Abstract
Blood eosinophils are a predictive biomarker of inhaled corticosteroid response in chronic obstructive pulmonary disease (COPD). We investigated blood eosinophil stability over 1 year using the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2019 thresholds of < 100, 100- < 300 and ≥ 300 eosinophils/μL in 225 patients from the COPDMAP cohort. Blood eosinophils showed good stability (rho: 0.71, p < 0.001, ICC 0.84), and 69.3% of patients remained in the same eosinophil category at 1 year. 85.3% of patients with eosinophils < 100 cells/μL had stable counts. The majority of blood eosinophil counts remain stable over 1 year using the GOLD 2019 thresholds.
Keywords: COPD, Eosinophil, Airway inflammation
Introduction
Randomised controlled trials have shown a relationship between blood eosinophil counts and the effects of inhaled corticosteroid (ICS) on exacerbations in chronic obstructive pulmonary disease (COPD) [1–3]. Data modelling suggests that ICS effects are observable at > 100 cells/μL, with the greatest effects at ≥300 cells/μL [4]. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2019 report recommends < 100 and ≥ 300 eosinophils/μL thresholds to identify patients who are least and most likely, respectively, to benefit from ICS treatment [3].
The stability of blood eosinophil counts over time is an issue that is relevant for the use of this biomarker in COPD patients. Changes in blood eosinophil counts that result in movement across the thresholds recommended by GOLD may influence pharmacological treatment decisions. Greater variability for repeated blood eosinophil counts has been reported at higher eosinophil levels [5–7], but the stability of eosinophil counts has not been assessed using current GOLD recommended thresholds. We have analysed the stability of blood eosinophil counts over 1 year in the COPDMAP observational cohort study (www.copdmap.org; study design described previously [8]) using the GOLD 2019 thresholds.
Methods
COPD patients with two blood eosinophil measurements taken at baseline and 12 months apart during stable state were included (n = 225) to determine within-subject variability over time. Patients with a previous asthma history or requiring maintenance oral corticosteroid therapy were excluded from this analysis. All patients provided written informed consent and local ethical approvals were obtained (11/L0/1630;10/H/1003/108; 07/H0406/157). Additional methods are in the online supplement (Additional file 1). Patients were subdivided into 3 groups using the baseline blood eosinophil count; < 100, 100- < 300 or ≥ 300 cells/μL. Data were analysed using spearman’s rank test (Prism 7.0, GraphPad, USA), intraclass correlation coefficient (ICC) of log-transformed data, analysis of variance (ANOVA), linear regression, Bland-Altman and repeatability coefficient analysis (RCA) calculated as 1.96 multiplied by times the within-subject standard deviation (SPSS 22.0, IBM, Armonk, USA) [9]. ICC values are interpreted as excellent (> 0.75), fair to good (0.40–0.75), or poor (< 0.40) [9]. P < 0.05 was considered statistically significant.
Results
Patients had a mean (SD) age of 69.8 (8.4) years, forced expiratory volume in 1 s (FEV1) 55.9% (18.2%) predicted, COPD assessment test (CAT) score 16.9 (7.5), and 1.6 (2.1) exacerbations per year; 67.1% were male, 29.3% were current smokers and 80.4% were on ICS therapy. The number of patients with blood eosinophils < 100, 100- < 300 and ≥ 300 cells/μL were 38 (16.9%), 139 (61.8%) and 48 (21.3%) respectively; clinical characteristics of these groups were similar.
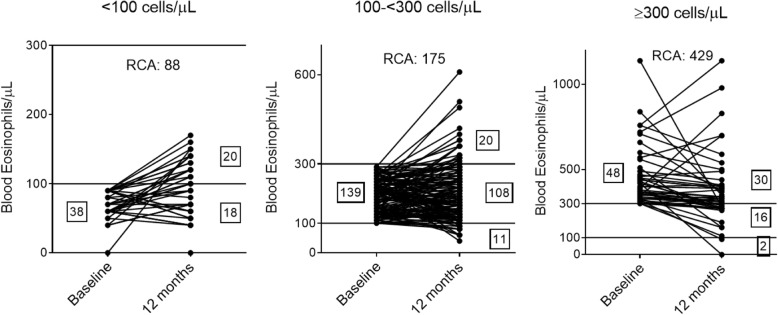
There was a significant correlation between blood eosinophil counts at baseline and 12 months (n = 225); rho = 0.71, p < 0.001. The ICC value was 0.84, indicating excellent repeatability. Bland-Altman regression analysis showed lowest and greatest variability at < 100 eosinophils/μL and ≥ 300 eosinophils/μL at baseline respectively (linear regression p < 0.001). Repeatability coefficients for blood eosinophils < 100, 100- < 300, and ≥ 300 cells/μL showed that 95% of measurements at 12 months were within 88, 175 and 429 cells/μL of the baseline value, respectively [Fig. 1]. 69.3% (n = 156) of patients had blood eosinophils that remained within the same category over 12 months; 47.4, 77.7 and 62.5% of patients remained stable at < 100, 100- < 300 cells/μL, and ≥ 300 cells/μL, respectively [Fig. 1]. Of those patients with blood eosinophils < 100 or ≥ 300 cells/μL who changed group, the majority (36/38 patients) moved to the adjacent group.
Fig. 1.
Stability of blood eosinophils stratified by baseline blood eosinophils < 100, 100–300 or ≥ 300 cells/μL. Number of patients are displayed in boxes. Repeatability coefficients (RCA) were 88, 175 and 429 cells/μL, respectively
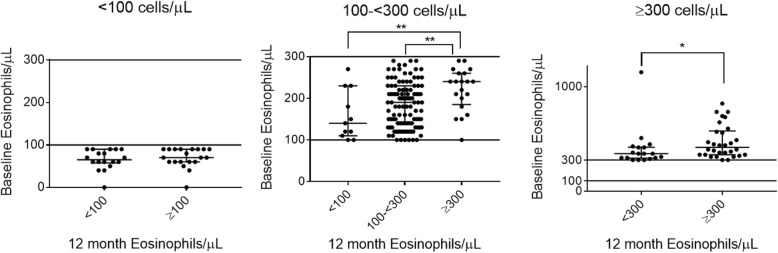
Baseline blood eosinophil counts were similar in patients who remained < 100 cells/μL compared to those who changed group [Fig. 2]. Blood eosinophil counts in patients who remained in the 100- < 300 cells/μL group were lower compared to those who changed to ≥ 300 cells/μL (medians 190 vs 240 cells/μL, respectively, p = 0.0053), while the lowest counts were observed in those who moved to < 100 cells/μL (median 140 cells/μL, p = 0.12 for comparison versus patients who remained in the 100- < 300 cells/μL group). For patients with blood eosinophils ≥ 300 cells/μL, those that moved below 300 cells/μL at 12 months had a lower baseline measurement compared to those who remained ≥ 300 cells/μL (median 360 vs 420, respectively, p = 0.024). Only 3 patients (out of 225) changed ICS use within the 12-month observation period; these patients were commenced on ICS treatment, and none dropped to a lower eosinophil group.
Fig. 2.
Comparison of baseline blood eosinophil counts in those who remained versus changed 12-month blood eosinophil group. Graphs stratified by baseline groups < 100, 100- < 300 or ≥ 300 cells/μL, respectively. Error bars represent median and IQR. * = p < 0.05. ** = p < 0.01
There were 99 patients who experienced ≥1 exacerbation within the 12 month period between stable state blood eosinophil measurements. The correlation between repeated blood eosinophil measurements was similar in patients with ≥1 exacerbation (rho = 0.73, p < 0.001) and those with no exacerbations (n = 126; rho = 0.71, p < 0.001). For patients with ≥1 exacerbation, 72.7% remained within the same group, whilst 66.7% of those with no exacerbations were stable over 12 months. Similar results were obtained when patients with exacerbations were divided into those with 1 exacerbation within the 12-month period (n = 64; blood eosinophils were stable in 71.9%) and those with ≥2 exacerbations (n = 35; blood eosinophils were stable in 74.3%).
Subgroup analysis of blood eosinophil stability according to ICS use showed similar results in those using ICS (n = 181; rho = 0.58, p < 0.001) and those not using ICS (n = 44; rho = 0.47, p = 0.001). For patients using on ICS, 70.2% had blood eosinophil counts that remained in the same group over 12 months, while this was 65.9% for those not using ICS.
Discussion
The main findings were that (1) blood eosinophil stability over 12-months was excellent when analysed by ICC (0.84), (2) regression analysis showed greater variability at higher eosinophil counts (3) 69.3% of patients remained stable within the same category (4) movement between groups was more likely when baseline values were closer to a threshold. The main clinical usefulness of these findings is to demonstrate that the majority of COPD patients remain within the same blood eosinophil category (defined by GOLD) after 1 year. This provides reassurance regarding treatment decisions using this biomarker.
GOLD 2020 now states that the thresholds of < 100 cells/μL and > 300 cells/μL are “estimates, rather than precise cut-off values” with respect to the prediction of ICS effects [10]. This concept is important when considering movement across these thresholds after repeat testing, which occurred in approximately 30% of patients in this study. The continuous nature of the blood eosinophil count – ICS response relationship means that small numerical changes after a repeat test are unlikely to be associated with a significant change in ICS responsiveness. We observed that movement across a threshold was more likely for baseline measurements that were closer to the threshold; this appears to be natural measurement variation across a threshold rather than a significant change in the pathophysiology of an individual. We suggest that these small numerical movements across a threshold should not change the original clinical interpretation based on the baseline blood eosinophil count. Similarly, 1-year stability in COPD patients (n = 27,557) at 12-months has been reported (ICC = 0.7), with lower blood eosinophil reliability for measurements close to thresholds [11]. Average blood eosinophil counts for repeated measurements in clinical practice may overcome this variability [11].
Previous studies have shown similar ICC values for blood eosinophil counts [6, 7, 11]. E.g. Southworth et al. studied a smaller COPD cohort (n = 82) using thresholds < 150, 150- < 300 and ≥ 300 cells/μL; ICC = 0.89 and 0.87 at 6 months and 2 years respectively, with 71 and 64% respectively of patients remaining within the same category [6]. Greulich et al. (n = 334) similarly found those with blood eosinophils < 150 cells/μL had greater stability over 18 months [12]. The importance of our results is that we have used the thresholds defined by GOLD. Furthermore, we observed that 192/225 (85.3%) patients had eosinophil measurements that were stable using the 100 eosinophils/μL threshold. Similarly, Southworth et al. reported 91 and 85% stability at 6 months and > 2 years respectively using 100 eosinophils/μL [6]. Using only the lower eosinophil threshold in the GOLD report therefore appears to provide stable results in the majority of cases.
More patients moved across the threshold from the < 100 cells/μL group (52.6%) at baseline compared to the ≥ 300 cells/μL group (37.5%). Most of this variation from the < 100 cells/μL group (n = 36/38) resulted in movement to the adjacent group (100- < 300 cells/μL). The discordance between variability of absolute eosinophil numbers and movement across a threshold can be attributed to the wider measurement range at ≥ 300 cells/μL e.g. 20% (6/30) of individuals who remained ≥ 300 cells/μL had an absolute change ≥ 200 cells/μL, while all patients (n = 18) who remained < 100 cells/μL changed < 50 cells/μL.
Increased blood eosinophil counts in a subset of COPD patients has been demonstrated even when individuals with asthma or allergy are excluded [13]. The mechanism causing higher blood eosinophil counts in a subset of COPD patients is unclear. Blood eosinophils can be raised in the context of parasitic infections, but this was unlikely to be the cause in this UK based cohort study [14].
There was a high percentage of ICS use in our study population (80.4%), likely due to patients being recruited across 3 hospital based research centres rather than primary care. It would be interesting to see similar data in patients in primary care, with lower exacerbation risk and ICS use. Our data had a 1 year follow up, and future analyses could extend stability analysis to longer time periods.
In conclusion, approximately 70% of blood eosinophil measurements remained in the same category over 1 year using the GOLD 2019 thresholds. Small numerical changes may cause movement across a threshold.
Supplementary information
Abbreviations
- ANOVA
Analysis of Variance
- CAT
COPD assessment test
- COPD
Chronic obstructive pulmonary disease
- FEV1
Forced expiratory volume in 1 s
- GOLD
Global Initiative for Chronic Obstructive Lung Disease
- ICC
Interclass correlation coefficient
- ICS
Inhaled corticosteroids
- RCA
Repeatability coefficient analysis
Authors’ contributions
DS was responsible for the concept and design of the study. GL analysed the data and DS oversaw all analyses. GL and DS were responsible for data interpretation and drafting the manuscript. TS, UK, GD, CEB, JW revised the manuscript critically for intellectual content. All authors have approved the final version to be published and are jointly accountable for all aspects of the work.
Funding
This study was funded by the MRC (United Kingdom). DS is supported by the NIHR Manchester BRC.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Ethics approval and consent to participate
The COPDMAP prospective observational cohort study (www.copdmap.org) recruited patients from 3 sites (Manchester, Leicester and London). The study was approved by local Research Ethics committees at each site (11/L0/1630; 10/H/1003/108; 07/H0406/157). All participants provided written informed consent prior to recruitment.
Consent for publication
Not applicable.
Competing interests
GL, TS and UK have nothing to disclose. GD reports personal fees from Micom Ltd., personal fees from Astra-Zeneca, outside the submitted work. CB reports grants from MRC, grants from NIHR, during the conduct of the study; grants and personal fees from AZ/MedImmune, from GSK, grants and personal fees from Chiesi, grants and personal fees from Novartis, personal fees from Sanofi, personal fees from Regeneron, grants and personal fees from BI, grants and personal fees from 4DPharma, grants and personal fees from Mologic, grants from Merck, from TEVA, outside the submitted work. JW reports grants from GSK, grants from Johnson and Johnson, other from Novartis, other from Boehringer Ingelheim, other from Astra Zeneca, other from GSK, grants from GSK, grants from Astra Zeneca, grants from Boehringer Ingelheim, grants from Novartis, outside the submitted work. DS reports personal fees from AstraZeneca, personal fees from Boehringer Ingelheim, personal fees from Chiesi, personal fees from Cipla, personal fees from Genentech, personal fees from GlaxoSmithKline, personal fees from Glenmark, personal fees from Menarini, personal fees from Mundipharma, personal fees from Novartis, personal fees from Peptinnovate, personal fees from Pfizer, personal fees from Pulmatrix, personal fees from Theravance, personal fees from Verona, outside the submitted work.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12931-020-1279-4.
References
- 1.Siddiqui SH, Guasconi A, Vestbo J, Jones P, Agusti A, Paggiaro P, Wedzicha JA, Singh D. Blood Eosinophils: a biomarker of response to Extrafine Beclomethasone/Formoterol in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;192(4):523–525. doi: 10.1164/rccm.201502-0235LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lipson DA, Barnhart F, Brealey N, Brooks J, Criner GJ, Day NC, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–1680. doi: 10.1056/NEJMoa1713901. [DOI] [PubMed] [Google Scholar]
- 3.Singh Dave, Agusti Alvar, Anzueto Antonio, Barnes Peter J., Bourbeau Jean, Celli Bartolome R., Criner Gerard J., Frith Peter, Halpin David M.G., Han Meilan, López Varela M. Victorina, Martinez Fernando, Montes de Oca Maria, Papi Alberto, Pavord Ian D., Roche Nicolas, Sin Donald D., Stockley Robert, Vestbo Jørgen, Wedzicha Jadwiga A., Vogelmeier Claus. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. European Respiratory Journal. 2019;53(5):1900164. doi: 10.1183/13993003.00164-2019. [DOI] [PubMed] [Google Scholar]
- 4.Bafadhel M, Peterson S, De Blas MA, Calverley PM, Rennard SI, Richter K, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018;6(2):117–126. doi: 10.1016/S2213-2600(18)30006-7. [DOI] [PubMed] [Google Scholar]
- 5.Bafadhel M, Pavord ID, Russell REK. Eosinophils in COPD: just another biomarker? Lancet Respir Med. 2017;5(9):747–759. doi: 10.1016/S2213-2600(17)30217-5. [DOI] [PubMed] [Google Scholar]
- 6.Southworth T, Beech G, Foden P, Kolsum U, Singh D. The reproducibility of COPD blood eosinophil counts. Eur Respir J. 2018;52(1):1800427. doi: 10.1183/13993003.00427-2018. [DOI] [PubMed] [Google Scholar]
- 7.Oshagbemi OA, Burden AM, Braeken DCW, Henskens Y, Wouters EFM, Driessen JHM, et al. Stability of blood Eosinophils in patients with chronic obstructive pulmonary disease and in control subjects, and the impact of sex, age, smoking, and baseline counts. Am J Respir Crit Care Med. 2017;195(10):1402–1404. doi: 10.1164/rccm.201701-0009LE. [DOI] [PubMed] [Google Scholar]
- 8.Kolsum U, Donaldson GC, Singh R, Barker BL, Gupta V, George L, et al. Blood and sputum eosinophils in COPD; relationship with bacterial load. Respir Res. 2017;18(1):88. doi: 10.1186/s12931-017-0570-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martin Bland J, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327(8476):307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 10.Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2020 Report). Available at URL: www.goldcopd.org. Published in Fontana, WI, USA.
- 11.Landis SH, Suruki R, Hilton E, Compton C, Galwey NW. Stability of blood eosinophil count in patients with COPD in the UK clinical practice research Datalink. COPD. 2017;14(4):382–388. doi: 10.1080/15412555.2017.1313827. [DOI] [PubMed] [Google Scholar]
- 12.Greulich T, Mager S, Lucke T, Koczulla AR, Bals R, Fähndrich S, et al. Longitudinal stability of blood eosinophil count strata in the COPD COSYCONET cohort. Int J Chron Obstruct Pulmon Dis. 2018;13:2999–3002. doi: 10.2147/COPD.S165909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh D, Kolsum U, Brightling CE, Locantore N, Agusti A, Tal-Singer R. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J. 2014;44(6):1697 LP–1691700. doi: 10.1183/09031936.00162414. [DOI] [PubMed] [Google Scholar]
- 14.Ramirez GA, Yacoub M-R, Ripa M, Mannina D, Cariddi A, Saporiti N, et al. Eosinophils from physiology to disease: a comprehensive review. Biomed Res Int. 2018;9095275. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].