arrow) corresponding to the superficial structures of the Achilles tendon complex.
The calcaneal facet anatomy corresponds to various pathologies that manifest on imaging. Retrocalcaneal bursitis, an inflammatory process affecting the bursa between the posterosuperior calcaneus and the deep components of the Achilles tendon complex, is anatomically situated at the superior facet of the calcaneus Sagittal PD fat saturated MRI of the ankle demonstrates a patient with Haglunds deformity, where there is retrocalcaneal bursitis occupying the region of the superior facet (arrow Fig. 6). Patients with partial thickness tears at the insertion may show isolated rupture of one or more muscles. For example, partial thickness rupture of the superficial component of the Achilles complex at the inferior facet would show isolated laxity of the medial gastrocnemius myotendinous junction (Fig. 7A–C).11, 12, 13, 14, 15, 16
Fig. 6.
Sagittal PD fat saturated MRI of the ankle demonstrates a patient with Haglunds deformity, where there is retrocalcaneal bursitis occupying the region of the superior facet (arrow).
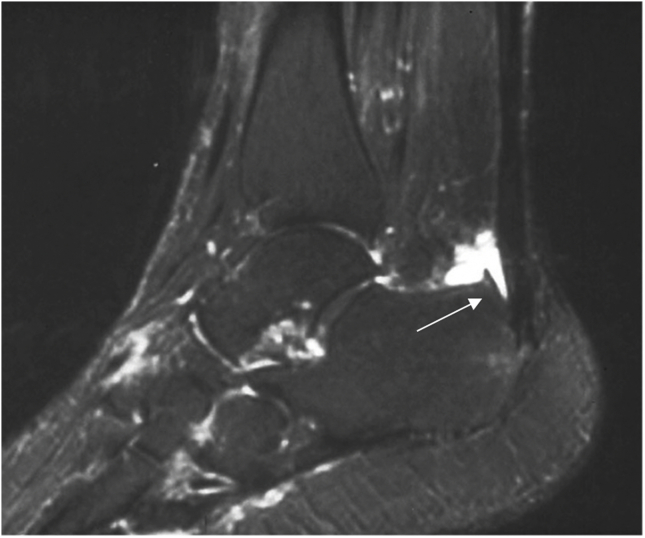
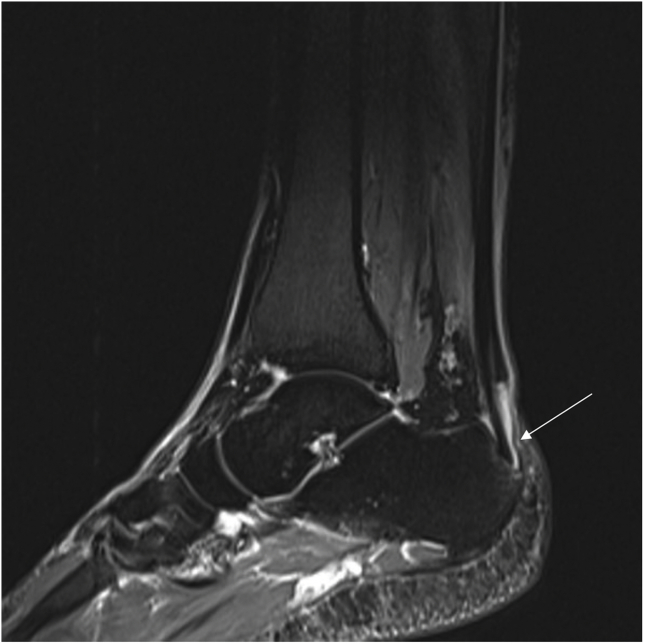
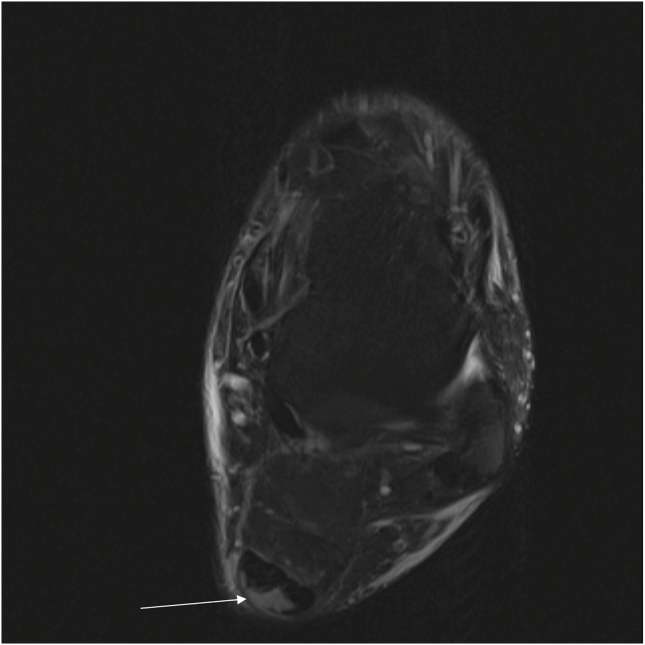
Fig. 7.
a)Sagittal STIR MRI of the ankle demonstrates partial thickness isolated tear of the Achilles tendon insertion at the inferior calcaneal facet (arrow) with retraction of the tendon superiorly. b)Axial PD fat saturated MRI of the ankle (same patient) demonstrates partial thickness tear of the superficial fibers of the Achilles tendon complex just proximal to its insertion on the inferior facet (arrow). c) Coronal PD MRI of the ankle (same patient) shows a corrugated and wavy morphology of the medial gastrocnemius myotendinous junction confirming isolated medial gastrocnemius tear (arrow). Note the normal intact morphology of the soleus muscle (thick arrow).
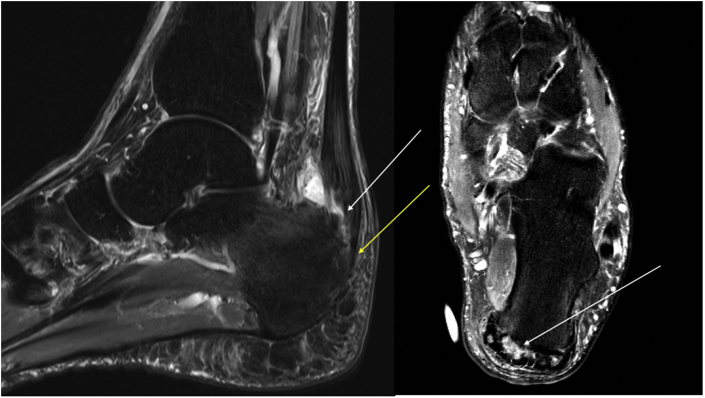
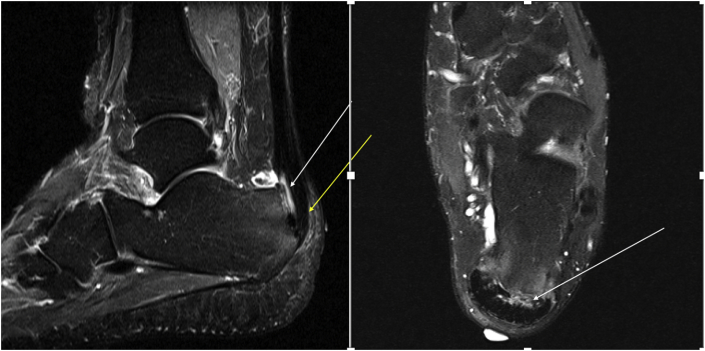
We can also see partial thickness tearing of the soleus tendon at its insertion on the lateral aspect of the middle calcaneal facet with an intact medial gastrocnemius complex (Fig. 8).
Fig. 8.
Sagittal STIR and axial PD FS MRI of the ankle demonstrates partial thickness tearing of the soleus tendon at its insertion on the lateral aspect of the middle calcaneal facet (white arrow). Note the intact medial gastrocnemius tendon at its insertion on the inferior calcaneal facet (yellow arrow).
4. Insertional achilles tendinopathy
Insertional tendinopathy, including insertional tears, can occur in the young and athletic, however it is commonly seen in the elderly obese population.17, 18, 19 Some studies have shown a correlation between Achilles tendon insertional injuries and systemic vasculopathies such as diabetes and hypertension.19,20 The etiology of why this sustains this specific type of tear is still unknown. There are some studies that assert that this is neither a degenerative process but a combined inflammatory and degenerative process.20, 21, 22 This phenomenon has been studied histologically.23
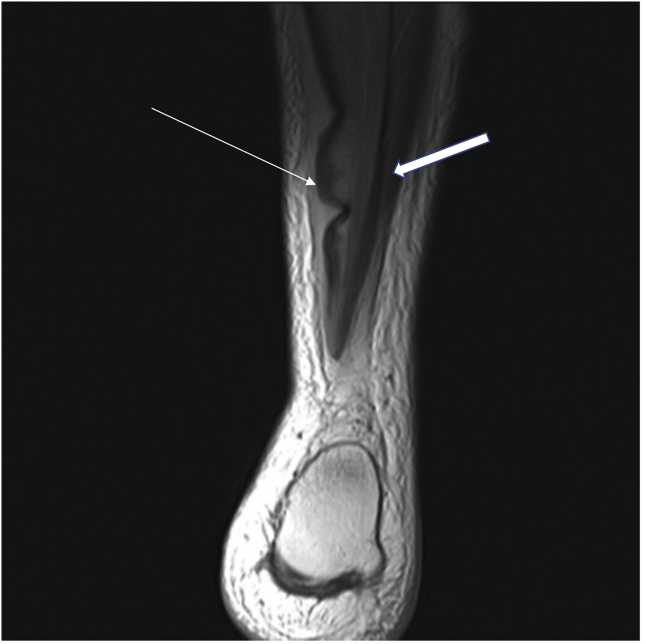
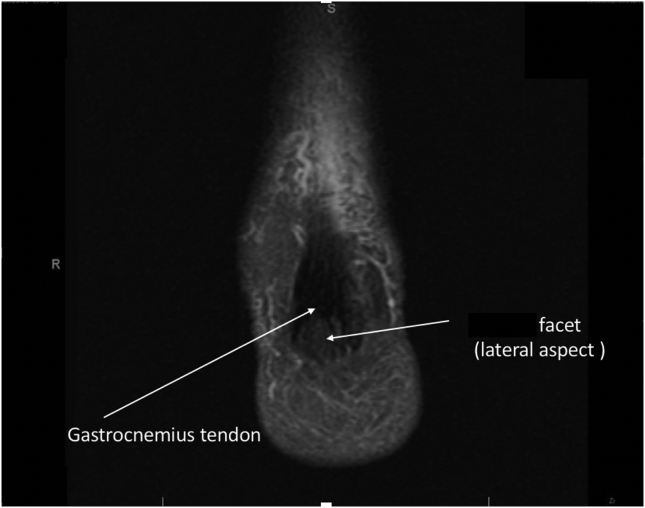
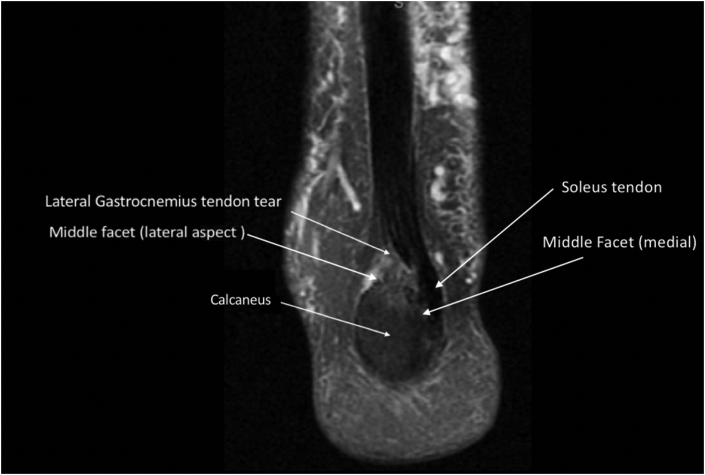
Of the Achilles tendon insertion tears reviewed, the most common sub-tendon injured was the lateral gastrocnemius as it inserts on the lateral aspect of the middle facet of the calcaneal tuberosity (Fig. 9, Fig. 10, Fig. 11, Fig. 12). This injury occurs at the sub-tendon footprints of the middle facet of the calcaneus. This injury spares the medial gastrocnemius sub tendon that inserts on the inferior calcaneal facet. Some studies assert that the tenuous blood supply of the lateral gastrocnemius tendon and its relative hypo-vascularity when compared to other regions of the Achilles tendon are the reasons why it is more prone to injury. Whatever, the cause of the increased incidence of this injury pattern further study of mechanism of injury and biomechanical strength of the individual sub-tendons warrants further study.
Fig. 9.
PDFS transverse of Left foot: Achilles tendon partial thickness sub-tendon tears at footprint of the middle facet.
Fig. 10.
PDFS coronal of an ankle demonstrates an intact medial gastrocnemius tendon inserting on inferior facet of calcaneus.
Fig. 11.
PDFS coronal of an ankle shows a partial thickness tear of the lateral gastrocnemius sub-tendon at its insertion on the lateral aspect of the middle facet of the calcaneus.
Fig. 12.
Sagittal STIR and axial PD FS MRI of the ankle demonstrates partial thickness tearing of the lateral gastrocnemius insertion at the lateral aspect of the middle calcaneal facet (white arrows). Note the intact medial gastrocnemius tendon insertion on the inferior facet (yellow arrow).
5. Operative management
Patients with insertional Achilles tendon tear that are symptomatic and failed conservative treatment 3–6 months from onset of symptoms are often candidates for surgical repair.24 Surgical repair always consists of a thorough debridement of the area after which several fixation techniques can be used. Tacking down the torn tendon with suture anchors to the calcaneus is performed if the tendon is salvageable. Sometimes a double row anchor repair may be performed. Many surgeons report better outcomes, earlier return to weight bearing, and increased biomechanical strength with repair.24
While direct repair without augmentation is preferred, patients with chronical insertional tendinopathy often require Achilles reconstruction once debridement has removed greater than 50% of the native tendon.25 Several techniques have been used, however using the flexor hallicus longus (FHL) tendon has been shown to be the most reproducible and reliable technique amongst surgeons. In the case of insertional reattachment using the FHL tendon, the tendon is completely removed from the calcaneus allowing proper debridement. In this case, a second anchor can be inserted in the center of the posterior surface of the calcaneal tuberosity, just at the footprint of the Achilles tendon. This study also concluded that using the FHL tendon results in good clinical outcomes with limited donor site morbidity.26
6. Conclusion
The Achilles tendon is formed from the confluence of the soleus and gastrocnemius muscles, with individual fascicles inserting into the middle and inferior calcaneal facets. The middle facet serves as an attachment for the soleus and lateral gastrocnemius fascicles, whereas the inferior facet is the primary insertion of the medial gastrocnemius component. The spiraling of the Achilles tendon as well as the torsional stress each sub-tendon is under due to this spiraling could possible explain the mechanism of certain Achilles tendon partial thickness insertional tears.
Knowledge of the Achilles insertional footprint and the calcaneal facet anatomy provides a better understanding of insertional pathologies of the Achilles tendon complex. This understanding of the anatomical structure allows improved understanding of the individual biomechanics of each tear, as well as providing improved surgical planning to ensure appropriate repair or reconstruction.
Conflicts of interest and source of funding
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. There are no relevant disclosures.
All authors significantly contributed to the document and have reviewed the final manuscript.
References
- 1.Ballal M.S., Walker C.R., Molloy A.P. The anatomical footprint of the Achilles tendon: a cadaveric study. Bone Joint Lett J. 2014;96-B(10):1344–1348. doi: 10.1302/0301-620X.96B10.33771. [DOI] [PubMed] [Google Scholar]
- 2.Anson B.J., McVay C.B. Surgical Anatomy. fifth ed. WB Saunders Company; Philadelphia: 1971. pp. 1186–1189. [Google Scholar]
- 3.Wood Jones F. Bailliere, Tindall and Cox; London: 1944. Structure and Function as Seen in the Foot; pp. 124–133. [Google Scholar]
- 4.Szaro P., Witkowski G., Smigielski R., Krajewski P., Ciszek B. Fascicles of the adult human Achilles tendon: an anatomical study. Ann Anat. 2009;191:586–593. doi: 10.1016/j.aanat.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Edama M., Kubo M., Onishi H. Structure of the Achilles tendon at the insertion on the calcaneal tuberosity. J Anat. 2016;229(5):610–614. doi: 10.1111/joa.12514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pękala P.A., Henry B.M., Ochała A. The twisted structure of the Achilles tendon unraveled: a detailed quantitative and qualitative anatomical investigation. Scand J Med Sci Sports. 2017;27(12):1705–1715. doi: 10.1111/sms.12835. [DOI] [PubMed] [Google Scholar]
- 7.Del Buono A., Chan O., Maffulli N. Achilles tendon: functional anatomy and novel emerging models of imaging classification. Int Orthop. 2013 Apr;37(4):715–721. doi: 10.1007/s00264-012-1743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doral M.N., Alam M., Bozkurt M. Functional anatomy of the Achilles tendon. Knee Surg Sport Traumatol Arthrosc. 2010;18:638–643. doi: 10.1007/s00167-010-1083-7. [DOI] [PubMed] [Google Scholar]
- 9.Edama M., Kubo M., Onishi H. Structure of the Achilles tendon at the insertion on the calcaneal tuberosity. J Anat. 2016;229:610–614. doi: 10.1111/joa.12514. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kachlik D., Baca V., Cepelik M., Hajek P., Mandys V., Musil V. Clinical anatomy of the calcaneal tuberosity. Ann Anat. 2008;190:284–291. doi: 10.1016/j.aanat.2008.02.001. PubMed PMID: 18417333. [DOI] [PubMed] [Google Scholar]
- 11.Pierre-jerome C., Moncayo V., Terk M.R. MRI of the Achilles tendon: a comprehensive review of the anatomy, biomechanics, and imaging of overuse tendinopathies. Acta Radiol. 2010;51(4):438–454. doi: 10.3109/02841851003627809. [DOI] [PubMed] [Google Scholar]
- 12.Read J.W., Peduto A.J. Tendon imaging. Sports Med Arthrosc Rev. 2000;8:32–55. [Google Scholar]
- 13.Millar A.P. Strains of the posterior calf musculature (tennis leg) Am J Sports Med. 1979;7:172–174. doi: 10.1177/036354657900700306. [DOI] [PubMed] [Google Scholar]
- 14.Miller W.A. Rupture of the musculotendinous juncture of the medial head of the gastrocnemius muscle. Am J Sports Med. 1977;5:191–193. doi: 10.1177/036354657700500505. [DOI] [PubMed] [Google Scholar]
- 15.Brewer B.J. Mechanism of injury to the musculotendinous unit: instructional lecture. Am Acad Orthop Surg. 1960;17:354–358. [Google Scholar]
- 16.Stauber W.T. Eccentric action of muscles: physiology, injury and adaptation. Exerc Sport Sci Rev. 1989;17:157–185. [PubMed] [Google Scholar]
- 17.Clement D.B., Taunton J.E., Smart G.W. Achilles tendinitis and peritendinitis: etiology and treatment. Am J Sports Med. 1984;12:179–184. doi: 10.1177/036354658401200301. [DOI] [PubMed] [Google Scholar]
- 18.Kvist M. Achilles tendon injuries in athletes. Ann Chir Gynaecol. 1991;80:188–201. [PubMed] [Google Scholar]
- 19.Holmes G.B., Lin J. Etiologic factors associated with symptomatic achilles tendinopathy. Foot Ankle Int. 2006;27:952–959. doi: 10.1177/107110070602701115. [DOI] [PubMed] [Google Scholar]
- 20.Irwin T.A. Current concepts review: insertional Achilles tendinopathy. Foot Ankle Int. 2010;31:933–939. doi: 10.3113/FAI.2010.0933. [DOI] [PubMed] [Google Scholar]
- 21.Zanetti M., Metzdorf A., Kundert H.P. Achilles tendons: clinical relevance of neovascularization diagnosed with power doppler US. Radiology. 2003;227:556–560. doi: 10.1148/radiol.2272012069. [DOI] [PubMed] [Google Scholar]
- 22.Knobloch K., Kraemer R., Lichtenberg A. Achilles tendon and paratendon microcirculation in midportion and insertional tendinopathy in athletes. Am J Sports Med. 2006;34:92–97. doi: 10.1177/0363546505278705. [DOI] [PubMed] [Google Scholar]
- 23.Rufai A., Ralphs J.R., Benjamin M. Structure and histopathology of the insertional region of the human Achilles tendon. J Orthop Res. 1995;13:585–593. doi: 10.1002/jor.1100130414. [DOI] [PubMed] [Google Scholar]
- 24.Shakked R.J., Raikin S.M. Insertional tendinopathy of the achilles: debridement, primary repair and when to augment. Foot Ankle Clin. 2017;22(4):761–780. doi: 10.1016/j.fcl.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Kolodziej P., Glisson R.R., Nunley J.A. Risk of avulsion of the Achilles tendon after partial excision for treatment of insertional tendonitis and Haglund's deformity: a biomechanical study. Kolodziej P1, Glisson RR, Nunley JA. Foot Ankle Int. 1999 Jul;20(7):433–437. doi: 10.1177/107110079902000707. [DOI] [PubMed] [Google Scholar]
- 26.De Cesar Netto C., Chinanuvathana A., Fonseca L.F.D., Dein E.J., Tan E.W., Schon L.C. Outcomes of flexor digitorum longus (FDL) tendon transfer in the treatment of Achilles tendon disorders. Foot Ankle Surg. 2017 Dec 19;25(3):303–309. doi: 10.1016/j.fas.2017.12.003. [DOI] [PubMed] [Google Scholar]