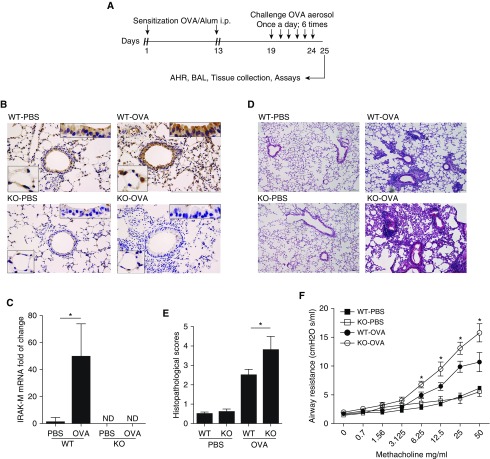
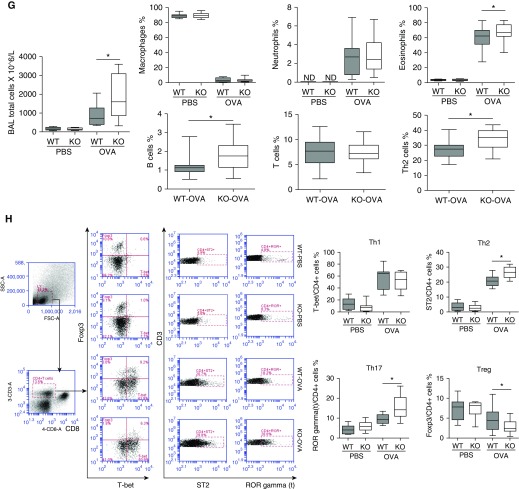
Figure 1.
Effect of IL-1 receptor–associated kinase M (IRAK-M) on ovalbumin (OVA)-induced airway inflammation and airway hyperresponsiveness (AHR). (A) Schematic representation of the OVA exposure protocol. (B) Representative images of immunohistochemical staining of IRAK-M in PBS- or OVA-treated wild-type (WT, upper panel) and IRAK-M knockout (KO, lower panel) mouse lungs. (C) IRAK-M mRNA levels in OVA- or PBS-treated WT or IRAK-M KO mouse lungs. IRAK-M gene expression was normalized to glyceraldehyde-3-phosphate dehydrogenase; n = 10 in each group; *P < 0.05. (D) Representative lung histological images and (E) semiquantitative histopathological scores from PBS- or OVA-treated WT and IRAK-M KO mice. n = 10 mice in each group; *P < 0.05. (F) Airflow resistance to methacholine stimulation in PBS- or OVA-treated WT and IRAK-M KO mice. n = 10–12 mice in each group; *P < 0.05 WT versus KO-OVA group. (G) Total number of inflammatory cells in bronchoalveolar (BAL) fluid of PBS- or OVA-treated WT and IRAK-M KO mice, and flow cytometry analysis for BAL cells using specific antibodies against different groups of leukocytes. n = 10–30 mice in each group; *P < 0.05. (H) FACS analysis of lung T-helper cell type 1 (Th1), Th2, Th17, and Treg cells using specific antibodies in PBS- or OVA-treated WT and IRAK-M KO mice. The percentages of Th1, Th2, Th17, and Treg cells are plotted. IRAK-M KO mice had a significantly higher percentage of Th2 cells and lower percentage of Treg cells in the lung than WT mice. n = 10–20 mice in each group; *P < 0.05. FSC, forward scatter; i.p., intraperitoneal; ND, not determined; SSC, side scatter.