Abstract
Background: There are numerous reports regarding increasing childhood and adolescent mental health problems. The aim of this study was to determine the prevalence of psychiatric disorders in Hamadan Province, west of Iran from July 2016 to May 2017.
Study design: A cross-sectional study.
Methods: The sample included 1025 Hamadan residents selected using multistage cluster sampling. Psychiatric disorders were assessed by semi-structured psychiatric interview Kiddie-Sads-Present and Lifetime Version (K-SADS-PL). The data were analyzed using the SPSS software. We used the multivariable logistic regression to predict the Odds Ratios (ORs).
Results: The prevalence of total psychiatric disorder was 8.6%. Psychiatric disorders in boys were higher than girls (12.6% and 4.9%, respectively). The psychiatric disorders were most prevalent in 6-9 yr old age group (11%). The prevalence of behavioral disorder was 3.8% with attention deficit hyperactivity disorder (ADHD) as the most prevalent case (2.0%). The prevalence of anxiety disorder was 2.8% in which the highest prevalence belonged to separation anxiety disorder (SAD) (1.1%). The prevalence of neurodevelopment disorder was 1.5% with the highest prevalence of 1% observed in epilepsy. The prevalence of mood disorder was 1.1% with the depressive disorder as the most prevalent one (1.0%). The prevalence of enuresis was 2.7%. The most common comorbidities were anxiety and mood disorders 5(50.0%).
Conclusion: The prevalence of these disorders in Hamadan was less than the prevalence in other cities of Iran. These findings can be helpful for large-scale planning for children and adolescents.
Keywords: Prevalence, Mental disorders, Child and adolescent, Iran
Introduction
Ten to twenty percent of children and adolescents influenced by mental and psychological problems around the globe every year1. Child and adolescent psychiatric disorders could have adverse effects on individuals, families, and communities 2. Psychiatric disorders not only cause personal and family problems but also are determining risk factors for substance abuse and criminality in adolescents which can predict negative consequences in adulthood as well3.
The prevalence of psychiatric disorders in 1998 was 12.5% and 11.1% in 2013 to 20144. A recent systematic review and meta-analysis of the prevalence of psychiatric disorders in adolescents in 27 countries showed an overall prevalence of psychiatric disorders of 13.4%5. In another study, the prevalence of psychiatric disorders was 10.l%6. In Iran, approximately 17.9% of 6-11-yr-old children in Tehran were suffered from psychiatric disorders7. In Ardabil Province of Iran, hyperactivity, oppositional defiant, and separation anxiety disorder had the highest prevalence, in contrast, psychosis, autism and panic disorders had the lowest prevalence8. The prevalence of psychiatric disorder in males and females was 11.30% and 9.76%, respectively9.
There was little change in the overall prevalence of mental disorders between 1998 and 2014 implying that new innovations in research, policy, and practice are needed to successfully address the major public health problem posed by a child and adolescent mental disorders in the community10. The failure to consider mental health problems in children and adolescents is a public health problem with wide-reaching consequences because a substantial proportion of mental health problems in adults originates from their early childhood which effects go beyond childhood and adolescence1.
Studies on the prevalence of psychiatric disorders in children and adolescents in different parts of the world provide a variety of the different reports and methodological weaknesses in epidemiological studies make it difficult to conclude many of these studies. The results of these studies are typically obtained using parental rating criteria, non-standard methods, small samples, and are often based on available samples, to use systematic methods.
We focused on the prevalence of psychiatric disorders with different methodology in children and adolescents aged 6 to 18 yr in Hamadan Province, west of Iran.
Methods
This research is a part of a national project conducted in the urban and rural areas of Iran, called “The Iranian Children and Adolescents' Psychiatric Disorders Study (IRCAP)”. The protocol and methodology of IRCAP study are fully described11. For evaluating psychiatric disorders in children and adolescents aged 6 to 18 yr, we used a semi-structured interview K-SADS-PL. Overall, 1020 (529 girls and 494 boys) children were sampled through Multistage cluster randomization. In addition to the main city, the rural population were randomly selected (using cluster sampling); in the next step, the blocks were selected randomly according to the postal code. We conducted this cross-sectional study between July 2016 and May 2017 in Hamadan Province.
The inclusion criteria stipulated that children and adolescents should be between 6 and 18 yr of age and be identified as Iranian population. Participants were excluded if the child or adolescent or their parents had restriction that forbidden their ability to sufficiently complete the questionnaire, such as sever developmental or psychosis or learning disabilities, or inability to read and speak Farsi. The interviews were performed by specialist clinical psychologists using the software.
The national institute for medical research development (NIMAD) supported this study (the ethics code of IR.NIMAD.REC.1395.001). Written consent was obtained from each subject. Other clinical and demographic data were also obtained from each individual.
Evaluation of Psychiatric Disorders
Psychiatric disorders in children and adolescents were evaluated using the Schedule for Affective Disorders and Schizophrenia for School-Age Children/Present and Lifetime Version (KSADS- PL) based on mother/main caregiver report. KSADS- PL is a semi-structured psychiatric interview that helps in diagnosis of psychiatric disorders in five categories:
-
“Affective disorders (depressive disorders [major depression, dysthymia] and mania, hypomania);
Psychotic disorders;
Anxiety disorders (social phobia/ agoraphobia/ specific phobia/ obsessive-compulsive disorder/ separation anxiety disorder/ generalized anxiety disorder/ panic disorder/ posttraumatic stress disorder);
Disruptive behavioral disorders (ADHD/conduct disorder/oppositional defiant disorder).
Substance abuse, tic disorders, eating disorders, and elimination disorders (enuresis/encopresis)”12. The interview opens with questions about basic demographics. Health and developmental history data should be obtained as this information may be helpful in making differential diagnoses12.
The test-retest reliability and inter-rater reliability of the Persian version of K-SADS-PL were 0.81 and 0.69, respectively in which the sensitivity and specificity of the Persian version of K-SADS were high. The K-SADS-PL was used to diagnose ADHD and its psychiatric comorbidities. We considered all the lifespan related psychiatric diagnoses13. An acceptable interrater agreement for K-SADS has been reported (kappa coefficients 0.90 to 0.94) 14.
Statistical Analysis
Data were analyzed using SPSS ver. 22 (Chicago, IL, USA). To investigate the relationship between scores of the K- SADS questionnaire and the demographic factors, we used descriptive analysis and 95% confidence interval. We used the multivariable logistic regression to predict the Odds Ratios (ORs)
Results
The prevalence of psychiatric disorders in boys was higher than girls (12.6% and 4.9%, respectively). Among three age groups, the psychiatric disorders were most prevalent in 6-9 yr old age group (11.0%). The prevalence of psychiatric disorders in rural areas was higher than in urban areas (10.6% and 8.3%, respectively). The prevalence of psychiatric disorders based on the demographic variables such as father’s and mother’s education (MSc or higher), father’s (unemployed) and mother’s job (unemployed or housewife) were more than other variables (Table 1).
Table 1. Frequency of Demographic Variables in Children and Adolescents (6-18) of Hamadan province and Prevalence of Psychiatric Disorders in Terms of these Variables .
| Variables |
Total
n=1020 |
With disorder, n=88 | Prevalence CI (95%) | |
| Number | Percent | Number | ||
| Sex | ||||
| Boy | 494 | 48.4 | 62 | 12.55(9.91, 15.76 ) |
| Girl | 529 | 51.9 | 26 | 4.91 (3.37, 7.10) |
| Age (yr) | ||||
| 6-9 | 346 | 33.9 | 38 | 10.98 (1.78, 5.60) |
| 10-14 | 335 | 32.8 | 24 | 7.16 (4.86, 10.43) |
| 15-18 | 339 | 33.2 | 26 | 7.67 (5.29, 11.00) |
| Place of residence | ||||
| Urban | 869 | 85.2 | 72 | 8.28 (6.64, 10.31) |
| Rural | 151 | 14.8 | 16 | 10.59 (6.63, 16.52) |
| Father’s education | ||||
| Illiterate | 42 | 4.2 | 3 | 7.14 (2.46, 19.01) |
| Primary school | 217 | 21.8 | 20 | 9.21 (6.05, 13.81) |
| Guidance & high school | 261 | 26.2 | 27 | 10.34 (7.20, 14.63) |
| Diploma | 227 | 22.8 | 17 | 7.48 (4.73, 11.67) |
| Bachelor | 185 | 18.6 | 10 | 5.41 (2.97, 9.67) |
| MSc or higher | 65 | 6.5 | 9 | 13.85 (7.46, 24.27) |
| Mother’s education | ||||
| Illiterate | 27 | 2.7 | 2 | 7.41 (2.06, 23.37) |
| Primary school | 253 | 24.9 | 22 | 8.69 (5.82, 12.82) |
| Guidance & high school | 244 | 24.0 | 25 | 10.25 (7.04, 14.69) |
| Diploma | 294 | 28.9 | 22 | 7.48 (4.99, 11.07) |
| Bachelor | 179 | 17.6 | 13 | 7.26 (4.29, 12.02) |
| MSc or higher | 20 | 2.0 | 3 | 15.00 (5.24, 36.04) |
| Father’s job | ||||
| Public sector | 307 | 30.8 | 21 | 6.84 (4.52, 10.23) |
| Private sector | 661 | 66.4 | 61 | 9.23 (7.25, 11.68) |
| Unemployed | 28 | 2.8 | 4 | 14.28 (5.70, 31.49) |
| Mother’s job | ||||
| Public sector | 86 | 8.5 | 5 | 5.81 (2.51, 12.89) |
| Private sector | 23 | 2.3 | 2 | 8.69 (2.42, 26.8) |
| Unemployed | 908 | 89.3 | 80 | 8.81 (7.14, 10.83) |
The odds ratio of gender (female): (OR=0.36; 95% CI: 0.22, 0.59) (P=0.001) and age (10-14): (OR=056; 95% CI: 0.32, 0.98) were statistically significant (P=0.049) (Table 2).
Table 2. Odds Ratios (95% CI) for total psychiatric disorder in term of demographic variables .
| Variables |
Crude OR
(CI 95%) |
P value |
Adjusted OR
(CI 95%) |
P value |
| Sex | ||||
| Male | 1.00 | 1.00 | ||
| Female | 0.36 (0.22, 0.58) | 0.001 | 0.36 (0.22, 0.59) | 0.001 |
| Age group (yr) | ||||
| 6-9 | 1.00 | 1.00 | ||
| 10-14 | 0.62 (0.36, 1.06) | 0.091 | 0.56 (0.32, 0.98) | 0.049 |
| 15-18 | 0.67 (0.39, 1.13) | 0.145 | 0.65 (0.37, 1.13) | 0.127 |
| Locus of life | ||||
| Urban | 1.00 | 1.00 | ||
| Rural | 1.31 (0.74, 2.32) | 0.352 | 1.16 (0.61, 2.21) | 0.652 |
| Father’s education | ||||
| Illiterate | 1.00 | 1.00 | ||
| primary school | 1.32 (0.37, 4.65) | 0.666 | 1.28 (0.32, 5.01) | 0.723 |
| High school | 1.50 (0.43, 5.18) | 0.522 | 1.28 (0.31, 5.22) | 0.728 |
| Diploma | 1.05 (0.29, 3.76) | 0.937 | 1.11 (0.25, 4.90) | 0.891 |
| Bachelor | 0.74(0.19, 2.83) | 0.663 | 1.07 (0.20, 5.66) | 0.934 |
| MSc or higher | 2.08 (0.53, 8.21) | 0.292 | 3.04 (0.51, 18.35) | 0.225 |
| Mother’s education | ||||
| Illiterate | 1.00 | 1.00 | ||
| primary school | 1.19 (0.26, 5.36) | 0.820 | 0.94 (0.18, 4.77) | 0.939 |
| High school | 1.42 (0.32, 6.38) | 0.642 | 1.32 (0.25, 7.01) | 0.747 |
| Diploma | 1.01 (0.22, 4.55) | 0.989 | 0.95 (0.17, 5.36) | 0.958 |
| Bachelor | 0.98 (0.21, 4.60) | 0.978 | 0.95 (0.15, 6.0)3 | 0.953 |
| MSc or higher | 2.20 (0.33, 14.63) | 0.413 | 1.99 (0.19, 20.39) | 0.561 |
| Father’s job | ||||
| Public sector | 1.00 | 1.00 | ||
| Private sector | 1.38 (0.83, 2.32) | 0.216 | 1.45 (0.68, 3.06) | 0.334 |
| unemployed | 2.27 (0.72, 7.15) | 0.161 | 2.21 (0.58, 8.41) | 0.247 |
| Mother's job | ||||
| Public sector | 1.00 | 1.00 | ||
| Private sector | 1.54 (0.28, 8.52) | 0.619 | 2.21 (0.32, 15.03) | 0.419 |
|
Unemployed (Housewife) |
1.56 (0.62, 3.97) | 0.346 | 1.83 (0.56, 5.96) | 0.312 |
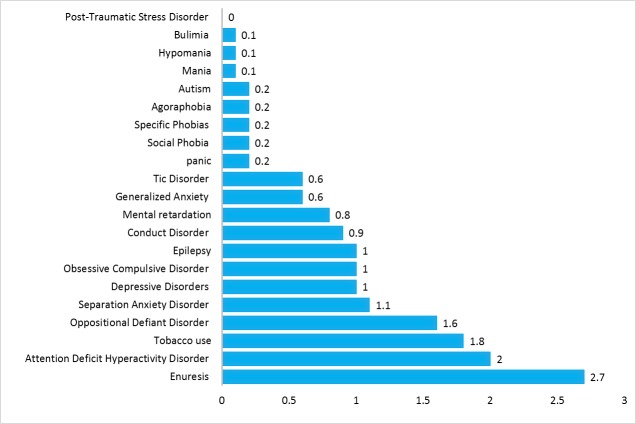
The prevalence of total psychiatric disorders in Hamadan Province was 8.6%. The prevalence of behavioral disorders was 3.8% with attention deficit hyperactivity disorder (ADHD) as the most prevalent one with a prevalence equal to 2.0%. The prevalence of anxiety disorders was 2.8% in which the highest prevalence belonged to separation anxiety disorder (SAD) (1.1%). The prevalence of neurodevelopment disorders was 1.5% with the highest prevalence of 1% observed in epilepsy. The prevalence of mood disorders was 1.1% with depressive disorder as the most prevalent one (1.0%). The prevalence of enuresis and tobacco use was 2.7% and 1.8%, respectively (Table 3, Figure 1 and Figure 2).
Table 3. The Prevalence of Psychiatric Disorders in the Hamedan province children and adolescents (6-18) .
| Psychiatric Disorders | Number |
Prevalence CI
(95%) |
| Mood disorders | ||
| Depressive disorders | 10 | 0.98 (0.53, 1.79) |
| Mania | 1 | 0.10 (0.02, 0.56) |
| Hypomania | 1 | 0.10 (0.02, 0.56) |
| Total mood disorder | 11 | 1.07 (0.60, 1.92) |
| Anxiety disorders | ||
| Panic | 2 | 0.20 (0.06, 0.72) |
| Separation anxiety disorder | 11 | 1.07 (0.60, 1.92) |
| Social phobia | 2 | 0.20 (0.06, 0.72) |
| Specific phobias | 2 | 0.20 (0.06, 0.72) |
| Agoraphobia | 2 | 0.20 (0.06, 0.72) |
| Generalized anxiety | 6 | 0.59 (0.27, 1.28) |
| Obsessive compulsive disorder | 10 | 0.98 (0.53, 1.79) |
| Post-traumatic stress disorder | 0 | 0.00 (0.00, 0.00) |
| Total anxiety disorders | 29 | 2.84 (1.98, 4.05) |
| Behavioral disorders | ||
| Attention deficit hyperactivity disorder | 20 | 1.96 (1.27, 3.01) |
| Oppositional defiant disorder | 16 | 1.57 (0.97, 2.53) |
| Conduct disorder | 9 | 0.88 (0.46, 1.67) |
| Tic disorder | 6 | 0.59 (0.27, 1.28) |
| Total behavioral disorders | 39 | 3.82 (2.81, 5.18) |
| Neurodevelopmental disorders | ||
| Mental retardation | 8 | 0.78 (0.40, 1.53) |
| Autism | 2 | 1.96 (0.06, 0.72) |
| Epilepsy | 10 | 0.98 (0.53, 1.79) |
| Total | 15 | 1.47 (0.89, 2.41) |
| Tobacco use | 18 | 1.76 (1.12, 2.77) |
| Enuresis | 28 | 2.74 (1.91, 3.94) |
| Bulimia | 1 | 0.10 (0.02, 0.56) |
| Total psychiatric disorders | 88 | 8.62 (7.06, 10.51) |
Figure 1.
The prevalence of psychiatric disorders in children and adolescents in Hamadan Province
Figure 2.
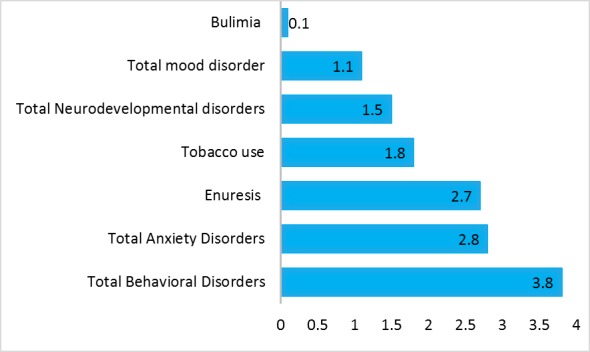
The prevalence of psychiatric disorders in children and adolescents in Hamadan Province
The most common comorbidities were in anxiety and mood disorders 5 (50.0%), mood and behavioral disorders 4 (40.0%), developmental and behavioral disorders 5 (33.3%), behavioral and substance abuse disorders 5 (27.8%), anxiety and behavioral disorders 6 (20.7) (Table 4).
Table 4. Comorbidity disorders according to the type of psychiatric disorder in Hamadan Province .
| Main disorder |
Mood
Disorders |
Anxiety
disorders |
Behavioral
Disorders |
Neurodevelopmental
disorders |
Substance abuse
disorders |
Elimination
Disorders |
Eating
Disorder |
| Mood Disorders | 11 | 5 | 4 | 1 | 1 | 0 | 1 |
| Anxiety Disorders | 5 | 29 | 6 | 1 | 2 | 4 | 0 |
| Behavioral Disorders | 4 | 6 | 39 | 5 | 5 | 3 | 1 |
| Neurodevelopmental disorders | 1 | 1 | 5 | 15 | 0 | 2 | 0 |
| Substance abuse disorders | 1 | 2 | 5 | 0 | 18 | 0 | 0 |
| Elimination Disorders | 0 | 4 | 3 | 2 | 0 | 28 | 0 |
Discussion
This study as a first one, was carried out in Hamadan Province with a large sample selected from the urban and rural areas to determine the prevalence rates of psychiatric disorders in children and adolescents in the age group of 6-18 yr old. The overall prevalence of psychiatric disorders in the studied age group (6-18) was 8.6% (95% CI: 7.06, 10.51). This finding is approximately consisted with previous study conducted in Iran in this age group (10.51%)9. The overall prevalence of psychiatric disorders in 1998 was 12.5% (95% CI: 11.4, 13.7) and 11.1% (95% CI: 10.1, 12.2) in 2013 to 20144.
Some distinct differences were found among groups in terms of the prevalence of disorders based on the demographic variables, with higher prevalence in three age groups of 6-9, 10-14 and 15-18 yr old. The prevalence of psychiatric disorders in boys was higher than girls and the psychiatric disorders were most prevalent in the 6-9 yr old subjects which are in line with previous findings 9,15-18. The prevalence of psychiatric disorders was higher in rural areas compared to urban areas, not consistent with the previous findings19, 20. In the United States, no association was observed between urban areas and the prevalence of major depression in adolescents. In addition, no significant differences were found in the prevalence of major depression or serious mental illness in adults between large metropolitan areas and rural areas, while the prevalence of both was slightly higher in two intermediate urban areas compared to large metropolitan areas. Contrary to expectations, the prevalence of mental disorders was not higher in most of the urban compared to rural areas21.
The prevalence of psychiatric disorders based on the demographic variables such as father’s and mother’s education (MSc or higher), father’s (unemployed) and mother’s job (unemployed or housewife) were more than other variables which are in line with the results of the other studies22,23.
Another important finding of this study was the higher prevalence of psychiatric disorders in parents with higher education, in line with other study22. The odds ratios of psychiatric disorders were higher in girls aged between 10-14 yr old. This finding is also consistent with previous study23. Total behavioral disorder was 3.8% with attention deficit hyperactivity disorder (ADHD) as the most prevalent one (2%) which is consistent with the results of other studies3, 23. The prevalence of total neurodevelopment disorder was 1.5% with the highest prevalence of 1% observed in epilepsy. The prevalence of total mood disorder was 1.1% with depressive disorder as the most prevalent one (1%). The prevalence of enuresis and tobacco use was 2.7% and 1.8, respectively, this prevalence of tobacco use was less than other finding24. ADHD, ODD, enuresis, and SAD disorders had the highest prevalence in the studied sample. In contrast, psychosis, autism, and panic disorders had the lowest prevalence. This finding was concordant with other study conducted in province of Iran 8. Conduct disorders 6.6% (7.1% for child sample and 6.0% for adolescent sample) and anxiety disorders 5.0% (5.9% for child sample and 6.0% for adolescent sample) were the most common groups of disorders and the risk factors are related to child characteristic (gender, poor general health, and stressful life experiences)25. The overall prevalence of psychiatric disorders in children and adolescents was 13.4% (CI 95% 11.3-15.9). The worldwide prevalence of anxiety, depressive and attention-deficit hyperactivity disorders were 6.5%, 2.6%, and 3.4%, respectively validated by our findings5.
In our study, the most common comorbidities were anxiety and mood disorders, mood and behavioral disorders, developmental and behavioral disorders, behavioral and substance abuse disorders and anxiety and behavioral disorders. More comorbid disorders; from anxiety disorder to conduct disorder and emotional disorders (depression or anxiety have highest comorbidity)25. The most common observed combinations were any mood disorder with any ADHD/hyperactivity disorder, any anxiety disorder with any mood disorder, seen in 16 subjects (21.9%), any ADHD/hyperactivity disorder with any conduct/oppositional disorder, and any anxiety disorder with any ADHD/ hyperactivity disorder 3. These findings are consistent with the findings of our study.
Some of the advantages of this study were that it is a population-based study, with face-to-face interviews, involving a large sample of children and adolescents. We used an international instrument, designed to generate diagnoses of psychiatric disorders in children and adolescents, validated for using in Iran applied by trained psychologists. The limitations of our study were based only on information obtained from the parents, children, and adolescents, because the KSADS- PL was not administered to children and adolescent teachers. Teachers’ reports could reveal some other symptoms not recognized by parents, contributing to a more accurate diagnosis of the psychiatric disorders.
Conclusion
The prevalence of these disorders (with a small difference) in Hamadan is less than the prevalence in other cities of Iran. These findings can be helpful for large-scale planning for children and adolescents.
Acknowledgements
We would like to thank all the interviewers involved in the study in Hamadan Province. We would also like to thank all the families of the participants for their cooperation.
Conflict of interest statement
The authors declare that there is no conflict of interests.
Funding
This study was supported by National Institution for Medical Research Development Islamic Republic of Iran (NIMAD) [Grant No. 940906]. Psychiatry and Psychology Research Center, Tehran University of Medical Sciences, and Research Center for Behavioral Disorders and Substances Abuse, Hamadan University of Medical Sciences Hamadan, Iran, involved in this survey.
Highlights
The prevalence of total psychiatric disorder was 8.6%.
The psychiatric disorders were most prevalent in 6-9 yr old age group (11%).
The highest prevalence was in behavioral disorders (attention deficit hyperactivity disorder) and the least prevalence was in mood disorder (depressive disorder).
Citation: Ahmadpanah M, Nazaribadie M, Mohammadi MR, Hooshyari Z, Alavi SS, Ghaleiha A, Jahangard L, Keshavarzi A, Farahmand Sabet M, Nabizadeh S, Bagheri N, Zaeri Omid P, Kokabi Heidarpoor F, Arji J, Jedi Ghader D, Abbasi S, Toluei N. The Prevalence of Psychiatric Disorders in Children and Adolescents in Hamadan Province, West of Iran. J Res Health Sci. 2018; 18(4): e00432.
References
- 1.Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O. et al. Child and adolescent mental health worldwide: evidence for action. The Lancet. 2011;378(9801):1515–25. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 2.Fleitlich-Bilyk B, Goodman R. Prevalence of child and adolescent psychiatric disorders in southeast Brazil. Am Acad Child Adolesc Psychiatry. 2004;43:727–34. doi: 10.1097/01.chi.0000120021.14101.ca. [DOI] [PubMed] [Google Scholar]
- 3.La Maison C, Munhoz TN, Santos IS, Anselmi L, Barros FC, Matijasevich A. Prevalence and risk factors of psychiatric disorders in early adolescence: 2004 Pelotas (Brazil) birth cohort. Soc Psychiatry Psychiatr Epidemiol. 2018;53(7):685–97. doi: 10.1007/s00127-018-1516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Merikangas KR. Time Trends in the Global Prevalence of Mental Disorders in Children and Adolescents: Gap in Data on US Youth. J Am Acad Child Adolesc Psychiatry. 2018;57(5):306–7. doi: 10.1016/j.jaac.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual Research Review: A meta‐analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56:345–65. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 6.Bilenberg N, Petersen DJ, Hørder K, Gillberg C. The prevalence of child‐psychiatric disorders among 8–9‐year‐old children in Danish mainstream schools. Acta Psychiatr Scand. 2005;111:59–67. doi: 10.1111/j.1600-0447.2004.00432.x. [DOI] [PubMed] [Google Scholar]
- 7.Alavi A, Mohammadi MR, Joshaghani N, Mahmoudi-Gharaei J. Frequency of psychological disorders amongst children in urban areas of Tehran. Iran J Psychiatry. 2010;5(2):55–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Khaleghi A, Mohammadi MR, Zandifar A, Ahmadi N, Alavi SS, Ahmadi A. et al. Epidemiology of psychiatric disorders in children and adolescents; in Tehran, 2017. Asian J Psychiatr. 2018;37:146–53. doi: 10.1016/j.ajp.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 9.Mohammadi MR, Ahmadi N, Salmanian M, Asadian-Koohestani F, Ghanizadeh A, Alavi A. et al. Psychiatric disorders in Iranian children and adolescents. Iran J Psychiatry. 2016;11(2):87–98. [PMC free article] [PubMed] [Google Scholar]
- 10.Sawyer MG, Reece CE, Sawyer ACP, Johnson SE, Lawrence D. Has the prevalence of child and adolescent mental disorders in Australia changed between 1998 and 2013 to 2014? J Am Acad Child Adolesc Psychiatry. 2018;57(5):343–50. doi: 10.1016/j.jaac.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Mohammadi MR, Ahmadi N, Kamali K, Khaleghi A, Ahmadi A. Epidemiology of psychiatric disorders in iranian children and adolescents (IRCAP) and its relationship with social capital, life style and parents' personality disorders: study protocol. Iran J Psychiatry. 2017;12(1):66–72. [PMC free article] [PubMed] [Google Scholar]
- 12.Kaufman J, Birmaher B, Brent D, Rao UMA, Flynn C, Moreci P. et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–8. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Ghanizadeh A. ADHD, bruxism and psychiatric disorders: does bruxism increase the chance of a comorbid psychiatric disorder in children with ADHD and their parents? Sleep Breath. 2008;12:375–80. doi: 10.1007/s11325-008-0183-9. [DOI] [PubMed] [Google Scholar]
- 14.Polanczyk GV, Eizirik M, Aranovich V, Denardin D, da Silva TL, da Conceição TV. et al. Interrater agreement for the schedule for affective disorders and schizophrenia epidemiological version for school-age children (K-SADS-E) Braz J Psychiatr. 2003;25(2):87–90. doi: 10.1590/s1516-44462003000200007. [DOI] [PubMed] [Google Scholar]
- 15. Alyahri A , Goodman R . The prevalence of DSM-IV psychiatric disorders among 7–10 year old Yemeni school children. Soc Psychiatry Psychiatr Epidemiol. 2008;43:224–30. doi: 10.1007/s00127-007-0293-x. [DOI] [PubMed] [Google Scholar]
- 16. Mullick MSI , Goodman R . The prevalence of psychiatric disorders among 5–10 year olds in rural, urban and slum areas in Bangladesh. Soc Psychiatry Psychiatr Epidemiol. 2005;40:663–71. doi: 10.1007/s00127-005-0939-5. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence D, Hafekost J, Johnson SE, Saw S, Buckingham WJ, Sawyer MG. et al. Key findings from the second Australian child and adolescent survey of mental health and wellbeing. Aust N Z J Psychiatry. 2016;50(9):876–86. doi: 10.1177/0004867415617836. [DOI] [PubMed] [Google Scholar]
- 18.Jaju S, Al-Adawi S, Al-Kharusi H, Morsi M, Al-Riyami A. Prevalence and age-of-onset distributions of DSM IV mental disorders and their severity among school going Omani adolescents and youths: WMH-CIDI findings. Child Adolesc Psychiatry Ment Health. 2009;3(1):29. doi: 10.1186/1753-2000-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Srinath S, Girimaji SC, Gururaj G, Seshadri S, Subbakrishna DK, Bhola P. et al. Epidemiological study of child & adolescent psychiatric disorders in urban & rural areas of Bangalore, India. Indian J Med Res. 2005;122(1):67–79. [PubMed] [Google Scholar]
- 20.Gamm L, Stone S , Pittman S . Mental health and mental disorders—A rural challenge: A literature review. J Rural Health. 2010;2:97–113. [Google Scholar]
- 21.Breslau J, Marshall GN, Pincus HA, Brown RA. Are mental disorders more common in urban than rural areas of the United States? Journal of psychiatric research. 2014;56:50–5. doi: 10.1016/j.jpsychires.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 22.McLaughlin KA, Breslau J, Green JG, Lakoma MD, Sampson NA, Zaslavsky AM. et al. Childhood socio-economic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Social Science & Medicine. 2011;73(7):1088–96. doi: 10.1016/j.socscimed.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merikangas KR, He J-p, Burstein M, Swanson SA, Avenevoli S, Cui L. et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barati M, Allahverdipour H, Hidarnia A, Niknami S. Predicting tobacco smoking among male adolescents in Hamadan City, west of Iran in 2014: an application of the prototype willingness model. J Res Health Sci. 2015;15:113–8. [PubMed] [Google Scholar]
- 25.Lesinskiene S, Girdzijauskiene S, Gintiliene G, Butkiene D, Puras D, Goodman R. et al. Epidemiological study of child and adolescent psychiatric disorders in Lithuania. BMC Public Health. 2018;18(1):548. doi: 10.1186/s12889-018-5436-3. [DOI] [PMC free article] [PubMed] [Google Scholar]