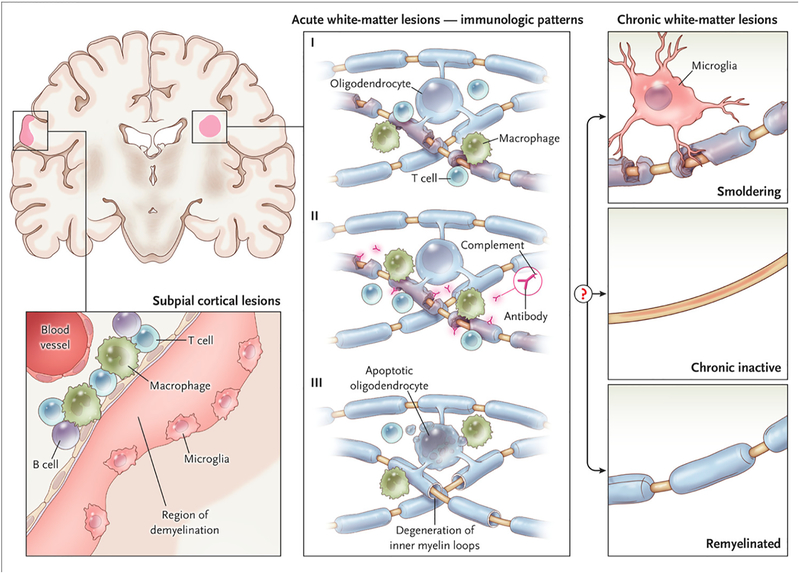
Figure 2. White and gray matter lesions.
Early active white matter demyelination falls into three major categories. The most common types (Patterns I and II) show a background of mononuclear phagocytes with perivascular and parenchymal T-cell infiltration; Pattern II is further distinguished by immunoglobulin and complement deposition. In ~25% of biopsied active lesions (Pattern III), oligodendrocyte apoptosis is accompanied by a “dying-back” oligodendrogliopathy, starting at the “inner tongue.” These lesions show resemble viral, toxic, and ischemic processes, and can be destructive. After the acute phase, factors that remain poorly understood determine whether surviving axons in a lesion are invested by a thin myelin sheath (“remyelinated”), whether inflammation resolves without remyelination (“chronic inactive”), or whether inflammation and slow myelin degeneration persist (“smoldering”). Smoldering lesions are most common in progressive MS. The subpial cortical lesion, which is also more common in progressive MS, is characterized by demyelination of the superficial cortex, possibly associated with inflammation in the overlying leptomeninges and sparse microglia at the border between demyelinated and myelinated neuropil.