Abstract
Objective
The aim of this systematic review was to present the outcome of Lisfranc joint injuries treated with closed reduction and screw percutaneous fixation.
Methods
We searched in Pubmed and Google Scholar Databases for articles regarding screw percutaneous fixation of Lisfranc injuries. Seven studies in total were found to be compatible to our search, according to PRISMA guidelines. Four of those met the criteria of the review and they were included in the meta-analysis. A total number of 106 patients were separated into five groups according to the type of injury and the mean AOFAS score of each group was calculated. Cases in which percutaneous fixation was converted to open treatment due to poor reduction were not included in the study. In addition we compared the outcome score between types of injury according to Myerson classification as well as between purely ligamentous and osseoligamentous injuries. The characteristics of all seven selected studies, such as kind of screw used for fixation, post operative protocol, complications and outcome are mentioned as well.
Results
Average AOFAS score was 86,2 for type A, 87,54 for type B, and 85 for type C injuries respectively. In pure dislocation group the average AOFAS score was 86,43 and in fracture dislocation group was 87,36. Good to excellent outcome can be expected in patients with different types of injury according to Myerson classification following percutaneous fixation of lisfranc joint injury. Patients with type B injury or a fracture dislocation injury might have better outcome, although this difference was not found to be statistically significant.
Conclusion
Percutaneous fixation of tarsometatarsal joint injuries is a relatively simple and safe method of treatment, leading to a good functional outcome, especially for Myerson type B as well as for fracture dislocation type of injuries, provided that an anatomical reduction has been achieved.
Level of Evidence
Level III, Therapeutic Study.
Keywords: Percutaneous fixation, Lisfranc fracture dislocation, Tarsometatarsal joint, Midfoot trauma, Systematic review
Introduction
Tarsometatarsal (TMT) joint complex injuries are rare, accounting 0,2% to 0,8% of all fractures.1, 2 Incidence of midfoot sprains or subtle Lisfranc disruption though is much higher.3, 4, 5 Up to 20% of these injuries are missed on the initial examination.5 Mechanism of injury can be either direct (high energy blunt trauma), or indirect by an axial or rotational force applied to a plantar flexed foot.1, 5 Thorough clinical examination and bilateral anteroposterior (AP) and true lateral weight bearing (WB) as well as oblique X rays6 are mandatory in order to evaluate properly a midfoot trauma.
Lisfranc joint complex is contained by three columns. The medial column contains the first metatarsal and medial cuneiform. The middle column contains the second, third metatarsal and middle and lateral cuneiform and the lateral one contains the fourth and fifth metatarsal with the cuboid.2 The base of the second metatarsal articulates with the middle cuneiform 8 mm more proximal to the medial cuneiform – first metatarsal joint, forming a mortise, which provides stability to the midfoot.1, 5 Tarsometatarsal ligamentous complex contains three ligaments; dorsal ligament and the stronger plantar oblique and interosseous ligaments. The so called Lisfranc ligament is an interosseous ligament between the medial cuneiform and the base of the 2nd metatarsal. It is stronger compared to the dorsal and plantar oblique ligament.1
Unstable midfoot trauma can be a challenging diagnosis. In subtle Lisfranc dislocation non weight bearing (NWB) X rays may be normal. Plantar ecchymosis1 (Fig. 1), tenderness over the TMT area, pain on abduction stress of the forefoot indicate a possible Lisfranc injury.5, 6 Bilateral weight bearing (WB) AP and lateral radiographs, as well as 30° oblique views are required to evaluate if there is any TMT joint disruption (Fig. 2, Fig. 3).5, 6 The main classification systems used in clinical practice for these injuries are the Hardcastle modified by Myerson7, 8 (type A: complete homolateral disruption, type B: partial incongruity, type C: divergent) and the Nunley and Vertullo9 classification system (stage I: midfoot sprain, no diastasis on the WB X rays, positive bone scintigraphy, stage II: 1 mm–5 mm diastasis between the first and second metatarsal, no arch collapse on the WB X rays, stage III: more than 5 mm diastasis, arch collapse).
Fig. 1.
Foot plantar ecchymosis after a Lisfranc injury.
Fig. 2.

Weight Bearing AP view. First and second metatarsal base widening is noticed.
Fig. 3.
Slight arch collapse on the lateral WB X ray.
Treatment ranges from conservative for midfoot sprains with no displacement on WB radiographs to surgical reduction and internal fixation for Lisfranc joint dislocation and fracture dislocation. Management should always aim to restore the TMT joint complex anatomy.10 Primary partial arthrodesis has been also proposed, mainly for purely ligamentous injuries.11, 12 Open reduction and internal fixation is considered to be the gold standard of treatment for Lisfranc joint dislocations. Closed reduction and percutaneous stable fixation using transarticular screws might be another option, which not much has been reported in the literature so far for.
The aim of the present review is to gather all the existing data regarding TMT joint injuries closed reduction and screw percutaneous fixation and evaluate its effectiveness, safety and clinical outcome. We compared the results of this technique between groups of patients with different type of injury according to Myerson type of injury, as well as between purely ligamentous group and osseoligamentous group of patients. Furthermore we intend to investigate which types of Lisfranc injury are more amenable to percutaneous fixation.
Materials and methods
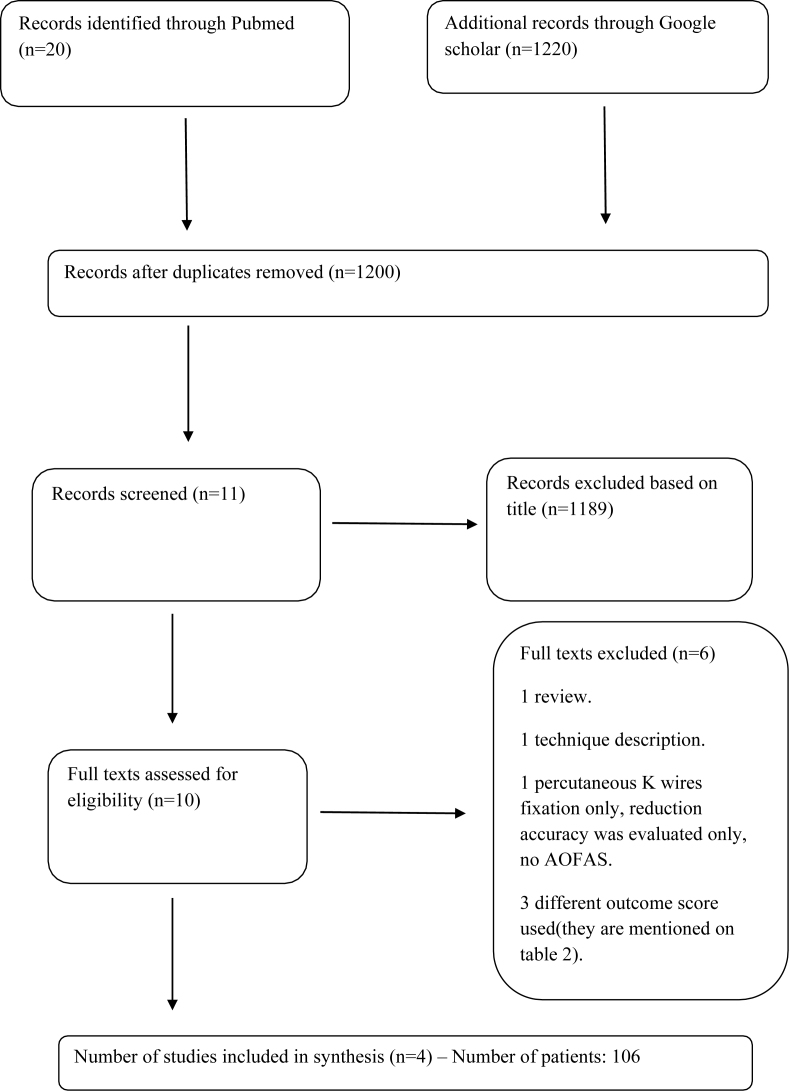
We searched the data in Pubmed and Google Scholar using the keywords ‘Lisfranc joint percutaneous fixation’. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used for the selection of studies which were included in the meta analysis (Fig. 4). Inclusion criteria were: 1. Method of treatment was closed reduction and percutaneous fixation using screws (and not K wires). 2. Functional outcome using AOFAS (American Orthopaedic Foot and Ankle Society) score was reported. 3. The same Myerson classification system was used (Patients with partial incongruity were considered to have type B injury). 4. Full text access. 5. Minimum follow up 6 months. Studies where open reduction was performed or Kirschner wires only were used for fixation were excluded from the meta analysis. In addition studies, where outcome scores other than AOFAS were used, or follow up time was too short, were excluded as well.
Fig. 4.
Searched studies according to PRISMA guidelines.
A total amount of 7 studies were found to present retrospective case series of patients who sustained Lisfranc joint injury and they were treated with screw percutaneous fixation. Number of patients, type of injury, implant of fixation, mean AOFAS score, complications, follow up, postoperative protocol of each study are presented on Table 1. Of those 7 studies, only 4 used the same parameters and they were included in the meta-analysis. A total number of 106 patients were studied and separated in to three groups depending on the type of injury according to the Myerson classification system and into two groups depending on whether the injury was a pure dislocation or a fracture dislocation. 23 patients sustained a type A injury, 68 type B and 15 type C injury. 53 patients sustained a pure dislocation, whereas 53 sustained a fracture dislocation. Low energy partially incongruous joint injuries were considered to be type B injuries TMT joint dislocations and fracture dislocations are not clearly defined in the literature and such characterization can be observer dependant. Lisfranc dislocations with only a fleck avulsion fracture of the base of the second metatarsal, or marginal fractures were considered to be purely ligamentous injuries.2, 13 Patients whose treatment started percutaneously but converted to an open procedure were excluded from the study.
Table 1.
Lisfranc injuries percutaneous fixation literature review.
| Study | No of patients | Type of injury | Method/screws | Mean functional score | Complications | Post Op protocol | Follow up/return to sports |
|---|---|---|---|---|---|---|---|
| Abdelgaid, 20132 | 32 | Type A: 9 | Perc fixation, 3,5 mm cannulated screws | AOFAS: 87 ± 9,45 | No | NWB cast for 6 weeks, PWB for another 6 weeks | 24–48 months (mean 38 months) |
| Type B: 19 | |||||||
| Type C: 4 | |||||||
| Perugia et al, 200213 | 42 | Type A: 14 | Perc fixation, 4,0 mm cannulated partial threaded cancellous screws | AOFAS: 81 ± 13,5 | No | NWB for 6 weeks, progressive WB CAM boot | 58,4 ± 17,3 months |
| Type B: 17, type C: 11 | |||||||
| Wagner et al 201314 | 22 | Type B: 22 | Perc fixation, 3,0 mm cannulated screws | AOFAS: 94 | One patient: transient paraesthesia (intermediate SPN branch) | NWB for 3 weeks, | 33,2 months (12–50 months) |
| CAM boot for another 3 weeks | |||||||
| Lien et al 201615 | 10 | Type B: 10 | Arthroscopic debridement, perc fixation, 3,5 mm cortical or cancellous screws. | AOFAS: 86,8 ± 10,1 | One patient: persistent widening of the Lisfranc distance | NWB cast for 4–6 weeks | 6 months |
| Mean time from injury to surgery: 7,6 ± 4,38 weeks (range: 3–16 weeks) | |||||||
| Vosbikian et al 201716 | 31 | Low energy, minimally displaced | Perc fixation, 4,0 mm fully threaded solid or cannulated screw | Mean FAAM-ADL: 94,2, | No | NWB splint for 2 weeks, NWB CAM boot for 4 weeks, progressive WB for another 6 weeks | 66 months (36–100 months) |
| Mean FAAM-sports: 90,4. | |||||||
| Percentage recovery: 91,4% | |||||||
| Bleazey et al 20133 | 13 | Type B2 (partial incongruity) | 3,7 or 4,3 solid screw | All patients returned to sports in average 16,6 weeks | No | NWB posterior splint for 3 weeks | average return to sports: 16,6 weeks |
| Nunley and Vertullo 20029 | 6 out of 8 (2 patients ORIF due to treatment delay) | Type B1: 3, type B2: 3 | Partially threaded 4,5 mm cannulated screws | Excellent outcome for the 6 patients treated with CRIF | No | NWB for 8 weeks, PWB increasing to FWB between 8 and 12 post op weeks | 27 months (9–72). Average return to sports: 14,4 weeks |
Abbreviations: NWB, non weight bearing; PWB, partial weight bearing; FWB, full weight bearing; CAM, controlled ankle movement; SPN, superficial peroneal nerve; ORIF, open reduction internal fixation; AOFAS, american orthopaedic foot and ankle society; FAAM, foot and ankle ability measure; ADL, activities of daily living.
The average and median AOFAS was calculated for each type of injury, and for patients with purely ligamentous and osseoligamentous injuries using the Microsoft Excel 2007 program. Standard deviation was also calculated. AOFAS scores of different groups of patients according to the type of injury were compared using the student t test statistical method.
Results
The mean AOFAS score was 90 ± 12,85 for type A, 90 ± 11,02 for type B, 90 ± 13,94 for type C injuries respectively. In pure dislocation group the mean AOFAS score was 90 ± 12,89 and in fracture dislocation group was 90 ± 10,67. Average AOFAS score was 86,2 for type A, 87,54 for type B, and 85 for type C injuries respectively. In pure dislocation group the average AOFAS score was 86,43 and in fracture dislocation group it was 87,36. Overall good to excellent results were reported in all groups of patients and comparing them we found no statistical difference in terms of outcome (Table 2). Patients with type B injury as well as patients sustained a fracture dislocation injury seem to have better outcome. This difference though was not statistically significant. Although Perugia et al13 found that patients with pure dislocation resulted to a significantly worse outcome than patients with fracture dislocation, this difference was eliminated combining the patients of this study with the patients sustained pure dislocation in the other three studies.
Table 2.
AOFAS score difference between types of Lisfranc Injury.
| Comparison between types of injury | P-value |
|---|---|
| A–B | 0,66 |
| B–C | 0,52 |
| A–C | 0,79 |
| Pure dislocation – fracture dislocation | 0,69 |
Apart from the 4 studies which they were analysed, it is important to mention three more studies relevant to the subject of this review (Table 1), which they were not included to meta analysis for minor reasons, such as different outcome score, type of injury not clearly defined, or not applicable follow up time etc. Vosbikian et al16 studied 31 patients who sustained a low energy lisfranc injury, treated with a closed reduction and percutaneous fixation using a 4,0 mm fully threaded solid or cannulated screw. Average follow up time was 66 months and the average foot and ankle ability measure (FAAM) for activities of daily living (ADL) and FAAM for sport's activities was 94,2 and 90,4 respectively. Postoperatively a 2 weeks non weight bearing (NWB) splint was applied followed by a NWB controlled ankle movement (CAM) boot for another 4 weeks and progressive weight bearing (WB) for another 6 weeks. Bleazey et al3 presented a case series of 13 patients with a type B Lisfranc injury, who were treated with 3,7 or 4,3 solid screw percutaneous fixation. Post operative protocol was very short including a NWB posterior splint for only 3 weeks, proceeding to progressive WB afterwards. All patient returned to sports 16,6 weeks post operation. Finally Nunley and Vertullo9 described 6 patients with Lisfranc injury who were treated with a percutaneous internal fixation (PRIF) using partially threaded 4,5 mm cannulated screws. NWB was suggested for 8 weeks followed by increasing WB between 8 and 12 weeks post operation. Mean follow up time was 27 months and all patients achieved excellent outcome, returning to sports 14,4 weeks post operation.
Of all the patients who were included in the review study, only one patient developed intermediate superficial peroneal nerve (SPN) transient paraesthesia14 and one patient had a persistent widening of the Lisfranc distance.15 Screws used for fixation varied between studies (Table 1) and no screw breakage was reported. Lien et al15 recommended an arthroscopically assisted debridement and reduction of the Lisfranc joint followed by PRIF (percutaneous internal fixation), which can be of a significant value, especially in delayed treatment where closed reduction might be impossible. In this study particularly, the mean interval from injury to the operation was 7,6 ± 4,38 weeks.
Discussion
Tarsometatarsal foot injuries are relatively rare and they can range from low energy subtle injuries to high energy with gross soft tissue damage.1, 17 Failure to identify and treat properly these injuries leads to a significant disability. While high energy, very displaced Lisfranc dislocations can be easily diagnosed, low energy subtle midfoot trauma can be missed.1 As mentioned in the introduction section, proper clinical examination and imaging are necessary, in order to detect this kind of injury.1, 5 The main classification systems used so far are the Myerson and Nunley–Vertullo, which are useful regarding the anatomical description of the injury, but they are not reliable nor prognostic.18
Goal of treatment should always be accurate reduction and stable fixation.10 There are few debates in the literature regarding the most appropriate method of treatment. Open reduction and internal fixation (ORIF) is the mainstay of treatment for displaced Lisfranc injuries, using either transarticular screws or dorsal bridge plating, which avoids cartilage violation. Several authors reported better functional and radiological outcomes with dorsal bridge plating instead of transarticular screws,19, 20 whereas others found no difference between the two, highlighting the importance of reduction as opposed to the used technique.21 Primary partial arthrodesis (PPA) has also been proposed to treat Lisfranc dislocations. Smith et al22 presented a meta analysis, where PPA was found to be superior to ORIF only in terms of hardware removal. Lower rate of second surgery and hardware removal was reported in the PPA group of patients. Outcome scores and anatomic reduction were the same between the two groups.
To our knowledge, not much have been written regarding percutaneous fixation of Lisfranc injuries (Fig. 5, Fig. 6). The aim of this review is to present the existing data about PRIF. Four studies were met the criteria of the meta analysis, showing good to excellent results with percutaneous fixation regardless type of injury and provided that reduction was accurate. Type B injuries and fracture dislocations demonstrate slightly better outcome, but this difference was not statistically significant, based on our results (Table 2). Perugia et al13 found worse outcome in patients with pure dislocation type of injury. Combining these patients though with the patients of the other three studies this difference was eliminated. It is interesting that the median AOFAS score for all types of injury was similar, highlighting the importance of accurate reduction and secure stabilization as compared to the type of injury. Some authors advocate arthroscopy of the TMT joint to aid in reduction, especially in cases where treatment is delayed and accurate reduction is not feasible.5, 15 It is also supported that open reduction is preferable if the injury is high energy and too unstable,17 provided that the soft tissue envelope allows for an open surgery.
Fig. 5.
Post operation AP view of the patient shown in Fig. 1, Fig. 2. Reduction of the second metatarsal base is noticed.
Fig. 6.
Post operation lateral view. Arch is restored.
Post operative protocol was variable among studies. There are authors suggesting no weight bearing (NWB) cast for 6 weeks, followed by a CAM (controlled ankle movement) boot and progressively increasing weight bearing for another 6 weeks,2, 13 whereas others recommend 3 weeks NWB in a cast or splint followed by PWB in a CAM boot for another 3 weeks.14, 15 There are also studies showing an interval of approximately 16 weeks from operation to the return to sports.3, 9 Robertson et al17 reported quicker return to sports after percutaneous Lisfranc fixation as compared to open methods (ORIF or PPA), especially for low energy injuries. It is reasonable that the more unstable the injury is, the more extended period of NWB is applied.
Very few complications were noted in the existing data, such as persistent displacement15 due to delayed treatment and SPN paraesthesia.14 Conversion to open procedure in cases where closed reduction failed to achieve reduction,2 were not considered as complications of PRIF. In addition, no screw breakage was noted in the presented studies, despite that variable type of screws, cannulated or solid were used. We found also no infection or wound dehiscence, makes sense, as the operation is performed through stab incisions, allowing the surgeon to proceed, even if the swelling of the foot has not been fully subsided.
Our results show good outcome after percutaneous screw fixation of Lisfranc joint unstable injuries. Accurate reduction of the TMT joint complex is crucial. If there is any doubt regarding reduction, the surgeon should convert to open reduction and internal fixation. This review has several limitations. 1) Patients' Demographics, such as age, gender, occupation were not taken in mind. 2) variable follow up among studies. 3) Studied articles were retrospective level IV case series with no control group, 4) no comparison to open reduction was implicated, 5) significantly different number of patients in each subgroup of injury type, affecting the reliability of the statistical comparison, 6) Follow up in the study of Bleazy et al and Lien et al is 4 and 6 months respectively, which is less than one year, but we thought that this was not a reason to exclude them from our review. 7) Relatively small number of patients. 8) Distinguishing fracture dislocation from a pure dislocation injury can be objective. Randomized controlled trials comparing PRIF to ORIF or PPA are necessary in order to come to safe conclusions regarding the proper way of treating these injuries.
Conclusion
Treatment of Lisfranc joint dislocation by closed or open means is still a matter of debate. Percutaneous screw fixation is an effective, safe and relatively simple method of treating tarsometatarsal joint trauma, especially Myerson type B (partial incongruous) injuries and fracture dislocation injuries. A good to excellent functional outcome can be expected with PRIF, as long as anatomic reduction of Lisfranc joint has been achieved.
Conflict of interest
Authors declare that there is no conflict of interest.
Acknowledgements
Marianthi Kalliopi Arvanitaki, Economist Msc, for supporting the statistical analysis.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Weatherford B.M., Anderson J.G., Bohay D.R. Management of tarsometatarsal joint injuries. J Am Acad Orthop Surg. 2017 Jul;25(7):469–479. doi: 10.5435/JAAOS-D-15-00556. [DOI] [PubMed] [Google Scholar]
- 2.Abdelgaid Sherif Mohamed, Salah Mahmoud, Abdulsalam Samir, Abdulmalak Farid. Closed reduction & percutaneous fixation of lisfranc joints injuries: possibility, technique & results. Clin Res Foot Ankle. 2013 May;1(2) [Google Scholar]
- 3.Bleazey S.T.∖., Brigido S.A., Protzman N.M. Technique tip: percutaneous fixation of partial incongruous Lisfranc injuries in athletes. Foot Ankle Spec. 2013 Jun;6(3):217–221. doi: 10.1177/1938640013486515. [DOI] [PubMed] [Google Scholar]
- 4.Meyer S.A., Callaghan J.J., Albright J.P., Crowley E.T., Powell J.W. Midfoot sprains in collegiate football players. Am J Sports Med. 1994 May-June;22(3):392–401. doi: 10.1177/036354659402200316. [DOI] [PubMed] [Google Scholar]
- 5.Escudero M.I., Symes M., Veljkovic A., Younger A.S.E. Low-energy lisfranc injuries in an athletic population: a comprehensive review of the literature and the role of minimally invasive techniques in their management. Foot Ankle Clin. 2018 Dec;23(4):679–692. doi: 10.1016/j.fcl.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Puna R.A., Tomlinson M.P. The role of percutaneous reduction and fixation of lisfranc injuries. Foot Ankle Clin. 2017 Mar;22(1):15–34. doi: 10.1016/j.fcl.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Myerson M.S., Fisher R.T., Burgess A.R., Kenzora J.E. Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot Ankle. 1986 Apr;6(5):225–242. doi: 10.1177/107110078600600504. [DOI] [PubMed] [Google Scholar]
- 8.Hardcastle P.H., Reschauer R., Kutscha-Lissberg E., Schoffmann W. Injuries to the tarsometatarsal joint: incidence, classification and treatment. J Bone Joint Surg Br. 1982 Jun;64(3):349–356. doi: 10.1302/0301-620X.64B3.7096403. [DOI] [PubMed] [Google Scholar]
- 9.Nunley J.A., Vertullo C.J. Classification, investigation, and management of midfoot sprains: lisfranc injuries in the athlete. Am J Sports Med. 2002 Nov-Dec;30(6):871–878. doi: 10.1177/03635465020300061901. [DOI] [PubMed] [Google Scholar]
- 10.Stavlas P., Roberts C.S., Xypnitos F.N., Giannoudis P.V. The role of reduction and internal fixation of Lisfranc fracture-dislocations: a systematic review of the literature. Int Orthop. 2010 Dec;34(8):1083–1091. doi: 10.1007/s00264-010-1101-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ly T.V., Coetzee J.C. Treatment of primarily ligamentous Lisfranc joint injuries: primary arthrodesis compared with open reduction and internal fixation. A prospective, randomized study. J Bone Joint Surg Am. 2006 Mar;88(3):514–520. doi: 10.2106/JBJS.E.00228. [DOI] [PubMed] [Google Scholar]
- 12.Henning J.A., Jones C.B., Sietsema D.L., Bohay D.R., Anderson J.G. Open reduction internal fixation versus primary arthrodesis for lisfranc injuries: a prospective randomized study. Foot Ankle Int. 2009 Oct;30(10):913–922. doi: 10.3113/FAI.2009.0913. [DOI] [PubMed] [Google Scholar]
- 13.Perugia D., Basile A., Battaglia A., Stopponi M., De Simeonibus A.U. Fracture dislocations of Lisfranc's joint treated with closed reduction and percutaneous fixation. Int Orthop. 2003 Feb;27(1):30–35. doi: 10.1007/s00264-002-0396-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wagner E., Ortiz C., Villalón I.E., Keller A., Wagner P. Early weight-bearing after percutaneous reduction and screw fixation for low-energy lisfranc injury. Foot Ankle Int. 2013 Jul;34(7):978–983. doi: 10.1177/1071100713477403. [DOI] [PubMed] [Google Scholar]
- 15.Lien S.B., Shen H.C., Lin L.C. Combined innovative portal arthroscopy and fluoroscopy-assisted reduction and fixation in subtle injury of the lisfranc joint complex: analysis of 10 cases. J Foot Ankle Surg. 2017 Jan – Feb;56(1):142–147. doi: 10.1053/j.jfas.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Vosbikian M., O'Neil J.T., Piper C., Huang R., Raikin S.M. Outcomes after percutaneous reduction and fixation of low-energy lisfranc injuries. Foot Ankle Int. 2017 Jul;38(7):710–715. doi: 10.1177/1071100717706154. [DOI] [PubMed] [Google Scholar]
- 17.Robertson G.A.J., Ang K.K., Maffulli N., Keenan G., Wood A.M. Return to sport following Lisfranc injuries: a systematic review and meta-analysis. Foot Ankle Surg. 2018 Aug;(18):30142–30145. doi: 10.1016/j.fas.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 18.Shariff S., Clark C., Dega R. Lisfranc injury classifications. Internet J Orthop Surg. 2008;11(1) [Google Scholar]
- 19.Hu S.J., Chang S.M., Li X.H., Yu G.R. Outcome comparison of Lisfranc injuries treated through dorsal plate fixation versus screw fixation. Acta Ortop Bras. 2014 Nov;22(6):315–320. doi: 10.1590/1413-78522014220600576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirzner N., Zotov P., Goldbloom D., Curry H., Bedi H. Dorsal bridge plating or transarticular screws for Lisfranc fracture dislocations. Bone Joint J. 2018 Apr;100-B(4):468–474. doi: 10.1302/0301-620X.100B4.BJJ-2017-0899.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lau S., Guest C., Hall M., Tacey M., Joseph S., Oppy A. Functional outcomes post lisfranc injury-transarticular screws, dorsal bridge plating or combination treatment? J Orthop Trauma. 2017 Aug;31(8):447–452. doi: 10.1097/BOT.0000000000000848. [DOI] [PubMed] [Google Scholar]
- 22.Smith N., Stone C., Furey A. Does open reduction and internal fixation versus primary arthrodesis Improve patient outcomes for lisfranc trauma? A systematic review and meta-analysis. Clin Orthop Relat Res. 2016 Jun;474(6):1445–1452. doi: 10.1007/s11999-015-4366-y. [DOI] [PMC free article] [PubMed] [Google Scholar]