Abstract
Background:
High tibial osteotomy (HTO) was developed to treat early medial compartment osteoarthritis in varus knees.
Purpose:
To evaluate the midterm and long-term outcomes of HTO in a large population-based cohort of patients.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
Data from the California Office of Statewide Health Planning and Development were used to identify patients undergoing HTO from 2000 to 2014. Patients with infectious arthritis, rheumatological disease, congenital deformities, malignancy, concurrent arthroplasty, or skeletal trauma were excluded. Demographic information was assessed for every patient. Failure was defined as conversion to total or unicompartmental knee arthroplasty. Differences between patients requiring arthroplasty and those who did not were identified using univariate analysis. Multivariate analysis was performed, and Kaplan-Meier survivorship estimates for 5- and 10-year survival were computed.
Results:
A total of 1576 procedures were identified between 2000 and 2014; of these, 358 procedures were converted to arthroplasty within 10 years. Patients who went on to arthroplasty after HTO were older (48.23 ± 6.76 vs 42.66 ± 9.80 years, respectively; P < .001), had a higher incidence of hypertension (25.42% vs 17.82%, respectively; P = .001), and had a higher likelihood of having ≥1 comorbidity (38.0% vs 31.4%, respectively; P = .044). Patients were 8% more likely to require arthroplasty for each additional year in age (relative risk [RR], 1.08). Female patients were also at an increased risk of conversion to arthroplasty compared with male patients (RR, 1.38). Survivorship at 5 and 10 years was 80% and 56%, respectively, and the median time to failure was 5.1 years.
Conclusion:
HTO may provide long-term survival in select patients. Careful consideration should be given to patient age, sex, and osteoarthritis of the knee when selecting patients for this procedure.
Keywords: knee, osteotomy, varus, malalignment
High tibial osteotomy (HTO) was developed as a joint-preserving surgical procedure to treat young patients with isolated medial or lateral compartment arthritis of the knee and corresponding varus or valgus malalignment of the lower extremity.9 The procedure is carried out in patients with good or minimally reduced knee range of motion in whom nonoperative measures have failed to improve disabling knee pain. When joint-preserving measures fail, total or unicompartmental knee arthroplasty (TKA or UKA, respectively) has grown in popularity as a treatment option for severe knee osteoarthritis (OA). Consequently, knee arthroplasty may serve a complementary role to HTO in treating patients with advanced disease. However, there may still be significant overlap in the patient population meeting indications for either HTO or knee arthroplasty, particularly for unicompartmental disease or in knees with less severe OA.
The increased utilization of UKA and TKA has resulted in a decline in the frequency of tibial osteotomy.1,5,6,17,24 For younger patients, however, the risk of prosthesis loosening and polyethylene wear after knee arthroplasty must be considered because these implants may be subjected to greater mechanical stress over a longer period of time compared with those in elderly patients.11 Recent literature12 also suggests that HTO may be more cost-effective than knee arthroplasty in patients aged 50 to 60 years.
Although some studies1,5,13,19 report greater than 90% survivorship at 10 years from surgery, risk factors such as increasing age and severity of OA have repeatedly been shown to reduce survivorship after HTO. More research is needed to better establish guidelines for appropriate patient selection for HTO. The purpose of this study was to evaluate the midterm and long-term outcomes of HTO in a large population-based cohort of patients.
Methods
Data from the California Office of Statewide Health Planning and Development (OSHPD), a mandatory statewide discharge database, were utilized for this study. This database contains data from all public and private inpatient hospitals, ambulatory surgery centers, and emergency departments in the state of California. It includes demographic data for each patient, such as age, sex, race, total hospital charges, and up to 25 medical diagnoses with each admission. Diagnosis and procedure codes are listed as International Classification of Diseases, Ninth Revision (ICD-9) and Current Procedural Terminology (CPT) billing codes. Patients are tagged with a unique record linkage number that remains consistent throughout all admissions within the state of California.
HTO procedures were identified by flagging any admission containing ICD-9 procedure code 77.27 and CPT codes 27705, 27709, and 27457. Patients with lower extremity trauma, infectious arthritis, rheumatological disease, congenital deformities, malignancy, or concurrent arthroplasty were excluded. A full list of inclusion and exclusion codes is provided in Appendix Table A1. While laterality cannot be determined directly from the database, concurrent diagnosis and procedure codes were reviewed for all patients with 2 qualifying osteotomy procedures to determine whether the second HTO was a revision or contralateral procedure. This methodology is similar to what has been conducted in other database studies of this type.4,23
Failure was defined as conversion to TKA or UKA, and the cohort was stratified based on whether each patient went on to fail. For the purposes of this study, conversion to TKA or UKA was combined into a single outcome as “conversion to arthroplasty.” Age, sex, race, diagnosis group (OA, acquired genu varum, other acquired deformity, derangement of internal knee structures, osteochondral defects, traumatic arthritis, and other arthropathy), concurrent procedures (arthroscopic surgery, osteochondral graft, synovectomy, and meniscectomy), and comorbidities (asthma, chronic kidney disease, congestive heart failure, depression, diabetes mellitus, hypertension, obesity, and peripheral vascular disease) were assessed for each admission. The grade of OA in each knee was not available through the OSHPD. Obesity was based on an ICD-9 diagnosis code (Appendix Table A1) and was calculated based on body mass index, which was also not directly available in this database. Subsequent readmissions to an inpatient hospital, ambulatory surgery center, or emergency department in California after the index procedure were identified and sequenced using the record linkage number and discharge or service dates.
Total reoperation rates were identified and summarized. Statistically significant differences between patients who required arthroplasty and those who did not were identified using the Student t test and chi-square test. Multinomial logistic regression was constructed using variables with P < .2 in the univariate analysis. To check for confounding, variables were individually dropped from the model, and the new model was then compared with the original model. Any variable that was found to cause more than a 15% change in another variable was considered a confounder and removed from the final model. A Hosmer-Lemeshow goodness-of-fit test was used to evaluate model fit, which assesses whether the observed event rates match expected event rates in subgroups of the model population.3 Kaplan-Meier survivorship curves were constructed to estimate 5- and 10-year survival. If a patient underwent multiple revisions, only the time to initial arthroplasty was included in the analysis. Statistical significance was set at P < .05. All statistical analyses were performed using Stata/MP 13.1 software (StataCorp).
Results
Patient Characteristics
After exclusions, 1576 procedures were identified between the years 2000 and 2014 (Table 1). Within the identified cohort, 44 patients underwent bilateral procedures. A total of 358 procedures (23%) were converted to arthroplasty within the time period investigated (2000-2014). On univariate analysis, patients who went on to arthroplasty after HTO tended to be older at the time of osteotomy (48.23 ± 6.76 vs 42.66 ± 9.80 years, respectively; P < .001), with a higher incidence of hypertension (25.42% vs 17.82%, respectively; P = .001) and a higher likelihood of having ≥1 comorbidity (38.0% vs 31.4%, respectively; P = .044) compared with those who did not. Those patients who converted to arthroplasty were also more likely to have a diagnosis of OA (81.6% vs 58.3%, respectively; P < .001) and genu varum (20.7% vs 14.0%, respectively; P = .002) at the time of their osteotomy procedure. Yet, patients undergoing arthroplasty were less likely to have a diagnosis of any other acquired deformity (13.7% vs 20.8%, respectively; P = .003) or other arthropathy (7.5% vs 13.1%, respectively; P = .004). Other patient characteristics can be found in detail in Table 1.
TABLE 1.
Patient Demographic Informationa
| Total Cohort (N = 1576) | Arthroplasty (n = 358) | No Arthroplasty (n = 1218) | P Value | |
|---|---|---|---|---|
| Age, mean ± SD, y | 43.93 ± 9.49 | 48.23 ± 6.76 | 42.66 ± 9.80 | <.001 |
| Sex | .067 | |||
| Male | 1092 (69.29) | 234 (65.36) | 858 (70.44) | |
| Female | 484 (30.71) | 124 (34.64) | 360 (29.56) | |
| Race | <.001 | |||
| White | 972 (61.68) | 228 (63.69) | 744 (61.08) | |
| Black | 92 (5.84) | 16 (4.47) | 76 (6.24) | |
| Hispanic | 248 (15.74) | 40 (11.17) | 208 (17.08) | |
| Asian | 48 (3.05) | 7 (1.96) | 41 (3.37) | |
| Other | 41 (2.60) | 4 (1.12) | 37 (3.04) | |
| Missing | 175 (11.10) | 63 (17.60) | 112 (9.20) | |
| Primary health insurance | <.001 | |||
| Medicare | 44 (2.79) | 15 (4.19) | 29 (2.38) | |
| Medi-Cal | 50 (3.17) | 9 (2.51) | 41 (3.37) | |
| Private | 973 (61.74) | 247 (68.99) | 726 (59.61) | |
| Workers’ compensation | 318 (20.18) | 78 (21.79) | 240 (19.70) | |
| Self-pay | 10 (0.63) | 2 (0.56) | 8 (0.66) | |
| Other payer | 44 (2.79) | 3 (0.84) | 41 (3.37) | |
| Missing | 137 (8.69) | 4 (1.12) | 133 (10.92) | |
| Comorbidities | ||||
| Obesity | 191 (12.12) | 44 (12.29) | 147 (12.07) | .910 |
| Hypertension | 308 (19.54) | 91 (25.42) | 217 (17.82) | .001 |
| Diabetes mellitus | 80 (5.08) | 19 (5.31) | 61 (5.01) | .821 |
| Depression | 67 (4.25) | 15 (4.19) | 52 (4.27) | .948 |
| Asthma | 94 (5.96) | 29 (8.10) | 65 (5.34) | .052 |
| Chronic kidney disease | 3 (0.19) | 0 (0.00) | 3 (0.25) | >.999 |
| Congestive heart failure | 2 (0.13) | 1 (0.28) | 1 (0.08) | .403 |
| Peripheral vascular disease | 2 (0.13) | 1 (0.28) | 1 (0.08) | .403 |
| No. of comorbidities | .044 | |||
| None | 1058 (67.13) | 222 (62.01) | 836 (68.64) | |
| 1 | 336 (21.32) | 89 (24.86) | 247 (20.28) | |
| 2 | 142 (9.01) | 34 (9.50) | 108 (8.87) | |
| 3 | 33 (2.09) | 9 (2.51) | 24 (1.97) | |
| 4 | 7 (0.44) | 4 (1.12) | 3 (0.25) | |
| Diagnosis category | ||||
| Osteoarthritis | 1002 (63.58) | 292 (81.56) | 710 (58.29) | <.001 |
| Other acquired deformity | 302 (19.16) | 49 (13.69) | 253 (20.77) | .003 |
| Derangement of internal structures | 465 (29.51) | 96 (26.82) | 369 (30.30) | .204 |
| Osteochondral defect | 324 (20.56) | 68 (18.99) | 256 (21.02) | .405 |
| Traumatic arthropathy | 37 (2.35) | 8 (2.23) | 29 (2.38) | .872 |
| Other arthropathy | 187 (11.87) | 27 (7.54) | 160 (13.14) | .004 |
| Concurrent procedure | ||||
| Arthroscopic surgery | 400 (25.38) | 76 (21.23) | 324 (26.60) | .040 |
| Osteochondral graft | 15 (0.95) | 3 (0.84) | 12 (0.99) | >.999 |
| Synovectomy | 84 (5.33) | 11 (3.07) | 73 (5.99) | .031 |
| Meniscectomy | 354 (22.46) | 76 (21.23) | 278 (22.82) | .525 |
| Chondroplasty or microfracture | 78 (4.95) | 7 (1.96) | 71 (5.83) | .003 |
aData are reported as n (%) unless otherwise indicated. Bolded P values indicate statistically significant difference between the arthroplasty and no arthroplasty groups (P < .05).
Risk Factors
After controlling for potential confounders identified on univariate analysis, patients were 8% more likely to require arthroplasty for each additional year in age (relative risk [RR], 1.08 [95% CI, 1.06-1.10]). Female patients were also at an increased risk of conversion to arthroplasty compared with male patients (RR, 1.38 [95% CI, 1.06-1.79]). In contrast, those who underwent simultaneous arthroscopic surgery (RR, 0.74 [95% CI, 0.55-1.00]) or synovectomy (RR, 0.50 [95% CI, 0.25-0.96]) were at a decreased risk of conversion to arthroplasty. The Hosmer-Lemeshow goodness-of-fit test indicated a good model fit (P > .05). Risk factor analysis is presented in detail in Table 2.
TABLE 2.
Adjusted Risk Factors for Conversion to Arthroplasty After High Tibial Osteotomya
| Relative Risk (95% CI) | P Value | |
|---|---|---|
| Age | 1.08 (1.06-1.10) | <.001 |
| Female sex (reference: male) | 1.38 (1.06-1.79) | .017 |
| Osteoarthritis | 2.40 (1.78-3.25) | <.001 |
| No. of comorbidities | 1.00 (0.86-1.17) | .986 |
| Arthroscopic surgery | 0.74 (0.55-1.00) | .048 |
| Synovectomy | 0.50 (0.25-0.96) | .038 |
aBolded P values indicate statistical significance (P < .05).
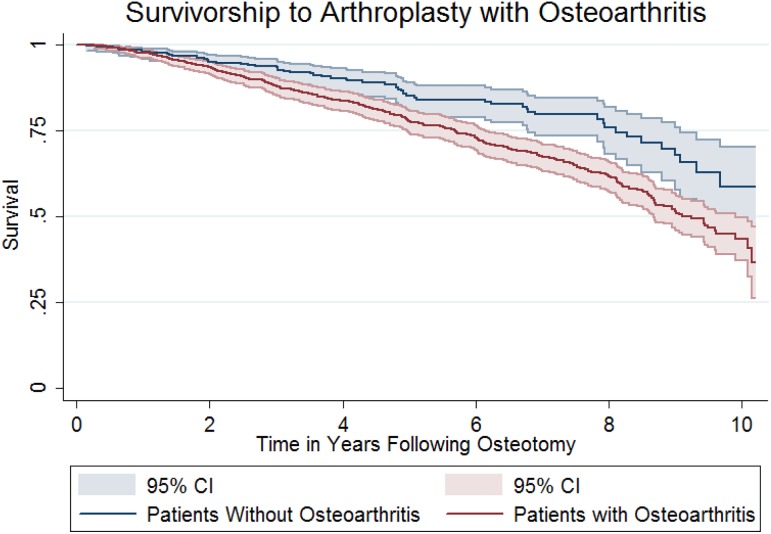
Survivorship
The mean follow-up during the study period was 4.5 years (range, 0-15 years). Overall survivorship at 5 and 10 years was 80% and 56%, respectively, and the median time to failure was 5.1 years (range, 0.15-14.5 years) (Figure 1).
Figure 1.
Kaplan-Meier survival estimate for survivorship to knee arthroplasty after high tibial osteotomy.
In patients with OA (n = 1002), survivorship at 5 and 10 years was 78% and 52%, respectively, and the median time to failure was 5.5 years (range, 0.27-14.5 years) (Figure 2). In patients without OA (n = 574), survivorship at 5 and 10 years was 85% and 67%, respectively, and the median time to failure was 4.9 years (range, 0.16-13.6 years) (Figure 2). The rate of conversion to total hip arthroplasty in patients without OA was 12%.
Figure 2.
Kaplan-Meier survival estimate for survivorship to knee arthroplasty after high tibial osteotomy for patients with and without osteoarthritis.
Discussion
HTO in a large database cohort of patients revealed overall survival rates similar to those of prior studies.13,16,22 Although a diagnosis of OA was the strongest risk factor for conversion to arthroplasty, increasing age and female sex were also found to be risk factors on multivariate analysis. Concomitant procedures such as synovectomy and arthroscopic surgery were associated with lower rates of conversion to arthroplasty, whereas patient factors such as number of comorbidities and race did not affect outcomes.
The 5-year survival rate of 80% and 10-year survival rate of 56% are within the range of published survival rates, although on the lower end. In our study, patients who converted to hip arthroplasty were significantly older than those who did not undergo arthroplasty. However, further analysis to control for potential confounding variables showed that patients were 8% more likely to require arthroplasty for each additional year in age. The discrepancy in the survival rates with previous studies may be because the mean follow-up time was just 4.5 years, with only about half our patient cohort having 5- to 10-year follow-up. Studies with at least 10-year follow-up report 5-year survival rates from 73% to 99% and 10-year survival rates from 51% to 98%, with the average time to revision between 6 and 13 years. The differences in the current data may in part be caused by the age of the cohort and the prevalence of OA, which prior studies have found to be risk factors for failure.5,6,8,15,16,22 In the subgroup of patients without OA, the median age was 41 years (range, 18-60 years), and the 5- and 10-year survival rates were 85% and 67%, respectively. Additionally, 12% of patients in this group were converted to arthroplasty, which is in agreement with results published by Flecher et al5 and Koshino et al.13
Several prior studies have demonstrated that increasing severity of OA leads to shorter survival times after HTO. A study by van Raaij et al22 found 10-year survival rates of 90% in patients with Ahlback grade ≤1 compared with 62% in patients with grade ≥2. Flecher et al5 found that patients with Ahlback grade 1 or 2 OA had significantly lower failure rates with a hazard ratio of 0.29. In contrast, DeMeo et al2 performed HTO in 20 patients with Outerbridge grade 4 OA and found a 25% rate of conversion to arthroplasty at an average of 6.6 years. The current data were obtained from a large database with defined variables, and it was therefore impossible to grade the severity of OA for patients. However, it is reasonable to assume that patients without a diagnosis of OA had at most Ahlback grade 1 OA (ie, joint space narrowing without obliteration of the joint), making it an appropriate surrogate. Of note, the high prevalence of concomitant OA accompanying genu varum in the general population makes it difficult to determine the differential effects of genu varum versus OA in our sample of patients.
Increasing patient age has also been correlated with higher failure rates after HTO in multiple studies.5–8,16 Flecher et al5 reported that the failure rate was 2.1 times higher in patients older than 50 years compared with those younger than 30 years. Gstöttner et al6 found a 5% increase in the rate of conversion to TKA with every 1-year increase in the patient’s age. Hui et al8 compared patients younger and older than 50 years and found a hazard ratio of 3.7 in patients older than 50 years. On multivariate analysis, age was a significant predictor of patients undergoing arthroplasty, with an 8% increased risk with every 1-year increase in age. Although it is unclear what age cutoff should be used, a large increase in failure rates tends to occur in the 50- to 60-year-old age group. For patients in older age groups who may be candidates for HTO, other risk factors should also be considered when deciding to operate. Notably, the effect of age on revision compared with that of a preoperative diagnosis of OA is relatively small, and thus, physiological age and disease severity may be better indicators of revision likelihood rather than absolute biological age.
Female sex was found to be associated with a 38% increase in the likelihood of conversion to arthroplasty. In the study by van Raaij et al,22 100 patients were evaluated after closing wedge HTO with an average follow-up of 12 years and survival rates were found to be 59% for female patients and 85% for male patients. Niinimäki et al16 reported on 3195 HTO procedures using a national registry and found poorer survivorship in female patients, with a hazard ratio of 1.26. Although several studies have reported worse survivorship in female patients compared with male patients after HTO, it is unclear why. Sprenger and Doerzbacher21 suggested that the degree of valgus correction may play a role, but further studies are needed to elucidate this finding.
HTO performed simultaneously with cartilage repair or meniscal procedures has shown promising results. Schuster et al20 analyzed 85 patients (91 knees) who underwent HTO with medial femoral condyle debridement. A subset of patients also underwent microfracture as well as partial medial meniscectomy. The authors found a 95% survival rate at 5-year follow-up, with 3 patients converting to UKA and 1 patient converting to TKA. Although all of the patients had Kellgren-Lawrence grade 3 or 4 OA, the average age was 50 years, and this younger age may have contributed to the relatively high survival rate. Pascale et al18 performed a prospective randomized trial comparing HTO alone (20 patients) with HTO with microfracture (20 patients). At 5-year follow-up, no significant difference was found between the study groups, and only 2 patients (5%) converted to TKA. Kahlenberg et al10 in 2017 published a systematic review of 4 studies (839 knees) that evaluated the use of cartilage repair in conjunction with HTO. The most common cartilage technique used was microfracture (22%), and the overall rate of conversion to arthroplasty was 6.8% at a mean of 4.9 to 13 years. Patients who had concurrent osteochondral grafts did not have higher rates of conversion to arthroplasty. Patients who underwent concomitant arthroscopic surgery (25%) or meniscectomy (22%) did not have significantly higher rates of conversion to arthroplasty, further supporting prior literature. A 2018 systematic review and meta-analysis confirmed the major benefit of HTO itself and the negligible benefit of concomitant procedures during HTO on clinical or radiological outcomes.14 However, these concurrent procedures do not appear to be detrimental, and in the case of cartilage repair/restoration procedures, there may be some utility, as they lead to improved arthroscopic, histological, and magnetic resonance imaging findings.
This study is limited by factors inherent in database research, including the potential for sampling bias, the lack of radiographic and clinical data, and errors in data entry and coding. In particular, the OSHPD database does not report functional outcomes of surgery, surgical techniques, patient-reported outcomes, previous surgery at outside institutions or before the study time point, or radiographic analysis of deformity severity or correction. Therefore, it was not possible to determine the severity of OA in our patient population, which has been shown in multiple studies to be a significant predictor of outcomes after HTO. Additionally, there was no opportunity to comment on preoperative and postoperative coronal alignment, another important factor in HTO survival, or to report on patient outcomes or indications for conversion to arthroplasty. Finally, it was not possible to quantify clinical failures that forgo further surgical intervention, and thus, the true failure incidence is likely underreported in the present study.
The greatest strength of this study is the large number of patients who underwent HTO with midterm to long-term follow-up from a data source that captures all patients, procedures, and admissions within the state of California. The all-inclusive nature of this database limits sampling bias inherent in other databases. The current study also presents clinically meaningful data with regard to the primary endpoint of conversion to arthroplasty. These findings may provide data for further cost analysis studies, as they report on a population of 38 million people. These data may also be used to guide clinical decision making as well as to counsel patients on the risk factors of conversion to arthroplasty after HTO.
Conclusion
HTO may provide long-term survival in select patients. Careful consideration should be given to patient age, sex, and OA of the knee when selecting patients for this procedure.
Appendix
TABLE A1.
Inclusion and Exclusion Codesa
| Code | |
|---|---|
| Inclusion procedures | |
| CPT | |
| Osteotomy, tibia | 27705 |
| 27709 | |
| 27457 | |
| ICD-9 | |
| Wedge osteotomy, tibia | 77.27 |
| Inclusion diagnoses | |
| ICD-9 | |
| Osteoarthritis | 715.00-715.98 |
| Genu varum | 736.42 |
| Other acquired deformity | 736.41 |
| 736.5-736.9 | |
| 738.8-738.9 | |
| Derangement of internal structures | 717.0-717.9 |
| Osteochondral defect | 717.7 |
| 718.05-718.09 | |
| 733.92 | |
| Traumatic arthritis | 716.10-716.19 |
| Other arthritis | 716.50-716.99 |
| 718.80-718.99 | |
| 719.80-719.99 | |
| Exclusion procedures: prior or index admission | |
| CPT | |
| Hip arthroplasty | 27125-27138 |
| Knee arthroplasty | 27440-27488 |
| Ankle arthroplasty | 27702-27003 |
| 27870-27871 | |
| ICD-9 | |
| Hip arthroplasty | 00.70-00.77 |
| 81.51-81.53 | |
| Knee arthroplasty | 00.80-00.84 |
| 81.54-81.55 | |
| Ankle arthroplasty | 81.56 |
| Open reduction of fracture, with internal fixation | 79.35 |
| Ankle fusion | 81.11 |
| Exclusion diagnoses: prior or index admission | |
| ICD-9 | |
| Poliomyelitis | 138 |
| Neoplasm | 170.6-170.9 |
| 171.3-171.9 | |
| 173.7 | |
| 195.5-195.8 | |
| 196.5-196.9 | |
| 198.5 | |
| 203.00-203.82 | |
| 213.7 | |
| 238.0 | |
| Rickets | 268.0-268.1 |
| Mucopolysaccharidosis | 277.5 |
| Developmental delay | 315.8-315.9 |
| 783.40 | |
| Intellectual disability | 318.0-318.2 |
| 319 | |
| Hereditary spastic paraplegia | 334.1 |
| Cerebral palsy | 343.0-343.9 |
| Paraplegia and quadriplegia | 344.01 |
| 344.1 | |
| Infective arthritis | 711.00-711.99 |
| Pressure ulcer | 707.0-707.09 |
| Rheumatological disease | 710.0-710.2 |
| 714.0-714.9 | |
| 720.0 | |
| Dislocation | 718.20-718.76 |
| Soft tissue infection | 682.6 |
| 728.0 | |
| 728.86 | |
| Osteomyelitis | 730.00-730.99 |
| Osteitis deformans | 731.0-731.1 |
| Osteochondropathy | 732.1-732.9 |
| Pathological fracture | 733.10-733.19 |
| Bone cyst | 733.20-733.29 |
| Aseptic necrosis | 733.42 |
| Malunion of fracture | 733.81 |
| Nonunion of fracture | 733.82 |
| Spina bifida | 741.00-741.93 |
| Congenital deformity | 754.30-754.44 |
| 755.30-755.69 | |
| Other congenital anomalies | 756.4-756.9 |
| Lower extremity trauma | 808.0-808.9 |
| 820.00-821.39 | |
| 823.00-823.92 | |
| 827.0-828.1 | |
| 835.00-835.13 | |
| 836.0-836.69 | |
| 905.4-905.4 | |
| Complication of orthopaedic device | 996.4-996.49 |
| 996.66-996.67 | |
| 996.77-996.78 | |
| Joint replacement status and care | V43.64-V43.65 |
| V54.81-V54.82 | |
| Arthrodesis status | V45.5 |
| Care for internal fixation device | V54.01-V54.09 |
| Outcome procedure | |
| CPT | |
| Knee arthroplasty | 27440-27447 |
| 27486-27487 | |
| ICD-9 | |
| Knee arthroplasty | 00.80-0082 |
| 81.54-81.55 | |
aCPT, Current Procedural Terminology; ICD-9, International Classification of Diseases, Ninth Revision.
Footnotes
One or more of the authors declared the following potential conflict of interest or source of funding: C.T.V. has received honoraria and consulting fees from Osiris Therapeutics. G.F.H. has received educational support from Arthrex and Micromed and speaking fees from Arthrex. A.E.W. has received educational support from Arthrex and Smith & Nephew and hospitality payments from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H. The long-term outcome of high tibial osteotomy. J Bone Joint Surg Br. 2008;90(5):592–596. [DOI] [PubMed] [Google Scholar]
- 2. DeMeo PJ, Johnson EM, Chiang PP, Flamm AM, Miller MC. Midterm follow-up of opening-wedge high tibial osteotomy. Am J Sports Med. 2010;38(10):2077–2084. [DOI] [PubMed] [Google Scholar]
- 3. Fagerland MW, Hosmer DW. A generalized Hosmer-Lemeshow goodness-of-fit test for multinomial logistic regression models. The Stata Journal. 2012;12(3):447–453. [Google Scholar]
- 4. Farng E, Zingmond D, Krenek L, Soohoo NF. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20(4):557–563. [DOI] [PubMed] [Google Scholar]
- 5. Flecher X, Parratte S, Aubaniac JM, Argenson JN. A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res. 2006;452:91–96. [DOI] [PubMed] [Google Scholar]
- 6. Gstöttner M, Pedross F, Liebensteiner M, Bach C. Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg. 2008;128(1):111–115. [DOI] [PubMed] [Google Scholar]
- 7. Howells NR, Salmon L, Waller A, Scanelli J, Pinczewski LA. The outcome at ten years of lateral closing-wedge high tibial osteotomy. Bone Joint J. 2014;96(11):1491–1497. [DOI] [PubMed] [Google Scholar]
- 8. Hui C, Salmon LJ, Kok A, et al. Long-term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am J Sports Med. 2010;39(1):64–70. [DOI] [PubMed] [Google Scholar]
- 9. Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43(4):746–751. [DOI] [PubMed] [Google Scholar]
- 10. Kahlenberg CA, Nwachukwu BU, Hamid KS, Steinhaus ME, Williams RJ. Analysis of outcomes for high tibial osteotomies performed with cartilage restoration techniques. Arthroscopy. 2017;33(2):486–492. [DOI] [PubMed] [Google Scholar]
- 11. Keeney JA, Eunice S, Pashos G, Wright RW, Clohisy JC. What is the evidence for total knee arthroplasty in young patients? A systematic review of the literature. Clin Orthop Relat Res. 2010;469(2):574–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Konopka JF, Gomoll AH, Thornhill TS, Katz JN, Losina E. The cost-effectiveness of surgical treatment of medial unicompartmental knee osteoarthritis in younger patients. J Bone Joint Surg Am. 2015;97(10):807–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Koshino T, Yoshida T, Ara Y, Saito I, Saito T. Fifteen to twenty-eight years’ follow-up results of high tibial valgus osteotomy for osteoarthritic knee. Knee. 2004;11(6):439–444. [DOI] [PubMed] [Google Scholar]
- 14. Lee OS, Ahn S, Ahn JH, Teo SH, Lee YS. Effectiveness of concurrent procedures during high tibial osteotomy for medial compartment osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2018;138(2):227–236. [DOI] [PubMed] [Google Scholar]
- 15. Naudie D, Bourne RB, Rorabeck CH, Bourne TJ. Survivorship of the high tibial valgus osteotomy: a 10-to 22-year followup study. Clin Orthop Relat Res. 1999;367:18–27. [PubMed] [Google Scholar]
- 16. Niinimäki TT, Eskelinen A, Mann BS, Junnila M, Ohtonen P, Leppilahti J. Survivorship of high tibial osteotomy in the treatment of osteoarthritis of the knee. J Bone Joint Surg Br. 2012;94(11):1517–1521. [DOI] [PubMed] [Google Scholar]
- 17. Papachristou G, Plessas S, Sourlas J, Levidiotis C, Chronopoulos E, Papachristou C. Deterioration of long-term results following high tibial osteotomy in patients under 60 years of age. Int Orthop. 2006;30(5):403–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pascale W, Luraghi S, Perico L, Pascale V. Do microfractures improve high tibial osteotomy outcome? Orthopedics. 2011;34(7):e251–e255. [DOI] [PubMed] [Google Scholar]
- 19. Schallberger A, Jacobi M, Wahl P, Maestretti G, Jakob RP. High tibial valgus osteotomy in unicompartmental medial osteoarthritis of the knee: a retrospective follow-up study over 13-21 years. Knee Surg Sports Traumatol Arthrosc. 2010;19(1):122–127. [DOI] [PubMed] [Google Scholar]
- 20. Schuster P, Schulz M, Mayer P, Schlumberger M, Immendoerfer M, Richter J. Open-wedge high tibial osteotomy and combined abrasion/microfracture in severe medial osteoarthritis and varus malalignment: 5-year results and arthroscopic findings after 2 years. Arthroscopy. 2015;31(7):1279–1288. [DOI] [PubMed] [Google Scholar]
- 21. Sprenger TR, Doerzbacher JF. Tibial osteotomy for the treatment of varus gonarthrosis. J Bone Joint Surg Am. 2003;85(3):469–474. [PubMed] [Google Scholar]
- 22. van Raaij T, Reijman M, Brouwer RW, Jakma TS, Verhaar JN. Survival of closing-wedge high tibial osteotomy: good outcome in men with low-grade osteoarthritis after 10-16 years. Acta Orthop. 2008;79(2):230–234. [DOI] [PubMed] [Google Scholar]
- 23. Villacis D, Sivasundaram L, Pannell WC, Heckmann N, Omid R, Hatch GF., 3rd Complication rate and implant survival for reverse shoulder arthroplasty versus total shoulder arthroplasty: results during the initial 2 years. J Shoulder Elbow Surg. 2016;25(6):927–935. [DOI] [PubMed] [Google Scholar]
- 24. Wright J, Heck D, Hawker G, et al. Rates of tibial osteotomies in Canada and the United States. Clin Orthop Relat Res. 1995;319:266–275. [PubMed] [Google Scholar]