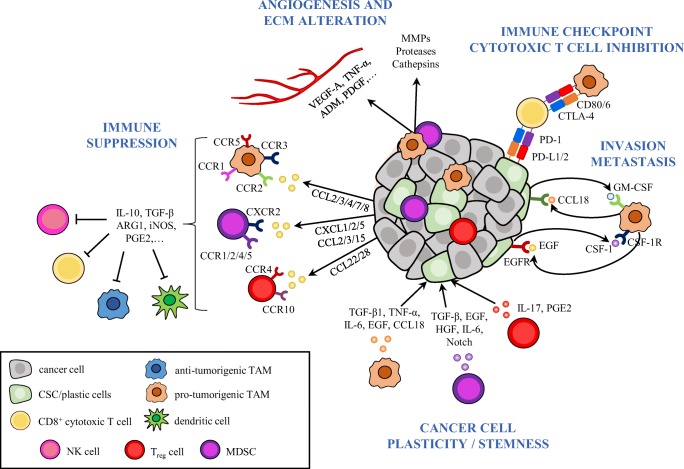
Fig. 1.
The tumor-immunosuppressive network limits cytotoxic immune-cell responses to cancer cells and promotes cancer-cell plasticity. This schema illustrates some of the mechanisms evolved by tumors to block cytotoxic immune cell responses and to promote tumor progression and metastasis. Immune cells, such as TAMs, MDSCs, and Treg cells are recruited into the tumor and become educated by cancer (stem) cell-derived cytokines and chemokines to acquire pro-tumorigenic functions. These cancer and tumor-infiltrating immune cells disrupt immune surveillance through multiple mechanisms, including inhibition of antigen presentation by DCs, T cell proliferation, M1 macrophage polarization and NK-cell cytotoxicity. In addition, cancer cells and immunosuppressive TAMs inhibit cytotoxic T cell function by activating immune checkpoint pathways. Immunosuppressive cells enhance tumor progression by directly promoting EMT and CSC properties in cancer cells through the secretion of cytokines such as TGF-β, IL-6, EGF, among others, and support invasion and metastasis by secreting a variety of pro-tumorigenic cytokines and growth factors. Paracrine signal loops between CSCs and TAMs have been described, which enhance cancer-cell plasticity, immunosuppression and tumor progression. Hence, CSC-derived CSF-1 and GM-CSF promote TAM activation and, in turn, macrophage-derived EGF or CCL18 induce EMT, CSC state, and tumor cell invasion. Finally, immunosuppressive TAMs and MDSCs produce pro-angiogenic factors such as VEGF, TNF-α, ADM, PDGF, among others, to promote angiogenesis, or secrete MMPs, serine proteases, and cathepsins, leading to ECM alterations. MDSC, myeloid-derived suppressor cell; NK, natural killer; TAM, tumor-associated macrophage; Treg, regulatory T cells