Abstract
Background
Poor diet and insufficient physical activity are major risk factors for non‐communicable diseases. Developing healthy diet and physical activity behaviors early in life is important as these behaviors track between childhood and adulthood. Parents and other adult caregivers have important influences on children's health behaviors, but whether their involvement in children's nutrition and physical activity interventions contributes to intervention effectiveness is not known.
Objectives
• To assess effects of caregiver involvement in interventions for improving children's dietary intake and physical activity behaviors, including those intended to prevent overweight and obesity
• To describe intervention content and behavior change techniques employed, drawing from a behavior change technique taxonomy developed and advanced by Abraham, Michie, and colleagues (Abraham 2008; Michie 2011; Michie 2013; Michie 2015)
• To identify content and techniques related to reported outcomes when such information was reported in included studies
Search methods
In January 2019, we searched CENTRAL, MEDLINE, Embase, 11 other databases, and three trials registers. We also searched the references lists of relevant reports and systematic reviews.
Selection criteria
Randomised controlled trials (RCTs) and quasi‐RCTs evaluating the effects of interventions to improve children's dietary intake or physical activity behavior, or both, with children aged 2 to 18 years as active participants and at least one component involving caregivers versus the same interventions but without the caregiver component(s). We excluded interventions meant as treatment or targeting children with pre‐existing conditions, as well as caregiver‐child units residing in orphanages and school hostel environments.
Data collection and analysis
We used standard methodological procedures outlined by Cochrane.
Main results
We included 23 trials with approximately 12,192 children in eligible intervention arms. With the exception of two studies, all were conducted in high‐income countries, with more than half performed in North America. Most studies were school‐based and involved the addition of healthy eating or physical education classes, or both, sometimes in tandem with other changes to the school environment. The specific intervention strategies used were not always reported completely. However, based on available reports, the behavior change techniques used most commonly in the child‐only arm were "shaping knowledge," "comparison of behavior," "feedback and monitoring," and "repetition and substitution." In the child + caregiver arm, the strategies used most commonly included additional "shaping knowledge" or "feedback and monitoring" techniques, as well as "social support" and "natural consequences."
We considered all trials to be at high risk of bias for at least one design factor. Seven trials did not contribute any data to analyses. The quality of reporting of intervention content varied between studies, and there was limited scope for meta‐analysis. Both validated and non‐validated instruments were used to measure outcomes of interest. Outcomes measured and reported differed between studies, with 16 studies contributing data to the meta‐analyses. About three‐quarters of studies reported their funding sources; no studies reported industry funding. We assessed the quality of evidence to be low or very low.
Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component
Seven studies compared dietary behavior change interventions with and without a caregiver component. At the end of the intervention, we did not detect a difference between intervention arms in children's percentage of total energy intake from saturated fat (mean difference [MD] −0.42%, 95% confidence interval [CI] −1.25 to 0.41, 1 study, n = 207; low‐quality evidence) or from sodium intake (MD −0.12 g/d, 95% CI −0.36 to 0.12, 1 study, n = 207; low‐quality evidence). No trial in this comparison reported data for children's combined fruit and vegetable intake, sugar‐sweetened beverage (SSB) intake, or physical activity levels, nor for adverse effects of interventions.
Physical activity interventions with a caregiver component versus interventions without a caregiver component
Six studies compared physical activity interventions with and without a caregiver component. At the end of the intervention, we did not detect a difference between intervention arms in children's total physical activity (MD 0.20 min/h, 95% CI −1.19 to 1.59, 1 study, n = 54; low‐quality evidence) or moderate to vigorous physical activity (MVPA) (standard mean difference [SMD] 0.04, 95% CI −0.41 to 0.49, 2 studies, n = 80; moderate‐quality evidence). No trial in this comparison reported data for percentage of children's total energy intake from saturated fat, sodium intake, fruit and vegetable intake, or SSB intake, nor for adverse effects of interventions.
Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component
Ten studies compared dietary and physical activity interventions with and without a caregiver component. At the end of the intervention, we detected a small positive impact of a caregiver component on children's SSB intake (SMD −0.28, 95% CI −0.44 to −0.12, 3 studies, n = 651; moderate‐quality evidence). We did not detect a difference between intervention arms in children's percentage of total energy intake from saturated fat (MD 0.06%, 95% CI −0.67 to 0.80, 2 studies, n = 216; very low‐quality evidence), sodium intake (MD 35.94 mg/d, 95% CI −322.60 to 394.47, 2 studies, n = 315; very low‐quality evidence), fruit and vegetable intake (MD 0.38 servings/d, 95% CI −0.51 to 1.27, 1 study, n = 134; very low‐quality evidence), total physical activity (MD 1.81 min/d, 95% CI −15.18 to 18.80, 2 studies, n = 573; low‐quality evidence), or MVPA (MD −0.05 min/d, 95% CI −18.57 to 18.47, 1 study, n = 622; very low‐quality evidence). One trial indicated that no adverse events were reported by study participants but did not provide data.
Authors' conclusions
Current evidence is insufficient to support the inclusion of caregiver involvement in interventions to improve children's dietary intake or physical activity behavior, or both. For most outcomes, the quality of the evidence is adversely impacted by the small number of studies with available data, limited effective sample sizes, risk of bias, and imprecision. To establish the value of caregiver involvement, additional studies measuring clinically important outcomes using valid and reliable measures, employing appropriate design and power, and following established reporting guidelines are needed, as is evidence on how such interventions might contribute to health equity.
Plain language summary
Effects of involving parents and other adult caregivers in children's diet and physical activity interventions
Review question
Does it make a difference if parents or other adult caregivers are involved in interventions to encourage children to eat healthier or be more physically active?
Background
Diet and physical activity behaviors are important determinants of health. Parents and other adult caregivers have an essential role in shaping children's health habits by controlling availability of and access to healthy foods and opportunities to be active; supporting, encouraging, and role‐modeling healthy behaviors; and adopting supportive feeding styles and practices. For these reasons, it often is argued that parent and caregiver involvement in children's diet and physical activity interventions is important; however, it remains unclear if involvement of parents and caregivers actually provides benefit.
Objectives
We assessed the effects of involving parents or other adult caregivers in children's healthy eating and physical activity interventions compared to the effects of the same child interventions without a parent or caregiver component. We were particularly interested in understanding effects on children's dietary intake, children's physical activity levels, and adverse effects of interventions.
Study characteristics
We found 23 studies, published between 1982 and 2019, that implemented diet interventions, physical activity interventions, or combined diet and physical activity interventions with children or adolescents, and evaluated the effects of adding an intervention component involving parents or other adult caregivers. Approximately 12,192 children aged 2 to 18 years were examined. More than half of studies took place in North America, and all but two were conducted in high‐income countries. Most studies were school‐based and involved the addition of healthy eating or physical education classes, or both, sometimes in tandem with other changes to the school environment. The breadth of information provided about intervention content varied between studies. The most commonly used intervention techniques were those aimed at shaping participants' knowledge, such as providing instruction about how to perform a behavior (e.g. dance, cooking lessons). About three‐quarters of studies reported their funding source; no studies reported industry funding.
Key results
The findings of this review suggest that adding a parent or caregiver component to dietary behavior change interventions or physical activity interventions may make little or no difference to children's dietary intake or physical activity levels. For interventions that target both diet and physical activity behaviors, involving a parent or caregiver probably slightly reduces children's sugar‐sweetened beverage intake by the end of the intervention. We do not know whether any of these types of interventions result in adverse effects because these data are not available.
Quality of evidence
Overall, the evidence from studies is of low or very low quality, which means that we are uncertain about study results.
Currentness of evidence
The evidence is current to January 2019.
Summary of findings
Background
Description of the condition
Non‐communicable diseases (NCDs), including cardiovascular diseases, cancer, type 2 diabetes mellitus, chronic respiratory diseases, and chronic kidney disease, are the leading causes of disability worldwide (Lozano 2012), and they account for more than two‐thirds of all global deaths (NCD Countdown 2030 Collaborators 2018). In 2015, the United Nations set reducing the probability of dying between 30 years and 70 years of age from NCDs as Sustainable Development Goal (SDG) target 3.4 (United Nations 2015). Poor diet and insufficient physical activity are important independent risk factors for NCD development and for obesity, and are leading contributors to the global burden of disease (Forouzanfar 2016; GBD 2017 Diet Collaborators 2019). In fact, recent research suggests that poor diet is responsible for more deaths globally than any other risk factor, including smoking tobacco (GBD 2017 Diet Collaborators 2019). In light of this impact, diet and physical activity behaviors have been identified as priority areas for public health action (Beaglehole 2011; WHO 2013; WHO 2016). Because these behaviors develop early in life, children and adolescents are a target population for prevention (WHO 2013; WHO 2016).
Low consumption of nutritious foods, such as fruits, vegetables, whole grains, nuts, and seeds, is a major contributor to disease burden (GBD 2017 Diet Collaborators 2019). Meta‐analyses have shown that fruits and vegetables have a significant protective effect for ischemic heart disease and stroke (Gan 2015; Hu 2014), and it is likely that they protect against some types of cancer (Marmot 2007; Wang 2014). The World Health Organization (WHO) recommends consuming at least 400 grams of fruits and vegetables per day (equivalent to five 80‐gram servings) to prevent chronic diseases (WHO 2003). However, an estimated 78% of the world population does not meet this recommendation (Hall 2009). Similarly, there is strong evidence linking increased intake of whole grains, nuts, and seeds to reduced risk of cardiovascular disease and type 2 diabetes (Afshin 2014; Ye 2012), but low consumption of these foods is widespread (GBD 2017 Diet Collaborators 2019; Micha 2015). In 2017, low intake of whole grains was the leading dietary risk factor for mortality among women and the second most important risk factor for mortality among men (GBD 2017 Diet Collaborators 2019). Other dietary factors associated with health benefits include omega‐3 fatty acids from seafood, fiber, polyunsaturated fatty acids, milk, and calcium (GBD 2017 Diet Collaborators 2019).
Reducing intake of sodium, processed and red meats, trans fats, and sugar‐sweetened beverages (SSBs) is recommended to promote population health and to prevent NCDs (GBD 2017 Diet Collaborators 2019; UN General Assembly 2012; WHO 2013). For decades, sodium intake has been associated with hypertension and NCDs, particularly cardiovascular disease (He 2009). The WHO recommends sodium intake no greater than 2 grams per day (equivalent to 5 grams of salt) (WHO 2003), but most populations consume much more (Brown 2009; GBD 2017 Diet Collaborators 2019). In 2010, global mean sodium intake was nearly twice the recommended limit (Powles 2013). Findings from prospective studies have shown consumption of processed and red meats to be associated with type 2 diabetes and colorectal cancer (Chan 2011; Micha 2012). There is also a link between processed meat and ischemic heart disease, likely due in part to the high sodium content of processed meat (Micha 2012). Evidence from controlled trials and observational studies indicates that trans fatty acids also adversely affect cardiovascular indicators and increase risk of ischemic heart disease (Mozaffarian 2009; Teegala 2009). Furthermore, meta‐analyses of prospective studies have found SSB consumption to be associated with weight gain (Malik 2013), type 2 diabetes (Imamura 2015; Malik 2010), hypertension (Xi 2015), ischemic heart disease (Huang 2014; Xi 2015), and chronic kidney disease (Cheungpasitporn 2014).
At the same time, physical activity is associated with numerous health benefits (Lee 2012), including protection against cardiovascular disease (Sofi 2008), type 2 diabetes (Jeon 2007), certain types of cancer (Thune 2001), and cardiovascular disease−related death (Lee 2012; Nocon 2008). Despite this, available data suggest a global inactivity crisis. Worldwide, 31% of adults and 80% of adolescents do not meet minimum recommendations for physical activity (Hallal 2012). A 15‐country comparison involving high‐, middle‐, and low‐income countries found that no countries had at least 80% of children and adolescents meeting physical activity guidelines (Tremblay 2014). Insufficient physical activity accounts for more than 5.3 million deaths per year, or 9% of premature mortality (Lee 2012). Even among physically active people, prolonged sedentary behavior is associated with higher risk of type 2 diabetes, cardiovascular disease, and cardiovascular and all‐cause mortality (Biswas 2015; Wilmot 2012).
In all world regions, the prevalence of obesity among children and adolescents has increased in recent decades (Black 2013; De Onis 2010; Lobstein 2015; Ng 2014). A global shift in diet toward highly processed foods, meat, and dairy products, combined with increases in sedentary behavior, is believed to have contributed to this phenomenon (Popkin 2013). Social inequalities in child and adolescent obesity are well documented. Although prevalence is highest in high‐income countries, most overweight children younger than five years live in low‐ and middle‐income countries (Black 2013). In high‐income countries, excess weight is more common among socially disadvantaged groups, but the inverse may be true in low‐ and middle‐income countries (Barriuso 2015; Chung 2016; Dinsa 2012; Wu 2015). Epidemiologic evidence suggests that diet quality and activity levels follow a socioeconomic gradient. In high‐income countries, greater socioeconomic position is associated with higher‐quality diets, more physical activity, and less sedentary time (Bauman 2012; Darmon 2008; Mayén 2014; Mielke 2016; Stalsberg 2010). High levels of obesity appear to be more prevalent in high‐income countries with greater income inequality than in high‐income countries with less income inequality (Wilkinson 2011). Data from low‐ and middle‐income countries are more limited, but available information suggests that associations between social advantage and obesity‐related behaviors differ from those observed in high‐income countries. For instance, in low‐ and middle‐income countries, adolescents from the wealthiest households appear to be the most sedentary (Mielke 2016). One reason for this could be that lower socioeconomic groups have to rely on walking or cycling for transportation and may be more likely to work in physically demanding jobs, such as farm or factory labor. For the most disadvantaged, obesity may co‐occur with undernutrition or micronutrient deficiencies due to common underlying factors or physiological links (Tzioumis 2014).
Overweight conditions in childhood and adolescence are associated with immediate and longer‐term health risks and decreased quality of life (Buttitta 2014; Daniels 2009). Virtually every organ system is adversely impacted by excess body weight, including cardiovascular, metabolic, pulmonary, gastrointestinal, and skeletal systems. Related health conditions in overweight and obese youth include cardiovascular disease symptoms, type 2 diabetes, breathing disorders, and fatty liver disease (Daniels 2009; Pulgarón 2014). Excess adiposity during childhood also can influence pubertal development in both boys and girls (Solorzano 2010). In addition, overweight children and adolescents experience psychological comorbidities such as internalizing disorders (e.g. anxiety, depression), externalizing disorders (e.g. impulsivity, attention deficit hyperactivity disorder), sleep problems, and uncontrolled eating (Puder 2010; Pulgarón 2014).
There is a strong correlation between childhood obesity and adult obesity (Simmonds 2016). Current trends suggest that young people today—particularly those from marginalized or otherwise vulnerable population groups—could suffer greater illness and live shorter lives than previous generations (Olshansky 2005). Developing healthy diet and physical activity behaviors during childhood and adolescence is an important step in preventing obesity and NCDs, particularly because these behaviors are likely to track into adulthood (Craigie 2011). For example, long‐term prospective cohort studies have found that diet and television viewing habits in childhood are predictors of similar behaviors decades later (Mikkilä 2005; Smith 2015). Consequently, early intervention is emphasized to instil healthy behaviors and to prevent the onset of overweight and obesity.
Description of the intervention
Interventions to improve children's and adolescents' health behaviors often encompass multiple components, including education, environmental modifications, and caregiver involvement. Narrative reviews have consistently argued that involving parents or other adult caregivers is important (Bautista‐Castaño 2004; Golan 2004; Lindsay 2006; McLean 2003; Sharma 2006). For childhood obesity interventions, some meta‐analyses have shown that parent and family involvement contributes to their success (Niemeier 2012; Young 2007), although these benefits may not be retained in the long run (Yavuz 2015). Caregiver involvement could comprise a range of behavior change techniques such as providing information or instruction, prompting intention formation, identifying barriers, self‐monitoring, offering opportunities for social comparison, or restructuring environments (Golley 2011). However, interventions that involve caregivers show inconsistent effectiveness (Stice 2006), and it is unclear which kinds of caregiver involvement lead to more effective outcomes. Without this information, it is not possible to specify the types of caregiver involvement and intervention strategies that may promote behavior change.
How the intervention might work
Parents and other adult caregivers have important influences on child development and play an essential role in shaping children's and adolescents' diet and physical activity habits by providing the contextual environment within which they develop these behaviors (De Vet 2011; Draper 2015; Golan 2004; Lindsay 2006; Patrick 2005). Caregivers' involvement in interventions could work through a number of mechanisms. Physical aspects of the home environment, which are largely controlled by caregivers, appear to be related to what children eat and to their physical activity levels. For example, less access to fruits and vegetables at home is associated with lower consumption among children and adolescents (Pearson 2009), and the presence of electronic media in children's bedrooms has been related to sedentary behavior (Tandon 2012). Outside of the home, caregivers may serve as gatekeepers to physical activity by establishing the activities in which children can participate.
Caregivers also have an important psychosocial influence on children's habit formation. Children are more likely to eat a healthy diet when their caregivers model healthy eating themselves (De Vet 2011; Golan 2004; Patrick 2005; Pearson 2009; Skouteris 2011). Additionally, caregivers' feeding styles and practices and nutrition knowledge, as well as food beliefs, attitudes, and preferences, have been shown to be associated with children's diets (Blissett 2011; Clark 2007; Draper 2015; Golan 2004; Patrick 2005; Scaglioni 2011; Skouteris 2011). Consequently, it follows that intervention activities targeted at caregivers may be beneficial for supporting and promoting healthy eating and physical activity among children and adolescents.
Current theories of child development are based on the transactional view, which emphasizes the interdependent and bidirectional effects of interactions between the child and his or her social settings (Sameroff 2010). Caregivers and children are continuously interacting, both shaping and being shaped by the other's actions. As children move from early childhood into adolescence, caregiver and family influences often decrease as peer influences become more important (National Research Council 2004; Sameroff 2010). However, caregivers continue to influence diet, physical activity, and sedentary behaviors (Draper 2015). Given the continual shifts in child−caregiver relationships as children grow, the most beneficial forms of caregiver involvement and behavior change techniques to promote child behavior change may differ for different child age groups. A systematic review of universal parental support interventions to promote healthy dietary habits and physical activity behaviors or to prevent overweight and obesity among children found that these interventions appear to work better when children are younger (Kader 2015).
Why it is important to do this review
Improving health‐related behavior among children and adolescents has the potential to improve the overall health of the next generation and to reduce the burden of NCDs. At least four Cochrane Reviews have indicated a need for greater attention to the involvement of caregivers in behavior change interventions. Waters 2011 and Brown 2019 evaluated effects of childhood obesity prevention interventions but did not distinguish which intervention components contributed to favorable effects. Luttikhuis 2009 focused on treatment of children with obesity and included studies with or without family involvement, but review authors did not perform a subgroup analysis on family involvement. Loveman 2015 examined the efficacy of diet, physical activity, and behavioral interventions delivered to parents only for treatment of overweight and obesity in children and found limited evidence that parental interventions helped reduce child body mass index (BMI).
A number of other reviews have explored the contributions of caregiver involvement (in particular, parents) to children's nutrition and physical activity interventions (Golley 2011; Hingle 2010; Kader 2015; Ling 2017; Morris 2015; Niemeier 2012; O'Connor 2009; Van Lippevelde 2012). Some reviews concluded that caregiver involvement promotes intervention success (Golley 2011; Niemeier 2012), but others suggested that evidence to support the claim that caregiver involvement is important in children's nutrition and physical activity interventions is lacking (Hingle 2010; Kader 2015; Ling 2017; Morris 2015; O'Connor 2009; Van Lippevelde 2012). In addition, the effects of different behavior change techniques employed with caregivers are not yet established.
Our review aimed to fill this evidence gap by updating and expanding upon a previous review (Van Lippevelde 2012), which sought to assess the contributions of parental (i.e. caregiver) involvement to intervention effectiveness. The previous review focused on "determining the impact of parental involvement in school‐based obesity prevention interventions" (targeting both nutrition‐ and physical activity−related behaviors) for children aged 6 to 18 years and considered evidence published between 1990 and 2010. Our review incorporated a broader scope of research evidence by including both school‐based and non−school‐based interventions as well as studies targeting children and adolescents aged 2 to 18 years. When the data allowed, we considered which behavior change techniques were employed. To support the growing demand for information on effects of interventions on health equity, we also evaluated how the interventions were implemented, and whether study authors reported on sociodemographic factors known to be important from an equity perspective.
Objectives
To assess effects of caregiver involvement in interventions for improving children's dietary intake and physical activity behaviors, including those intended to prevent overweight and obesity
To describe intervention content and behavior change techniques employed, drawing from a behavior change technique taxonomy developed and advanced by Abraham, Michie, and colleagues (Abraham 2008; Michie 2011; Michie 2013; Michie 2015)
To identify content and techniques related to reported outcomes when such information was reported in included studies
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs) and quasi‐RCTs of parallel‐group design, with individuals or clusters as the unit of randomization. Due to the nature of our comparator interventions, we did not find cross‐over trials. In future updates of this review, should there be eligible RCTs with a cross‐over design, we will include data only from the first period for each arm to avoid risk of contamination. Please refer to Table 4 and to our protocol, Morgan 2017, for a full report of methods archived for use in future updates.
1. Methods planned in the protocol but not used in this review.
| Topic | Method |
| Unit of analysis issues |
Cluster‐randomized trials We will then combine the estimates and their corrected SEs from the cluster‐randomized trial with those from trials of parallel‐group design using the generic inverse variance method in Review Manager 2014 |
| Dealing with missing data | For interventions in which there is substantial attrition (≥ 15% for at least 1 of the groups) of trial participants (caregivers, children, or caregiver‐child units), we will report the attrition rate and perform sensitivity analyses (see "Sensitivity analysis") |
| Assessment of heterogeneity | If we identify unexplained heterogeneity, we will not pool results into an overall effect estimate but instead will present the individual effect sizes per study for the specific outcome, in a table |
| Assessment of reporting biases | If we have 10 or more studies included for an outcome, we will use funnel plots to assess the possibility of small‐study effects. In the case of asymmetry, we will consider various explanations such as publication bias, poor study design, and the effect of study size |
| Subgroup analysis and investigation of heterogeneity | When data allow, we will perform the subgroup analyses listed below, to explore substantial and considerable heterogeneity across studies
|
| Sensitivity analyses | When data allow, we will perform sensitivity analyses to assess the following, and will report results in tables
|
BCT: behavior change technique.
RCT: randomized controlled trial.
SE: standard error.
Types of participants
Caregiver−child units, where the child was aged 2 to 18 years and was actively involved in the intervention. We excluded caregiver−child units where the child was under two years of age because interventions for this age group are likely to be focused on complementary feeding (which is not the focus of this review) and are unlikely to include children as key intervention participants. We defined caregivers as parents, guardians, or other adults responsible for caring for the child in the home setting. We excluded caregiver−child units residing in orphanages and school hostel environments because the adult‐to‐child ratio and relationships might have differed from traditional home environments. A child could have had one or more caregivers involved in the intervention (e.g. mother, mother and father, a parent and a grandparent, foster parent[s]).
Caregiver−child units in which the child was of normal weight, overweight, or obese weight status were eligible. However, if a trial included only children with a pre‐existing health condition (e.g. diabetes mellitus, obesity, undernutrition), we excluded that trial because this review did not seek to assess interventions specifically meant as treatment. Thus, trials that included children from the general population—some of whom may have had pre‐existing health conditions—were eligible. We included caregivers regardless of their age, weight, nutritional status, or comorbidities.
We included trials conducted in any country (high‐, middle‐, and low‐income) that targeted caregiver−child units in any setting (e.g. school, community, home, primary health care), except inpatient hospital settings.
Types of interventions
Intervention group
Interventions to improve children's dietary intake or physical activity behavior, or both, with children as active participants and at least one component involving caregivers. For the caregiver component(s), caregiver participation could have been active or inactive. We defined active caregiver intervention components as those in which caregivers were asked to physically attend events or participate in other intervention activities. We defined inactive caregiver intervention components as those where caregiver participation was limited to providing information that did not require a response, for example, receipt of a newsletter or pamphlet. Interventions were delivered to children and to caregiver−child units in an individual or group context.
Control group
Interventions to improve children's dietary intake or physical activity behavior, or both, which did not include a component involving caregivers or included caregivers in only a marginal capacity. Multi‐component interventions were appropriate, as long as intervention components across groups were similar, except for specific caregiver involvement.
Comparisons
Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component
Physical activity interventions with a caregiver component versus interventions without a caregiver component
Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component
Types of outcome measures
Primary outcomes
Children's dietary intake (i.e. total energy intake, percentage of total energy intake from fat, percentage of total energy intake from saturated fat, percentage of total energy intake from trans fat, percentage of total energy from carbohydrates, percentage of total energy from protein, sodium intake, fruit and vegetable intake, sugar‐sweetened beverage [SSB] intake, and water intake), as measured by instruments such as 24‐hour dietary recalls and food frequency questionnaires
Children's physical activity levels (i.e. total physical activity, time spent in moderate to vigorous physical activity [MVPA], time spent in light physical activity [LPA], time spent in weight‐bearing physical activity, steps), as measured by instruments such as accelerometers, pedometers, and physical activity questionnaires
Adverse effects (as defined by trial authors), such as family conflict or disordered eating or activity behaviors
Secondary outcomes
Children's dietary quality, measured by dietary quality score, dietary diversity score, or similar measures
Children's sedentary behavior, measured by accelerometers, sedentary time questionnaires, or similar measures
Pevalence of overweight and obesity among children, as measured using reference cut‐points such as those produced by the World Health Organization (WHO) (WHO Multicentre Growth Reference Study Group 2006), the International Obesity Task Force (Cole 2000), or the US Centers for Disease Control and Prevention (CDC) (Kuczmarski 2002)
Children's body mass index (BMI) or weight‐for‐height parameter, as measured by, for example, WHO BMI‐for‐age or weight‐for‐height Z scores (WHO Multicentre Growth Reference Study Group 2006)
Caregiver's dietary intake (i.e. total energy intake, percentage of total energy intake from fat, percentage of total energy intake from saturated fat, percentage of total energy intake from trans fat, percentage of total energy from carbohydrates, percentage of total energy from protein, sodium intake, fruit and vegetable intake, SSB intake, water intake), measured by instruments such as 24‐hour dietary recalls and food frequency questionnaires
Caregiver's physical activity levels (i.e. total physical activity, time spent in MVPA, time spent in LPA, time spent in weight‐bearing physical activity, steps), measured by instruments such as accelerometers, pedometers, and physical activity questionnaires
Studies had to address at least one of the outcomes pre‐specified above to be eligible.
We reported data collected at time points during and after the intervention period ended (follow‐up). When relevant, and as data allowed, we grouped time points across studies. We also applied a grouping approach for results obtained from follow‐up periods after intervention completion.
Search methods for identification of studies
We ran the original searches in May 2017 and updated the searches in January 2019 to identify eligible studies, regardless of year, language, or publication status. When necessary, we sought Chinese to English translation.
Electronic searches
We searched the online databases listed below.
Cochrane CENTRAL Register of Studies Online (CRSO), in the Cochrane Library, which includes the Cochrane Developmental, Psychosocial and Learning Problems Specialised Register (searched January 14, 2019).
MEDLINE Ovid (1946 to January Week 1, 2019; searched January 15, 2019).
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid (searched January 15, 2019).
MEDLINE Epub Ahead of Print (searched January 15, 2019).
Embase Ovid (1974 to January 14, 2019; searched January 15, 2019).
Education Resources Information Center (ERIC) EBSCOhost (1966 to January 16, 2019).
Cumulative Index to Nursing and Allied Health Literature (CINAHL) Plus EBSCOhost (1937 to January 16, 2019).
Latin American and Caribbean Health Sciences Literature (lilacs.bvsalud.org/en; LILACS; searched January 18, 2019).
Cochrane Database of Systematic Reviews (CDSR; 2017, Issue 5), part of the Cochrane Library (searched January 14, 2019).
Database of Abstracts of Reviews of Effects (DARE; 2015, Issue 1; final issue), part of the Cochrane Library (searched May 8, 2017).
Epistimonikos (www.epistemonikos.org; searched January 16, 2019).
Conference Proceedings Citation Index−Science Web of Science (CPCI‐S; 1990 to January 16, 2019).
Conference Proceedings Citation Index−Social Science & Humanities Web of Science (CPCI‐SS&H; 1990 to January 16, 2019).
ProQuest Dissertations & Theses Global ProQuest (1980 to January 16, 2019).
Trials Register of Promoting Health Interventions (TRoPHI; eppi.ioe.ac.uk/webdatabases4/Intro.aspx?ID=12; searched January 16, 2019).
ClinicalTrials.gov (clinicaltrials.gov; searched January 14, 2019).
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; apps.who.int/trialsearch/default.aspx; searched January 14, 2019).
The strategies applied for each database are reported in Appendix 1.
Searching other resources
We screened the reference lists of included studies and relevant reviews to identify any additional trials that may not have been found by the electronic searches. For all included studies, we searched online for trial registration.
Data collection and analysis
Selection of studies
We imported all search results into the Covidence web‐based software platform for screening and extraction (Covidence). Working in pairs, four review authors (EHM, MF, RAS, US) and a research assistant independently screened the titles and abstracts of all records identified by the searches and applied the pre‐specified eligibility criteria to identify potentially eligible studies (Criteria for considering studies for this review). When at least one review author considered a study to be relevant, we obtained the full‐text report, and two review authors (EHM, US) independently assessed it for eligibility. In cases where we needed additional information to decide whether or not a study was eligible, we emailed trial authors for clarity (e.g. for more detail about the intervention or the randomization process). We resolved any discrepancies through discussion until we reached consensus. When necessary, we sought input from another review author (AS). We listed studies that required discussion to reach consensus regarding inclusion in the Characteristics of excluded studies tables, alongside reasons for exclusion. We recorded our decisions on all records in a PRISMA diagram (Moher 2009).
Data extraction and management
Working in pairs, four review authors (EHM, AS, MF, US) and a research assistant independently extracted data from included studies using a standardized, pre‐piloted data extraction form in Covidence. EHM reviewed all extracted data and resolved any discrepancies. When she had difficulty, EHM asked for the input of another review author (AS). For each included study, we extracted the information described below.
Methods: study design, study grouping, study aim, study period, total number of arms, description of study arms, number of clusters per arm (for cluster‐randomized trials), average cluster size (for cluster‐randomized trials), sample size justification and outcome used, unit of allocation, how missing data were handled, limitations reported by study authors, randomization ratio and stratification, and whether participants were offered compensation or incentives.
Population: recruitment methods, inclusion criteria, exclusion criteria, children's age, total number of participants randomized overall and by relevant group, baseline imbalances between relevant groups, total number of participants analyzed by relevant group, attrition by relevant group, and description of the sample for which baseline characteristics were reported.
Participants in each relevant intervention arm: PROGRESS‐Plus (child gender/sex, child mean age, race/ethnicity/culture/language, place of residence, caregiver education, religion, household income/socioeconomic status, social capital, caregiver work hours and other characteristics that may indicate disadvantage, disability, sexual orientation, caregiver civil status), child weight status, child diet, child physical activity, caregiver weight status, caregiver diet, and caregiver physical activity.
Intervention group details: brief name/description of the intervention (Template for Intervention Description and Replication [TIDieR] #1); focus of the intervention; behavior change techniques (BCTs) used, why—rationale, theory, or goal (TIDieR #2); how, where, and when and how much (TIDieR #6 to 8); who—providers (TIDieR #5); economic variables and resources required for replication; strategies to address disadvantage; subgroups; assessment time points (including time points during and after the intervention); co‐interventions; what—materials and procedures (TIDieR #3 to 4); tailoring (TIDieR #9); modifications (TIDieR #10); how well—planned and actual (TIDieR #11 to 12); and whether sensitivity analyses were conducted.
Comparison group details: brief name/description of the intervention (TIDieR #1); focus of the intervention; behavior change techniques (BCTs) used, why—rationale, theory, or goal (TIDieR #2); how, where, and when and how much (TIDieR #6 to 8); who—providers (TIDieR #5); economic variables and resources required for replication; strategies to address disadvantage; subgroups; assessment time points (including time points during and after the intervention); co‐interventions; what—materials and procedures (TIDieR #3 to 4); tailoring (TIDieR #9); modifications (TIDieR #10); how well—planned and actual (TIDieR #11 to 12); and whether sensitivity analyses were conducted.
Outcomes: for each outcome: measurement tool, whether the tool was validated, whether the tool was used as validated or adapted, person who measured or reported the outcome, units, total numbers in intervention and comparison groups, and end values or change indicated at each time point.
Other information: study name, country, setting, types of reports used, corresponding author's name and email address, reported conflicts of interest, and reported sponsorship source.
Risk of bias: high, low, or uncertain risk of bias together with a reason for the judgment; judgment criteria are outlined below in Assessment of risk of bias in included studies.
For English language reports, we contacted trial authors when reported information was unclear or contradictory, or when important details or data were missing. We entered extracted data into the Characteristics of included studies tables. To the extent that data allowed, EHM or US extracted the same information from studies awaiting classification and from ongoing studies and entered this information in the Characteristics of studies awaiting classification and Characteristics of ongoing studies tables, respectively.
When trial authors did not report or provide the number of children randomized with consent per relevant intervention arm, we estimated these values using information on total sample size, number of intervention arms, and the randomization ratio. When no information on the number of randomized children was reported, we used the number of children analyzed as an approximation. We documented these estimations in the relevant Characteristics of included studies tables.
When data allowed, we prioritized within‐group change values for analyses. When both end values and within‐group change values were presented, we extracted both, so that we could utilize the end value data to calculate the assumed risk for the "Summary of findings" tables.
Assessment of risk of bias in included studies
Working in pairs, four review authors (EHM, AS, MF, US) and a research assistant independently evaluated the risk of bias for included studies in Covidence. EHM and AS discussed these initial determinations and made final judgments. When different outcomes had different risks of bias, we indicated this in the "Risk of bias" table. To perform this evaluation, we used the following seven criteria for RCTs, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a).
Random sequence generation. Did each eligible participant have an equal chance of being allocated to the intervention or control group?
Allocation concealment. Was the randomization process kept strictly confidential (i.e. was each allocation unpredictable), especially from researchers and participants?
Blinding of participants and personnel. Did participants or personnel, or both, have any knowledge of the allocated interventions?
Blinding of outcome assessment. Did outcome assessors, or participants if outcomes were measured by self‐report, have any knowledge of the allocated interventions?
Incomplete outcome data. Was it clear why certain results or relevant outcome information was omitted? Also, was it clear how many people were randomized to each group, and whether (and if so, why) participants from the different groups dropped out or did not provide outcome data? We considered attrition bias with respect to total attrition and differential attrition. We regarded high total attrition to be rates ≥ 15% and high differential attrition for the two study arms to be rates ≥ 10%.
Selective reporting. Were reported outcomes in line with the trial's protocol or pre‐specified methods? Were the outcome data reported (or if not, could they be provided) by study authors to allow entry into meta‐analyses?
Other sources of bias. Was the study free from other problems that could put it at high risk of bias, including conflicts of interest and sources of bias identified by study authors?
Following procedures outlined in the Cochrane Handbook for Systematic Reviews of Interventions, we assigned each of these criteria one of three ratings: "low risk of bias," "high risk of bias," or "unclear risk of bias," alongside reasons for our ratings (Higgins 2011a). We resolved disagreements through discussion until reaching consensus, and, when needed, we asked another person with experience in Cochrane Reviews but who was not involved in our review for arbitration.
For cluster‐RCTs, we also added and assessed the domains listed below, per the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
Recruitment bias. Were trial participants included in the trial after the clusters were randomized?
Baseline imbalances. Were there substantial differences in important characteristics between clusters or between participants within a cluster?
Loss of clusters. Were clusters omitted from the analysis, or were there missing outcomes for individuals within clusters?
Incorrect analysis. Did trial authors fail to take clustering into account when performing the analysis?
We set out to assess comparability between individually randomized trials and cluster‐randomized trials using sensitivity analyses (see Sensitivity analysis), but data did not allow this.
Measures of treatment effect
We used Review Manager 5 (RevMan) to manage the data and carry out the review (Review Manager 2014). We reported all effect sizes alongside 95% confidences intervals (CIs).
Dichotomous data
For dichotomous data, we used the number of events as the numerator and the total sample size by outcome as the denominator in each comparison group and computed the risk ratio (RR).
Continuous data
For continuous data, we reported results by outcome as the difference in the mean change between intervention and control groups, and we computed the mean difference (MD). When studies reported continuous data using different units, we calculated the standardized mean difference (SMD) for continuous outcomes.
Unit of analysis issues
Multiple treatment groups
In trials where there was more than one intervention or control group, we first tried to create a single pair‐wise comparison following procedures provided in Higgins 2011b. When this was not appropriate or feasible, we chose the intervention and control pairs that were most relevant to our systematic review and excluded the other arms for analysis purposes (Higgins 2011b). We reported only data on relevant study arms in the Characteristics of included studies tables.
Cluster‐randomized trials
Regarding cluster‐randomized trials, we followed guidance on adjusting for clustering as outlined in Higgins 2011b. When study authors had appropriately adjusted for clustering, we included the data in a meta‐analysis by using the trial's reported effect estimate and its standard deviation (SD). In this case, we used the inverse variance analysis method in Review Manager 2014 for the meta‐analyses. When study authors did not adequately adjust the data relevant to our review for clustering (e.g. study authors adjusted for clustering in regression analyses but reported unadjusted change or end values by group), we applied the "approximate method," which involves calculating an effective sample size for comparison groups. We did this by dividing the original sample size by the design effect, which is 1 + (c − 1) ICC, where c is the average cluster size and ICC is the intracluster correlation coefficient. If available, we extracted the desired information from the study; otherwise, we emailed the trial authors. If we did not receive the information we needed, we estimated the ICC to be 0.01. The Cochrane Handbook for Systematic Reviews of Interventions indicates that values lower than 0.05 are typical (Higgins 2011b). Estimated values are arbitrary, but we preferred to use them to make adjustments due to the implausibility that the ICC is actually zero. For continuous data, only the sample size needed to be reduced; we did not change the means and SDs. For dichotomous outcomes, we divided the sample size and the number of people who experienced the event by the same design effect. We did not combine adjusted estimates from cluster‐randomized trials with those from trials using a parallel‐group design using the generic inverse variance analysis method in Review Manager 2014 as planned (Morgan 2017), because we had values for the totals, means, and SDs per group.
Dealing with missing data
When results reported for one or more outcomes of interest did not include data on all randomized study participants, we applied the "available case" analysis for dichotomous and continuous data. Following the approach described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b), we analysed "data for only those participants whose results are known...", and we judged the potential impact of the missing data as part of our assessment of risk of attrition bias.
When trial authors did not report all relevant statistics by outcome (e.g. sample size and number of events by group for dichotomous data and sample size, mean, SD by group for continuous data), we first explored whether it was possible to calculate or estimate the required data from other statistics reported using formulas specified in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c). If we were unable to calculate or estimate these statistics with reasonable confidence, we attempted to contact the trial authors by email. When we did not receive a response, or when we received a response for which we lacked confidence, we did not impute the missing values but reported available data in the text (see Effects of interventions).
For interventions in which there was substantial attrition (≥ 15%) of trial participants (caregivers, children, or caregiver−child units), we planned to perform sensitivity analyses (see Sensitivity analysis) to assess the impact of studies with substantial attrition. However, because only a small number of studies were included per meta‐analysis, we concluded that it was not useful to do so.
Assessment of heterogeneity
We assessed heterogeneity by outcome:
through visual inspection of forest plots, by looking at the physical overlap of CIs across included studies; or
-
statistically, by means of:
Chi2 test for heterogeneity;
I2 statistic to quantify heterogeneity; and
Tau2 statistic to measure the extent of heterogeneity among intervention effects across studies included in the meta‐analysis.
In our meta‐analyses, we considered substantial heterogeneity as I2 greater than 30% and either Chi2 less than 0.10 or Tau2 greater than 0. In cases of heterogeneity, we planned to perform subgroup analyses (see Subgroup analysis and investigation of heterogeneity), where feasible. We defined feasibility as at least five trials included in the meta‐analysis. Unexplained heterogeneity with more than five included studies did not arise in this review. See Table 4 in this review and refer to our protocol, Morgan 2017, for an explanation of how we plan to present data if we identify unexplained heterogeneity in future updates.
Assessment of reporting biases
Due to the small number of studies identified, we were unable to assess reporting bias. See Table 4 in this review and refer to our protocol, Morgan 2017, for a summary of how we will assess reporting bias in future updates of this review.
Data synthesis
Because of the probably diverse nature of eligible interventions (e.g. components of the intervention, methods of delivery, details on intervention providers and their training, number of sessions and their frequency and duration, BCTs employed), we anticipated heterogeneity across the included studies. Therefore, we used the random‐effects model of the inverse variance analysis method for all meta‐analyses (i.e. when we could pool the data from two or more studies). In cases where we had only one eligible study with relevant data by outcome, we used the fixed‐effect model. If we were unable to include data for a particular outcome in analyses, we reported available results in the text. When included studies did not provide change data and the end values were skewed, we included these data in meta‐analyses but indicated that this was the case. We determined that data were skewed if the mean minus two times the SD was less than zero.
When units of measurement differed between studies and we had to use the SMD, we did not pool change values and end values. When both change values and end values were available from one or more studies, we used the format of data (i.e. change values or end values) that facilitated pooling using the SMD.
When necessary outcome statistics were available, we presented meta‐analyses for end‐of‐intervention assessments and exact P values. For studies in which the trial authors calculated treatment effect but did not report complete outcome statistics, we reported the P value provided by study authors, which may be approximate (e.g. P < 0.05). Additionally, we grouped data collected at time points during and at the end of interventions into five categories: three months or less, longer than three months to six months or less, longer than six months to one year or less, longer than one year to two years or less, and longer than two years to three years or less. We made this decision to reflect the likely similarities in dose at a specific time point across studies of different durations. For example, we pooled midpoint data from a two‐year study using end‐of‐intervention data from a one‐year study. We presented follow‐up data separately.
To enable comparison and critique of the specific strategies used to change diet and physical activity behaviors in children and adolescents, we documented and categorized BCTs used in interventions in line with a pre‐defined taxonomy. We applied the BCT taxonomy (version 1; v1), which comprises a list of 93 hierarchically clustered BCTs (Michie 2015). We applied published definitions for each taxonomy item (Michie 2015). The BCT taxonomy (v1) can be used to reliably identify BCTs in lifestyle interventions for children and adolescents, including interventions specifically targeted at caregivers and families (Michie 2015). Because of the considerable power that would be required to use all items in a meta‐analysis, we examined taxonomy items in 16 clusters of conceptually coherent BCTs (Michie 2015). We reported the BCTs used in included studies in the table of Characteristics of included studies. Data from included studies did not allow us to perform subgroup analyses to examine effects of BCT clusters on each outcome (Subgroup analysis and investigation of heterogeneity).
We used the PROGRESS‐Plus checklist to guide our consideration of health equity. We analysed relevant information descriptively and considered the potential implications for health equity, and whether the review identified research needs relevant to promotion of health equity in the Discussion section. When data from primary studies allowed, we highlighted caregivers' education and paid work hours, household income, and setting (rural or urban) because these factors have been associated with children's eating and activity behaviors (Crockett 1995; Gordon‐Larsen 2000). Because recruitment strategies and mode of delivery may influence who is able to take part, we also extracted this information. When data allowed, we collected data on the intervention process and on implementation factors. We reported this information in the table of Characteristics of included studies.
Subgroup analysis and investigation of heterogeneity
We planned subgroups in the event of substantial heterogeneity in meta‐analyses, but we did not encounter cases in which this was feasible. Please refer to Table 4 in this review and to our protocol, Morgan 2017, for a summary of our planned subgroup analyses for future updates of this review.
Sensitivity analysis
We planned sensitivity analyses, but as with subgroup analyses, these were not feasible. For details on analyses planned and available for future updates of this review, please refer to Table 4 in this review and to our protocol (Morgan 2017).
"Summary of findings" table
Two review authors (EHM, AS) used the GRADE approach to assess the quality of evidence for seven outcomes addressed by the included studies: children's percentage of total energy intake from saturated fat, sodium intake, fruit and vegetable intake, SSB intake, total physical activity, MVPA, and adverse effects (Schünemann 2011). Grouped end‐of‐intervention data were assessed for each comparison. The GRADE approach assesses quality as high, moderate, low, or very low according to five criteria: limitations in study design and implementation (i.e. risk of bias), directness of evidence, heterogeneity, precision of effect estimates, and likelihood of publication bias. We used GRADEpro GDT (GRADEprofiler Guideline Development Tool) to import data from Review Manager 2014 and to construct "Summary of findings" tables for our three pre‐specified comparisons (see Types of interventions).
Results
Description of studies
Results of the search
The searches yielded a total of 41,867 records (41,850 from searching databases and 17 additional records from searching the reference lists of included studies and 32 relevant systematic reviews and conducting an Internet search for reported trial registrations). After removing duplicates, four review authors (EHM, MF, RAS, US) and a research assistant independently screened the titles and abstracts of 28,927 records and found 1138 that were potentially relevant. We retrieved the full‐text reports, and EHM and US screened them for eligibility. We were unable to assess the eligibility of 20 records, which were primarily dissertations or government documents published more than 20 years ago, or conference abstracts without a corresponding full‐text publication.
EHM and US made final decisions based on agreement on eligibility and resolved discrepancies through a process of consensus. We identified multiple reports of the same studies and determined that 23 studies (from 49 reports) met the inclusion criteria. See Figure 1 for a PRISMA diagram documenting our search and decision process.
1.
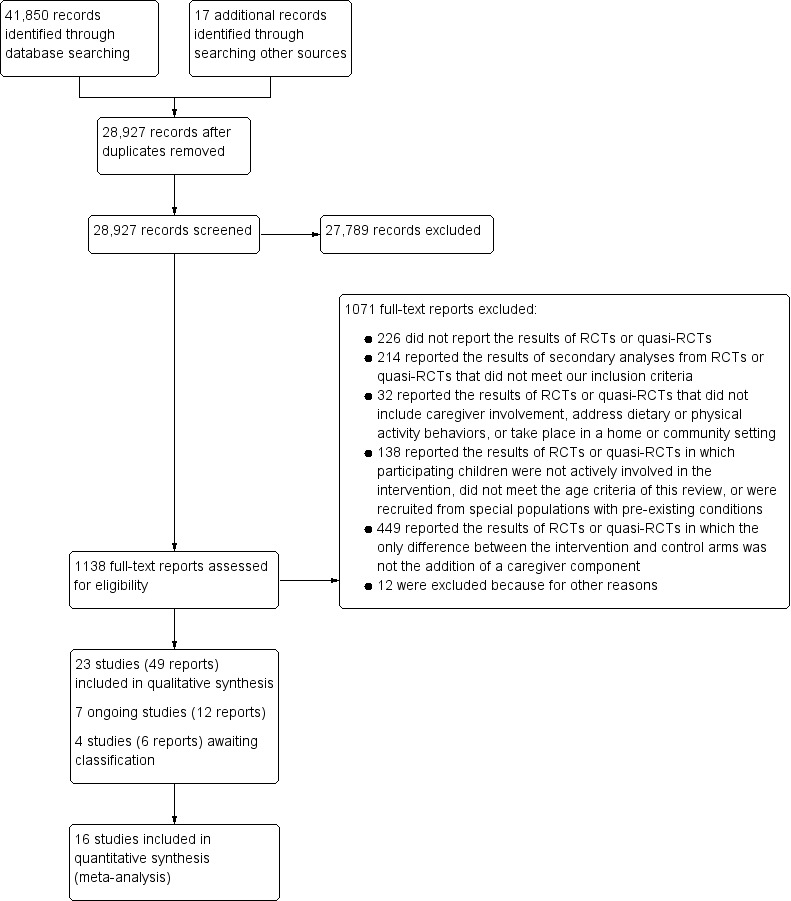
Study flow diagram.
We contacted the authors of all eligible studies with English language reports with requests for additional information, clarification, and further data. We received responses from 15 authors. Of these study authors, 11 provided additional information or clarification (although often not complete responses to all queries) (Ducheyne 2014a; Frenn 2013a; Haerens 2006a; Hopper 1992a; Kirks 1982a; Lin 2017a; Luepker 1996a; Perry 1988a; Vandongen 1995; Werch 2003a; Yeh 2018a), and three shared additional data (Haerens 2006a; Hopper 1992a; Luepker 1996a). The authors of four studies responded but did not share any additional information or data (Adamo 2017a; Crespo 2012a; Ievers Landis 2005; Petchers 1987). We received no response from the authors of seven studies (Alhassan 2018a; Baghurst 2014; Cottrell 2005; De Bock 2013a; De Bourdeaudhuij 2002; Dietsch 1990; Voll 2013). We did not reach out to the authors of one study published in Chinese—Wang 2007a—because no English language reports on this study were available.
Included studies
This review includes 23 studies with approximately 12,192 children in the eligible intervention arms (see Characteristics of included studies). Seven of these studies contributed no data to the analyses (Baghurst 2014; De Bourdeaudhuij 2002; Ducheyne 2014a; Frenn 2013a; Kirks 1982a; Petchers 1987; Wang 2007a). Below is a summary of the included studies; an interactive map of study characteristics can be explored at cebhc.co.za/eppi‐mapper.
Study design
Twenty studies were cluster‐RCTs with a parallel‐group design. The other three studies were individual RCTs with a parallel‐group design (Alhassan 2018a; Baghurst 2014; Werch 2003a).
Setting
All but two studies included in this review took place in a high‐income country. Lin 2017a took place in the Islamic Republic of Iran (hereafter referred to as Iran), and Wang 2007a took place in the People's Republic of China (hereafter referred to as China); both countries are classified as upper‐middle income by the World Bank. Sixteen studies were conducted in North America—14 in the USA (Alhassan 2018a; Baghurst 2014; Cottrell 2005; Crespo 2012a; Dietsch 1990; Frenn 2013a; Hopper 1992a; Ievers Landis 2005; Kirks 1982a; Luepker 1996a; Perry 1988a; Petchers 1987; Werch 2003a; Yeh 2018a), and two in Canada (Adamo 2017a; Voll 2013). Four studies took place in Europe, with three in Belgium (De Bourdeaudhuij 2002; Ducheyne 2014a; Haerens 2006a), and one in Germany (De Bock 2013a). One study was conducted in Australia (Vandongen 1995).
Participants were recruited through schools, preschools, or daycare centers for all studies except two: Ievers Landis 2005 recruited through the Girl Scouts Council in one region of the USA, and Alhassan 2018a recruited African American girls at community locations in a city in the USA. In all but four studies, recruitment and implementation of the the child‐only intervention (control group) were conducted at the same location. In one of these exceptions, all group activities took place at a centrally located elementary school, but newsletters were sent to the children's homes (Alhassan 2018a). In the second exception, children were asked to wear pedometers at all times (hence no specific intervention location) (Cottrell 2005). In the third, the intervention was delivered both at school and throughout the community (Crespo 2012a). In the fourth, intervention materials for the adolescent were mailed directly to his or her home (De Bourdeaudhuij 2002).
The caregiver component was most often delivered at home (Baghurst 2014; Crespo 2012a; De Bourdeaudhuij 2002; Ducheyne 2014a; Hopper 1992a; Kirks 1982a; Perry 1988a; Petchers 1987; Vandongen 1995; Voll 2013; Werch 2003a), at school (Alhassan 2018a; De Bock 2013a; Lin 2017a; Yeh 2018a), in an unspecified location where classes could be held (Ievers Landis 2005; Wang 2007a), online (Frenn 2013a), or through a combination of these media (Adamo 2017a; Dietsch 1990; Haerens 2006a; Luepker 1996a). In one study, caregivers received material at home and were asked to wear pedometers at all times (hence no specific intervention location) (Cottrell 2005).
Participants
Across the 23 studies, the age of child participants ranged from approximately 3 to 18 years. When trial authors reported child grade rather than age, we assumed the following age distributions: kindergarten, four to six years; first grade, five to seven years; second grade, six to eight years, third grade, seven to nine; fourth grade, 8 to 10; fifth grade 9 to 11; sixth grade, 10 to 12; seventh grade, 11 to 13; eighth grade, 12 to 14; ninth grade, 13 to 15; tenth grade, 14 to 16; eleventh grade, 15 to 17; and twelfth grade, 16 to 18.
Two studies limited recruitment to children between three and five years of age who were enrolled in a participating preschool (Yeh 2018a), or in a daycare facility (Adamo 2017a); one limited recruitment to children between four and six years of age who were enrolled in a participating preschool (De Bock 2013a); one limited recruitment to pre‐adolescent girls between 8 and 11 years of age who had not yet undergone menarche (Ievers Landis 2005); and one limited recruitment to girls ages 7 to 10 years (Alhassan 2018a). One study restricted recruitment to students at participating secondary schools between 15 and 18 years of age (De Bourdeaudhuij 2002), and another restricted recruitment to students at participating secondary schools between 13 and 18 years of age (Lin 2017a). For all other studies, grade in school was a primary determinant of eligibility: three recruited kindergarten students (Cottrell 2005; Crespo 2012a; Kirks 1982a); two recruited first grade students (Crespo 2012a; Kirks 1982a); four recruited second grade students (Baghurst 2014; Crespo 2012a; Kirks 1982a; Perry 1988a); five recruited third grade students (Baghurst 2014; Crespo 2012a; Kirks 1982a; Luepker 1996a; Wang 2007a); three recruited fourth grade students (Ducheyne 2014a; Voll 2013; Wang 2007a); four recruited fifth grade students (Frenn 2013a; Hopper 1992a; Voll 2013; Wang 2007a); five recruited sixth grade students (Frenn 2013a; Hopper 1992a; Petchers 1987; Vandongen 1995; Voll 2013); three recruited seventh grade students (Dietsch 1990; Frenn 2013a; Haerens 2006a); and three recruited eighth grade students (Frenn 2013a; Haerens 2006a; Werch 2003a). With the exception of one study—Ievers Landis 2005—all included studies engaged both boys and girls.
Interventions
Comparison 1
Seven included studies focused on dietary behavior change (comparison 1): De Bourdeaudhuij 2002, Kirks 1982a, Lin 2017a, Perry 1988a, Vandongen 1995, Wang 2007a, Yeh 2018a. The duration of these interventions varied from one month in Lin 2017a to seven months in Yeh 2018a. The duration of the caregiver component was not reported for two studies (Vandongen 1995; Wang 2007a); the child‐only interventions were nine months and one school term for these studies, respectively. In four included studies in comparison 1, the caregiver component was delivered at the individual or family level (De Bourdeaudhuij 2002; Kirks 1982a; Perry 1988a; Vandongen 1995). In the remaining three studies—Lin 2017a, Wang 2007a, Yeh 2018a—the caregiver component was delivered in a group class context.
De Bourdeaudhuij 2002 used tailored feedback letters to deliver nutrition education focused on fat reduction. In the child‐only arm, six weeks after completing an initial questionnaire, participating adolescents (aged 15 to 18 years) were sent a tailored feedback letter addressing personal fat intake level, motivation to reduce intake, awareness of intake, and attitude and self‐efficacy related to fat reduction. Reported BCTs used in the letters aligned with the "goals and planning," "feedback and monitoring," "shaping knowledge," "comparison of behavior," "repetition and substitution," and "antecedents" clusters. In the child + caregiver arm, a parent also completed an initial questionnaire about himself or herself and received a tailored feedback letter. No attempts were made to encourage adolescents and parents to share or discuss their results within the family. The same list of BCTs reported to be used with adolescents in the child‐only arm was applied separately with caregivers in the child + caregiver arm.
Kirks 1982a used a school‐based nutrition program for children in kindergarten to third grade plus nutrition education for parents. In the child‐only arm, classroom teachers delivered a nutrition education program over four months following a curriculum guide. Based on the reported information, this program aligned with the "shaping knowledge" BCT cluster. In the child + caregiver arm, the intervention team also sent home biweekly newsletters for parents on nutrition education, and provided parents with access to a dietitian to answer questions on food, nutrition, and health topics, and to assist in family menu analyses and dietary counseling. As described, these additional strategies aligned with the BCT clusters of "feedback and monitoring," "social support," "shaping knowledge," and "comparison of outcomes."
Lin 2017a used a Health Action Process Approach−based nutrition intervention for adolescents aged 13 to 18 years plus a similar nutrition education intervention for mothers. In the child‐only arm, adolescents participated in a 30‐minute discussion session about the importance of a healthy diet, including consuming sufficient fruits and vegetables, and then were asked to complete a goal‐setting and action‐planning brochure and to self‐monitor their daily fruit and vegetable intake for a month. Study authors used Michie's taxonomy to describe BCTs in the "goals and planning," "feedback and monitoring," "natural consequences," and "comparison of outcomes" clusters (Michie 2013). In the child + caregiver arm, mothers were invited to participate in a 30‐minute discussion about healthy eating, especially the importance of adequate fruit and vegetable intake, and were provided with a brochure with similar structure and content to that provided to the adolescents. Study authors reported using the same BCTs that were used with adolescents in the child‐only arm with mothers in the child + caregiver arm.
Perry 1988a used a school‐based nutrition program for third grade students and an equivalent home‐based program for families. In the child‐only arm, classroom teachers taught the 15‐session "Hearty Heart and Friends" curriculum over five weeks, which emphasized differentiation between "everyday" and "sometimes" foods, while modeling healthy eating by cartoon characters, skill development in food selection and preparation, and goal‐setting with reinforcement. Study authors reported that use of BCTs aligned with the "goals and planning," "shaping knowledge," "natural consequences," "comparison of behavior," and "reward and threat" clusters. In the child + caregiver arm, a "Home Team" packet was also sent to the child's home each week for five weeks. Each packet contained a guide describing two to three hours of activities on eating pattern changes for the child and the parent to complete together. Both child and parent received participation points for completing the activities together and received small items and entry into a grand prize drawing as participation incentives. As described, the child + caregiver intervention additionally used BCTs aligned with the "goals and planning," "feedback and monitoring," "social support," "shaping knowledge," "comparison of behavior," "repetition and substitution," and "reward and threat" clusters.
Vandongen 1995 used a school‐based nutrition program for 10‐ to 12‐year‐old children and a home‐based program for families. In the child‐only arm, teachers presented 10 × one‐hour lessons focused on improving nutrition knowledge and attitudes and eating habits using specially prepared resources. Based on reported information, these lessons aligned with the "shaping knowledge" BCT cluster. In the child + caregiver arm, five comics with nutrition messages were enlisted to deliver educational materials for the child and the caregiver. Caregivers were also encouraged to assist the child with homework, help prepare healthy recipes, and engage in other activities. Children were rewarded for returning completed homework sheets to school. As described, the additional materials and activities used in this intervention arm aligned with the "social support," "shaping knowledge," and "reward and threat" BCT clusters.
Wang 2007a used a school‐based nutrition program for children in the third, fourth, and fifth grades plus nutrition classes for caregivers. In the child‐only arm, children received nutrition lectures and exposure to other educational materials at school during one term. Strategies reported to be used in this intervention arm aligned with the "shaping knowledge" and "comparison of outcomes" BCT clusters. In the child + caregiver arm, nutrition classes also were offered to caregivers. Based on reported information, these classes for caregivers aligned with the "shaping knowledge" BCT cluster.
Yeh 2018a used a preschool‐based nutrition program for African American children from low‐income families plus nutrition education for caregivers. In the child‐only arm, children received 30‐minute nutrition education sessions twice a week for seven months. These classes included introduction of healthy foods using hand puppets, discussion of the food groups, and fresh fruit and vegetable tastings. Study authors reported that use of BCTs aligned with the "shaping knowledge," "comparison of outcomes," and "antecedents" clusters. In the child + caregiver arm, caregivers additionally received a one‐hour nutrition class every month, focused on topics that they selected. Each class included a presentation followed by a group discussion and related interactive activities. As described, the BCTs utilized in these classes aligned with the "shaping knowledge," "natural consequences," "comparison of behavior," "repetition and substitution," and "comparison of outcomes" clusters. Sessions for both children and caregivers were taught by dietetic interns.
Comparison 2
Six included studies focused on physical activity behavior change (comparison 2): Adamo 2017a,Alhassan 2018a,De Bock 2013a,Ducheyne 2014a,Voll 2013,Werch 2003a. The duration of these interventions varied from one week in Voll 2013 to nine months in Werch 2003a. In four included studies, the caregiver component was delivered at the individual or family level (Adamo 2017a; Ducheyne 2014a; Voll 2013; Werch 2003a). In two studies, the caregiver component was group‐based (Alhassan 2018a; De Bock 2013a).
Adamo 2017a used a train‐the‐trainer approach to implement a physical activity program for preschoolers in childcare centers, supplemented by a home component for parents. In the child‐only arm, childcare providers and center providers attended two workshop training sessions and bimonthly booster sessions focused on increasing knowledge and improving the quality of physical activity opportunities for children. Centers were also provided with the "Activity Begins in Childhood" resource training packet, which included a recommended activity program, equipment, and log sheets to track daily activities. BCTs that childcare providers reportedly were encouraged to use with children aligned with the "social support," "shaping knowledge," "comparison of behavior," "repetition and substitution," "comparison of outcomes," "reward and threat," and "antecedents" clusters. In the child + caregiver arm, parents additionally were asked to watch two webinars, were given copies of the program training materials, and were sent biweekly postcards detailing preschooler‐friendly physical activities and community resources over about six months. Reported strategies applied separately or differently in the child + caregiver arm aligned with the "social support," "shaping knowledge," "natural consequences," and "antecedents" BCT clusters.
Alhassan 2018a used a culturally tailored dance program for girls, along with involvement of mothers in the dance classes. In both arms, girls participated in after‐school sessions three days per week for 12 weeks. These sessions included a one‐hour dance intervention plus a healthy snack and homework tutoring. Three dance styles were introduced—African, Hip Hop, and Jazz—and each was accompanied by educational materials that emphasized the history of the dance style and its impact on African American culture. Mothers and daughters in both arms received weekly health newsletters with similar content, although the newsletters for daughters also contained activities to complete and highlighted the impact of historical African American female figures. Intervention strategies reported to be used with participants in the child‐only arm align with the following BCT clusters: "shaping knowledge," "comparison of behavior," "repetition and substitution," and "comparison of outcomes." In the child + caregiver arm, mothers were invited to join their daughters for the dance classes. Strategies applied separately or differently in the child + caregiver arm align with the "social support," "shaping knowledge," "comparison of behavior," "repetition and substitution," and "comparison of outcomes" BCT clusters.
De Bock 2013a used an existing, state‐sponsored physical activity program for preschoolers plus a participatory parent‐focused intervention. In the child‐only arm, specially trained, external physical activity teachers taught 40 standardized one‐hour gym lessons at preschools over a six‐month period. Study authors reported the use of BCTs that aligned with the "shaping knowledge," "comparison of behavior," "repetition and substitution," and "comparison of outcomes" clusters. In the child + caregiver arm, parents and teachers were encouraged to create small teams that would carry out projects to promote physical activity in the school community. Projects could be original ideas or could be selected from a list of project ideas developed by the researchers. Reported BCTs applied separately or differently in the child + caregiver arm aligned with the "goals and planning," "feedback and monitoring," "social support," "shaping knowledge," "comparison of outcomes," and "antecedents" clusters.
Ducheyne 2014a used a cycle training course for children in the fourth grade plus homework tasks to be completed by both child and parent. In the child‐only arm, children participated in a 45‐minute weekly cycle training course for four weeks on the school playground. Sessions used practical exercises, integrated elements of play, and included exercises from different levels of difficulty. As described, teaching strategies used in the sessions aligned with the "shaping knowledge," "comparison of behavior," "repetition and substitution," and "comparison of outcomes" BCT clusters. In the child + caregiver arm, parents were asked to help their child complete weekly homework assignments related to cycling safety. As described, these homework assignments leveraged strategies aligned with the "social support" and "shaping knowledge" BCT clusters.
Voll 2013 targeted screen time by tracking the Turnoff Week Challenge with children in the fourth to sixth grade plus homework tasks to be completed by both child and caregiver. In the child‐only arm, children completed a brief Turnoff Week tracker form daily in class for one week. Use of this tracking form aligned with the "feedback and monitoring" and "repetition and substitution" BCT clusters. In the child + caregiver arm, caregivers were asked to complete two homework assignments, each of which took 5 to 10 minutes to complete. The first homework provided information on the benefits of physical activity, encouraged goal‐setting, and asked children and caregivers to complete a physical activity together and to reflect on the experience. The second homework prompted caregivers and children to complete a five‐minute fitness activity together and to reflect on their experience. BCTs reported to be used in the child + caregiver arm aligned with the "goals and planning," "feedback and monitoring," "social support," "shaping knowledge," "natural consequences," "repetition and substitution," "identity," and "self‐belief" BCT clusters.
Werch 2003a provided individual consultations with eighth graders and mailed print materials to parents to promote physical activity. The intervention focused on promotion of sports participation and, in addition to encouraging physical activity, aimed to prevent alcohol use. In the child‐only arm, adolescents were administered a sport and alcohol prevention consultation tailored to their responses to screening questions. At the end of the consultation, they were asked to sign a student contract that provided a nurse recommendation regarding each of the health behaviors targeted in the consultation. As described, strategies used in the consultations aligned with the "goals and planning," "feedback and monitoring," "shaping knowledge," "natural consequences," and "comparison of outcomes" BCT clusters. In the child + caregiver arm, caregivers additionally were mailed five health and fitness information cards, the bottom of which could be torn off and used to gather parent feedback. As described, the content of these cards aligned with the "shaping knowledge" BCT cluster.
Comparison 3
Ten included studies focused on both diet and physical activity behavior change (comparison 3): Baghurst 2014,Cottrell 2005,Crespo 2012a,Dietsch 1990,Frenn 2013a,Haerens 2006a,Hopper 1992a,Ievers Landis 2005,Luepker 1996a,Petchers 1987. The duration of these interventions varied from three to four weeks in Frenn 2013a, to three years in Crespo 2012a and Luepker 1996a. Three studies did not report the duration of the caregiver component (Baghurst 2014; Ievers Landis 2005; Petchers 1987); the child‐only interventions were provided for eight weeks, an average of three months, and one school year for these three studies, respectively. In two studies, the caregiver component was delivered in a group class context (Dietsch 1990; Ievers Landis 2005). In all other studies, the caregiver component was delivered at the individual or family level.
Baghurst 2014 used a school‐based nutrition program for children in the second and third grades plus nutrition information packets for caregivers. In the child‐only arm, classroom teachers delivered five in‐class lessons from the Reading Across MyPyramid (RAMP) curriculum over an eight‐week period. In the child + caregiver arm, caregivers additionally received nutrition education packets based on the US Department of Agriculture Dietary Guidelines for Americans; the number of packets was not reported. Based on reported information, both intervention arms utilized strategies aligning with only the "shaping knowledge" BCT cluster.
Cottrell 2005 used pedometers, step logs, and health information packets to promote healthy eating and physical activity. In the child‐only arm, kindergartners received a pedometer and a daily step log to use over a four‐week period, and caregivers received age‐appropriate information about diet and exercise guidelines. BCTs reported to be used in the child‐only arm aligned with the "feedback and monitoring," "shaping knowledge," and "antecedents" clusters. In the child + caregiver arm, caregivers additionally received their own pedometer and daily step log, as well as obesity prevention information packets with recommendations on ways to increase steps. Caregivers in this arm with obese children were also given information on ways to reduce caloric intake. As described, the additional materials and information delivered to this intervention arm aligned with the "feedback and monitoring," "shaping knowledge," "natural consequences," and "antecedents" BCT clusters.
Crespo 2012a used school and community environmental change strategies plus a community health worker−led family and home intervention to promote healthy eating and physical activity and to prevent excess weight gain among Latino elementary school children. In the child‐only arm, a range of community change efforts and school programs were implemented with the intent to change physical and social structures, policies, and the availability of protective and harmful products, and to provide culturally appropriate media messages. Intervention activities were intended to build or maintain strength over the three‐year intervention and, as reported, aligned with the "social support," "shaping knowledge," "reward and threat," and "antecedents" BCT clusters. In the child + caregiver arm, promotoras (Latina community health workers) additionally visited families each month for seven consecutive months and then made four booster calls over the subsequent two years. The visits and booster calls were designed to support caregivers in promoting fruit and vegetable intake, choosing water instead of SSB, decreasing TV viewing, and increasing active play. The additional intervention activities reportedly used in the child + caregiver arm aligned with the "goals and planning," "feedback and monitoring," "social support," "shaping knowledge," "natural consequences," "comparison of outcomes," "reward and threat," "antecedents," and "identity" BCT clusters.
Dietsch 1990 used a school‐based nutrition and exercise promotion program for seventh graders plus nutrition education for parents. In the child‐only arm, children received 15 lessons that included information about nutrition and the benefits of exercise, along with techniques such as goal‐setting and assertiveness training. Caregivers were mailed the results of their own health status assessments, along with norms for people of the same age and sex. Strategies reported to be used aligned with the "goals and planning," "feedback and monitoring," "shaping knowledge," "natural consequences," and "comparison of behavior" BCT clusters. In the child + caregiver arm, caregivers additionally were invited to four intervention sessions consisting of low‐impact aerobic activity, a snack, a one‐hour presentation, and receipt of the results of their health status assessments and corresponding normative information. These sessions were offered one evening per week for four consecutive weeks. Caregivers were also offered two booster sessions three and six months following the final lesson and received four monthly newsletters. Of note, caregivers participating in the child + caregiver arm did not necessarily have a child participating in the child‐only intervention, as the child‐only intervention was offered to seventh grade students, and caregivers of sixth, seventh, and eighth grade students were invited to the child + caregiver arm. As described, the additional intervention activities delivered to the child + caregiver arm aligned with the "goals and planning," "feedback and monitoring," "shaping knowledge," "natural consequences," "comparison of behavior," "repetition and substitution," "comparison of outcomes," and "reward and threat" BCT clusters.
Frenn 2013a used online programs focused on promoting physical activity and reducing dietary fat intake among middle‐school students. In the child‐only arm, fifth to eighth grade students completed an eight‐module, online program in classroom settings where each child had a computer. Concepts were illustrated in four short videos featuring culturally diverse child actors from similar schools. Each module took 10 to 30 minutes to complete, and children progressed at their own pace over a three‐ to four‐week period. As described, the content of the modules aligned with the "goals and planning," "feedback and monitoring," "shaping knowledge," "comparison of behavior," and "repetition and substitution" BCT clusters. In the child + caregiver arm, caregivers additionally were asked to complete six online modules at home over the same period. Each caregiver module could be completed in 5 to 10 minutes and, as reported, aligned with the "feedback and monitoring," "social support," "shaping knowledge," "natural consequences," "comparison of behavior," and "identity" BCTs.
Haerens 2006a used a school‐based nutrition and physical activity program, including environmental and educational components for seventh and eighth graders plus caregiver education and tailored dietary feedback. In the child‐only arm, work groups at each school organized physical activity opportunities and promoted water and fruit intake. Each year for two years, children completed computer‐tailored diet and physical activity interventions (one hour each) based on the results of a physical fitness test and questions on fat and fruit intake. Strategies reported to be used in the child‐only arm aligned with the "feedback and monitoring," "shaping knowledge," "natural consequences," "comparison of behavior," "repetition and substitution," and "antecedents" BCT clusters. In the child + caregiver arm, caregivers additionally were invited to an interactive meeting, were sent information on healthy eating and physical activity in school papers and newsletters, and were asked to complete an adult version of the computer‐tailored intervention for fat intake at home. As described, these additional materials and activities for caregivers aligned with the "feedback and monitoring," "social support," "shaping knowledge," and "natural consequences" BCT clusters.
Hopper 1992a used a school‐based physical fitness and nutrition education program and a home‐based program for families. In the child‐only arm, children received three 40‐minute physical fitness sessions and two 30‐minute nutrition education sessions each week for six weeks. These sessions were taught by classroom teachers assisted by a physical education specialist and a nutrition education specialist. As described, the BCTs used in the sessions aligned with the "goals and planning," "feedback and monitoring," "social support," "shaping knowledge," "natural consequences," "comparison of behavior," and "repetition and substitution" clusters. In the child + caregiver arm, children additionally were given weekly packets over the six‐week intervention period to bring home and read with their family. Packets included information on healthy food preparation and family‐friendly exercise activities and, as described, used BCTs aligned with the "goals and planning," "feedback and monitoring," "social support," "shaping knowledge," "repetition and substitution," and "reward and threat" clusters.
Ievers Landis 2005 used the "Know Bones About It" program on calcium intake and weight‐bearing physical activity plus caregiver educational sessions. In the child‐only arm, girls received six educational sessions focused on healthy lifestyle behaviors for prevention of osteoporosis, over a period of about six months. Sessions took place during Girl Scout meetings and each lasted approximately 30 minutes. Strategies reported to be used in these sessions with girls aligned with the "goals and planning," "feedback and monitoring," "social support," "shaping knowledge," "natural consequences," "comparison of behavior," "repetition and substitution," "comparison of outcomes," and "reward and threat" BCT clusters. In the child + caregiver arm, primary caregivers were additionally invited to two interactive sessions that addressed preventing osteoporosis, role modeling, coaching, problem‐solving, and providing rewards. Strategies reported to be used in the sessions additionally offered in the child + caregiver arm aligned with the "goals and planning," "social support," "natural consequences," "comparison of outcomes," "reward and threat," "antecedents," and "identity" BCT clusters.
Luepker 1996a used a school‐based cardiovascular disease prevention program for third grade students and family education. The multi‐site intervention, known as the "Child and Adolescent Trial for Cardiovascular Health (CATCH)," lasted for three years and also included tobacco prevention components. In the child‐only arm, relevant intervention components included school food service modifications (continuous for three years), physical education class enhancement (continuous for three years), and classroom curricula implemented over a fixed time period each year. Strategies reported to be used in the child‐only arm aligned with the "goals and planning," "feedback and monitoring," "shaping knowledge," "comparison of behavior," "repetition and substitution," "reward and threat," and "antecedents" BCT clusters. In the child + caregiver arm, families additionally were invited to take part in "Home Team" programs and received 19 activity packets over the course of the three years. As with the "Home Team" program used by Perry 1988a, scorecards were used to record points for completing activities together and for giving small rewards as participation incentives. Third and fourth grade students and their caregivers also were invited to family fun nights held at the schools. The additional materials and activities reported to be used in the child + caregiver arm aligned with the "goals and planning," "feedback and monitoring," "social support," "shaping knowledge," "comparison of behavior," "repetition and substitution," "reward and threat," and "antecedents" BCT clusters.
Petchers 1987 used the Chicago Heart Health Curriculum's "Body Power!" school‐based program for sixth graders plus health information for caregivers. In the child‐only intervention, children were taught five inter‐related modules on cardiovascular health. Each module was designed to be taught through two × 40‐minute lessons per week for five to six weeks (or the equivalent). One module focused specifically on diet and digestion, and another focused on exercise and the skeletal and muscular systems. Other modules covered basic information on the circulatory system, the dangers of smoking, and risk factors for cardiovascular health and disease prevention. As described, the program incorporated strategies aligned with the "feedback and monitoring," "shaping knowledge," "natural consequences," and "comparison of behavior" BCT clusters. In the child + caregiver arm, families additionally were sent 17 newsletters with health tips and a health booklet/log. As described, these materials aligned with the "feedback and monitoring," "shaping knowledge," and "natural consequences" BCT clusters.
Outcomes
Considerable heterogeneity was evident in the timing and methods of measurement for all outcomes. Even when studies measured outcomes, often they did not report data and we could not retrieve data from the study authors. Seven studies contributed no data to this review (Baghurst 2014; De Bourdeaudhuij 2002; Ducheyne 2014a; Frenn 2013a; Kirks 1982a; Petchers 1987; Wang 2007a). Below we present the eligible outcomes for which data are available during the intervention, at the end of the intervention, and after the intervention period (follow‐up). For further detail on time points and methods, see Characteristics of included studies and Data and analyses.
Primary outcomes
-
Children's dietary intake
Total energy intake: data available from four studies (Haerens 2006a; Hopper 1992a; Luepker 1996a; Vandongen 1995)
Percentage of total energy intake from fat: data available from five studies (Dietsch 1990; Haerens 2006a; Hopper 1992a; Luepker 1996a; Vandongen 1995)
Percentage of total energy intake from saturated fat: data available from three studies (Dietsch 1990; Luepker 1996a; Vandongen 1995)
Percentage of total energy intake from trans fat: no data available
Percentage of total energy intake from carbohydrate: data available from two studies (Hopper 1992a; Luepker 1996a)
Percentage of total energy intake from protein: data available from three studies (Hopper 1992a; Luepker 1996a; Vandongen 1995)
Sodium intake: data available from four studies (Hopper 1992a; Luepker 1996a; Perry 1988a; Vandongen 1995)
Fruit and vegetable intake: data available from one study (Crespo 2012a)
Fruit intake: data available from three studies (Dietsch 1990; Haerens 2006a; Lin 2017a)
Vegetable intake: data available from two studies (Dietsch 1990; Lin 2017a)
SSB intake: data available from three studies (Crespo 2012a; Dietsch 1990; Haerens 2006a)
Water intake: data available from three studies (Crespo 2012a; Haerens 2006a; Luepker 1996a)
-
Children's physical activity levels
Total physical activity: data available from three studies (Adamo 2017a; Haerens 2006a; Luepker 1996a)
MVPA: data available from five studies (Adamo 2017a; Alhassan 2018a; De Bock 2013a; Haerens 2006a; Luepker 1996a)
Moderate physical activity: data available from one study (Werch 2003a)
Vigorous physical activity: data available from one study (Werch 2003a)
LPA: data available from four studies (Adamo 2017a; Alhassan 2018a; Haerens 2006a; Luepker 1996a)
Weight‐bearing physical activity: data available from one study (Ievers Landis 2005)
Steps: data available from two studies (Adamo 2017a; Cottrell 2005)
Total physical activity score: data available from one study (Voll 2013)
Adverse effects: no data available
Secondary outcomes
Children's dietary quality: no data available
Children's sedentary behavior: data available from four studies (Adamo 2017a; Alhassan 2018a; De Bock 2013a; Luepker 1996a)
Prevalence of overweight and obesity among children: data available from three studies (Crespo 2012a; Haerens 2006a; Luepker 1996a)
Children's BMI or weight‐for‐height parameter: data available from eight studies (Adamo 2017a; Crespo 2012a; De Bock 2013a; Haerens 2006a; Hopper 1992a; Luepker 1996a; Vandongen 1995; Yeh 2018a)
-
Caregivers' dietary intake
Total energy intake: no data available
Percentage of total energy intake from fat: no data available
Percentage of total energy intake from saturated fat: no data available
Percentage of total energy intake from trans fat: no data available
Percentage of total energy intake from carbohydrate: no data available
Percentage of total energy intake from protein: no data available
Sodium intake: no data available
Fruit and vegetable intake: no data available
Fruit intake: no data available
Vegetable intake: no data available
SSB intake: no data available
Water intake: no data available
-
Caregivers' physical activity levels
Total physical activity: no data available
MVPA: data available from one study (Alhassan 2018a)
Moderate physical activity: no data available
Vigorous physical activity: no data available
LPA: data available from one study (Alhassan 2018a)
Weight‐bearing physical activity: no data available
Steps: no data available
Total physical activity score: data available from one study (Voll 2013)
Excluded studies
We excluded 1071 reports after full‐text screening. Of these, seven studies merited closer inspection, and EHM and US sought additional consultation before determining their eligibility (Brannon 2018; DeVilliers 2009; Harrington 2005; Natale 2016; Regev 2012; Russell Mayhew 2007; Treu 2017). All seven were ultimately excluded (Characteristics of excluded studies). For Regev 2012 and Russell Mayhew 2007, EHM and US consulted with AS to determine eligibility. Both studies were subsequently excluded because they did not address outcomes relevant to this review. Regev 2012 examined the impact of a movement therapy group, with and without mother participation, on Israeli children six to eight years of age. All children had been referred for diagnosis and emotional therapy. Although the intervention addressed physical movement, study authors did not measure physical activity behaviors. Russell Mayhew 2007 examined the impact of a wellness‐based eating disorder prevention program, with and without caregiver involvement, on Canadian children and adolescents. The intervention measured self‐concept and eating attitudes but did not measure changes in dietary intake. For three studies for which conference abstracts appeared likely to be relevant but full‐text reports could not be obtained, we contacted the study authors for clarification on methods before determining that these studies did not meet our eligibility criteria (DeVilliers 2009; Harrington 2005; Natale 2016). The methods applied by DeVilliers 2009 and Natale 2016 did not meet our eligibility criteria. Harrington 2005 does appear to meet our inclusion criteria; however, study authors informed us that results from this trial were never published and that the data can no longer be accessed. For two additional studies for which we were able to access the full‐text reports but were unable to assess eligibility, we contacted the study authors for clarification on methods (Brannon 2018; Treu 2017). With feedback from the study authors, we determined that Treu 2017 was not a randomized study. Brannon 2018 was a cross‐over trial that used an n‐of‐1 RCT design to assess whether receiving text messages from different people would help adolescents meet their physical activity goals, increase physical activity time, and decrease sedentary behavior. We determined this study to be ineligible after the corresponding author indicated that only one day of data were available for each condition (Brannon 2018).
For the remaining 1064 reports, EHM and US agreed on study exclusion.
Reasons for all exclusions are summarized below.
226 reports did not report the results of RCTs or quasi‐RCTs.
214 reports presented the results of secondary analyses from RCTs or quasi‐RCTs that did not meet our inclusion criteria.
32 reports described the results of RCTs or quasi‐RCTs that did not include caregiver involvement, address dietary or physical activity behaviors, or take place in a home or community setting.
138 reports presented the results of RCTs or quasi‐RCTs in which participating children were not actively involved in the intervention, did not meet the age criteria of this review, or were recruited from a special population with pre‐existing conditions (e.g. obesity).
449 reports described the results of RCTs or quasi‐RCTs in which the only difference between the intervention (child + caregiver) and control (child‐only) arms was not the addition of a caregiver component.
12 reports were excluded for other reasons, including non‐research publications (e.g. editorial, summary of projects funded under a grant).
Ongoing studies
There are seven ongoing studies: Cunningham Sabo 2016,Kovalskys 2017a,NCT00065247,NCT02809196,NCT02942823,Armstrong 2019a,Yin 2019a (see the Characteristics of ongoing studies tables). For five of these studies, we emailed the study authors to check on study status (Kovalskys 2017a; NCT00065247; NCT02809196; NCT02942823; Yin 2019a). For the other two studies (Armstrong 2019a; Cunningham Sabo 2016), the timeline indicated in the protocol papers and at trial registration made it clear that the study was ongoing. We categorized a study as ongoing if the primary outcome paper has not yet been published but available information indicates that the study meets review eligibility criteria.
Cunningham Sabo 2016 is a cluster‐RCT with fourth grade students and their families in Colorado, USA, aimed at preventing childhood obesity by promoting healthy food and activity behaviors. Over four years, annual cohorts will participate in the five arms: (1) school‐based intervention; (2) school‐based intervention plus family intervention; (3) school‐based intervention plus online parent‐based intervention; (4) school‐based intervention plus both family interventions; and (5) online parent‐based intervention. It is unclear whether there is also a no intervention control arm. For the purpose of this review, the school‐based intervention arm represents the child‐only condition, and all other study arms represent versions of the child + caregiver condition.
Kovalskys 2017a is a cluster‐RCT with first grade children and their families in Buenos Aires, Argentina, aimed at increasing MVPA and improving eating habits at home and at school. The study ran during the second semester of first grade and the first semester of second grade (July 2015 to November 2016) and involved two components: "active breaks," which are implemented during school breaks by a physical activity instructor, and the "virtual" intervention, which involves delivery of Web‐based contents to families via a multi‐platform application. Schools are allocated to one of four intervention arms: (1) active breaks, (2) virtual intervention, (3) active breaks and the virtual intervention, or (4) no intervention. For the purpose of this review, the school‐based intervention represents the child‐only condition, and the combined school‐based and family‐based interventions represent the child + caregiver condition.
NCT00065247 is cluster‐RCT with first and second grade children (age six to nine years) and their families in Massachusetts and Rhode Island, USA, aimed at improving bone quality and muscle strength. After‐school programs were randomized to one of three study arms: (1) the Beat Osteoporosis: Nourish and Exercise Skeletons (BONES) project; (2) the BONES project plus a caregiver component; or (3) no intervention. The BONES project curriculum is delivered four days per week for a 20‐ to 25‐week period per year and involves weight‐loading physical activity, nutrition and bone health education, and calcium‐rich snacks. Caregivers in the BONES project plus caregiver component arm receive a newsletter and a worksheet five times per year. The project ran for two years. For the purpose of this review, the BONES project represents the child‐only condition, and the BONES project plus a caregiver component represents the child + caregiver condition.
NCT02809196 is an individually randomized trial aimed at promoting healthful dietary habits among adolescents aged 14 to 15 years participating in the Danish National Birth Cohort. The Texts For Healthy Teens (T4HT) intervention involves a short message service (SMS)‐based health educational program targeting a cluster of dietary factors. This study will examine if the impact of the standardized program is reinforced when a friend or the mother of the participant (or both) is also asked to participate, and if the impact is reinforced if the intervention is tailored to target only one participant‐selected dietary factor rather than a cluster of factors. The standardized program includes 121 messages distributed over 12 weeks. The tailored program focuses on SSB, fruits and vegetables, or fish and includes about 40 messages distributed over four weeks. Participants are randomized into one of nine intervention arms: (1) tailored SMS program implicating friend and mother; (2) standardized SMS program implicating friend and mother; (3) tailored SMS program implicating friend, not mother; (4) standardized SMS program implicating friend, not mother; (5) tailored SMS program implicating mother, not friend; (6) standardized SMS program implicating mother, not friend; (7) tailored SMS program not implicating mother or friend; (8) standardized SMS program not implicating mother or friend; or (9) no SMS program. For the purpose of this study, multiple combinations of the intervention arms represent the child‐only and child + caregiver conditions: when arm 3 is the child‐only arm, arm 1 is the child + caregiver arm; when arm 4 is the child‐only arm, arm 2 is the child + caregiver arm; when arm 7 is the child‐only arm, arm 5 is the child + caregiver arm; and when arm 8 is the child‐only arm, arm 6 is the child + caregiver arm.
NCT02942823 is an individually randomized obesity prevention trial with children aged 9 to 12 years and their caregivers in Germany, aimed at improving nutrition, physical activity, and psychosocial factors. The intervention involves a motion‐controlled serious game that integrates knowledge‐based and cognitive tasks. The game consists of two 35‐minute sessions. Fourth grade children and their parents are randomly allocated to one of two intervention conditions. In the child‐only arm, students play both sessions of the serious game at school within a two‐week period. In the child + caregiver condition, children additionally take the game home on a tablet to play with their parents between the first and second sessions.
Armstrong 2019a is an obesity prevention cluster‐RCT in Maryland, USA, aimed at improving motor skills, physical activity, and willingness to try new foods among children aged three to five years from low‐income communities. Childcare centers will be assigned to to one of three arms: (1) data collection only; (2) childcare center−based lessons delivered by trained childcare staff, including 18 weeks of motor skills lessons and 12 weeks of nutrition lessons; or (3) childcare center−based lessons plus a Web‐based intervention for caregivers designed to promote physical activity, nutrition, and wellness, with topics co‐ordinated with activities conducted in the classrooms.
Yin 2019a is a cluster‐RCT in San Antonio, Texas, targeting key enablers and barriers to obesity prevention in childcare settings serving low‐income populations. The intervention is culturally tailored to the Latino community, is administered through Head Start centers, and involves center‐based components (policy changes at the Head Start center, staff development, a gross motor program, and nutrition education) and home‐based components (parent engagement and education and home visits). Head Start centers are randomized to one of three conditions: combined center and home−based intervention; center‐based intervention; or no intervention. Three‐year‐old children and their families are eligible to take part. For the purpose of this review, the center‐based intervention represents the child‐only arm, and the combined center and home−based intervention represents the child + caregiver arm.
Studies awaiting classification
Four studies are awaiting classification (Kobak 2016; NTR5755; Ruiter 2015a; Swindle 2017a). For each, except Swindle 2017a, which is currently recruiting participants, we made two attempts to contact the corresponding study author for further information and results but did not receive a reply. Additional information is necessary to determine if these studies meet review eligibility criteria (Criteria for considering studies for this review). For an overview of these studies, see the Characteristics of studies awaiting classification tables.
Kobak 2016 was a cross‐over RCT in Ohio, USA, designed to assess the extent and intensity of children's physical activity and sedentary behavior in different social conditions. Wearing an accelerometer, children participated in three simulated recess conditions in a playground setting: (1) playing alone, (2) playing with a parent, and (3) playing with a friend.
NTR5755 is a follow‐up study to Ruiter 2015a. In this cluster‐RCT, children 9 to 12 years of age were recruited from schools taking part in an existing school‐based intervention, "KERNgezond." This intervention aims to investigate whether children's diet and physical activity behaviors are healthier if their parents follow an e‐learning parenting program compared to children whose parents receive only a folder about healthy eating and physical activity. The intervention arms are not described in the trial registration.
Ruiter 2015a is a cluster‐RCT for children 9 to 13 years of age and their parents in the Nijmegen region of The Netherlands. Participants were recruited from schools taking part in an existing school‐based overweight prevention program, "Scoring for Health." Schools were randomized to either (1) the underlying "Scoring for Health" program plus a brochure for parents, or (2) the "Scoring for Health" program plus a brochure for parents and an e‐learning parenting program focused on preventing overweight in children.
Swindle 2017a is a cluster‐RCT for children age three to five years and their caregivers in Arkansas, USA. Head Start centers are randomized to either (1) an evidence‐based obesity prevention program for early childcare centers, or (2) an enhanced version of the program that involves caregiver input.
Risk of bias in included studies
We present the results of individual "Risk of bias" assessments in the "Risk of bias" table for each study (see Characteristics of included studies). For an overall visual summary of the risk of bias of included studies, see Figure 2 and Figure 3.
2.
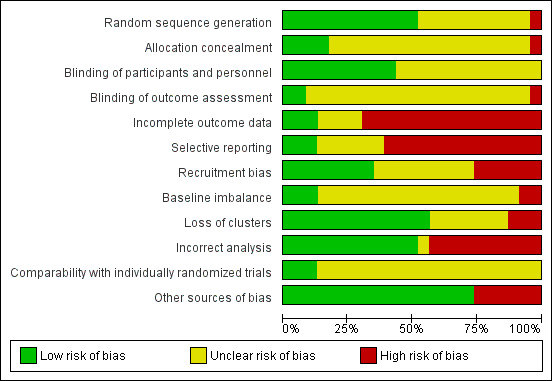
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
3.
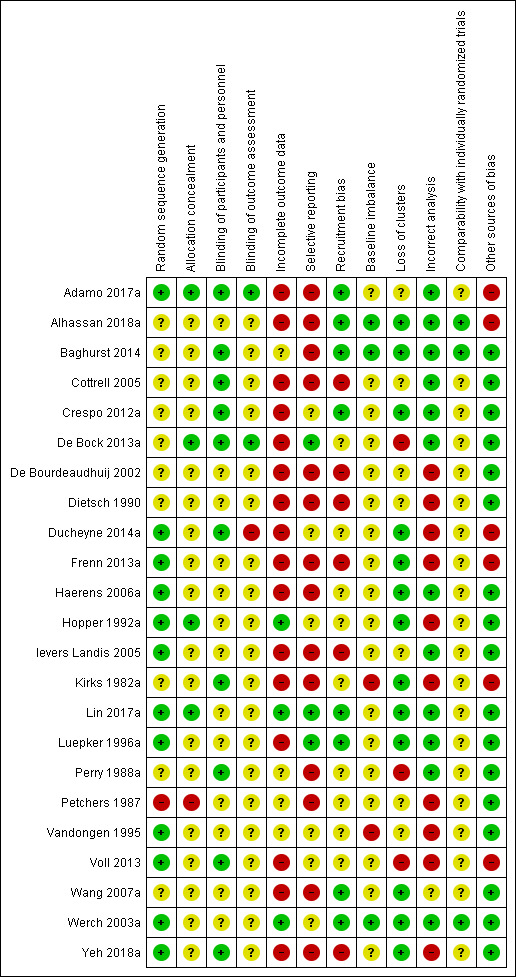
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Random sequence generation
We judged only one study to be at high risk of bias with respect to the random sequence generation domain (Petchers 1987). As noted under the allocation domain, Petchers 1987 guaranteed three schools that they would not be allocated to the no‐intervention control arm, and that they would be assigned to the child + caregiver or the child‐only arm.
Twelve studies described a low‐risk method of random sequence generation in published reports (Adamo 2017a; Ievers Landis 2005; Lin 2017a; Voll 2013; Werch 2003a), or through email correspondence (Ducheyne 2014a; Frenn 2013a; Haerens 2006a; Hopper 1992a; Luepker 1996a; Vandongen 1995; Yeh 2018a).
We were unable to determine the risk of bias related to random sequence generation for 10 studies because the process was insufficiently described and we were unable to retrieve additional information from the study authors (Alhassan 2018a; Baghurst 2014; Cottrell 2005; Crespo 2012a; De Bock 2013a; De Bourdeaudhuij 2002; Dietsch 1990; Kirks 1982a; Perry 1988a; Wang 2007a).
Allocation
We considered Petchers 1987 to be at high risk of selection bias because the three participating schools were guaranteed assignment to the child + caregiver or the child‐only arm before randomization, as a result of prior participation in the control arm of another study. We judged four studies to be at low risk of selection bias because study authors described adequate concealment of allocation (Adamo 2017a; De Bock 2013a; Hopper 1992a; Lin 2017a).
We determined the remaining 18 trials to be at unclear risk of bias because study authors did not describe the methods used to conceal allocation (Alhassan 2018a; Baghurst 2014; Cottrell 2005; Crespo 2012a; De Bourdeaudhuij 2002; Dietsch 1990; Ducheyne 2014a; Frenn 2013a; Haerens 2006a; Ievers Landis 2005; Kirks 1982a; Luepker 1996a; Perry 1988a; Vandongen 1995; Voll 2013; Wang 2007a; Werch 2003a; Yeh 2018a).
Blinding
Blinding of participants and personnel
We judged no studies to be at high risk of performance bias. Due to the nature of the interventions, blinding of personnel was not possible in most of the included studies. We considered children 10 years of age and younger to be unlikely to be influenced by knowing their study allocation. The young age of the children in nine trials suggests that their performance was unlikely to have been influenced by lack of blinding (Adamo 2017a; Baghurst 2014; Cottrell 2005; Crespo 2012a; De Bock 2013a; Ducheyne 2014a; Kirks 1982a; Perry 1988a; Yeh 2018a). We judged these trials to be at low risk of bias. We additionally judged one study to be at low risk of bias because the true purpose of the study was concealed until after the intervention was provided (Voll 2013).
We considered 13 trials to be at unclear risk of bias because the children were old enough for all or part of the study that their performance may have been influenced by lack of blinding (Alhassan 2018a; De Bourdeaudhuij 2002; Dietsch 1990; Frenn 2013a; Haerens 2006a; Hopper 1992a; Ievers Landis 2005; Lin 2017a; Luepker 1996a; Petchers 1987; Vandongen 1995; Wang 2007a; Werch 2003a). Dietsch 1990, Haerens 2006a, Hopper 1992a, Lin 2017a,Luepker 1996a, Petchers 1987, Vandongen 1995, Wang 2007a, and Werch 2003a did not provide information about blinding. In Alhassan 2018a, neither participants nor personnel were blinded, and this may or may not have influenced performance. In De Bourdeaudhuij 2002, participants were blinded to the study condition. However, because they were recruited from only two secondary schools, it is possible that children or caregivers, or both, from different classes could have spoken about the intervention. For Frenn 2013a, blinding of personnel was not a concern because the intervention was delivered online. Participants were not blinded, and knowledge of the intervention may or may not have influenced their performance. In Ievers Landis 2005, participants and Girl Scout troop leaders were masked to group assignment. However, study facilitators were not masked, and this may or may not have influenced performance.
Blinding of outcome assessment
We determined one study to be at high risk of detection bias (Ducheyne 2014a). In Ducheyne 2014a, researchers were not blinded to the condition that they were testing for in the practical cycling test, and other outcomes, such as time spent cycling to school and child anthropometry (data not available), were measured by caregiver report.
We judged two studies to be at low risk of bias for this domain (Adamo 2017a; De Bock 2013a). In Adamo 2017a and De Bock 2013a, outcome assessors were masked and physical activity was measured by accelerometry.
We judged all 20 other studies to be at unclear risk of bias. In two studies, study authors reported that outcome assessors were not blinded (Ievers Landis 2005; Vandongen 1995). However, in these two studies, diet and physical activity data were reported by participants, and responses may or may not have been influenced by lack of blinding. The remaining 18 trials provided no information on blinding of outcome assessment (Alhassan 2018a; Baghurst 2014; Cottrell 2005; Crespo 2012a; De Bourdeaudhuij 2002; Dietsch 1990; Frenn 2013a; Haerens 2006a; Hopper 1992a; Kirks 1982a; Lin 2017a; Luepker 1996a; Perry 1988a; Petchers 1987; Voll 2013; Wang 2007a; Werch 2003a; Yeh 2018a). These studies often measured diet and activity outcomes using self‐reported or caregiver‐reported instruments, and it is possible that assessment was influenced by lack of blinding.
Incomplete outcome data
We evaluated 16 studies to be at high risk of attrition bias (Adamo 2017a; Alhassan 2018a; Cottrell 2005; Crespo 2012a; De Bock 2013a; De Bourdeaudhuij 2002; Dietsch 1990; Ducheyne 2014a; Frenn 2013a; Haerens 2006a; Ievers Landis 2005; Kirks 1982a; Luepker 1996a; Voll 2013; Wang 2007a; Yeh 2018a). For Adamo 2017a, Alhassan 2018a, Crespo 2012a, De Bourdeaudhuij 2002, Dietsch 1990, Frenn 2013a, Haerens 2006a, Ievers Landis 2005, Kirks 1982a, Luepker 1996a, Wang 2007a, and Yeh 2018a, we extracted or calculated rates of total and differential attrition and determined one or both of these rates to exceed the thresholds outlined above in Assessment of risk of bias in included studies. For Haerens 2006a, Luepker 1996a, and Yeh 2018a, study authors provided the data needed to calculate attrition. We could not calculate attrition rates for Cottrell 2005, De Bock 2013a, Ducheyne 2014a, and Voll 2013; however, published articles from these studies provided adequate information to show substantial missing data.
We considered three studies to be at low risk of attrition bias due to limited attrition (Hopper 1992a; Lin 2017a; Werch 2003a). Information on attrition was not published for Hopper 1992a but was provided by the study authors.
Because of inadequate information on missing data, we judged four studies to be at unclear risk of attrition bias (Baghurst 2014; Perry 1988a; Petchers 1987; Vandongen 1995).
Selective reporting
To be judged at low risk of reporting bias, we required that the trial was registered or a protocol was published, and that pre‐specified outcomes were available for inclusion in this review in a format that could be entered into meta‐analysis. Only three studies met this criteria (De Bock 2013a; Lin 2017a; Luepker 1996a). De Bock 2013a registered the trial, published the study protocol, and reported the results for primary and secondary outcomes. Lin 2017a registered the trial and reported the results for primary and secondary outcomes. Luepker 1996a published the design and methods of the study and reported or provided statistics for primary outcomes and those relevant to this review.
We judged 14 studies to be at high risk of reporting bias (Adamo 2017a; Alhassan 2018a; Baghurst 2014; Cottrell 2005; De Bourdeaudhuij 2002; Dietsch 1990; Frenn 2013a; Haerens 2006a; Ievers Landis 2005; Kirks 1982a; Perry 1988a; Petchers 1987; Wang 2007a; Yeh 2018a). Most of these studies measured relevant outcomes but did not report all outcomes completely and at all measurement time points. Adamo 2017a was a registered trial with a published study protocol. Study authors indicated that they would assess outcomes at midpoint (three months) and at the end of the intervention (six months). Although end‐of‐intervention data were published, midpoint data were not reported and we could not retrieve them from the study authors. Alhassan 2018a was a registered trial with pre‐specified outcomes, including physical activity levels and body mass index (BMI). Although BMI was measured at each time point, study authors did not report the results for this outcome. Further, although means and standard deviations were reported for time spent in moderate to vigorous physical activity (MVPA), in light intensity physical activity (LPA), and in sedentary behavior, study authors discussed changes in vigorous physical activity (VPA) but did not report corresponding outcome statistics. Baghurst 2014 and Frenn 2013a measured relevant outcomes but did not report or provide means or standard deviations and therefore could not be included in the meta‐analysis. De Bourdeaudhuij 2002 and Kirks 1982a measured and reported mean end values for relevant outcomes but did not report or provide variance statistics. Dietsch 1990 reported means and standard deviations for several relevant dietary outcomes. However, outcome data for children's total energy intake and percentage of total energy intake from carbohydrates and protein were measured but not reported, and we could not retrieve the data from study authors. Ievers Landis 2005 measured both total physical activity and weight‐bearing physical activity but reported outcome statistics for weight‐bearing physical activity only. Haerens 2006a provided outcome statistics for all relevant measured outcomes, except the physical activity outcome assessed by accelerometry at the end of the intervention (21 months), which trial authors could not retrieve. Perry 1988a measured several dietary outcomes relevant to this review but did not present most results in a format that we could utilize. The only exception was sodium intake at one‐year follow‐up, for which outcome data were reported in a format that we could enter into a meta‐analysis. Yeh 2018a measured both child anthropometrics and diet but reported only anthropometric data in a format that we could use. From Cottrell 2005, we were able to include the physical activity outcome data in a meta‐analysis but could not utilize the dietary outcome data due to lack of confidence in the values reported. Petchers 1987 measured diet and exercise behaviors, but measured outcomes were not reported completely, nor did they align with those analyzed in this review. Similarly, the dietary outcomes measured by Wang 2007a were not relevant to this review.
We could not judge the risk of reporting bias for the remaining six studies (Crespo 2012a; Ducheyne 2014a; Hopper 1992a; Vandongen 1995; Voll 2013; Werch 2003a). None of these trials were registered, and we did not identify study protocols. Four of these studies either reported or provided relevant outcome statistics in a format that could be entered into meta‐analysis (Hopper 1992a; Vandongen 1995; Voll 2013; Werch 2003a). Crespo 2012a measured and reported dietary, physical activity, sedentary behavior, and anthropometric outcomes completely and in a format that facilitated use in meta‐analysis; however, the physical activity and sedentary behavior outcomes used did not align with those analyzed in this review. Similarly, Ducheyne 2014a collected and adequately reported a physical activity outcome but used a measure that was not included in this review.
Recruitment bias
The following five domains—recruitment bias, baseline imbalance, loss of clusters, incorrect analysis, and comparability with individually randomized trials—are relevant to cluster‐randomized trials only. Therefore, for each of these domains, we consider the three individually randomized trials to be at low risk of bias (Alhassan 2018a; Baghurst 2014; Werch 2003a).
We judged six studies to be at high risk of recruitment bias because they recruited participants after randomization (Cottrell 2005; De Bourdeaudhuij 2002; Dietsch 1990; Frenn 2013a; Ievers Landis 2005; Yeh 2018a). We reached this judgement for Yeh 2018a following correspondence with the study author.
We considered eight studies to be at low risk of bias (Adamo 2017a; Alhassan 2018a; Baghurst 2014; Crespo 2012a; Lin 2017a; Luepker 1996a; Wang 2007a; Werch 2003a). We judged Adamo 2017a, Crespo 2012a, Lin 2017a, and Luepker 1996a to be at low risk of recruitment bias because researchers randomized clusters after collecting baseline data. We also judged Wang 2007a to be at low risk of recruitment bias because randomization was carried out after participant recruitment but before baseline data collection. We rated Alhassan 2018a, Baghurst 2014, and Werch 2003a to be at low risk of bias for this domain because participants were randomized individually.
For the remaining nine studies, it is unclear whether recruitment and consent occurred before or after randomization (De Bock 2013a; Ducheyne 2014a; Haerens 2006a; Hopper 1992a; Kirks 1982a; Perry 1988a; Petchers 1987; Vandongen 1995; Voll 2013).
Baseline imbalance
We judged risk of bias for the baseline imbalance domain to be high for two studies (Kirks 1982a; Vandongen 1995). Kirks 1982a included only one school (cluster) per study arm, and study authors attributed unanticipated results to one of the classes in the child‐only school being "exceptional" (quote) and noted that it would have been better if the treatment groups were truly matched. In Vandongen 1995, study authors reported significant between‐group differences in some baseline variables at baseline.
We evaluated the remaining 18 cluster‐RCTs to be at unclear risk of bias because similarities and differences between intervention arms or clusters were not reported (Adamo 2017a; Cottrell 2005; Crespo 2012a; De Bock 2013a; De Bourdeaudhuij 2002; Dietsch 1990; Ducheyne 2014a; Frenn 2013a; Haerens 2006a; Hopper 1992a; Ievers Landis 2005; Lin 2017a; Luepker 1996a; Perry 1988a; Petchers 1987; Voll 2013; Wang 2007a; Yeh 2018a).
Because concerns about baseline imbalance are specific to cluster‐RCTs, we judged three studies to be at low risk of bias for this domain (Alhassan 2018a; Baghurst 2014; Werch 2003a).
Loss of clusters
We judged three cluster‐RCTs to be at high risk of bias (De Bock 2013a; Perry 1988a; Voll 2013). De Bock 2013a and Perry 1988a reported that clusters were lost from the trial, and although Voll 2013 did not report on loss of clusters, the very high level of attrition suggests that this was likely.
We rated 13 studies to be at low risk of bias. Of these, we judged 10 cluster‐RCTs in which no clusters were lost to be at low risk of bias (Crespo 2012a; Ducheyne 2014a; Frenn 2013a; Haerens 2006a; Hopper 1992a; Kirks 1982a; Lin 2017a; Luepker 1996a; Wang 2007a; Yeh 2018a). Unpublished information to support this determination was provided by Frenn 2013a, Hopper 1992a, Lin 2017a, and Yeh 2018a. Because this domain is not relevant to individually randomized trials, we judged Alhassan 2018a, Baghurst 2014, and Werch 2003a to be at low risk of bias.
In the remaining seven studies, it is unclear whether any clusters were lost (Adamo 2017a; Cottrell 2005; De Bourdeaudhuij 2002; Dietsch 1990; Ievers Landis 2005; Petchers 1987; Vandongen 1995).
Incorrect analysis
In 10 cluster‐RCTs, study authors did not report adjusting for clustering in their analysis or did not report intracluster correlation coefficients (ICCs) (De Bourdeaudhuij 2002; Dietsch 1990; Ducheyne 2014a; Frenn 2013a; Hopper 1992a; Kirks 1982a; Petchers 1987; Vandongen 1995; Voll 2013; Yeh 2018a). For this reason, we judged these studies to be at high risk of bias for this domain.
We determined nine studies to be at low risk of bias because study authors described how they accounted for clustering in their analyses (Adamo 2017a; Cottrell 2005; Crespo 2012a; De Bock 2013a; Haerens 2006a; Ievers Landis 2005; Lin 2017a; Luepker 1996a; Perry 1988a). Because concerns about adjustment for clustering are specific to cluster‐RCTs, we additionally judged Alhassan 2018a, Baghurst 2014, and Werch 2003a to be at low risk of bias for this domain.
We were unable to assess whether Wang 2007a accounted for clustering.
Comparability with individually randomized trials
None of the 20 cluster‐RCTs provided sufficient information to permit judgment on comparability with individually randomized trials (Adamo 2017a; Cottrell 2005; Crespo 2012a; De Bock 2013a; De Bourdeaudhuij 2002; Dietsch 1990; Ducheyne 2014a; Frenn 2013a; Haerens 2006a; Hopper 1992a; Ievers Landis 2005; Kirks 1982a; Lin 2017a; Luepker 1996a; Perry 1988a; Petchers 1987; Vandongen 1995; Voll 2013; Wang 2007a; Yeh 2018a). This domain is not relevant for individually randomized trials, so we judged Alhassan 2018a, Baghurst 2014, and Werch 2003a to be at low risk of bias.
Other potential sources of bias
We judged six studies to be at high risk of other potential sources of bias (Adamo 2017a; Alhassan 2018a; Ducheyne 2014a; Frenn 2013a; Kirks 1982a; Voll 2013). Ducheyne 2014a, Frenn 2013a, and Kirks 1982a included only one to two clusters per intervention arm. Additionally, Frenn 2013a reported that the sample size was insufficient to examine between‐group differences in the outcomes of interest, and that when caregivers in the child + caregiver group did not want to participate in the intervention, study authors compared their data with data from the child‐only arm. In Voll 2013, some clusters had only one or two participating children. Adamo 2017a reported important baseline imbalances between the child + caregiver and child‐only arms, and Alhassan 2018a reported significant differences in the characteristics of mothers who dropped out and those with complete data.
We judged the remaining 17 studies to be at low risk of bias (Baghurst 2014; Cottrell 2005; Crespo 2012a; De Bock 2013a; De Bourdeaudhuij 2002; Dietsch 1990; Haerens 2006a; Hopper 1992a; Ievers Landis 2005; Lin 2017a; Luepker 1996a; Perry 1988a; Petchers 1987; Vandongen 1995; Wang 2007a; Werch 2003a; Yeh 2018a). Although Baghurst 2014, De Bock 2013a, and Perry 1988a each reported an additional potential source of bias, we determined that these potential sources of bias did not pose a substantial risk, and we judged these studies to be at low risk of bias in this domain. We detected no other potential sources of bias for the 14 remaining studies (Cottrell 2005; Crespo 2012a; De Bourdeaudhuij 2002; Dietsch 1990; Haerens 2006a; Hopper 1992a; Ievers Landis 2005; Lin 2017a; Luepker 1996a; Petchers 1987; Vandongen 1995; Wang 2007a; Werch 2003a; Yeh 2018a).
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings for the main comparison. Dietary behavior change interventions with a caregiver component compared to interventions without a caregiver component for improving children's dietary intake.
| Dietary behavior change interventions with a caregiver component compared to interventions without a caregiver component for improving children's dietary intake | ||||||
| Patient or population: children aged 7 to 18 years Setting: child + caregiver arm: home and school; child‐only arm: school Intervention: dietary behavior change interventions with a caregiver component Comparison: dietary behavior change Interventions without a caregiver component | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk—dietary behavior change Interventions without a caregiver component | Corresponding risk—dietary behavior change interventions with a caregiver component | |||||
|
Percentage of children's total energy intake from saturated fat Measured by food record Assessed at end of intervention (9 months) |
Mean percentage of total energy from saturated fat in the control group was 14.29% | Mean percentage of total energy from saturated fat in the intervention group was 0.42% lower (1.25 lower to 0.41 higher) | ‐ | 207 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | WHO recommends that intake of saturated fat is less than 10% of total energy intake (WHO 2018) |
|
Children's sodium intake (g/d) measured by food record Assessed at end of intervention (9 months) |
Mean sodium intake in the control group was 2.2 g/d | Mean sodium intake in the intervention group was 0.12 g/d less (0.36 less to 0.12 more) | ‐ | 207 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | WHO recommends that adults consume less than 2 grams of sodium per day. This estimate should be adjusted downward for children based on their energy requirements (WHO 2018) |
| Children's fruit and vegetable intake (not measured) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for children's combined fruit and vegetable intake |
| Children's SSB intake (not measured) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for children's SSB intake |
| Children's total physical activity (not measured) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for children's total physical activity |
| Children's MVPA (not measured) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for children's MVPA |
| Adverse effects (not measured) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for adverse effects |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MVPA: moderate to vigorous physical activity; RCT: randomized controlled trial; SSB: sugar‐sweetened beverage; WHO: World Health Organization. | ||||||
| GRADE Working Group grades of evidence. High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded by one level for indirectness: one trial only. bDowngraded by one level for imprecision: CI includes both potentially important benefits and potentially unimportant harms.
Summary of findings 2. Physical activity interventions with a caregiver component compared to interventions without a caregiver component for improving children's physical activity behaviors.
| Physical activity interventions with a caregiver component compared to interventions without a caregiver component for improving children's physical activity behaviors | ||||||
| Patient or population: children aged 3 to 11 years Setting: child + caregiver arm: home, online, school; child‐only arm: school, home Intervention: physical activity interventions with a caregiver component Comparison: physical activity interventions without a caregiver component | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk—physical activity interventions without a caregiver component | Corresponding risk—physical activity interventions with a caregiver component | |||||
|
Percentage of children's total energy intake from saturated fat (not measured) |
‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for percentage of children's total energy intake from saturated fat |
|
Children's sodium intake (not measured) |
‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for children's sodium intake |
| Children's fruit and vegetable intake (not measured) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for children's fruit and vegetable intake |
| Children's SSB intake (not measured) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for children's SSB intake |
|
Children's total physical activity (min/h) Measured by accelerometry Assessed at end of intervention (6 months) |
Mean total physical activity score in the control group was 26.8 min/h | Mean total physical activity score in the intervention group was0.2 min/h more (1.19 less to 1.59 more) | ‐ | 54 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | WHO recommends that physical activity beyond 60 minutes of MVPA per day provides additional benefits (WHO 2010) |
|
Children's MVPA (% time spent/d and min/h) Measured by accelerometry Assessed at end of intervention (12 weeks and 6 months) |
‐ | Mean MVPA score in the intervention group was 0.04 standard deviations higher (0.41 lower to 0.49 higher) | ‐ | 80 (2 RCTs) | ⊕⊕⊕⊝ Moderateb | WHO recommends that youth aged 5 to 17 years should do at least 60 minutes of MVPA daily (WHO 2010) The observed standard deviation of 0.04 probably represents a trivial, non‐significant difference between arms |
| Adverse effects (not measured) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for adverse effects |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MVPA: moderate to vigorous physical activity; RCT: randomized controlled trial; SSB: sugar‐sweetened beverage; WHO: World Health Organization. | ||||||
| GRADE Working Group grades of evidence. High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded by one level for indirectness: one trial only. bDowngraded by one level for risk of bias: high attrition.
Summary of findings 3. Combined dietary and physical activity interventions with a caregiver component compared to interventions without a caregiver component for improving children's dietary intake and physical activity behaviors.
| Combined dietary and physical activity interventions with a caregiver component compared to interventions without a caregiver component for improving children's dietary intake and physical activity behaviors | ||||||
| Patient or population: children aged 4 to 14 years Setting: child + caregiver arm: home, school, not reported; child‐only arm: school, community Intervention: combined dietary and physical activity interventions with a caregiver component Comparison: combined dietary and physical activity interventions without a caregiver component | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk—combined dietary and physical activity interventions without a caregiver component | Corresponding risk—combined dietary and physical activity interventions with a caregiver component | |||||
|
Children's percentage of total energy intake from saturated fat Measured by food frequency questionnaire and 24‐hour recall Follow‐up: end of intervention (9 months) |
Mean percentage of total energy intake from saturated fat in the control group was 10.34% | Mean percentage of total energy intake from saturated fat in the intervention groups was0.06% higher (0.67 lower to 0.80 higher) | ‐ | 216 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | WHO recommends that intake of saturated fat is less than 10% of total energy intake (WHO 2018) |
|
Children's sodium intake (mg/d) Measured by 24‐hour recall Follow‐up: end of intervention (2.5 months and 2.5 years) |
Mean sodium intake in the control group was 3112.11 mg/d | Mean sodium intake in the intervention group was 35.94 mg/d more (322.60 fewer to 394.47 more) | ‐ | 315 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | WHO recommends that adults consume less than 2 grams of sodium per day. This estimate should be adjusted downward for children based on their energy requirements (WHO 2018) |
|
Children's fruit and vegetable intake (servings/d) Measured by food frequency questionnaire Follow‐up: end of intervention (3 years) |
Mean fruit and vegetable intake in the control group was 1.84 servings/d | Mean fruit and vegetable intake in the intervention group was 0.38 servings/d more (0.51 fewer to 1.27 more) | ‐ | 134 (1 RCT) | ⊕⊝⊝⊝ Very lowa,c,d | WHO recommends consuming more than 400 grams of fruit and vegetables per day (WHO 2018) |
|
Children's SSB intake (SSB drinks/d, soft drink glasses/d and regular soda servings/d) Measured by questionnaires Follow‐up: end of intervention (9 months, 21 months, and 3 years) |
‐ | Mean SSB intake in the intervention group was 0.28 standard deviations lower (0.44 lower to 0.12 lower) | ‐ | 651 (3 RCTs) | ⊕⊕⊕⊝ Moderatea | WHO recommends reducing consumption of SSB. The recommendation for intake of free sugars is less than 10% of total energy intake (WHO 2018) The observed standard deviation of 0.28 probably represents a small, significant difference between arms |
|
Children's total physical activity (min/d) Measured by questionnaires Follow‐up: end of intervention (21 months and 2.5 years) |
Mean total physical activity score in the control group was 135.54 min/d | Mean total physical activity score in the intervention group was 1.81 min/d more (15.18 less to 18.8 more) | ‐ | 573 (2 RCTs) | ⊕⊕⊝⊝ Lowa,c | WHO recommends that physical activity beyond 60 minutes of MVPA per day provides additional benefits (WHO 2010) |
|
Children's MVPA (min/d) Measured by questionnaire Follow‐up: end of intervention (2.5 years) |
Mean MVPA score in the control group was 123.97 min/d | Mean MVPA score in the intervention group was 0.05 min/d less (18.57 less to 18.47 more) | ‐ | 622 (1 RCT) | ⊕⊝⊝⊝ Very lowa,c,d | WHO recommends that youth aged 5 to 17 years should do at least 60 minutes of MVPA daily (WHO 2010) |
| Adverse effects (not reported by intervention arm) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data for adverse effects by intervention arm |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MVPA: moderate to vigorous physical activity; RCT: randomized controlled trial; SSB: sugar‐sweetened beverage; WHO: World Health Organization. | ||||||
| GRADE Working Group grades of evidence. High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded by one level for risk of bias: high attrition. bDowngraded by one level for indirectness: small effective sample size. cDowngraded by one level for imprecision: CI includes both potentially important benefits and potentially important harms. dDowngraded by one level for indirectness: one trial only.
Below, we present the results for each outcome by comparison. Despite the inclusion of numerous studies, the scope for meta‐analyses was limited due to heterogeneous outcome measures and measurement time points, as well as absence or incomplete reporting of data for outcomes key to this review. When it was not possible to pool outcome data, we provided a narrative description of study results.
For the most important primary outcomes (children's percentage of total energy intake from saturated fat, children's sodium intake, children's fruit and vegetable intake, children's SSB intake, children's total physical activity, children's moderate to vigorous physical activity [MVPA], and adverse effects), we presented end‐of‐intervention data and reported the GRADE rating in Table 1, Table 2, and Table 3. In our Data and analyses, we grouped data at the end of the intervention and from pre‐specified time points during the intervention, as described in the Methods section.
1. Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component
Data available for this comparison came exclusively from published reports and were reported as end values. With the exception of Lin 2017a and Wang 2007a, we contacted all study authors for additional outcome statistics but received no further data. We did not request additional outcome data from Lin 2017a, as study authors provided all necessary outcome statistics, including the design effect, in the trial report. Intracluster correlation coefficient (ICC) values were not available for any of the other trials, so for these trials, we calculated design effects using an estimated ICC of 0.01, as described in the Methods section. Three studies included in this comparison contributed no data to the analyses (De Bourdeaudhuij 2002; Kirks 1982a; Wang 2007a).
Primary outcomes
Children's dietary intake
Total energy intake
Vandongen 1995 was the only study to report children’s total energy intake. These study authors presented end‐of‐intervention (nine‐month) means and confidence intervals (CIs) separately for boys and girls in mega‐joules (MJ) per day. We merged data for the two sexes, converted CIs to standard deviations, and converted units to kcal/d. After adjustment for the design effect, the effective sample size was 207 children. Our analysis did not detect a difference in total energy intake between the child + caregiver and child‐only arms at the end of the intervention (mean difference [MD] 4.77 kcal/d, 95% CI −141.46 to 151.00, 1 study, n = 207; Analysis 1.1).
1.1. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 1 Children's dietary intake—total energy intake (kcal/d): end of intervention.
Perry 1988a (five‐week intervention) collected 24‐hour recall data at both one‐year and two‐year follow‐up assessments and, from their reporting of other dietary outcomes (percentage of total energy intake from fat and saturated fat), it is clear that study authors calculated total energy intake. However, they did not report total energy intake for either assessment, and we could not retrieve the data. Similarly, De Bourdeaudhuij 2002 assessed diet using a food frequency questionnaire at the end of the intervention (10 weeks) and computed total energy intake to calculate percentage of total energy from fat but did not report data for this outcome.
Percentage of total energy intake from fat
Three studies measured percentage of children's total energy intake from fat (De Bourdeaudhuij 2002; Perry 1988a; Vandongen 1995), but necessary outcome statistics were available only from Vandongen 1995, which presented end‐of‐intervention (nine‐month) means and CIs separately for boys and girls. As directly above, we merged data for the two sexes, converted CIs to standard deviations, and adjusted the sample size for design effect. Our analysis did not detect a difference in this outcome between the child + caregiver and child‐only arms at the end of the intervention (MD −0.34%, 95% CI −2.10 to 1.42, 1 study, n = 207; Analysis 1.2).
1.2. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 2 Children's dietary intake—percentage energy intake from fat: end of intervention.
De Bourdeaudhuij 2002 presented mean percentages at the end of the intervention (10 weeks; child + caregiver arm = 36.3%; child‐only arm = 37.1%) but did not report measures of variance. After adjustment for design effect, the effective sample size for this study was 92 adolescents. Perry 1988a reported statistics for percentage of total energy from fat from the one‐year follow‐up assessment but grouped results from the child + caregiver arm with those from the caregiver‐only arm and results from the child‐only arm with those from the no‐intervention (control) arm. Study authors did not present data for the two‐year follow‐up period.
Percentage of total energy intake from saturated fat
Two studies measured percentage of children's total energy intake from saturated fat (Perry 1988a; Vandongen 1995). As with percentage of children's total energy intake from fat, necessary outcome statistics were available only from Vandongen 1995, because Perry 1988a grouped results from the one‐year follow‐up assessment across study arms, and results for the two‐year follow‐up assessment were not available. For Vandongen 1995, the data were presented and adjusted as described above under "Total energy intake." At the end of the intervention (nine months), our analysis found that the addition of a caregiver component may make little or no difference in this outcome (mean difference [MD] −0.42%, 95% CI −1.25 to 0.41, 1 study, n = 207; Analysis 1.3; low‐quality evidence; Table 1).
1.3. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 3 Children's dietary intake—percentage energy intake from saturated fat: end of intervention.
Percentage of total energy intake from protein
Vandongen 1995 was the only study to measure and report percentage of children's total energy intake from protein. Data were presented and adjusted as described above under "Total energy intake." At the end of the intervention (nine months), our analysis did not detect a difference in this outcome between the child + caregiver and child‐only arms (MD −0.06%, 95% CI −1.06 to 0.94, 1 study, n = 207; Analysis 1.4).
1.4. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 4 Children's dietary intake—percentage energy intake from protein: end of intervention.
Sodium intake
Two studies measured and reported data on children’s sodium intake (Perry 1988a; Vandongen 1995). Because one study reported this outcome at the end of the intervention and the other reported this outcome at a follow‐up time point after the intervention had ended, we did not pool the data from these two studies.
For Perry 1988a (five‐week intervention), outcome statistics (means and standard errors) were published for the one‐year follow‐up assessment, but data were not available for the two‐year assessment. For one‐year follow‐up data, we converted standard errors to standard deviations and adjusted the sample size using the design effect. Our analysis did not detect a difference in sodium intake between the child + caregiver and child‐only arms (MD −0.11 mg/kcal, 95% CI −0.33 to 0.11, 1 study, n = 85; Analysis 1.5).
1.5. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 5 Children's dietary intake—sodium intake (mg/kcal): follow‐up time point.
The Vandongen 1995 data were presented and adjusted according to the same approach described above under "Total energy intake." At the end of the intervention (nine months), study authors found that the addition of a caregiver component might make little or no difference in children's sodium intake (MD −0.12 g/d, 95% CI −0.36 to 0.12, 1 study, n = 207; Analysis 1.6; low‐quality evidence; Table 1).
1.6. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 6 Children's dietary intake—sodium intake (g/d): end of intervention.
Fruit and vegetable intake
No trial in this comparison reported data for combined fruit and vegetable intake.
Two studies measured and reported children's fruit intake (Kirks 1982a; Lin 2017a). Although Kirks 1982a reported mean intake in servings per day at end‐of‐intervention (four‐month) and five‐year follow‐up periods, study authors did not report measures of variance, so data could not be included in the meta‐analysis. After adjustment for the design effect, the effective sample size in Kirks 1982a was 42 children at the end‐of‐intervention assessment and 33 children at the follow‐up assessment. At the end of the intervention, children in the child + caregiver arm ate 3.02 servings of fruit per day, and children in the child‐only arm ate 2.89 servings of fruit per day. At five‐year follow‐up, children in the child + caregiver arm ate 2.38 servings of fruit per day, and children in the child‐only arm ate 2.20 servings of fruit per day. Study authors did not report significant differences in fruit intake between the child + caregiver and child‐only arms. Lin 2017a provided complete outcome statistics for end‐of‐intervention (one‐month) and six‐month follow‐up assessments. After adjustment for the design effect, the effective sample size was 428 children at the end of the intervention and 420 at the follow‐up assessment. Our analysis detected differences between intervention conditions and found higher fruit intake in the child + caregiver arm at the end of the intervention (MD 1.18 servings/d, 95% CI 0.97 to 1.39, 1 study, n = 428; Analysis 1.7) and at follow‐up (MD 1.19 servings/d, 95% CI 0.95 to 1.43, 1 study, n = 420; Analysis 1.8).
1.7. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 7 Children's dietary intake—fruit intake: end of intervention.
1.8. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 8 Children's dietary intake—fruit intake: follow‐up time point.
Kirks 1982a and Lin 2017a also measured and reported children's vegetable intake. As with fruit intake, Kirks 1982a reported mean intake in servings per day at the end of the intervention and at five‐year follow‐up but did not report variance. The sample size was adjusted for the design effect as described above. At the end of the intervention, Kirks 1982a found that children in the child + caregiver arm ate 3.57 servings of vegetables per day, and children in the child‐only arm ate 3.08 servings of vegetables per day. At five‐year follow‐up, children in the child + caregiver arm ate 3.50 servings of vegetables per day, and children in the child‐only arm ate 2.27 servings of vegetables per day. At both time points, study authors reported that vegetable intake was significantly higher in the child + caregiver arm compared to the child‐only arm (P ≤ 0.05). Lin 2017a provided complete outcome statistics for vegetable intake at end‐of‐intervention (one‐month) and six‐month follow‐up assessments. After adjustment for the design effect, our analysis detected differences between intervention conditions and found higher vegetable intake in the child + caregiver arm at the end of the intervention (MD 0.56 servings/d, 95% CI 0.34 to 0.78, 1 study, n = 428; Analysis 1.9) and at follow‐up (MD 0.58 servings/d, 95% CI 0.36 to 0.80, 1 study, n = 420; Analysis 1.10).
1.9. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 9 Children's dietary intake—vegetable intake: end of intervention.
1.10. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 10 Children's dietary intake—vegetable intake: follow‐up time point.
No study reported data on the following primary outcomes: children's dietary intake in terms of percentage of total energy intake from trans fat and carbohydrate and sugar‐sweetened beverage (SSB) and water intake; children's physical activity levels in terms of total, moderate to vigorous, light and weight‐bearing physical activity, steps, and total physical activity score; and adverse effects.
Secondary outcomes
Children's dietary quality
Kirks 1982a measured and reported dietary quality and diversity scores at end‐of‐intervention (four‐month) and five‐year follow‐up periods but did not report measures of variance. Dietary quality was measured on a scale from 0 to 6, and dietary diversity was measured on a scale from 0 to 20. Effective sample sizes at each assessment were the same as reported above for "Fruit and vegetable intake." At the end‐of‐intervention assessment, the dietary quality score was 5.35 in the child + caregiver arm and 4.71 in the child‐only arm, and the dietary diversity score was 12.29 in the child + caregiver arm and 11.08 in the child‐only arm. For both measures, study authors reported the scores to be significantly higher in the child + caregiver arm compared to the child‐only arm (P ≤ 0.05). At five‐year follow‐up, the dietary quality score was 4.54 in the child + caregiver arm and 3.47 in the child‐only arm, and the dietary diversity score was 9.50 in the child + caregiver arm and 10.77 in the child‐only arm. At this assessment, study authors reported the dietary diversity score to be significantly higher (P ≤ 0.05) in the child + caregiver arm. They did not report significant differences in the dietary quality score between study arms.
Prevalence of overweight and obesity among children
Three studies measured height and weight at each study assessment to assess changes in weight status (Perry 1988a; Vandongen 1995; Yeh 2018a). However, no study reported data on prevalence of overweight and obesity after baseline.
Children's body mass index (BMI) or weight‐for‐height parameter
As noted directly above, three studies measured height and weight to evaluate changes in weight status (Perry 1988a; Vandongen 1995; Yeh 2018a). Perry 1988a did not report any results related to this outcome. Vandongen 1995 reported end‐of‐intervention (nine‐month) BMI (not standardized for age and sex) means and CIs separately for boys and girls. As with other outcomes, we converted CIs to standard deviations, and we combined data for the two sexes; after adjustment for the design effect, the effective sample size was 237 children. Yeh 2018a presented end‐of‐intervention (seven‐month) BMI percentile means and standard deviations. After adjustment for the design effect, the effective sample size was 76. At the end of the intervention across these two studies, we did not detect a difference in BMI between the child + caregiver and child‐only arms (standardized mean difference [SMD] −0.08, 95% CI −0.31 to 0.14, 2 studies, n = 313; Tau2 = 0.00; Chi2 = 0.31; degrees of freedom (df) = 1 (P = 0.58); I2 = 0%; Analysis 1.11).
1.11. Analysis.
Comparison 1 Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component, Outcome 11 Children's body mass index or weight‐for‐height parameter—body mass index (value or percentile): end of intervention.
Caregivers' dietary intake
Percentage of total energy intake from fat
De Bourdeaudhuij 2002 measured and reported caregivers' mean percentage of total energy intake from fat for the child + caregiver arm. However, no dietary data were collected from caregivers in the child‐only arm.
No study reported data on the following secondary outcomes: children's sedentary behavior; caregivers' dietary intake in terms of total energy intake, percentage of total energy intake from saturated fat, trans fat, carbohydrates and protein, sodium, fruits and vegetables, SSB, and water intake; and caregivers' physical activity levels in terms of total, moderate to vigorous, light and weight‐bearing physical activity, steps, and total physical activity score.
Summary
Seven studies compared dietary behavior change interventions with and without a caregiver component; three of these studies contributed data to the analyses. Data were available for seven primary outcomes for children's dietary intake: total energy intake, percentage of total energy intake from fat, percentage of total energy intake from saturated fat, percentage of total energy intake from protein, sodium intake, fruit intake, and vegetable intake. Additionally, data were available for children's BMI. We detected a difference between the child + caregiver and child‐only arms for two variables: fruit intake and vegetable intake. For both outcomes, intake was detected to be higher in the child + caregiver arm compared to the child‐only arm.
2. Physical activity interventions with a caregiver component versus interventions without a caregiver component
All data available for this comparison came from published reports. Although we contacted all study authors, they did not respond to our requests for data (Alhassan 2018a; De Bock 2013a; Voll 2013), or they were unable to provide additional statistics (Adamo 2017a; Ducheyne 2014a; Werch 2003a). With the exception of one study (Ducheyne 2014a), all studies contributed data to the analyses. Alhassan 2018a reported change values (means and standard deviations). Adamo 2017a reported both end values (mean and standard deviation) and within‐group change (mean and 95% CI); for all relevant outcomes, we extracted both end values and change values, and for change data, we converted CIs to standard deviations. Other trials reported end values only. When variance was reported as standard error, we converted it to standard deviation.
De Bock 2013a reported ICCs for each outcome, and we used these values to calculate effective sample sizes for this trial. Adamo 2017a adjusted the data in their analyses, and further adjustment was not necessary. For the other cluster‐RCTs (De Bock 2013a; Voll 2013), we used an estimated ICC of 0.01 (as described in the Methods section) to calculate the design effects that we used to adjust sample sizes. No sample size adjustment was necessary for Alhassan 2018a, as mother‐child dyads were individually randomized.
Primary outcomes
Children's dietary intake
Fruit and vegetable intake
De Bock 2013a asked caregivers to report children's fruit and vegetable intake but did not report relevant outcome data.
SSB intake
De Bock 2013a asked caregivers to report children's SSB intake but did not report relevant outcome data.
Children's physical activity levels
Total physical activity
Adamo 2017a measured total physical activity at the midpoint (three months) and the end (six months) of the intervention but reported data for the end‐of‐intervention assessment only. At the end of the intervention, the analysis revealed that addition of a caregiver component may make little or no difference in children's total physical activity levels (MD 0.20 min/h, 95% CI −1.19 to 1.59, 1 study, n = 54; Analysis 2.1; low‐quality evidence; Table 2.
2.1. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 1 Children's physical activity levels—total physical activity: end of intervention.
Moderate to vigorous physical activity
Three studies provided data on MVPA (Adamo 2017a; Alhassan 2018a; De Bock 2013a). As with total physical activity, Adamo 2017a measured MVPA in minutes per hour at the midpoint (three months) and the end (six months) of the intervention but reported only end‐of‐intervention data. Alhassan 2018a measured percentage of time per day spent in MVPA at the midpoint (six weeks) and at the end of the intervention (12 weeks), and reported changes from baseline for both time points. De Bock 2013a reported MVPA in minutes per day at the end of the intervention (six months) and at one‐year follow‐up. For De Bock 2013a, we adjusted the sample size with the design effect.
We grouped change data for Adamo 2017a and Alhassan 2018a and examined end‐of‐intervention data for De Bock 2013a separately because change data were not available and units of measurement differed across the three studies. At the end of the intervention, we did not detect a difference in this outcome in the pooled data from Adamo 2017a and Alhassan 2018a (SMD 0.04, 95% CI −0.41 to 0.49, 2 studies, n = 80; Tau2 = 0.0; Chi2 = 0.57; df = 1 (P = 0.45); I2 = 0%; Analysis 2.2; moderate‐quality evidence; Table 2) nor in the unpooled data from De Bock 2013a (MD 0.60 min/d, 95% CI ‐2.58 to 3.78, 1 study, n = 406; Analysis 2.3).
2.2. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 2 Children's physical activity levels—moderate to vigorous physical activity: end of intervention (change values).
2.3. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 3 Children's physical activity levels—moderate to vigorous physical activity: end of intervention (end values).
When we examined data by time point, we also did not detect differences in MVPA between the child + caregiver and child‐only arms at less than three months (MD −0.20, 95% CI −1.87 to 1.47, 1 study, n = 26; Analysis 2.4), at three to six months or less (end of intervention for all three studies; see Analysis 2.2 and Analysis 2.3 above), and at one‐year follow‐up (MD 1.76 min/d, 95% CI −2.24 to 5.76, 1 study, n = 324; Analysis 2.5).
2.4. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 4 Children's physical activity levels—moderate to vigorous physical activity: all intervention time points.
2.5. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 5 Children's physical activity levels—moderate to vigorous physical activity: follow‐up time point.
A third study reported outcome statistics (mean and standard error) for moderate activity and vigorous activity separately at six‐month follow‐up (approximately three months after the end of the intervention) (Werch 2003a). We clarified one outlier data point with the study author. At this follow‐up period, our analysis did not detect a difference between the child + caregiver and child‐only arms for moderate physical activity (MD 0.04 days/week, 95% CI −0.57 to 0.65, 1 study, n = 296; skewed data; Analysis 2.6) nor for vigorous physical activity (MD 0.48 days/week, 95% CI −0.05 to 1.01, 1 study, n = 296; Analysis 2.7). In the text of their trial report, Alhassan 2018a also discussed changes to vigorous physical activity but did not report data for this variable.
2.6. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 6 Children's physical activity levels—moderate physical activity: follow‐up time point.
2.7. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 7 Children's physical activity levels—vigorous physical activity: follow‐up time point.
Light physical activity
Two studies reported LPA data (Adamo 2017a; Alhassan 2018a). As with total physical activity and MVPA, Adamo 2017a measured LPA at the midpoint (three months) and at the end (six months) of the intervention but reported only end‐of‐intervention data. Alhassan 2018a measured LPA at the midpoint (six weeks) and at the end of the intervention (12 weeks) and reported changes from baseline at both time points.
When we pooled data for the end of the intervention, our analysis did not reveal a difference in LPA between the child + caregiver and child‐only arms (SMD −0.37, 95% CI −0.97 to 0.24, 2 studies, n = 80; Analysis 2.8). We also did not detect a difference in LPA between study arms when we examined data by intervention time point at less than three months (MD −0.03% time spent, 95% CI ‐0.81 to 0.74, 1 study, n = 26; Analysis 2.9) and at three to six or months or less (2 studies; same as Analysis 2.8).
2.8. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 8 Children's physical activity levels—light physical activity: end of intervention.
2.9. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 9 Children's physical activity levels—light physical activity: all intervention time points.
Steps
Adamo 2017a measured steps at the midpoint (three months) and at the end (six months) of the intervention, but midpoint data were not available. At the end of the intervention, our analysis did not detect a difference in steps between the child + caregiver and child‐only arms (MD 0.70 steps/h per 100 steps, 95% CI −0.19 to 1.59, 1 study, n = 54; Analysis 2.10).
2.10. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 10 Children's physical activity levels—steps: end of intervention.
Total physical activity score
Voll 2013 presented mean and standard deviation end values at the end‐of‐intervention (two‐week) assessment. Higher scores indicate more physical activity. After adjustment for design effect, the effective sample size was three. Our analysis of these data did not detect a difference in physical activity scores between the child + caregiver and child‐only arms (MD −0.39, 95% CI −1.36 to 0.58, 1 study, n = 3; Analysis 2.11).
2.11. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 11 Children's physical activity levels—total physical activity score: end of intervention.
No study reported data on the following primary outcomes: children's dietary intake in terms of total energy intake; percentage of total energy intake from fat, saturated fat, trans fat, carbohydrates and protein, and sodium and water intake; children's physical activity levels in terms of weight‐bearing physical activity; and adverse effects.
Secondary outcomes
Children's sedentary behavior
Three studies measured sedentary behavior (Adamo 2017a; Alhassan 2018a; De Bock 2013a). As with other outcomes, end‐of‐intervention (six‐month), but not midpoint (three‐month), data were available for Adamo 2017a. For Alhassan 2018a, outcome statistics were available for the midpoint (six weeks) and end‐of‐intervention (12‐week) time points. De Bock 2013a reported outcome statistics at end‐of‐intervention (six‐month) and one‐year follow‐up periods. For De Bock 2013a, we adjusted the sample size with the design effect.
As with children's MVPA, we grouped change data for Adamo 2017a and Alhassan 2018a and examined end‐of‐intervention data for De Bock 2013a separately. At the end of the intervention, we did not detect a difference in this outcome in the pooled data from Adamo 2017a and Alhassan 2018a (SMD 0.26, 95% CI −0.47 to 0.98, 2 studies, n = 80; Tau2 = 0.0; Chi2 = 2.26; df = 1 (P = 0.13); I2 = 56%; Analysis 2.12) nor in the unpooled data from De Bock 2013a (MD ‐3.40 min/d, 95% CI ‐16.81 to 10.01, 1 study, n = 340; Analysis 2.13).
2.12. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 12 Children's sedentary behavior—sedentary behavior: end of intervention (change values).
2.13. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 13 Children's sedentary behavior—sedentary behavior: end of intervention (end values).
When we examined data by time point, we also did not detect differences in sedentary behavior between the child + caregiver and child‐only arms at less than three months (MD −0.40, 95% CI −6.76 to 7.56, 1 study, n = 26; Analysis 2.14), at three to six or months or less (end of intervention for all three studies; see Analysis 2.12 and Analysis 2.13 above), and at one‐year follow‐up (MD −4.20 min/d, 95% CI −20.18 to 11.78, 1 study, n = 271; Analysis 2.15).
2.14. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 14 Children's sedentary behavior—sedentary behavior: all intervention time points.
2.15. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 15 Children's sedentary behavior—sedentary behavior: follow‐up time point.
Prevalence of overweight and obesity among children
Three studies measured height and weight at each assessment time point (Adamo 2017a;Alhassan 2018a;De Bock 2013a). A fourth study reported collection of parent‐reported height and weight (unclear whether at baseline only or also at the end of the intervention) (Ducheyne 2014a). However, no trial reported prevalence of overweight and obesity.
Children's BMI or weight‐for‐height parameter
Two studies reported BMI (non‐standardized) data (Adamo 2017a; De Bock 2013a). Additionally, Alhassan 2018a calculated BMI for each time point but did not report outcome statistics. As with other outcomes, data were available for Adamo 2017a at the end‐of‐intervention (six‐month) assessment but not at the midpoint (three‐month) assessment. De Bock 2013a reported outcome data at six months (end of the intervention) and at one‐year follow‐up, and we adjusted the sample size with the design effect. We did not detect a difference in BMI between the child + caregiver and child‐only arms at the end of the intervention (six months; MD 0.07, 95% CI −0.21 to 0.35, 2 studies, n = 441; Tau2 = 0.02; Chi2 = 1.58; df = 1 [P = 0.21]; I2 = 37%; Analysis 2.16) nor at one‐year follow‐up (MD −0.18, 95% CI −0.58 to 0.22, 1 study, n = 306; Analysis 2.17).
2.16. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 16 Children's body mass index or weight‐for‐height parameter—body mass index: end of intervention.
2.17. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 17 Children's body mass index or weight‐for‐height parameter—body mass index: follow‐up time point.
Caregivers' physical activity levels
Moderate to vigorous physical activity
Alhassan 2018a measured and reported caregivers' time spent in MVPA at the midpoint (six weeks) and at the end of the intervention (12 weeks). Our analysis did not detect a difference between study arms at the end‐of‐intervention assessment (MD 0.50% time spent, 95% CI −0.77 to 1.77, 1 study, n = 26; Analysis 2.19) nor at the midpoint assessment (MD 0.30% time spent, 95% CI ‐0.52 to 1.12, 1 study, n = 26; Analysis 2.20).
2.19. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 19 Caregiver's physical activity levels—moderate to vigorous physical activity: end of intervention.
2.20. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 20 Caregiver's physical activity levels—moderate to vigorous physical activity: all intervention time points.
Light physical activity
Alhassan 2018a also measured and reported caregivers' time spent in LPA at the midpoint (six weeks) and at the end of the intervention (12 weeks). As with MVPA, we did not observe a difference between study arms at the end‐of‐intervention assessment (MD 1.80% time spent, 95% CI −2.89 to 6.49, 1 study, n = 26; Analysis 2.21) nor at the midpoint assessment (MD −0.60% time spent, 95% CI −6.94 to 5.74, 1 study, n = 26; Analysis 2.22).
2.21. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 21 Caregiver's physical activity levels—light physical activity: end of intervention.
2.22. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 22 Caregiver's physical activity levels—light physical activity: all intervention time points.
Total physical activity score
Voll 2013 presented data for total physical activity score at the end‐of‐intervention (two‐week) assessment. As with the total physical activity score for children, higher values indicate more physical activity. After adjustment for design effect, the effective sample size was three. Our analysis of these data did not detect a difference in physical activity scores between the child + caregiver and child‐only arms (MD −0.25, 95% CI −6.79 to 6.29, 1 study, n = 3; Analysis 2.18).
2.18. Analysis.
Comparison 2 Physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 18 Caregivers' physical activity levels—total physical activity score: end of intervention.
No study reported data on the following secondary outcomes: children's dietary quality; caregivers' dietary intake in terms of total energy intake; percentage of total energy intake from fat, saturated fat, trans fat, carbohydrates and protein, sodium, fruit and vegetable, and SSB and water intake; and caregivers' physical activity levels in terms of total and weight‐bearing physical activity, and steps.
Summary
Six studies compared physical activity interventions with and without a caregiver component, and all but one contributed data to the analyses. Data were available for five primary outcomes for children's physical activity: total physical activity, MVPA, LPA, steps, and total physical activity score. Additionally, data were available for children's sedentary behavior and BMI. Across all outcomes with available data, we did not detect a difference between the child + caregiver and child‐only arms.
3. Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component
Data used for analyses in this comparison came from published reports and correspondence with study authors. We contacted the authors of each trial to request additional data. For three studies (Haerens 2006a; Hopper 1992a; Luepker 1996a), all data included in our analyses were provided by author correspondence. For relevant measured outcomes, Hopper 1992a shared both mean and standard deviation end values and within‐group change; we extracted both types of data. Haerens 2006a provided the same statistics for relevant measured outcomes. However, for prevalence of overweight and obesity, some change values included zero events, so for this outcome, we extracted end values only; for other outcomes, we extracted both end values and change data. Luepker 1996a also provided both mean and standard deviation end values and within‐group change for relevant measured diet and anthropometric outcomes. However, these study authors did not measure physical activity at baseline but did provide end value means and standard deviations for the end‐of‐intervention assessment and for all follow‐up assessments. We extracted end values and change values when they were available. The authors of the seven remaining trials did not respond (Baghurst 2014; Cottrell 2005; Dietsch 1990) or responded but did not provide additional statistics (Crespo 2012a; Frenn 2013a; Ievers Landis 2005; Petchers 1987). When outcome statistics were available for these trials, we reported and extracted end values (means and standard deviations). Three studies contributed no data to the analyses (Baghurst 2014; Frenn 2013a; Petchers 1987).
Two studies reported ICCs (Crespo 2012a; Ievers Landis 2005). Crespo 2012a reported that ICC values ranged from 0 and 0.019 across study outcomes; we therefore used the value at the middle of this range (0.0095) to calculate the design effects for each relevant outcome. Ievers Landis 2005 did not report the baseline ICC for weight‐bearing physical activity (the only relevant study outcome) but noted that the ICC for this variable was similar to that for calcium intake (ICC = 0.029). For this reason, we used the ICC for calcium intake to calculate the design effect for weight‐bearing physical activity. Haerens 2006a and Luepker 1996a provided baseline ICCs for all measured outcomes (except prevalence of overweight and obesity in Luepker 1996a), and we used these values to calculate design effects. For prevalence of overweight and obesity in Luepker 1996a, we applied the ICC for BMI Z score. For three trials that contributed data, but for which ICC values were not available (Cottrell 2005; Dietsch 1990; Hopper 1992a), we calculated design effects using an estimated ICC of 0.01, as described in the Methods section. For all cluster‐RCTs in this comparison, we adjusted sample sizes using the calculated design effects.
Primary outcomes
Children's dietary intake
Total energy intake
Three studies—Haerens 2006a, Hopper 1992a, Luepker 1996a—provided outcome statistics for total energy intake for all assessment time points at which diet was measured (Haerens 2006a at midpoint [nine months] and at the end of the intervention [21 months]; Hopper 1992a at the end of the intervention [2.5 months]; Luepker 1996a at the end of the intervention [2.5 years] and 5.5 years after baseline). Another study—Dietsch 1990—also measured total energy intake at the end of the intervention (nine months); however, outcome statistics for this variable were missing from the available report.
When we grouped end‐of‐intervention data, we did not detect a difference in children's total energy intake between the child + caregiver and child‐only arms (MD 14.45 kcal/d, 95% CI −117.20 to 146.10, 3 studies, n = 440; Tau2 = 0.00; Chi2 = 0.10; df = 2 (P = 0.95); I2 = 0%; Analysis 3.1). When we grouped data collected during and at the end of the intervention periods (Analysis 3.2), we did not detect a difference in total energy intake between the child + caregiver and child‐only arms at less than three months (MD −32.90 kcal/d, 95% CI −363.24 to 297.44, 1 study, n = 70); at longer than six months to one year or less (MD −27.82 kcal/d, 95% CI −200.01 to 144.37, 1 study, n = 111); at longer than one year to two years or less (MD 27.63 kcal/d, 95% CI −168.81 to 224.07, 1 study, n = 99); or at two to three years or less (MD 18.53 kcal/d, 95% CI −191.73 to 228.79, 1 study, n = 271). We also did not detect a difference in total energy intake between the two intervention arms at 5.5‐year follow‐up (MD −52.37 kcal/d, 95% CI −307.64 to 202.90, 1 study, n = 299; Analysis 3.3).
3.1. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 1 Children's dietary intake—total energy intake: end of intervention.
3.2. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 2 Children's dietary intake—total energy intake: all intervention time points.
3.3. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 3 Children's dietary intake—total energy intake: follow‐up time points.
Percentage of total energy intake from fat
Three studies—Haerens 2006a, Hopper 1992a, Luepker 1996a—provided outcome statistics for percentage of children's total energy intake from fat for all assessment time points at which diet was measured (Haerens 2006a at midpoint [nine months] and at the end of the intervention [21 months]; Hopper 1992a at the end of the intervention [2.5 months]; Luepker 1996a at the end of the intervention [2.5 years] and 5.5 years after baseline). A fourth study—Dietsch 1990—also reported end values at the end of the intervention (nine months), and another study—Frenn 2013a—measured dietary fat intake at the six to nine−month follow‐up assessment, but outcome statistics were not available.
When we grouped end‐of‐intervention data, we did not detect a difference in this outcome (MD 1.17%, 95% CI −0.65 to 3.00, 4 studies, n = 563; Tau2 = 0.00; Chi2 = 1.45; df = 3 (P = 0.69); I2 = 0%; Analysis 3.4). We also did not detect a difference in this outcome between arms when we grouped data by time point: at less than three months (MD 0.17%, 95% CI −3.87 to 4.21, 1 study, n = 70; Analysis 3.5); at longer than six months to one year or less (MD 0.58%, 95% CI −2.14 to 3.30, 2 studies, n = 405; Tau2 = 0.00; Chi2 = 0.32; df = 1 [P = 0.57]; I2 = 0%; Analysis 3.5); at longer than one year to two years or less (MD 3.12%, 95% CI −0.79 to 7.03, 1 study, n = 283; Analysis 3.5); at longer than two years to three years or less (MD 0.45%, 95% CI −2.49 to 3.39, 1 study, n = 151; Analysis 3.5); or at 5.5‐year follow‐up (MD −1.06%, 95% CI −4.19 to 2.07, 1 study, n = 168; Analysis 3.6).
3.4. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 4 Children's dietary intake—percentage energy from fat: end of intervention.
3.5. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 5 Children's dietary intake—percentage energy from fat: all intervention time points.
3.6. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 6 Children's dietary intake—percentage energy from fat: follow‐up time point.
Percentage of total energy intake from saturated fat
Outcome statistics for percentage of children's total energy intake from saturated fat were available for two studies: Dietsch 1990 and Luepker 1996a. Dietsch 1990 reported end values at the end of the intervention (nine months), whereas Luepker 1996a provided change data for assessments at the end of the intervention (2.5 years) and at 5.5‐year follow‐up.
When end‐of‐intervention data are merged, it is uncertain whether the addition of a caregiver component reduces children's percentage of total energy intake from saturated fat because the certainty of the evidence is very low (MD 0.06%, 95% CI −0.67 to 0.80, 2 studies, n = 216; Tau2 = 0.00; Chi2 = 0.03; df = 1 [P = 0.87]; I2 = 0%; Analysis 3.7; very low‐quality evidence; Table 3). We also did not detect a difference between intervention arms when we examined data by time point: at longer than six months to one year or less (MD 0.10%, 95% CI −0.75 to 0.95, 1 study, n = 59; Analysis 3.7); at longer than two years to three years or less (MD −0.04%, 95% CI −1.46 to 1.38, 1 study, n = 157; Analysis 3.7); and at 5.5‐year follow‐up (MD −0.54%, 95% CI −1.99 to 0.91, 1 study, n = 174; Analysis 3.8).
3.7. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 7 Children's dietary intake—percentage energy from saturated fat: end of intervention (includes all intervention time points).
3.8. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 8 Children's dietary intake—percentage energy from saturated fat: follow‐up time point.
Percentage of total energy intake from carbohydrates
Hopper 1992a and Luepker 1996a provided outcome statistics for percentage of total energy intake from carbohydrates. End‐of‐intervention (2.5‐month) data were available for Hopper 1992a, and end‐of‐intervention (2.5‐year) and 5.5‐year follow‐up data were available for Luepker 1996a. Another study also measured percentage of total energy intake from carbohydrates at the end of the intervention but did not report outcome statistics (Dietsch 1990).
We observed no differences in percentage of total energy intake from carbohydrates between the child + caregiver and child‐only arms when we grouped end‐of‐intervention data (MD −0.88%, 95% CI −3.49 to 1.74, 2 studies, n = 266; Tau2 = 0.00; Chi2 = 0.00; df = 1 [P = 0.98]; I2 = 0%; Analysis 3.9). We also observed no differences between intervention arms when we examined data by time point: at less than three months (MD −0.92%, 95% CI −5.73 to 3.89, 1 study, n = 70; Analysis 3.9); at longer than two years to three years or less (MD −0.86%, 95% CI −3.98 to 2.26, 1 study, n = 196; Analysis 3.9); or at 5.5‐year follow‐up (MD 0.88%, 95% CI −2.43 to 4.19, 1 study, n = 216; Analysis 3.10).
3.9. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 9 Children's dietary intake—percentage energy from carbohydrates: end of intervention (includes all intervention time points).
3.10. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 10 Children's dietary intake—percentage energy from carbohydrates: follow‐up time point.
Percentage of total energy intake from protein
The same outcome statistics available from Hopper 1992a and Luepker 1996a for percentage of total energy from protein were available for percentage of total energy from carbohydrates. As with percentage of total energy from protein, Dietsch 1990 also measured percentage of total energy intake from protein at the end of the intervention but did not report outcome statistics.
Our analyses did not detect a difference in percentage of children's total energy intake from protein between the child + caregiver and child‐only arms when we grouped end‐of‐intervention data (MD 0.45%, 95% CI −0.80 to 1.69, 2 studies, n = 241; Tau2 = 0.00; Chi2 = 0.09; df = 1 [P = 0.76]; I2 = 0%; Analysis 3.11). We also did not detect a difference between intervention arms when we examined data by time point: at less than three months (MD 0.77%, 95% CI −1.66 to 3.20, 1 study, n = 70; Analysis 3.11); at longer than two years to three years or less (MD 0.33%, 95% CI −1.12 to 1.78, 1 study, n = 171; Analysis 3.11); or at 5.5‐year follow‐up (MD 0.21%, 95% CI −1.22 to 1.64, 1 study, n = 189; Analysis 3.12).
3.11. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 11 Children's dietary intake—percentage energy from protein: end of intervention (includes all intervention time points).
3.12. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 12 Children's dietary intake—percentage energy from protein: follow‐up time point.
Sodium intake
Hopper 1992a and Luepker 1996a provided outcome statistics for sodium intake. Hopper 1992a measured sodium intake at the end of the intervention (2.5 months), and Luepker 1996a measured sodium intake at the end of the intervention (2.5 years) and at 5.5‐year follow‐up.
When end‐of‐intervention data were merged, it is uncertain whether the addition of a caregiver component reduces children's sodium intake because the quality of the evidence is very low (MD 35.94 mg/d, 95% CI −322.60 to 394.47, 2 studies, n = 315; Tau2 = 0.00; Chi2 = 0.01; df = 1 [P = 0.93]; I2 = 0%; Analysis 3.13; very low‐quality evidence; Table 3). When we examined data by time point, we also did not detect a difference in children's sodium intake between intervention arms at less than three months (MD 70.27 mg/d, 95% CI −743.71 to 884.25, 1 study, n = 70; Analysis 3.13), at longer than two years to three years or less (27.67 mg/d, 95% CI −371.70 to 427.04, 1 study, n = 245; Analysis 3.13), and at 5.5‐year follow‐up (MD 60.36 mg/d, 95% CI −397.55 to 518.27, 1 study, n = 270; Analysis 3.14).
3.13. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 13 Children's dietary intake—sodium intake: end of intervention (includes all intervention time points).
3.14. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 14 Children's dietary intake—sodium intake: follow‐up time point.
Fruit and vegetable intake
Crespo 2012a was the only trial to report children's fruit and vegetable intake as a combined outcome variable. Outcome statistics were available for the one‐, two‐, and three‐year (end‐of‐intervention) assessments. At the end of the intervention, it is uncertain whether the addition of a caregiver component increases children's fruit and vegetable intake because the quality of the evidence is very low (MD 0.38 servings/d, 95% CI −0.51 to 1.27, 1 study, n = 134; skewed data; Analysis 3.15; very low‐quality evidence; Table 3). Our analyses also did not detect a difference in this outcome between intervention arms at either of the intermediary assessment time points (Analysis 3.16): at longer than six months to one year or less (MD 0.54 servings/d, 95% CI −0.09 to 1.17, 1 study, n = 216; skewed data); or at longer than one year to two years or less (MD 0.46 servings/d, 95% CI −0.41 to 1.33, 1 study, n = 172; skewed data).
3.15. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 15 Children's dietary intake—fruit and vegetable intake: end of intervention.
3.16. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 16 Children's dietary intake—fruit and vegetable intake: all intervention time points.
Three trials measured children's fruit intake (Cottrell 2005; Dietsch 1990; Haerens 2006a). We did not extract end‐of‐intervention (one‐month) data for this outcome from Cottrell 2005 due to lack of confidence in the values reported. Outcome statistics were available for Dietsch 1990 at the end of the intervention (nine months), and for Haerens 2006a at midpoint (nine months) and at the end of the intervention (21 months).
When we grouped the end‐of‐intervention data, we found that involvement of caregivers probably slightly increases children's fruit intake (SMD 0.23, 95% CI 0.03 to 0.43, 2 studies, n = 417; Tau2 = 0.00; Chi2 = 0.01; df = 1 [P = 0.94]; I2 = 0%; skewed data; Analysis 3.17). When we grouped data by time point (Analysis 3.18), we detected fruit intake to be slightly higher in the child + caregiver arm at longer than six months to one year or less (SMD 0.19, 95% CI 0.01 to 0.38, 2 studies, n = 483; Tau2 = 0.00; Chi2 = 0.00; df = 1 [P = 0.95]; I2 = 0%; skewed data) but not at longer than one year to two years or less (SMD 0.10, 95% CI −0.11 to 0.31, 1 study, n = 358).
3.17. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 17 Children's dietary intake—fruit intake: end of intervention.
3.18. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 18 Children's dietary intake—fruit intake: all intervention time points.
Two trials measured children's vegetable intake (Cottrell 2005; Dietsch 1990). Due to the same concerns noted above for fruit intake, we did not extract end‐of‐intervention (one‐month) statistics for Cottrell 2005. Dietsch 1990 reported outcome statistics for the end of the intervention at nine months. We did not detect a difference in vegetable intake between the child + caregiver and child‐only arms (MD −0.04 servings/d, 95% CI −0.21 to 0.13, 1 study, n = 59; Analysis 3.19).
3.19. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 19 Children's dietary intake—vegetable intake: end of intervention (includes all intervention time points).
Sugar‐sweetened beverage (SSB) intake
Three studies measured intake of SSB (Crespo 2012a; Dietsch 1990; Haerens 2006a). Crespo 2012a measured SSB intake at the the one‐, two‐, and three‐year (end‐of‐intervention) assessments. Dietsch 1990 measured intake of regular soda and punch at the end of the intervention (nine months). We extracted outcome statistics for regular soda only because it was not possible to combine these two categories, and regular soda intake is more closely aligned with overall SSB intake. Haerens 2006a provided outcome statistics for soft drink intake from the study's midpoint (nine months) and end‐of‐intervention (21‐month) assessments.
When we combined data from the three studies, we found that the inclusion of a caregiver component probably slightly reduces SSB intake at the end of the intervention (SMD −0.28, 95% CI −0.44 to −0.12, 3 studies, n = 651; Tau2 = 0.00; Chi2 = 0.29; df = 2 [P = 0.86]; I2 = 0%; skewed data; Analysis 3.20; moderate‐quality evidence; Table 3). When we grouped the data by time point (Analysis 3.21), we detected SSB intake to be slightly lower in the child + caregiver arm at longer than six months to one year or less (SMD −0.25, 95% CI −0.39 to −0.11, 3 studies, n = 799; Tau2 = 0.00; Chi2 = 1.08; df = 2 [P = 0.58]; I2 = 0%; skewed data), but not at longer than one year to two years or less (SMD −0.21, 95% CI −0.45 to 0.03, 2 studies, n = 630; Tau2 = 0.02; Chi2 = 1.95; df = 1 [P = 0.16]; I2 = 49%) or longer than two years to three years or less (SMD −0.23, 95% CI −0.58 to 0.12, 1 study, n = 134; skewed data). We present data for all time points in Figure 4.
3.20. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 20 Children's dietary intake—sugar‐sweetened beverage intake: end of intervention.
3.21. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 21 Children's dietary intake—sugar‐sweetened beverage intake: all intervention time points.
4.
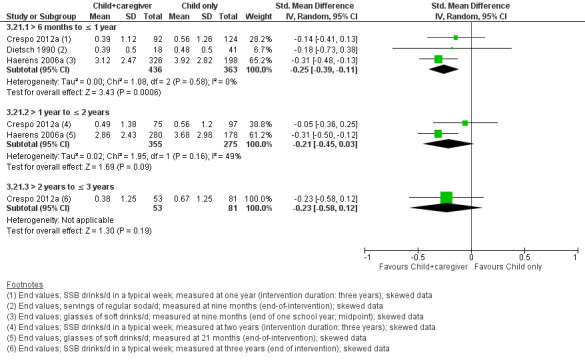
Forest plot of comparison: 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, outcome: 3.21 Children's dietary intake—sugar‐sweetened beverage intake: all intervention time points.
Water intake
Data on water intake were available from three studies (Crespo 2012a; Haerens 2006a; Luepker 1996a). Crespo 2012a reported outcome statistics from one‐year, two‐year, and three‐year (end‐of‐intervention) assessments. Haerens 2006a shared data from assessments at nine months and at the end of the intervention (21 months), and Luepker 1996a shared data for the end‐of‐intervention assessment at 2.5 years but was unable to provide data for 5.5‐year follow‐up.
We did not detect a difference in water intake between the child + caregiver and child‐only arms when we grouped the end‐of‐intervention data (SMD −0.08, 95% CI −0.24 to 0.09, 3 studies, n = 600; Tau2 = 0.00; Chi2 = 1.21; df = 2 [P = 0.55]; I2 = 0%; skewed data; Analysis 3.22). We also did not detect a difference in water intake between intervention arms when we examined the data by time point (Analysis 3.23; skewed data in all three subgroups): at longer than six months to one year or less (SMD 0.06, 95% CI −0.10 to 0.22, 2 studies, n = 610; Tau2 = 0.00; Chi2 = 0.03; df = 1 [P = 0.87]; I2 = 0%); at longer than one year to two years or less (SMD 0.03, 95% CI −0.15 to 0.20, 2 studies, n = 518; Tau2 = 0.00; Chi2 = 0.16; df = 1 [P = 0.69]; I2 = 0%); and at longer than two years to three years or less (SMD −0.18, 95% CI −0.43 to 0.07, 2 studies, n = 254; Tau2 = 0.00; Chi2 = 0.00; df = 1 [P = 0.98]; I2 = 0%).
3.22. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 22 Children's dietary intake—water intake: end of intervention.
3.23. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 23 Children's dietary intake—water intake: all intervention time points.
Children's physical activity levels
Total physical activity
Two studies provided outcome statistics for total physical activity (Haerens 2006a; Luepker 1996a). Haerens 2006a measured total physical activity at midpoint (nine months) and at the end of the intervention (21 months), and Luepker 1996a measured this outcome at the end of the intervention (2.5 years) and at three follow‐up assessments following the intervention (3.5, 4.5, and 5.5 years after baseline). Another study also reported assessment of total physical activity but did not report or share outcome statistics (Ievers Landis 2005).
When end‐of‐intervention data were merged, we found that the addition of a caregiver component may make little or no difference to children's total physical activity (MD 1.81 min/d, 95% CI ‐15.18 to 18.80, 2 studies, n = 573; Tau2 = 0.00; Chi2 = 0.71; df = 1 [P = 0.40]; I2 = 0%; some skewed data; Analysis 3.24; low‐quality evidence; Table 3). We did not detect a difference in total physical activity between trial arms when we examined data by intervention time point (Analysis 3.25) at longer than six months to one year or less (MD 5.49 min/d, 95% CI −18.31 to 29.29, 1 study, n = 107), at longer than one year to two years or less (MD 10.35 min/d, 95% CI −15.78 to 36.48, 1 study, n = 93), and at longer than two years to three years or less (MD −4.45 min/d, 95% CI −26.82 to 17.92, 1 study, n = 480; skewed data). We also did not detect a difference when we examined data from follow‐up assessments by time since the end of the intervention (Analysis 3.26; skewed data in all three subgroups): at longer than six months to follow‐up at one year or less (MD 5.56 min/d, 95% CI −17.09 to 28.21, 1 study, n = 589); at longer than one year to follow‐up of two years or less (MD 1.71 min/d, 95% CI −16.91 to 20.33, 1 study, n = 587); and at longer than two years to follow‐up of three years or less (MD 4.68 min/d, 95% CI −13.61 to 22.97, 1 study, n = 505).
3.24. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 24 Children's physical activity levels—total physical activity: end of intervention.
3.25. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 25 Children's physical activity levels—total physical activity: all intervention time points.
3.26. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 26 Children's physical activity levels—total physical activity: follow‐up time points.
Moderate to vigorous physical activity
Two studies provided outcome statistics for MVPA (Haerens 2006a; Luepker 1996a). Haerens 2006a measured this outcome at midpoint (nine months) and at the end of the intervention (21 months), but we could retrieve complete statistics only for the midpoint assessment. Luepker 1996a measured and provided data for this outcome at the end of the intervention (2.5 years) and at three follow‐up assessments after the intervention (3.5, 4.5, and 5.5 years after baseline). Another study also assessed MVPA and used these data in analyses but did not report or share outcome statistics (Frenn 2013a).
At the end‐of‐intervention assessment (Luepker 1996a only), it is uncertain whether the addition of a caregiver component increases MVPA because the quality of the evidence is very low (MD −0.05 min/d, 95% CI −18.57 to 18.47, 1 study, n = 622; skewed data; Analysis 3.27; very low‐quality evidence; Table 3). We also did not detect a difference in MVPA at any intervention (Analysis 3.28) or follow‐up (Analysis 3.29) time point: longer than six months to one year or less (MD 4.99 min/d, 95% CI −25.75 to 35.73, 1 study, n = 7); longer than two years to three years or less (MD −0.05 min/d, 95% CI −18.57 to 18.47, 1 study, n = 622; skewed data); longer than six months to one year or less after the end of the intervention (MD 5.08 min/d, 95% CI −13.21 to 23.37, 1 study, n = 763; skewed data); longer than one year to two years or less after the end of the intervention (MD 5.89 min/d, 95% CI −8,65 to 20.43, 1 study, n = 760; skewed data); and longer than two years to three years or less after the end of the intervention (MD −1.38 min/d, 95% CI −15,26 to 12.50, 1 study, n = 655; skewed data).
3.27. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 27 Children's physical activity levels—moderate to vigorous physical activity: end of intervention.
3.28. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 28 Children's physical activity levels—moderate to vigorous physical activity: all intervention time points.
3.29. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 29 Children's physical activity levels—moderate to vigorous physical activity: follow‐up time points.
Light physical activity
Two studies provided outcome statistics for LPA (Haerens 2006a; Luepker 1996a). As with MVPA, Haerens 2006a measured this outcome at midpoint (nine months) and at the end of the intervention (21 months), but we could retrieve complete statistics only for the midpoint assessment. Luepker 1996a measured and provided data for the end‐of‐intervention (2.5 years) assessment and for three follow‐up assessments after the intervention (3.5, 4.5, and 5.5 years after baseline).
At the end‐of‐intervention assessment (Luepker 1996a only), we did not detect a difference in LPA between the child + caregiver and child‐only arms (MD −4.16 min/d, 95% CI −12.07 to 3.75, 1 study, n = 484; skewed data; Analysis 3.30). We also did not detect a difference in LPA at any intervention (Analysis 3.31) or follow‐up (Analysis 3.32) time point: longer than six months to one year or less (MD 8.06 min/d, 95% CI −135.25 to 151.37, 1 study, n = 4); longer than two years to three years or less (MD −4.16 min/d, 95% CI −12.07 to 3.75, 1 study, n = 484; skewed data); longer than six months to one year or less after the end of the intervention (MD 0.89 min/d, 95% CI −8.55 to 10.33, 1 study, n = 594; skewed data); longer than one year to two years or less after the end of the intervention (MD −2.72 min/d, 95% CI −11.27 to 5.83, 1 study, n = 593; skewed data); or longer than two years to three years or less after the end of the intervention (MD 5.99 min/d, 95% CI −3.40 to 15.38, 1 study, n = 510; skewed data).
3.30. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 30 Children's physical activity levels—light physical activity: end of intervention.
3.31. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 31 Children's physical activity levels—light physical activity: all intervention time points.
3.32. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 32 Children's physical activity levels—light physical activity: follow‐up time points.
Weight‐bearing physical activity
Ievers Landis 2005 did not collect data immediately following the intervention (approximately six months) but measured outcomes at one year, two years, and three years after baseline. Data from the two‐year and three‐year follow‐up assessments were not reported and could not be retrieved. At the first follow‐up assessment, study authors measured weight‐bearing physical activity in hours per week, but on account of high skewness and kurtosis collapsed data into six categories ranging from zero (no weight‐bearing physical activity) to five (more than four hours of weight‐bearing physical activity per week). The analysis did not detect a difference in this outcome between the child + caregiver and child‐only arms (MD 0.20 hours/week, 95% CI −0.37 to 0.77, 1 study, n = 121; skewed data; Analysis 3.33).
3.33. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 33 Children's physical activity levels—weight‐bearing physical activity: follow‐up time point.
Steps
Cottrell 2005 reported steps per week for each week of the four‐week intervention. The analysis did not detect a difference in the average number of steps per week between the child + caregiver and child‐only arms in the final week of the intervention (MD 2016.00 steps/week, 95% CI −75.37 to 4107.37, 1 study, n = 44; Analysis 3.34) or during any preceding week (Analysis 3.35): first week (MD 327.00 steps/week, 95% CI −1816.45 to 2470.45, 1 study, n = 44); second week (MD 990.00 steps/week, 95% CI −818.08 to 2798.08, 1 study, n = 44); or third week (MD 1396.00 steps/week, 95% CI −683.59 to 3475.59, 1 study, n = 44).
3.34. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 34 Children's physical activity levels—steps: end of intervention.
3.35. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 35 Children's physical activity levels—steps: all intervention time points.
Adverse effects
Ievers Landis 2005 indicated, "No adverse events were reported by any of the study participants" (quote) but did not give data or provide information on what measures were used.
No study reported data on the following primary outcomes: children's dietary intake in terms of percentage of total energy intake from trans fat; and children's physical activity levels in terms of total physical activity score.
Secondary outcomes
Children's sedentary behavior
Luepker 1996a measured time spent watching television or playing video games at the end of the intervention (2.5 years) and at follow‐up assessments at 3.5 years, 4.5 years, and 5.5 years after baseline. The analysis did not detect a difference in sedentary behavior between the child + caregiver and child‐only arms at the end of the intervention (MD 12.42 min/d, 95% CI −27.16 to 52.00, 1 study, n = 379; skewed data; Analysis 3.36), nor at any of the follow‐up assessments (Analysis 3.37): longer than six months to one year or less after the end of the intervention (MD 11.87 min/d, 95% CI −31.27 to 55.01, 1 study, n = 465; skewed data); longer than one year to two years or less after the end of the intervention (MD 13.41 min/d, 95% CI −12.80 to 39.62, 1 study, n = 464; skewed data); and longer than two years to three years or less after the end of the intervention (MD 7.46 min/d, 95% CI −19.05 to 33.97, 1 study, n = 399; skewed data).
3.36. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 36 Children's sedentary behavior—sedentary behavior: end of intervention (includes all intervention time points).
3.37. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 37 Children's sedentary behavior—sedentary behavior: follow‐up time points.
Prevalence of overweight and obesity among children
Four studies measured height and weight at each study assessment (Crespo 2012a; Haerens 2006a; Hopper 1992a; Luepker 1996a). Crespo 2012a reported the percentage of overweight children and the percentage of obese children in their sample. We summed these values at each assessment (one year, two years, and at the end of the intervention at three years) and converted the percentages to numbers. Haerens 2006a also provided percentages of overweight and obese children at nine months and 21 months (end of intervention), and we converted these percentages to numbers. Hopper 1992a did not use these data to calculate prevalence of overweight and obesity and were unable to calculate this outcome. Luepker 1996a provided the number of overweight and obese children at the end of the intervention (2.5 years) and at follow‐up assessment 5.5 years after baseline.
Upon pooling of end‐of‐intervention data for Crespo 2012a, Haerens 2006a, and Luepker 1996a, our analysis did not reveal a difference in prevalence of overweight and obesity among children in the child + caregiver and child‐only arms (risk ratio [RR] 1.02, 95% CI 0.89 to 1.17, 3 studies, n = 1866; Tau2 = 0.00; Chi2 = 0.32; df = 2 [P = 0.85]; I2 = 0%; Analysis 3.38). We also did not detect a difference in prevalence of overweight and obesity at any intervention (Analysis 3.39) or follow‐up (Analysis 3.40) time point: longer than six months to one year or less (RR 1.02, 95% CI 0.80 to 1.30, 2 studies, n = 641; Tau2 = 0.00; Chi2 = 0.42; df = 1 [P = 0.51]; I2 = 0%); longer than one year to two years or less (RR 0.98, 95% CI 0.76 to 1.27, 2 studies, n = 590; Tau2 = 0.00; Chi2 = 0.06; df = 1 [P = 0.81]; I2 = 0%); longer than two years to three years or less (RR 1.02, 95% CI 0.88 to 1.18, 2 studies, n = 1448; Tau2 = 0.00; Chi2 = 0.32; df = 1 [P = 0.57]; I2 = 0%); and longer than two years to three years or less after the end of the intervention (RR 1.13, 95% CI 0.95 to 1.35, 1 study, n = 1201).
3.38. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 38 Prevalence of overweight and obesity among children—prevalence: end of intervention.
3.39. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 39 Prevalence of overweight and obesity among children—prevalence: all intervention time points.
3.40. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 40 Prevalence of overweight and obesity among children—prevalence: follow‐up time point.
Children's BMI or weight‐for‐height parameter
Five studies calculated children's BMI as an outcome (Crespo 2012a; Frenn 2013a; Haerens 2006a; Hopper 1992a; Luepker 1996a). Crespo 2012a reported both BMI Z scores and percentiles. To avoid duplicative evaluation of this outcome, we extracted Z scores only. Frenn 2013a calculated change in child BMI percentiles by group but did not report or provide outcome statistics. Hopper 1992a provided BMI (not standardized for age and sex) at the end of the intervention. Haerens 2006a provided BMI Z scores at midpoint (nine months) and at the end of the intervention (21 months), and Luepker 1996a provided BMI Z scores at the end of the intervention (2.5 years) and the follow‐up assessment of 5.5 years after baseline.
Upon pooling of end‐of‐intervention data for Crespo 2012a, Haerens 2006a, Hopper 1992a, and Luepker 1996a, we did not detect a difference in children's BMI (or BMI Z score) between the child + caregiver and child‐only arms (SMD 0.05, 95% CI −0.04 to 0.15, 4 studies, n = 1861; Tau2 = 0.00; Chi2 = 2.05; df = 3 [P = 0.56]; I2 = 0%; some skewed data; Analysis 3.41). We detected differences between study arms at one time point, with children in the child + caregiver arm found to have a slightly higher BMI compared to children in the child‐only arm at three years after the end of the intervention (MD 0.08, 95% CI 0.01 to 0.15, 1 study, n = 1189; Analysis 3.43). We did not detect a difference in BMI at other time points (Analysis 3.42): less than three months (MD 0.20, 95% CI −0.26 to 0.66, 1 study, n = 72); longer than six months to one year or less (MD −0.01, 95% CI −0.17 to 0.15, 2 studies, n = 612; Tau2 = 0.00; Chi2 = 0.03; df = 1 [P = 0.87]; I2 = 0%; skewed data); longer than one year to two years or less (MD −0.04, 95% CI −0.21 to 0.14, 2 studies, n = 517; Tau2 = 0.00; Chi2 = 0.13; df = 1 [P = 0.72]; I2 = 0%; skewed data); and longer than two years to three years or less (MD 0.07, 95% CI −0.03 to 0.18, 2 studies, n = 1444; Tau2 = 0.00; Chi2 = 0.45; df = 1 [P = 0.50]; I2 = 0%; skewed data). We present data for all intervention time points in Figure 5 and for the follow‐up time point in Figure 6.
3.41. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 41 Children's body mass index or weight‐for‐height parameter—body mass index: end of intervention.
3.43. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 43 Children's body mass index or weight‐for‐height parameter—body mass index: follow‐up time point.
3.42. Analysis.
Comparison 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, Outcome 42 Children's body mass index or weight‐for‐height parameter—body mass index: all intervention time points.
5.
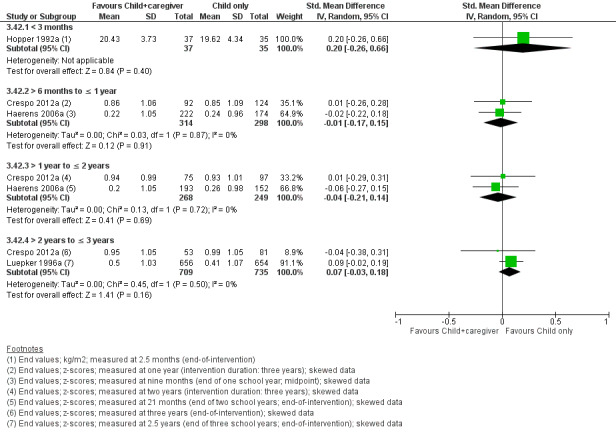
Forest plot of comparison: 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, outcome: 3.42 Children's body mass index or weight‐for‐height parameter—body mass index: all intervention time points.
6.
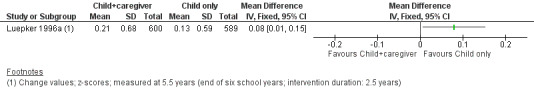
Forest plot of comparison: 3 Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component, outcome: 3.43 Children's body mass index or weight‐for‐height parameter—body mass index: follow‐up time point.
Caregivers' dietary intake
Total energy intake
Dietsch 1990 and Hopper 1992a measured total energy intake. However, as noted in the Included studies section, the caregiver sample from Dietsch 1990 included those with children in sixth through eighth grades at participating schools, and the child sample was restricted to seventh grade students. For this reason, we have not used these data in this review. Hopper 1992a collected data only from caregivers in the child + caregiver only arm, so no comparison is available for this outcome or others.
Percentage of total energy intake from fat
Frenn 2013a measured percentage of total energy intake from fat but did not report or provide outcome statistics. Two other studies also measured percentage of total energy intake from fat (Dietsch 1990; Hopper 1992a), but due to the methodological issues noted above under "Total energy intake," we have not used these data in this review.
Percentage of total energy intake from saturated fat
Two studies measured percentage of total energy intake from saturated fat (Dietsch 1990; Hopper 1992a), but due to the methodological issues noted above under "Total energy intake," we have not used these data in this review.
Percentage of energy from carbohydrates
Two studies measured percentage of total energy intake from carbohydrates (Dietsch 1990; Hopper 1992a), but due to the methodological issues noted above under "Total energy intake," we have not used these data in this review.
Percentage of total energy intake from protein
Two studies measured percentage of total energy intake from protein (Dietsch 1990; Hopper 1992a), but due to the methodological issues noted above under "Total energy intake," we have not used these data in this review.
Caregivers' physical activity levels
Moderate to vigorous physical activity
Frenn 2013a measured caregivers' MVPA and used this variable in analyses but did not report or share outcome statistics.
Steps
Cottrell 2005 measured and reported the average number of weekly steps taken by caregivers in the child + caregiver arm for each week of the intervention but did not assess this outcome among caregivers in the child‐only arm.
No study reported data on the following secondary outcomes: children's dietary quality; caregivers' dietary intake in terms of percentage of total energy intake from trans fat, sodium, fruit and vegetable, SSB, and water intake; and caregivers' physical activity levels in terms of total, light, and weight‐bearing physical activity, and total physical activity score.
Summary
Ten studies compared dietary and physical activity interventions with and without a caregiver component, and seven of these studies contributed data to the analyses. Data were available for 11 primary outcomes for children's dietary intake: total energy intake; percentage of total energy intake from fat; percentage of total energy intake from saturated fat; percentage of energy intake from carbohydrates; and percentage of total energy intake from protein, sodium intake, fruit and vegetable intake, fruit intake, vegetable intake, SSB intake, and water intake. Data were available for five primary outcomes for children's physical activity levels: total physical activity, MVPA, LPA, weight‐bearing physical activity, and steps. Additionally, data were available for children's sedentary behavior, prevalence of overweight and obesity, and BMI. Statistically significant differences between the child + caregiver and child‐only arms were identified for three outcomes. At the end of the intervention, we detected a small positive effect of the caregiver component on children's SSB intake and fruit intake. When we grouped data by time point, we found children in the child + caregiver arm also had higher fruit intake compared to children in the child‐only arm, when measured at longer than six months to one year or less from baseline. We also found children in the child + caregiver arm to have a higher BMI compared to children in the child‐only arm three years after the end of a 2.5‐year intervention.
Discussion
Summary of main results
This review evaluated the effects of caregiver involvement in interventions with children to improve their dietary intake and physical activity behaviors.
Our search yielded 28,927 unique records (28,910 from searching of databases and 17 from additional sources). Following screening, 23 studies met our inclusion criteria, with a total sample of approximately 12,192 children in the relevant study arms. Seven studies examined dietary behavior change interventions with a caregiver component, six studies examined physical activity interventions with a caregiver component, and 10 studies examined combined dietary and physical activity interventions with a caregiver component. We contacted the authors of all but one English language study (n = 21) to request outcome data not included in the published papers and received additional outcome data for three studies. Authors of 11 studies responded to say that data beyond what was included in the published reports were no longer available or could not be provided, and authors of seven studies did not respond to our requests.
In total, 16 studies contributed data to our analyses. We were able to perform 20 meta‐analyses to examine end‐of‐intervention effects and effects from individual trials when relevant outcome data were not available or could not be pooled for more than one study. In the diet‐only comparison, we detected a small significant effect on children's fruit intake and children's vegetable intake, with children in the child + caregiver arm consuming more fruits and vegetables than children in the child‐only arm. This finding was based on data from one study in Iran with an effective sample size of 428 children. In the combined diet and physical activity comparison, we observed evidence of a small significant effect (moderate‐quality evidence) on children's sugar‐sweetened beverage (SSB) intake, with children in the child + caregiver arm consuming less SSB than children in the child‐only arm (Table 3). This finding was based on data from three cluster‐randomized controlled trials (RCTs) with a combined effective sample size of 651 children. We also observed a small significant effect on children's fruit intake, with children in the child + caregiver arm consuming more fruit than children in the child‐only arm (two studies contributing evidence; n = 417). We did not identify conclusive evidence of an effect on any other primary or secondary outcome at the end of the intervention.
When we grouped data by assessment time points during and after the intervention period, we were able to perform an additional 13 meta‐analyses, and we examined effects from individual trials when data from multiple trials were not available to be pooled. As with our findings related to end‐of‐intervention data, we observed evidence of an effect for fruit intake and vegetable intake in the diet‐only comparison, with children in the child + caregiver arm consuming slightly more fruits and more vegetables than children in the child‐only arm five months after the end of the intervention (one study contributing evidence; n = 420). We did not observe evidence of an effect for any outcome in the physical activity−only comparison. In the combined diet and physical activity comparison, we found evidence of effects of caregiver involvement for children's SSB intake, fruit intake, and body mass index (BMI) at specific time points. For SSB, we found caregiver involvement to have a positive effect on children's SSB intake (lower intake) when measured at longer than six months to one year or less (three studies contributing evidence; n = 799), but not when SSB intake was measured at longer than one year to two years or less (two studies contributing evidence; n = 630) or longer than two years to three years or less (one study contributing evidence; n = 134). There was a small positive effect of caregiver involvement on children's fruit intake when measured at longer than six months to one year or less (two studies contributing evidence; n = 483), but not when fruit intake was measured at longer than one year to two years or less (one study contributing evidence; n = 358). Also, there was a small negative effect of caregiver involvement on BMI at three years after the end of the intervention (one study contributing evidence; n = 1189).
Due to the limited number of studies with relevant outcomes, we were unable to conduct our preplanned subgroup and sensitivity analyses (Morgan 2017). Within a single comparison, no outcome had evidence from at least five studies. In fact, across all comparisons, only three outcomes—children's total energy intake from fat, moderate to vigorous physical activity (MVPA), and BMI—had evidence from five or more studies. We could not evaluate adverse effects because no trial reported relevant outcome data. In research, the investigators’ priority is to determine the intervention’s effectiveness while protecting the safety of participants. It is prudent for researchers to contribute to improvements in the safety of interventions by tracking and reporting all adverse events. Findings of impact on caregivers' dietary intake and on physical activity behaviors were also scarce; only two studies measured caregivers' physical activity and none measured caregivers' dietary intake for both intervention arms. This was not unexpected given that all but one study focused on evaluating children's behavior and health outcomes.
Thirteen studies reported use of a behavior change model or theory underpinning the intervention. Based on available reports of intervention activities, behavior change techniques (BCTs) used in the child‐only arm fit within an average of four BCT clusters (range one to nine), with the most common being "shaping knowledge" (21 studies), "comparison of behavior" (13 studies), "feedback and monitoring" (12 studies), and "repetition and substitution" (11 studies). The additional intervention components administered to the child + caregiver arm aligned with an average of five (range one to nine) BCT clusters, with the most common being "shaping knowledge" (21 studies), "feedback and monitoring" (14 studies), "social support" (14 studies), and "natural consequences" (11 studies).
Overall, current evidence is insufficient to support caregiver involvement in dietary and physical activity behavior change interventions. Involvement of caregivers may or may not be useful or detrimental.
Overall completeness and applicability of evidence
This review summarizes findings from three individually randomized RCTs and 20 cluster‐RCTs. Studies were published between 1982 and 2019. In over 35 years of research, the body of evidence is not large enough and of high enough quality to provide definitive answers about whether caregiver involvement in these types of interventions is effective. A major limitation is the limited number of studies per comparison that addressed each outcome. This prevented subgroup analyses for age, country or setting, active versus inactive caregiver component, duration versus intensity of intervention, individual versus group context, and BCT clusters employed, as well as sensitivity analyses to assess the influence of studies' risk of bias, attrition, and study design.
All but two studies took place in a high‐income country, and those took place in upper middle‐income countries (Iran and China). This is an important limitation because patterns of obesity, as well as the quantity and nature of public health initiatives to address obesity and its risk factors, differ between countries at different income levels (Black 2013; De Onis 2010; Lobstein 2015; Ng 2014; Roberto 2015). The child‐only component of 15 trials was based in schools, two in preschools, one in day cares, one at Girl Scouts, one at home, and three in multiple settings; the caregiver component typically was administered at the same setting or through materials sent home or delivered online. It is unclear whether the evidence would be generalizable to children in low‐ or middle‐income countries or to interventions conducted in other settings.
Use of an established BCT taxonomy and standardized terminology to describe intervention content facilitates evaluation of which activities and techniques support behavior change (Michie 2015). Studies included in this review, especially smaller and older studies, did not always report intervention strategies completely, and only one study systematically described the use of BCTs following an established framework (Lin 2017a). We extracted those strategies for which we had confidence and categorized them by BCT cluster. Lack of detail in reporting the BCTs may have limited completeness of the evidence.
Several interventions were designed specifically to reach children from low‐income households or other vulnerable population subgroups. For example, Alhassan 2018a targeted African American girls, Baghurst 2014 tested the intervention in a school with a large low‐income student population, Crespo 2012a targeted Latino children living near the US−Mexico border, and Yeh 2018a focused on African American children attending early childhood education centers for low‐income children. We sought to systematically identify factors relevant to health inequalities using the PROGRESS‐Plus checklist. However, incomplete reporting of PROGRESS‐Plus characteristics combined with insufficient evidence limited our ability to determine the extent to which caregiver involvement in children's diet and physical activity interventions may promote health equity. Although economic disadvantage appears to be an important factor in site selection for some studies, it is not clear how factors such as household income, race, ethnicity, or other social markers such as gender may interact to contribute to particular outcomes.
Most trials did not have published protocols, and only four were registered in a trial registry (Adamo 2017a; Alhassan 2018a; De Bock 2013a; Lin 2017a). For most interventions, study authors did not pre‐specify the specific diet and physical activity outcomes of interest. Often, the measurement instruments employed could be used to generate a wider range of outcomes than those reported or provided by the study authors. For instance, three studies measured diet using 24‐hour dietary recall, which captures information about all foods and beverages consumed. Technically, any diet outcome can be calculated from 24‐hour dietary recall data. However, the outcomes of interest to this review often were not available in the included trials. Advances in nutrition and public health sciences also may have contributed to the diversity of diet and physical activity outcomes measured and reported by the trial authors.
Unfortunately, the included studies did not evaluate all of the outcomes of interest to this review. In particular, no data are available on children's trans fat intake, caregivers' dietary intake, or adverse effects. As noted under Differences between protocol and review, we did not limit this review to outcomes measured by validated instruments. Nonetheless, when diet or physical activity was measured via self‐reported or caregiver‐reported instruments, most study authors described evaluation of instrument reliability and validity.
The overall applicability of evidence is limited. At the end of the intervention, outcome data were available for slightly more than half of the outcomes of interest, and meta‐analysis was possible for one‐third of outcomes. The number of participants included in analyses varied, with effective sample sizes ranging from n = 3 for child and caregiver physical activity score in the physical activity−only intervention comparison to n = 1866 for prevalence of overweight and obesity among children in the combined diet and physical activity−intervention comparison.
Quality of the evidence
We noted several limitations in the methods of the included studies. As shown in Figure 3, we considered one study to be at high risk of selection bias due to inadequate random sequence generation, one to be at high risk of selection bias due to insufficient concealment of allocation, one to be at high risk of detection bias, 16 to be at high risk of attrition bias, 14 to be at high risk of reporting bias, six to be at high risk of recruitment bias, two to be at high risk of bias due to baseline imbalances, three to be at high risk of bias due to loss of clusters, 10 to be at high risk of bias due to incorrect analyses, and six to be at high risk of other sources of bias. We did not assess any studies to be at high risk of performance bias. Further, of the 23 included trials, 15 did not report a priori calculating of the sample size needed to achieve adequate power, and several studies noted inadequate sample size or power to be a study limitation.
We assessed and reported the overall quality of evidence for the seven outcomes we consider most important for this review in the "Summary of findings" tables using the GRADE approach (Schünemann 2011). For the diet‐only comparison, we judged the quality of the evidence to be low for the two outcomes for which data were available (children's percentage of total energy intake from saturated fat and sodium intake). We downgraded the quality for both outcomes for indirectness and imprecision because the data came from only one trial, and the confidence intervals (CIs) included both potentially important benefits and potentially unimportant harms. For the physical activity−only comparison, we assigned total physical activity a low quality rating and MVPA a moderate quality rating. We downgraded the quality of the evidence for both outcomes for risk of bias because of high attrition, and we additionally downgraded total physical activity for indirectness because only one trial contributed data. For the combined diet and physical activity comparison, we assigned four outcomes a very low quality rating (children's percentage of total energy intake from saturated fat, sodium intake, fruit and vegetable intake, and MVPA), one outcome a low quality rating (children's total physical activity), and one outcome a moderate quality rating (children's SSB intake). We downgraded all outcomes for high attrition. For all except SSB intake, we also downgraded the quality of the evidence for imprecision because the CIs include both potentially important benefits and potentially important harms. We additionally downgraded the quality of the evidence for children's percentage of total energy intake from saturated fat, sodium intake, fruit and vegetable intake, and MVPA for indirectness, either because data were drawn from one trial only or because the effective sample size was small, or for both reasons.
In summary, we have limited confidence in the evidence, and future, high‐quality research is likely to have an important impact on confidence in the estimate of intervention effect. Readers should interpret the findings of this review with caution due to the limited number of studies contributing to the analyses for each outcome and comparison, diversity of intervention design and content, heterogeneity in outcome measurement, and poor reporting for some studies. Based on the evidence reviewed, we cannot recommend or refute caregiver involvement in interventions to improve children's dietary intake or physical activity behavior.
Potential biases in the review process
To identify all relevant studies, we searched 17 databases for RCTs and quasi‐RCTs that investigated the effects of caregiver involvement on interventions for improving children’s dietary intake and physical activity, including those intended to prevent overweight and obesity. We searched MEDLINE using the sensitivity and precision−maximizing version of the Cochrane Highly Sensitive Search Strategy for identifying randomized trials (Lefebvre 2008). We adapted this search, as appropriate, for the other databases. We screened the reference lists of included studies and relevant reviews to identify additional trials not found by electronic searches. In total, we screened more than 28,900 titles and abstracts, and we believe it is unlikely that we missed any important trials.
To avoid bias, we independently screened the titles and abstracts of all records identified by the searches in duplicate for study eligibility; for any study considered to be relevant by at least one review author, two review authors independently assessed the full‐text report for eligibility. We independently and in duplicate extracted data from eligible studies using a standardized, pre‐piloted data extraction form, and the first review author resolved all discrepancies. Two review authors also independently evaluated risk of bias for the included studies and reached consensus on any disagreements through discussion. Not all trial authors responded to our requests for data or were able to provide the necessary outcome data. In such cases, we could not include the data for those outcomes in the review. When published reports indicated measurement of an outcome, we reported that outcome in the corresponding Characteristics of included studies table and noted data availability.
We have declared our Declarations of interest and Sources of support. We adhered as far as possible to our published protocol (Morgan 2017), and we documented all deviations in the Differences between protocol and review section.
Agreements and disagreements with other studies or reviews
Multiple reviews have documented that prevention interventions targeting children's individual diet and physical activity behaviors have modest or no effect on obesity (Brown 2019; Kobes 2018; Waters 2011). However, the authors of the most recent Cochrane Review on this topic emphasized that more nuanced categorization of intervention components is needed (Brown 2019). Our present review contributes to addressing this gap in knowledge by focusing on one specific intervention component: caregiver involvement.
For the most part, our findings are in line with those of other reviews studying the effectiveness of caregiver involvement in interventions to improve children’s dietary intake and physical activity behaviors. We evaluated a considerably larger body of evidence than the review we sought to update and expand upon (Van Lippevelde 2012), yet we reached a similar conclusion: the evidence is insufficient to determine whether inclusion of a caregiver component impacts intervention effectiveness, perhaps with the exception of SSB consumption.
A number of previous reviews reported only weight‐ or BMI‐related outcomes (e.g. Ling 2017; Luttikhuis 2009; Niemeier 2012; Stice 2006; Yavuz 2015; Young 2007). Three reviews concluded that caregiver involvement in interventions more effectively reduced BMI in children and adolescents (Luttikhuis 2009; Niemeier 2012; Young 2007); two of these reviews focused entirely on weight loss treatment versus prevention (Luttikhuis 2009; Young 2007). One review determined that weight status improved in the short term but not at long‐term follow‐up (Yavuz 2015); this review included only children six years old and younger. In a review of obesity prevention interventions for children and adolescents, Stice 2006 did not find parental involvement to be associated with significantly larger effects. A more recent review examining the effects of lifestyle interventions on BMI among preschool children examined numerous aspects of parental involvement as potential intervention moderators (Ling 2017). The review authors found that prevention interventions that involved parents did not have significantly different effects than prevention interventions that did not involve parents. However, interventions with more sessions for parents had decreased effects, and interventions with behavior change strategies for parents (not defined) yielded greater effects than those without these strategies. Review authors concluded that their findings "do not support any added value of parental involvement" (quote). In the present review, we found that caregiver involvement resulted in a significant increase in BMI at one follow‐up time point, measured by one trial in the combined diet and physical activity comparison. However, analysis of pooled end‐of‐intervention data revealed no significant difference, nor did analyses of pooled data at any other time point.
Other reviews focused on diet or physical activity outcomes. Although some reviews determined that caregiver involvement promotes intervention success (Golley 2011; Kader 2015), others found that there were not enough studies to justify conclusions (Hingle 2010; O'Connor 2009; Van Lippevelde 2012). As mentioned, our review examined a number of diet and physical activity outcomes and found only a few small positive differences at the end of the intervention (children’s SSB intake, fruit intake, and vegetable intake).
Two prior reviews that focused on diet or physical activity outcomes sought to determine whether specific intervention content influenced intervention effectiveness (Golley 2011; Van Lippevelde 2012). These reviews did not calculate pooled effect sizes and reported their results narratively. Golley 2011 applied an older BCT taxonomy to code intervention content and categorize BCTs into five processes of behavior change, from identifying and motivating readiness to change, building self‐efficacy and independence, to helping prevent and manage relapse. Study authors classified a trial as supporting "intervention effectiveness" (quote) when there was a significant change in an objective measure of adiposity or a health risk factor, or when there was at least one significant change in dietary intake or physical activity combined with a significant change in at least one determinant of nutrition or activity behavior. Study authors concluded that intervention effectiveness was enhanced when the BCTs used spanned a behavior change process. Van Lippevelde 2012 extracted information on intervention and study characteristics, including theory and intervention strategies, as well as effect indicators. These review authors suggested that studies including more BCTs in the caregiver component and focusing more on home‐related determinants of diet and physical activity may be more likely to report effectiveness of the intervention. Because we were unable to conduct subgroup analyses by BCT cluster, the present review does not contribute further evidence on whether specific BCTs influence intervention effectiveness.
Authors' conclusions
Implications for practice.
Because most of the 23 studies identified by this review are more than 10 years old and are at high or unclear risk of bias, caregivers and healthcare professionals should be aware that currently available evidence is not sufficient to support claims regarding the benefit of including caregiver involvement in interventions to improve children’s dietary intake and physical activity. This does not mean we found evidence that the interventions are ineffective; rather, we did not find evidence of an improvement in children’s dietary intake or physical activity, other than a small significant increase in fruit intake, a small significant increase in vegetable intake, a small significant decrease in SSB consumption, and a small significant increase in BMI. Factors to consider when interpreting this evidence are that studies included in this systematic review primarily came from high‐income countries within Western cultures, and that content and delivery of the interventions were highly variable. In fact, one of the studies that found caregiver involvement to have an impact on children's fruit intake and vegetable intake took place in Iran, and trial authors emphasized that study findings may not be applicable to Western countries due to cultural differences. Further, even within high‐income countries represented by multiple trials (e.g. USA, Belgium), it is unclear how context and factors related to inequality, such as participants' income, and social markers, such as race, nationality, ethnicity, and gender, contributed to intervention impact. For these reasons, the evidence generated does not guide decision‐making about policy changes that can better support child diet and physical activity behaviors.
Implications for research.
This review highlights the need for well‐designed RCTs to evaluate the effectiveness of caregiver‐involved interventions to improve children’s dietary intake and physical activity. These trials must be prospectively registered, must adhere to CONSORT standards of reporting trials (Schultz 2010), and must specify intervention content using an established framework that relies on internationally recognized terms and definitions (Michie 2015).
Major improvements needed in future research design include selection of similar, valid, and reliable outcome measures; documentation of how behavior change theory is operationalized as specific BCTs; pre‐specification of outcomes of interest; use of sample size calculations to guide recruitment and enrollment; use of effective strategies to minimize attrition and loss to follow‐up; appropriate and complete reporting of results to enable meta‐analysis; documentation and reporting of adverse effects; consideration of secondary outcomes, implementation factors, and cost‐effectiveness; and consistent collection of end‐of‐intervention data, as well as follow‐up data after the end of the intervention. In particular, new research must focus on replication while addressing these key methodological and reporting issues.
In addition to improvements in research design, there is a need to increase the relevance of the evidence for different populations. Outcomes of public health interventions, such as those included in this review, strongly depend on cultural and environmental factors; thus, review findings cannot be readily transferred but require evidence and expert judgment as to their applicability to different contexts (Rychetnik 2002). The need for evidence is especially pressing in low‐ and middle‐income countries facing both a growing burden of non‐communicable diseases (NCDs) and severe resource constraints that keep them from applying some of the strategies pursued in high‐income countries. Even within high‐income countries, socioeconomic disparities and other factors known to be associated with health inequities might, in some cases, contribute to differences in intervention efficacy. Diversifying the settings in which research is carried out may improve the relevance of the evidence, as will consistent reporting of participant characteristics known to be important to health equity using a framework such as PROGRESS‐Plus (Lorenc 2013). When possible, important lessons may be learned by presenting data on intervention effectiveness for different population groups. Such reporting may shed light on intervention efficacy with respect to increasing health equity and may facilitate evidence synthesis in future reviews.
Acknowledgements
The protocol for this review was partially developed during the World Health Organization (WHO)/Cochrane/Cornell University Summer Institute for Systematic Reviews in Nutrition for Global Policy Making, hosted by the Division of Nutritional Sciences, Cornell University, Ithaca, New York, USA, July 27 to August 7, 2015. WHO partially supported this program in 2015. The views and opinions expressed are those of the reviewers and are not necessarily those of WHO.
Work on this review also was partially supported by a Fellowship from Cochrane South Africa to Emily H Morgan, to finance her travel to Stellenbosch University for two weeks in 2018 to facilitate collaboration.
Anel Schoonees is supported in part by the Research, Evidence and Development Initiative (READ‐It). READ‐It (project number 300342‐104) is funded by UK aid from the UK government; however, the views expressed do not necessarily reflect the UK government’s official policies.
This review was produced within Cochrane Developmental, Psychosocial and Learning Problems (CDPLP). We acknowledge the help and support of CDPLP, especially Geraldine Macdonald (Co‐ordinating Editor), Joanne Duffield (Managing Editor), Sarah Davies (Deputy Managing Editor), and Margaret Anderson (Information Specialist), who helped developed and implement the search.
We also would like to recognize Heidi Van Deventer for assistance with data extraction and screening of reference lists of relevant reviews, Bongumusa Gwala for screening of reference lists of relevant reviews, Yuan Chi and Andrew Ying for Chinese‐English data extraction, Alfred Musekiwa for statistical advice, Judy Ward and Tamryn Marchelle Davids for help retrieving screened reports, and Galen Eldridge for copyediting support. Finally, we would like to thank the following reviewers for their comments and contributions: Professor Mary Barker, MRC (Medical Research Council) Lifecourse Epidemiology Unit, University of Southampton, UK; Professor Michael P Kelly, Senior Visiting Fellow, Institute of Public Health, University of Cambridge, UK; and Mbaka Fon Nji, Cameroon.
Appendices
Appendix 1. Search strategies 2017
1 Cochrane Central Register of Controlled Trials (CENTRAL), in the Cochrane Library
Searched May 4, 2017 (6162 records) and updated January 14, 2019 (1984 records)
#1 Child:MH #2 Adolescent:MH #3 ((child* or toddler* or preschool* or pre‐school* or schoolchild* or school child* or schoolage* or school age* or pre‐teen or adolescent* or teen* or young adult* or youth* or young person* or young people) ):TI,AB,KY #4 #1 OR #2 OR #3 #5 MESH DESCRIPTOR parents EXPLODE ALL TREES #6 MESH DESCRIPTOR family EXPLODE ALL TREES #7 MESH DESCRIPTOR Parent‐Child Relations #8 MESH DESCRIPTOR Caregivers #9 MESH DESCRIPTOR Grandparents #10 MESH DESCRIPTOR Parenting #11 MESH DESCRIPTOR Parent‐Child Relations EXPLODE TREES 1 #12 (parent* not parenteral ):TI,AB,KY #13 ((mother* or father* or caregiver* or carer* or care‐giver* or guardian* or grandparent* or grandfather* or grandmother* or family or familial or families or home* or household or house‐hold*) ):TI,AB,KY #14 #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 #15 #4 AND #14 #16 MESH DESCRIPTOR diet EXPLODE ALL TREES #17 MESH DESCRIPTOR Nutrition Therapy #18 MESH DESCRIPTOR Food Preferences #19 ((health* adj2 (diet* or eat* or food* or meal*))):TI,AB,KY #20 ((diet* or eat* or food* or meal*) adj2 health*) :TI,AB,KY #21 ((diet* adj2 (modif* or therap* or intervention* or strateg*))):TI,AB,KY #22 ((modif* or therap* or intervention* or strateg*) adj2 diet*):TI,AB,KY #23 (((eat* or food* or diet*) adj2 habit*)):TI,AB,KY #24 (habit* adj2 (eat* or food* or diet*)):TI,AB,KY #25 MESH DESCRIPTOR Exercise Movement Techniques EXPLODE ALL TREES #26 MESH DESCRIPTOR Exercise Therapy EXPLODE ALL TREES #27 MESH DESCRIPTOR Exercise EXPLODE ALL TREES #28 MESH DESCRIPTOR Physical Education and Training #29 MESH DESCRIPTOR Physical Fitness #30 MESH DESCRIPTOR Sports EXPLODE TREES 1 #31 ((aquatic* or aerobic* or cycle or cycing or exercise* or strength* or fitness* or running or sport* or swim* or walking )):TI,AB,KY #32 MESH DESCRIPTOR Sedentary Lifestyle #33 ((inactiv* or in‐activ* or sedentary or screen time or screen‐time or screentime)):TI,AB,KY #34 MESH DESCRIPTOR Health Promotion #35 MESH DESCRIPTOR Health Education #36 ( (health* adj2 (educat* or lifestyle* or live* or living or promot*))):TI,AB,KY #37 ((educat* or lifestyle* or live* or living or promot*) adj2 health*):TI,AB,KY #38 #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 #39 #15 AND #38
2 MEDLINE Ovid
Searched May 4, 2017 (6271 records) and updated January 15, 2019 (1203 records)
This strategy uses the sensitivity‐ and precision‐maximizing version of the Cochrane Highly Sensitive Search Strategy for identifying randomized trials (Lefebvre 2008).
1 exp child/ 2 adolescent/ 3 (child$ or toddler$ or preschool$ or pre‐school$ or schoolchild$ or schoolage$ or pre‐teen or adolescen$ or teen$ or young adult$ or youth$ or young person$ or young people).tw. 4 or/1‐3 5 exp Parents/ 6 ((parent$ or mother$ or father$) not parenteral$).tw. 7 Caregivers/ 8 (caregiver$ or care‐giver$ or carer$ or guardian$).tw. 9 Grandparents/ 10 (grandparent$ or grandfather$ or grandmother$).tw. 11 family/ 12 (family or familial or families).tw. 13 (home$ or household$ or house‐hold$).tw. 14 Family Relations/ 15 parent‐child relations/ 16 father‐child relations/ 17 mother‐child relations/ 18 Parenting/ 19 or/5‐18 20 4 and 19 21 exp diet/ 22 exp food habits/ 23 food preferences/ 24 exp Nutrition Therapy/ 25 (health$ adj2 (diet$ or eat$ or food$ or meal$)).tw. 26 (diet$ adj5 (modif$ or therap$ or intervention$ or strateg$)).tw. 27 ((eating or food or diet$) adj2 habit$).tw. 28 exp exercise/ 29 physical$ activ$.tw. 30 exp Exercise Movement Techniques/ 31 exp Exercise Therapy/ 32 exp "Physical Education and Training"/ 33 Physical Fitness/ 34 exp Sports/ 35 aerobic$.tw. 36 (cycle or cycling).tw. 37 (exercise$ or strength$ or fitness).tw. 38 sport$.tw. 39 (walking or running).tw. 40 (aquatic$ or swim$).tw. 41 Sedentary Lifestyle/ 42 (inactiv$ or in‐activ$ or sedentary or screen time or screen‐time or screentime).tw. 43 Health Education/ 44 exp Health Promotion/ 45 (health$ adj2 (educat$ or lifestyle$ or live$ or living or promot$)).tw. 46 or/21‐45 47 20 and 46 48 randomized controlled trial.pt. 49 controlled clinical trial.pt. 50 randomi#ed.ab. 51 placebo.ab. 52 clinical trials as topic.sh. 53 randomly.ab. 54 trial.ti. 55 or/48‐54 56 exp animals/ not humans.sh. 57 55 not 56 58 47 and 57
3 MEDLINE In‐Process & Other Non‐Indexed Citations Ovid
Searched May 4, 2017 (2490 records) and updated January 15, 2019 (1859 records)
1 (child$ or toddler$ or preschool$ or pre‐school$ or schoolchild$ or schoolage$ or pre‐teen or adolescen$ or teen$ or young adult$ or youth$ or young person$ or young people).tw,kf. 2 ((parent$ or mother$ or father$) not parenteral$).tw,kf. 3 (caregiver$ or care‐giver$ or carer$ or guardian$).tw,kf. 4 (grandparent$ or grandfather$ or grandmother$).tw,kf. 5 (family or familial or families).tw,kf. 6 (home$ or household$ or house‐hold$).tw,kf. 7 or/2‐6 8 1 and 7 9 (health$ adj2 (diet$ or eat$ or food$ or meal$)).tw,kf. 10 (diet$ adj5 (modif$ or therap$ or intervention$ or strateg$)).tw,kf. 11 ((eating or food or diet$) adj2 habit$).tw,kf. 12 (nutrition adj2 therapy).tw,kf. 13 (physical$ activ$).tw,kf. 15 (cycle or cycling).tw,kf. 16 (exercise$ or strength$ or fitness).tw,kf. 17 sport$.tw,kf. 18 (walking or running).tw,kf. 19 (aquatic$ or swim$).tw,kf. 20 (inactiv$ or in‐activ$ or sedentary or screen‐time or screen time or screentime).tw,kf. 21 (health$ adj2 (educat$ or lifestyle$ or live$ or living or promot$)).tw,kf. 22 or/9‐21 23 8 and 22 24 (random$ or control$ or group$ or cluster$ or placebo$ or trial$ or assign$ or prospectiv$ or meta‐analysis or systematic review or longitudinal$).tw,kf. 25 23 and 24
4 MEDLINE Epub Ahead of Print
Searched May 4, 2017 (607 records) and updated January 15, 2019 (608 records)
1 (child$ or toddler$ or preschool$ or pre‐school$ or schoolchild$ or schoolage$ or pre‐teen or adolescen$ or teen$ or young adult$ or youth$ or young person$ or young people).tw,kf. 2 ((parent$ or mother$ or father$) not parenteral$).tw,kf. 3 (caregiver$ or care‐giver$ or carer$ or guardian$).tw,kf. 4 (grandparent$ or grandfather$ or grandmother$).tw,kf. 5 (family or familial or families).tw,kf. 6 (home$ or household$ or house‐hold$).tw,kf. 7 or/2‐6 8 1 and 7 9 (health$ adj2 (diet$ or eat$ or food$ or meal$)).tw,kf. 10 (diet$ adj5 (modif$ or therap$ or intervention$ or strateg$)).tw,kf. 11 ((eating or food or diet$) adj2 habit$).tw,kf. 12 (nutrition adj2 therapy).tw,kf. 13 (physical$ activ$).tw,kf. 15 (cycle or cycling).tw,kf. 16 (exercise$ or strength$ or fitness).tw,kf. 17 sport$.tw,kf. 18 (walking or running).tw,kf. 19 (aquatic$ or swim$).tw,kf. 20 (inactiv$ or in‐activ$ or sedentary or screen‐time or screen time or screentime).tw,kf. 21 (health$ adj2 (educat$ or lifestyle$ or live$ or living or promot$)).tw,kf. 22 or/9‐21 23 8 and 22 24 (random$ or control$ or group$ or cluster$ or placebo$ or trial$ or assign$ or prospectiv$ or meta‐analysis or systematic review or longitudinal$).tw,kf. 25 23 and 24
5 Embase Ovid
Searched May 4, 2017 (5410 records) and updated January 15, 2019 (1174 records)
1 parent/ 2 father/ 3 mother/ 4 grandparent/ 5 caregiver/ 6 family/ 8 ((parent$ or mother$ or father$) not parenteral$).tw. 9 (caregiver$ or care‐giver$ or carer$ or guardian$).tw. 10 (grandparent$ or grandfather$ or grandmother$).tw. 11 (family or familial or families).tw. 12 or/1‐11 13 exp child/ 14 adolescent/ 15 (child$ or toddler$ or preschool$ or pre‐school$ or schoolchild$ or schoolage$ or school‐age$ or pre‐teen or adolescen$ or teen$ or young adult$ or youth$ or young person$ or young people).tw. 16 or/13‐15 17 12 and 16 18 exp diet/ 19 exp feeding behavior/ 20 exp diet therapy/ 21 (health$ adj2 (diet$ or eat$ or food$ or meal$)).tw. 22 (diet$ adj3 (modif$ or therap$ or intervention$ or strateg$)).tw. 23 ((eating or food or diet$) adj2 habit$).tw. 24 exp exercise/ 25 exp kinesiotherapy/ 26 physical education/ 27 fitness/ 28 exp sport/ 29 aerobic$.tw. 30 (cycle or cycling).tw. 31 (exercise$ or strength$ or fitness).tw. 32 sport$.tw. 33 (walking or running).tw. 34 (aquatic$ or swim$).tw. 35 sedentary lifestyle/ 36 exp physical activity/ 37 physical$ activ$.tw. 38 (inactiv$ or in‐activ$ or sedentary or screen time or screen‐time or screentime).tw. 39 health education/ 40 exp Health Promotion/ 41 (health$ adj2 (educat$ or lifestyle$ or live$ or living or promot$)).tw. 42 or/18‐41 43 17 and 42 44 Randomized controlled trial/ 45 controlled clinical trial/ 46 Placebo/ 47 placebo.tw. 48 crossover procedure/ 49 (random$ adj2 (allocat$ or assign$ or cluster$ or quasi$)).tw. 50 random$ controlled trial.tw. 51 RCT.tw. 52 (crossover or cross‐over).tw. 53 or/44‐52 54 43 and 53
6 ERIC EBSCOhost
Searched May 4, 2017 (5311 records) and updated January 16, 2019 (269 records)
S1 DE "Nutrition" OR DE "Nutrition Instruction" S2 DE "Eating Habits" S3 DE "Breakfast Programs" or DE "Lunch Programs" S4 TI (health* N2 (diet* or eat* or food* or meal*)) OR AB (health* N2 (diet* or eat* or food* or meal*)) S5 TI (diet* N5 (modif* or therap* or intervention* or strateg*)) OR AB(diet* N5 (modif* or therap* or intervention* or strateg*)) S6 TI ((eating or food or diet*) N2 habit*) OR AB ((eating or food or diet*) N2 habit*) S7 (DE "Physical Activities" OR DE "Athletics" OR DE "Dance" OR DE "Exercise") S8 DE "Aquatic Sports" OR DE "Racquet Sports" OR DE "Team Sports" S9 DE "Physical Education" OR DE "Adapted Physical Education" OR DE "Movement Education" OR DE "Health Related Fitness" OR DE "Physical Recreation Programs" or DE "Playground Activities" OR "Recreational Activities") S10 TI(physical* N1 activ*) OR AB(physical* N1 activ*) S11 TI(aerobic*) OR AB(aerobic*) S12 TI(cycle or cycling) or AB(cycle or cycling) S13 TI (exercise* or strength* or fitness) OR AB(exercise* or strength* or fitness) S14 TI("screen time" or screen‐time or screentime) OR AB ("screen time" or screen‐time or screentime) S15 TI(sport*) OR AB(sport*) S16 TI(walking or running) OR AB (walking or running) S17 TI (aquatic* or swim*) OR AB(aquatic* or swim*) S18 TI(inactiv* or in‐activ* ) OR AB(inactiv* or in‐activ*) S19 DE "Health Education" OR DE "Health Promotion" S20 TI ((health* N2 (educat* or lifestyle* or live* or living or promot*))) OR AB ((health* N2 (educat* or lifestyle* or live* or living or promot*))) S21 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 S22 DE "Early Adolescents" OR DE "Late Adolescents" OR DE "Children" OR DE "Preadolescents" OR DE "Young Children" OR DE "Adolescents" OR DE "Youth" S23 TI (child* or toddler* or preschool* or pre‐school* or schoolchild* or schoolage* or school‐age* or pre‐teen or adolescen* or teen* or young adult* or youth* or young person* or young people) OR AB (child* or toddler* or preschool* or pre‐school* or schoolchild* or schoolage* or school‐age* or pre‐teen or adolescen* or teen* or young adult* or youth* or young person* or young people) S24 S22 OR S23 S25 DE "Parents" OR DE "Parent Education" OR DE "Parent Influence" OR DE "Parent Participation" OR DE "Parent Responsibility" OR DE "Parent Role" OR DE "Mothers" OR DE "Fathers" S26 DE "Caregiver Role" OR DE "Caregivers" OR DE "Child Caregivers" S27 DE "Family Influence" OR DE "Family Involvement" OR DE "Family Role" S28 TI(parent* or mother* or father*) or AB(parent* or mother* or father*) S29 TI(caregiver* or care‐giver* or carer* or guardian*) OR AB(caregiver* or care‐giver* or carer* or guardian*) S30 DE "Grandparents" OR DE "Grandparents Raising Grandchildren" S31 TI(grandparent* or grandfather* or grandmother*) OR AB(grandparent* or grandfather* or grandmother*) S32 TI(family or familial or families) OR AB(family or familial or families) S33 TI (home* or household* or house‐hold*) OR AB(home* or household* or house‐hold*) S34 S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 S35 S24 AND S34 S36 S21 AND S35 S37 DE "Evaluation Research" OR DE "Control Groups" OR DE "Longitudinal Studies" OR DE "Followup Studies" OR DE "Program Effectiveness" OR DE "Program Evaluation" S38 TI ((random* N3 (allocat* or assign* or quasi* OR cluster*)) or trial* or control group*) OR AB ((random* N3 (allocat* or assign*or quasi* OR cluster*)) or trial* or control group*) S39 S37 OR S38 S40 S36 AND S39
7 CINAHL Plus EBSCOhost
Searched May 5, 2017 (3055 records) and updated January 16, 2019 (752 records)
S1 (MH "Diet+") S2 (MH "Food Habits") S3 (MH "Food Preferences") S4 (MH "Diet Therapy") S5 TI (health* N2 (diet* or eat* or food* or meal*)) OR AB (health* N2 (diet* or eat* or food* or meal*)) S6 TI (diet* N5 (modif* or therap* or intervention* or strateg*)) OR AB(diet* N5 (modif* or therap* or intervention* or strateg*)) S7 TI ((eating or food or diet*) N2 habit*) OR AB ((eating or food or diet*) N2 habit*) S8 (MH "Exercise+") OR (MH "Dancing") OR (MH "Walking") OR (MH "Physical Fitness+") OR (MH "Physical Activity") OR (MH "Sports+") S9 TI(physical* N1 activ*) OR AB(physical* N1 activ*) S10 TI(aerobic*) OR AB(aerobic*) S11 TI(cycle or cycling) or AB(cycle or cycling) S12 TI (exercise* or strength* or fitness) OR AB(exercise* or strength* or fitness) S13 TI(sport*) OR AB(sport*) S14 TI(walking or running) OR AB (walking or running) S15 TI (aquatic* or swim*) OR AB(aquatic* or swim*) S16 (MH "Life Style, Sedentary") S17 TI(inactiv* or in‐activ* or sedentary OR AB(inactiv* or in‐activ* or sedentary) S18 TI("screen time" or screen‐time or screentime) OR AB ("screen time" or screen‐time or screentime) S19 (MH "Health Education") S20 (MH "Health Promotion") S21 TI ((health* N2 (educat* or lifestyle* or live* or living or promot*))) OR AB ((health* N2 (educat* or lifestyle* or live* or living or promot*))) S22 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 S23 (MH "Infant") or(MH "Child") OR (MH "Adolescence") S24 TI (child* or toddler* or preschool* or pre‐school* or schoolchild* or schoolage* or school‐age* or pre‐teen or adolescen* or teen* or young adult* or youth* or young person* or young people) OR AB (child* or toddler* or preschool* or pre‐school* or schoolchild* or schoolage* or school‐age* or pre‐teen or adolescen* or teen* or young adult* or youth* or young person* or young people) S25 S23 OR S24 S26 (MH "Parents") OR (MH "Fathers") OR (MH "Mothers") OR (MH "Family") OR (MH "Grandparents") S27 (MH "Parenting") or (MH "Parent‐Child Relations") S28 (MH "Family") OR (MH "Family Relations") S29 (MH "Grandparents") S30 (TI(parent* or mother* or father*) or AB(parent* or mother* or father*) ) NOT parenteral* S31 (MH "Caregivers") S32 TI(caregiver* or care‐giver* or carer* or guardian*) OR AB(caregiver* or care‐giver* or carer* or guardian*) S33 S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 S34 S25 AND S33 S35 S22 AND S34 S36 (MH "Clinical Trials+") S37 MH random assignment S38 (MH "Crossover Design") S39 TI(crossover OR cross‐over) OR AB(crossover OR cross‐over) S40 PT randomized controlled trial S41 PT Clinical trial S42 (clinical trial*) or (control* N2 trial*) S43 (MH "Program Evaluation") S44 TI ((random* N3 (allocat* or assign* or quasi* OR cluster*)) or trial* or control group*) OR AB ((random* N3 (allocat* or assign* or quasi* OR cluster*)) or trial* or control group*) S45 S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 S46 S35 AND S45
8 LILACS (http://lilacs.bvsalud.org/en/)
Searched May 3, 2017 (90 records) and updated January 18, 2019 (20 records)
(child* OR toddler* OR adolescen* OR teen* OR youth*) AND (caregiver* OR carer* OR parent* OR guardian* OR grandparent* OR mother* OR father*) AND (diet* OR nutrition* OR intake* OR exercise* OR “physical activit*” OR sport* OR sedentary OR inactive* OR screen‐time OR “screen time” OR screentime) AND (instance:"regional") AND ( db:("LILACS") AND type_of_study:("clinical_trials" OR "systematic_reviews"))
9 Cochrane Database of Systematic Reviews, part of the Cochrane Library
Searched May 8, 2017 (85 records) and updated January 14, 2019 (21 records)
#1 (child* or toddler* or preschool* or pre next school* or schoolchild* or school next child* or schoolage* or school next age* or pre next teen or adolescent* or teen* or young next adult* or youth* or young next person* or young next people):ti #2 (parent* not parenteral):ti,ab #3 (mother* or father* or caregiver* or carer* or care next giver* or guardian* or grandparent* or grandfather* or grandmother* or family or familial or families or home* or household or house next hold*):ti,ab #4 {or #2‐#3} #5 #1 and #4 #6 (diet* or food next habit* or food next preference* or nutrition next therap*) .ti,ab #7 (health* near/2 (diet* or eat* or food* or meal*)):ti,ab #8 (diet* near/2 (modif* or therap* or intervention* or strateg*)):ti,ab #9 ((eat* or food* or diet*) near/2 habit*):ti,ab #10 (exercise* or strength* or (physical* next activ*) or fitness or sport* or aerobic* or cycle or cycling or running or jogging or walking or aquatic* or swim* or inactiv* or in next activ* or sedentary or screen‐time or "screen time" or screentime or "physical fitness" or "physical education" or "physical training"):ti,ab #11 (health* near/2 (educat* or promot* or lifestyle* or live* or living or train*)):ti,ab #12 {or #6‐#11} #13 #5 and #12 in Cochrane Reviews (Reviews and Protocols)
10 Database of Abstracts of Reviews of Effects, part of the Cochrane Library
The final issue of DARE was searched on May 8, 2017 (9 records). DARE ceased to be updated after this.
#1 (child* or toddler* or preschool* or pre next school* or schoolchild* or school next child* or schoolage* or school next age* or pre next teen or adolescent* or teen* or young next adult* or youth* or young next person* or young next people):ti #2 (parent* not parenteral):ti,ab #3 (mother* or father* or caregiver* or carer* or care next giver* or guardian* or grandparent* or grandfather* or grandmother* or family or familial or families or home* or household or house next hold*):ti,ab #4 {or #2‐#3} #5 #1 and #4 #6 (diet* or food next habit* or food next preference* or nutrition next therap*) .ti,ab #7 (health* near/2 (diet* or eat* or food* or meal*)):ti,ab #8 (diet* near/2 (modif* or therap* or intervention* or strateg*)):ti,ab #9 ((eat* or food* or diet*) near/2 habit*):ti,ab #10 (exercise* or strength* or (physical* next activ*) or fitness or sport* or aerobic* or cycle or cycling or running or jogging or walking or aquatic* or swim* or inactiv* or in nextactiv* or sedentary or screen‐time or "screen time" or screentime or "physical fitness" or "physical education" or "physical training"):ti,ab #11 (health* near/2 (educat* or promot* or lifestyle* or live* or living or train*)):ti,ab #12 {or #6‐#11} #13 #5 and #12 in Other Reviews
11 Epistimonikos (http://www.epistemonikos.org/)
Searched May 3, 2017 (54 records with 'Primary Study: RCT' filter and 84 with 'Systematic Review' filter) and updated January 16, 2019 (0 records with 'Primary Study: RCT' filter and 48 with 'Systematic Review' filter)
1 (title:((child$ OR toddler$ OR preschool$ OR pre‐school$ OR schoolchild$ OR schoolage$ OR pre‐teen$ OR adolescen$ OR teen$ OR "young adult$" OR youth$ OR "young person$" OR "young people")) OR abstract:((child$ OR toddler$ OR preschool$ OR pre‐school$ OR schoolchild$ OR schoolage$ OR pre‐teen$ OR adolescen$ OR teen$ OR "young adult$" OR youth$ OR "young person$" OR "young people"))) 2 (title:((parent$ OR mother$ OR father$ OR caregiver$ OR care‐giver$ OR carer$ OR guardian$ OR grandparent$ OR grandfather$ OR grandmother$ OR family OR familial OR families OR home$ OR household$ OR house‐hold$)) OR abstract:((parent$ OR mother$ OR father$ OR caregiver$ OR care‐giver$ OR carer$ OR guardian$ OR grandparent$ OR grandfather$ OR grandmother$ OR family OR familial OR families OR home$ OR household$ OR house‐hold$))) 3 (title:((diet$ OR nutrition$ OR intake$ OR exercise$ OR "physical activit$" OR sport$ OR sedentary OR inactiv$ OR screen‐time OR "screen time" OR screentime)) OR abstract:((diet$ OR nutrition$ OR intake$ OR exercise$ OR "physical activit$" OR sport$ OR sedentary OR inactiv$ OR screen‐time OR "screen time" OR screentime))) 4 1 AND 2 AND 3
12 Conference Proceedings Citation Index—Science Web of Science
Searched May 3, 2017 (327 records) and updated January 16, 2019 (29 records)
1 TS=(child* OR toddler* OR preschool* OR pre‐school* OR schoolchild* OR schoolage* OR pre‐teen* OR adolescen* OR teen* OR “young adult*” OR youth* OR “young person*” OR “young people”) 2 TS=(parent* OR mother* OR father* OR caregiver* OR care‐giver* or carer* OR guardian* OR grandparent* OR grandfather* OR grandmother* OR family OR familial OR families OR home$ OR household* OR house‐hold*) 3 TS=(diet* OR nutrition* OR intake* OR exercise OR “physical activit*” OR sport* OR sedentary OR inactiv* OR screen‐time OR “screen time” OR screentime) 4 TS=(random* OR trial*) 5 1 AND 2 AND 3 AND 4
13 Conference Proceedings Citation Index—Social Science & Humanities Web of Science
Searched May 3, 2017 (40 records) and updated January 16, 2019 (9 records)
1 TS=(child* OR toddler* OR preschool* OR pre‐school* OR schoolchild* OR schoolage* OR pre‐teen* OR adolescen* OR teen* OR “young adult*” OR youth* OR “young person*” OR “young people”) 2 TS=(parent* OR mother* OR father* OR caregiver* OR care‐giver* or carer* OR guardian* OR grandparent* OR grandfather* OR grandmother* OR family OR familial OR families OR home$ OR household* OR house‐hold*) 3 TS=(diet* OR nutrition* OR intake* OR exercise OR “physical activit*” OR sport* OR sedentary OR inactiv* OR screen‐time OR “screen time” OR screentime) 4 TS=(random* OR trial*) 5 1 AND 2 AND 3 AND 4
14 ProQuest Dissertations & Theses Global ProQuest
Searched May 3, 2017 (294 records) and updated January 16, 2019 (36 records)
(TI(child* OR toddler* OR preschool* OR pre‐school* OR schoolchild* OR schoolage* OR pre‐teen* OR adolescen* OR teen* OR "young adult*" OR youth* OR "young person*" OR "young people*") AND TI(caregiver* OR carer* OR parent* OR guardian* OR grandparent* OR mother* OR father*) AND TI(diet* OR nutrition* OR intake* OR exercise* OR "physical activ*" OR sport* OR sedentary OR inactiv* OR screen‐time OR "screen time" OR screentime))
15 Trials Register of Promoting Health Interventions (https://eppi.ioe.ac.uk/webdatabases4/Intro.aspx?ID=12)
Searched May 3, 2017 (203 records) and updated January 16, 2019 (1 record)
1 What type of study does this report describe?: RCT 2 Focus of the report: health promotion (used where no specific term is suitable) OR healthy eating OR obesity OR physical activity 3 Focus of the report: parenting 4 1 AND 2 AND 3
16 ClinicalTrials.gov (https://clinicaltrials.gov/)
Searched May 5, 2017 (527 records) and updated January 14, 2019 (421 records)
Interventional Studies | (diet OR nutrition OR intake OR exercise OR physical activity OR physically active OR sport OR sedentary OR inactive OR inactivity OR screentime OR screen time OR screen‐time) | (caregiver OR carer OR parent OR family OR guardian OR grandparent OR mother OR father)
17 World Health Organization International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/default.aspx)
Searched May 10, 2017 (733 records) and updated January 14, 2019 (211 records)
Title: caregiver OR carer OR parent OR family OR guardian OR grandparent OR mother OR father
Intervention: diet OR nutrition OR intake OR exercise OR physical activity OR physically active OR sport OR sedentary OR inactive OR inactivity OR screen‐time OR screen time OR screentime
Recruitment status: all
Data and analyses
Comparison 1. Dietary behavior change interventions with a caregiver component versus interventions without a caregiver component.
Comparison 2. Physical activity interventions with a caregiver component versus interventions without a caregiver component.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Children's physical activity levels—total physical activity: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Children's physical activity levels—moderate to vigorous physical activity: end of intervention (change values) | 2 | 80 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.41, 0.49] |
| 3 Children's physical activity levels—moderate to vigorous physical activity: end of intervention (end values) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Children's physical activity levels—moderate to vigorous physical activity: all intervention time points | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 < 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 ≥ 3 to ≤ 6 months | 3 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Children's physical activity levels—moderate to vigorous physical activity: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Children's physical activity levels—moderate physical activity: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Children's physical activity levels—vigorous physical activity: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Children's physical activity levels—light physical activity: end of intervention | 2 | 80 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.97, 0.24] |
| 9 Children's physical activity levels—light physical activity: all intervention time points | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 < 3 months | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.81, 0.74] |
| 9.2 ≥ 3 to ≤ 6 months | 2 | 80 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.97, 0.24] |
| 10 Children's physical activity levels—steps: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Children's physical activity levels—total physical activity score: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12 Children's sedentary behavior—sedentary behavior: end of intervention (change values) | 2 | 80 | Std. Mean Difference (IV, Random, 95% CI) | 0.26 [‐0.47, 0.98] |
| 13 Children's sedentary behavior—sedentary behavior: end of intervention (end values) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14 Children's sedentary behavior—sedentary behavior: all intervention time points | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 < 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 ≥ 3 to ≤ 6 months | 3 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Children's sedentary behavior—sedentary behavior: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16 Children's body mass index or weight‐for‐height parameter—body mass index: end of intervention | 2 | 441 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.21, 0.35] |
| 17 Children's body mass index or weight‐for‐height parameter—body mass index: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18 Caregivers' physical activity levels—total physical activity score: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19 Caregiver's physical activity levels—moderate to vigorous physical activity: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 20 Caregiver's physical activity levels—moderate to vigorous physical activity: all intervention time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 20.1 < 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 ≥ 3 to ≤ 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Caregiver's physical activity levels—light physical activity: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 22 Caregiver's physical activity levels—light physical activity: all intervention time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 22.1 < 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.2 ≥ 3 to ≤ 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Combined dietary and physical activity interventions with a caregiver component versus interventions without a caregiver component.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Children's dietary intake—total energy intake: end of intervention | 3 | 440 | Mean Difference (IV, Random, 95% CI) | 14.45 [‐117.20, 146.10] |
| 2 Children's dietary intake—total energy intake: all intervention time points | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 < 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 > 1 year to ≤ 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Children's dietary intake—total energy intake: follow‐up time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Children's dietary intake—percentage energy from fat: end of intervention | 4 | 563 | Mean Difference (IV, Random, 95% CI) | 1.17 [‐0.65, 3.00] |
| 5 Children's dietary intake—percentage energy from fat: all intervention time points | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 < 3 months | 1 | 70 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐3.87, 4.21] |
| 5.2 > 6 months to ≤ 1 year | 2 | 405 | Mean Difference (IV, Random, 95% CI) | 0.58 [‐2.14, 3.30] |
| 5.3 > 1 year to ≤ 2 years | 1 | 283 | Mean Difference (IV, Random, 95% CI) | 3.12 [‐0.79, 7.03] |
| 5.4 > 2 years to ≤ 3 years | 1 | 151 | Mean Difference (IV, Random, 95% CI) | 0.45 [‐2.49, 3.39] |
| 6 Children's dietary intake—percentage energy from fat: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Children's dietary intake—percentage energy from saturated fat: end of intervention (includes all intervention time points) | 2 | 216 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.67, 0.80] |
| 7.1 > 6 months to ≤ 1 year | 1 | 59 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.75, 0.95] |
| 7.2 > 2 years to ≤ 3 years | 1 | 157 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐1.46, 1.38] |
| 8 Children's dietary intake—percentage energy from saturated fat: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9 Children's dietary intake—percentage energy from carbohydrates: end of intervention (includes all intervention time points) | 2 | 266 | Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐3.49, 1.74] |
| 9.1 < 3 months | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐5.73, 3.89] |
| 9.2 > 2 years to ≤ 3 years | 1 | 196 | Mean Difference (IV, Random, 95% CI) | ‐0.86 [‐3.98, 2.26] |
| 10 Children's dietary intake—percentage energy from carbohydrates: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Children's dietary intake—percentage energy from protein: end of intervention (includes all intervention time points) | 2 | 241 | Mean Difference (IV, Random, 95% CI) | 0.45 [‐0.80, 1.69] |
| 11.1 < 3 months | 1 | 70 | Mean Difference (IV, Random, 95% CI) | 0.77 [‐1.66, 3.20] |
| 11.2 > 2 years to ≤ 3 years | 1 | 171 | Mean Difference (IV, Random, 95% CI) | 0.33 [‐1.12, 1.78] |
| 12 Children's dietary intake—percentage energy from protein: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13 Children's dietary intake—sodium intake: end of intervention (includes all intervention time points) | 2 | 315 | Mean Difference (IV, Random, 95% CI) | 35.94 [‐322.60, 394.47] |
| 13.1 < 3 months | 1 | 70 | Mean Difference (IV, Random, 95% CI) | 70.27 [‐743.71, 884.25] |
| 13.2 > 2 to ≤ 3 years | 1 | 245 | Mean Difference (IV, Random, 95% CI) | 27.67 [‐371.70, 427.04] |
| 14 Children's dietary intake—sodium intake: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15 Children's dietary intake—fruit and vegetable intake: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16 Children's dietary intake—fruit and vegetable intake: all intervention time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 > 1 year to ≤ 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Children's dietary intake—fruit intake: end of intervention | 2 | 417 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [0.03, 0.43] |
| 18 Children's dietary intake—fruit intake: all intervention time points | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 18.1 > 6 months to ≤ 1 year | 2 | 483 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [0.01, 0.38] |
| 18.2 > 1 year to ≤ 2 years | 1 | 358 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.11, 0.31] |
| 19 Children's dietary intake—vegetable intake: end of intervention (includes all intervention time points) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 20 Children's dietary intake—sugar‐sweetened beverage intake: end of intervention | 3 | 651 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.44, ‐0.12] |
| 21 Children's dietary intake—sugar‐sweetened beverage intake: all intervention time points | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 21.1 > 6 months to ≤ 1 year | 3 | 799 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.39, ‐0.11] |
| 21.2 > 1 year to ≤ 2 years | 2 | 630 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.45, 0.03] |
| 21.3 > 2 years to ≤ 3 years | 1 | 134 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.58, 0.12] |
| 22 Children's dietary intake—water intake: end of intervention | 3 | 600 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.24, 0.09] |
| 23 Children's dietary intake—water intake: all intervention time points | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 23.1 > 6 months to ≤ 1 year | 2 | 610 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.10, 0.22] |
| 23.2 > 1 year to ≤ 2 years | 2 | 518 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.15, 0.20] |
| 23.3 > 2 years to ≤ 3 years | 2 | 254 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.43, 0.07] |
| 24 Children's physical activity levels—total physical activity: end of intervention | 2 | 573 | Mean Difference (IV, Random, 95% CI) | 1.81 [‐15.18, 18.80] |
| 25 Children's physical activity levels—total physical activity: all intervention time points | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25.1 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 > 1 year to ≤ 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.3 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Children's physical activity levels—total physical activity: follow‐up time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 > 1 year to ≤ 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.3 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 Children's physical activity levels—moderate to vigorous physical activity: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 28 Children's physical activity levels—moderate to vigorous physical activity: all intervention time points | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 28.1 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28.2 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29 Children's physical activity levels—moderate to vigorous physical activity: follow‐up time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 29.1 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29.2 > 1 year to ≤ 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29.3 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 30 Children's physical activity levels—light physical activity: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 31 Children's physical activity levels—light physical activity: all intervention time points | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 31.1 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.2 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32 Children's physical activity levels—light physical activity: follow‐up time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 32.1 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32.2 > 1 year to ≤ 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32.3 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 33 Children's physical activity levels—weight‐bearing physical activity: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 34 Children's physical activity levels—steps: end of intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 35 Children's physical activity levels—steps: all intervention time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 35.1 1 week | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 35.2 2 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 35.3 3 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 35.4 4 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 36 Children's sedentary behavior—sedentary behavior: end of intervention (includes all intervention time points) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 37 Children's sedentary behavior—sedentary behavior: follow‐up time points | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 37.1 > 6 months to ≤ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 37.2 > 1 year to ≤ 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 37.3 > 2 years to ≤ 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 38 Prevalence of overweight and obesity among children—prevalence: end of intervention | 3 | 1866 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.89, 1.17] |
| 39 Prevalence of overweight and obesity among children—prevalence: all intervention time points | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 39.1 > 6 months to ≤ 1 year | 2 | 641 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.80, 1.30] |
| 39.2 > 1 year to ≤ 2 years | 2 | 590 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.76, 1.27] |
| 39.3 > 2 years to ≤ 3 years | 2 | 1448 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.88, 1.18] |
| 40 Prevalence of overweight and obesity among children—prevalence: follow‐up time point | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 41 Children's body mass index or weight‐for‐height parameter—body mass index: end of intervention | 4 | 1861 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.04, 0.15] |
| 42 Children's body mass index or weight‐for‐height parameter—body mass index: all intervention time points | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 42.1 < 3 months | 1 | 72 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.26, 0.66] |
| 42.2 > 6 months to ≤ 1 year | 2 | 612 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.17, 0.15] |
| 42.3 > 1 year to ≤ 2 years | 2 | 517 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.21, 0.14] |
| 42.4 > 2 years to ≤ 3 years | 2 | 1444 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.03, 0.18] |
| 43 Children's body mass index or weight‐for‐height parameter—body mass index: follow‐up time point | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adamo 2017a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to evaluate the efficacy of an intervention program delivered in licensed childcare settings, with or without the addition of parent facilitated home physical activity promotion, to increase preschoolers’ overall physical activity levels and decrease sedentary time and adiposity" (quote) Study period: January 2013 to March 2014 (or later) Total number of arms: 3 Description of intervention arms: 1. Childcare intervention with parental involvement (child + caregiver); 2. Childcare intervention alone (child only); 3. No‐intervention comparison group (not eligible) Number of clusters per arm: 6 Average cluster size: 11.94 children Sample size justification and outcome used: to detect a 15‐minute difference in MVPA between the child‐only arm and the "wait‐list control" arm, with 80% power and a 5% probability of a type 1 error, 6 centers per arm with 15 preschoolers per arm were required. Estimate of intracluster correlation (ICC) came from a similar cluster‐RCT with school‐aged children, which reported an ICC for MVPA of 0.08. Unit of allocation: licensed daycare centers Missing data handling: data were analyzed by intention‐to‐treat. A sensitivity analysis was done to determine the effect of dropouts or missing data on the primary outcome Reported limitations: 1. May not have had sufficient power to detect a significant difference in primary outcomes; 2. Time frame used to compare the 2 relevant arms (child + caregiver and child only) may not have been accurate for all childcare centers; 3. Engagement with and adherence to the intervention by childcare providers and parents was suboptimal; 4. Baseline activity levels of the included children were high, making it more difficult to distinguish if the intervention had a significant effect; 5. There was a significant time effect in which all arms increased their physical activity Randomization ratio and stratification: 1:1:1; stratified by season (spring 2013, fall 2013, fall 2014) Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: an invitation letter was mailed to the directors of all licensed daycare centers and was followed up with a phone call. The first 18 daycare centers that expressed an interest and met eligibility criteria were randomized. All children in daycare centers meeting the eligibility criteria were approached for inclusion in the study and consented Inclusion criteria: cluster: licensed childcare center in Canada's National Capital Region enrolling ≥ 20 children aged 3 to 5 years; participants: children aged 3 to 5 years with English‐ or French‐speaking parents who reported planning to stay at their respective childcare centers for at least 6 months Exclusion criteria: not reported Age of participating children at baseline: 3 to 5 years Total number randomized by relevant group: total across all study arms: n = 215; child + caregiver arm: n = 94; child‐only arm: n = 59 Baseline imbalances between relevant groups: significant differences not reported, but the child + caregiver arm had 72% boys (68/94) compared to the child‐only arm, which had 39% (23/59). They were also significantly older (P = 0.016) than the child‐only arm and had more fat‐free mass than the child‐only arm (P = 0.004) Total number analyzed by relevant group: children's physical activity levels, measured by accelerometry (child + caregiver arm: n = 35, child‐only arm: n = 19); children's weight status (child + caregiver arm: n = 52, child‐only arm: n = 36) Attrition by relevant group: child + caregiver arm: 44.7% (42/94); child‐only arm: 39.0% (23/59) Description of sample for baseline characteristics reported above: consented children (child + caregiver arm: n = 94; child‐only arm: n = 59) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 3 months, and 6 months (end of intervention)
|
|
| Identification |
Study name: Activity Begins in Childhood (ABC) Country: Canada Setting: licensed daycare centers in Ottawa, Canada Types of reports: published protocol; published journal article; trial registration Comments: used the following reports: (1) Adamo 2014; (2) Adamo 2017b; (3) Trial registration (ISRCTN94022291) Author's name: Kristi B Adamo Email: kadamo@cheo.on.ca; kadamo@uottowa.ca Conflicts of interest: "The authors declare that they have no competing interests" (quote) Sponsorship source: Canadian Institutes of Health Research (CIHR) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Judgment comment: used a computer‐generated randomization sequence, stratified by daycare center size, language of delivery, and season |
| Allocation concealment | Low risk | Quote: "to ensure adequate allocation concealment, the computer‐generated randomization sequence was kept centrally by a data manager not affiliated with this trial" (Adamo 2014, p 309) |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: the investigator and the analyst—but not center staff—were blinded to center assignment. Given that the children were aged 3 to 5 years, their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Low risk | Judgment comment: outcomes were measured objectively by accelerometer, and the investigator and the analyst were blinded to center allocation |
| Incomplete outcome data All outcomes | High risk | Judgment comment: we calculated attrition rates by summing the number of participants who left the childcare center, graduated from the childcare center, or did not participate in data collection because of burden, and dividing by the number of children randomized. Total attrition was 34.4% (74/215) for the study overall and 42.5% (65/153) for the 2 relevant study arms. Differential attrition for the 2 relevant study arms was 5.7% (42/94 vs 23/59). Among children who stayed in the trial, some had incomplete data. There were baseline differences between children with and without missing data. Efforts to address this included sensitivity analysis to investigate influence of dropouts and missing data on primary outcomes. Sensitivity analyses included a sample with children that had at least 1 hour of physical activity data from at least 1 day (n = 128 of 215 children enrolled across all 3 study arms). Findings of the sensitivity analysis were not different from findings of the main analysis |
| Selective reporting | High risk | Judgment comment: the trial was registered and the protocol was published. Expected outcomes were pre‐specified and addressed in the article. However, study authors reported in the protocol that "The primary outcome (MVPA) will be measured at baseline and at three months and six months post‐intervention" (quote; Adamo 2014, p 310), but results for 3 months were not reported and could not be retrieved from the study authors |
| Recruitment bias | Low risk | Judgment comment: randomization occurred following baseline data collection |
| Baseline imbalance | Unclear risk |
Quote: "baseline child characteristics, physical activity levels, general anthropometrics, and accelerometer wear time were comparable between groups..." (Adamo 2017b, p 44) Judgment comment: the study authors did not report on similarities and differences between clusters |
| Loss of clusters | Unclear risk | Judgment comment: the study authors did not report whether any clusters were lost |
| Incorrect analysis | Low risk | Quote: "to account for the cluster‐randomized design, a linear mixed effects model with a random effect for center was used to compare change in primary and secondary outcomes from baseline to six months" (Adamo 2014, p 313) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: there was insufficient information to permit judgment |
| Other sources of bias | High risk | Judgment comment: the child + caregiver arm had 72% boys (68/94) compared to the child‐only arm, which had 39% (23/59). They were also significantly older (P = 0.016) than the child‐only arm and had more fat‐free mass than the child‐only arm (P = 0.004) |
Alhassan 2018a.
| Methods |
Study design: randomized controlled trial Study grouping: parallel group Study aim: "...to examine the feasibility and efficacy of a 12‐week culturally tailored mother‐daughter PA intervention on the PA levels of pre‐adolescent African‐American girls" (quote) Study period: study start date: January 2013; primary completion date: August 2014 Total number of arms: 3 Description of intervention arms: 1. Dancing intervention with mother involvement (child + caregiver); 2. Dancing intervention alone (child‐only); 3. No‐intervention comparison group (not eligible) Sample size justification and outcome used: "the sample size and power calculation were based on a three‐group model in which we examined differences in rate‐of‐change in percent of time spent in MVPA between any two groups over 12 weeks" (quote). The sample size calculation was based on the Stanford GEMS pilot study and baseline data from the GEMS 2‐year intervention. To detect a difference between 20 and 50 minutes of MVPA per day between any 2 groups, with 80% power and an alpha level of 0.05, approximately 20 dyads per arm (60 overall) were needed Unit of allocation: mother‐daughter dyad Missing data handling: hierarchical linear modeling (HLM) software was used, which "accommodates for missing data, retaining participants who contribute data for at least one‐time point for the dependent variable" (quote) Reported limitations: 1. Small sample size due to high attrition rates; 2. Attrition rate highest among control group participants (non‐uniform attrition); 3. No transportation provided for participants; 4. Intervention did not directly target the home environment Randomization ratio and stratification: 1:1:1; stratified by girls' BMI percentile (≥ 85th percentile, < 85th percentile) Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: participants were recruited via flyers, radio announcements, and face‐to‐face recruitment. Eligible children and mothers were asked to provide written assent or informed consent upon enrollment into the study Inclusion criteria: child: female and 7 to 11 years old on the date of randomization, identified by her mother as African American or Black; mother: self‐defined as African American or Black and defined herself as the primary maternal figure that resided with the child Exclusion criteria: participant: child had any condition limiting her ability to participate in the physical activity intervention or in the assessment of physical activity, child had any medical condition that limited growth or took any medications affecting growth, or the girl or mother were unable to read and complete the informed consent in English Age of participating children at baseline: 7 to 11 years Total number randomized by relevant group: total across all study arms: n = 76; child + caregiver arm: n = 28; child‐only arm: n = 25 Baseline imbalances between relevant groups: significant between‐group baseline differences were observed for girls' age (P = 0.02) and for mothers' marital status (P = 0.002) and for education level (P = 0.04) Total number analyzed by relevant group: total across all study arms: n = 32; child + caregiver arm: n = 14; child‐only arm: n = 12 Attrition by relevant group: child + caregiver arm: 50.0% (14/28); child‐only arm: 48.0% (12/25) Description of sample for baseline characteristics reported above: consented children and mothers (child + caregiver arm: n = 28; child‐only arm: n = 25) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 6 weeks, and 12 weeks (end of intervention)
|
|
| Identification |
Study name: Mothers And dauGhters daNcing togEther Trial (MAGNET) Country: USA Setting: elementary school in Springfield, Massachusetts Types of reports: published protocol; published journal article; trial registration Comments: used the following reports: (1) Alhassan 2018; (2) Burkart 2017; (3) Trial registration (NCT01588379) Author's name: Sofiya Alhassan Email: alhassan@kin.umass.edu Conflicts of interest: "Authors have no conflict of interest to report" (quote) Sponsorship source: Canadian Institutes of Health Research (CIHR) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Judgment comment: insufficient information to permit judgment |
| Allocation concealment | Unclear risk | Judgment comment: methods to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no blinding was done. Given that children were aged 7 to 10 years, their performance was not likely to have been influenced by lack of blinding. However, outcomes related to the caregivers may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information was provided on blinding of outcome assessors. Height and weight were measured. Physical activity was assessed by accelerometer. BMI may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgment comment: we calculated attrition rates by dividing the number of dropouts by the number of children participating at baseline. Total attrition at 12 weeks (end of intervention) was 57.9% (44/76) for the study overall and 50.9% (27/53) for the 2 relevant study arms. Differential attrition for the 2 relevant study arms was 2.0% (14/28 vs 13/25) |
| Selective reporting | High risk | Judgment comment: the trial was registered and expected outcomes pre‐specified. However, study authors reported in the Abstract that vigorous physical activity was measured, but results for these were not reported in the Results section. Also, in the trial registry entry, study authors pre‐specified BMI as a secondary outcome, but results for this were not reported in the article |
| Recruitment bias | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Baseline imbalance | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Loss of clusters | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Incorrect analysis | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Comparability with individually randomized trials | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Other sources of bias | High risk | Judgment comment: significant differences in mothers' BMI, income, and marital status (measured at baseline) were observed between dyads that dropped out and those with complete data |
Baghurst 2014.
| Methods |
Study design: randomized controlled trial Study grouping: parallel group Study aim: "...to examine the effectiveness of a child‐only (i.e. control) versus a child‐plus‐parent (i.e. experimental) nutritional education program in reducing risk factors associated with childhood obesity" (quote). These included knowledge of nutrition, dietary behavior, physical activity behavior, and sense of self‐efficacy Missing data handling: not reported Study period: not reported Total number of arms: 2 Description of intervention arms: 1. Child‐plus‐parent nutritional education program (child + caregiver); 2. Child‐only nutritional education program (child only) Sample size justification and outcome used: not reported Unit of allocation: individual child Missing data handling: not reported Reported limitations: 1. Self‐reported data may be unreliable, particularly among children Randomization ratio and stratification: 1:1 Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although the study authors do not report data on household income/socioeconomic status by intervention arm, they noted that the site of the study was a Title 1 school, which is determined by high concentration of low‐income students Recruitment methods: following permission from the school principal, 8 classrooms (4 second grade and 4 third grade) were recruited for the intervention study. All potential students and parents were asked to take part in the intervention, and parents were also provided with an informational package. Children were randomized after parental consent was received Inclusion criteria: participants: second and third grade students at participating school and a caregiver Exclusion criteria: not reported Age of participating children at baseline: second to third grade (estimated to be 6 to 9 years of age) Total number randomized by relevant group: total across both study arms: n = 176; child + caregiver arm: n = 93; child‐only arm: n = 83 Baseline imbalances between relevant groups: significant differences not reported Total number analyzed by relevant group: not reported Attrition by relevant group: not reported Description of sample for baseline characteristics reported above: consented children (child + caregiver arm: n = 93; child‐only arm: n = 83) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline and 10 weeks (end of intervention)
|
|
| Identification |
Study name: not reported Country: USA Setting: low‐income school in a rural area of the Western USA Types of reports: published journal article Comments: used only 1 report: Baghurst 2014 Author's name: Timothy Baghurst Email: tim.baghurst@okstate.edu Conflicts of interest: not reported Sponsorship source: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk |
Quote: "after parental consent forms were collected, child study participants were randomly placed into one of two study groups..." (p 233) Judgment comment: the method used to generate the random sequence was not described |
| Allocation concealment | Unclear risk | Judgment comment: methods to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: no information was provided on blinding of participants and personnel. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged approximately 6 to 9 years, so their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Because all outcomes were self‐reported by study participants, outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | Unclear risk | Judgment comment: attrition rates were not reported and could not be calculated |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Dietary and physical activity outcomes were reported incompletely and could not be entered into meta‐analysis. We could not retrieve relevant data from the study authors |
| Recruitment bias | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Baseline imbalance | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Loss of clusters | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Incorrect analysis | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Comparability with individually randomized trials | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Other sources of bias | Low risk | Judgment comment: the study authors noted that "self‐reporting data is historically unreliable particularly with children" (quote; p 236). However, they selected "four existing validated instruments" (quote; p 231) to measure their study outcomes to minimize this bias. We detected no other sources of bias |
Cottrell 2005.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to evaluate the effectiveness of intervention approaches aimed at incorporating parental participation and increasing parents' knowledge and practice in delivering a healthy diet and more opportunities for physical activity to their children" (quote) Study period: 4 weeks during the 2003‐2004 school year Total number of arms: 2 Description of intervention arms: 1. Child and parental participation (child + caregiver); 2. Child participation only (child only) Number of clusters per arm: child + caregiver arm: n = 14; child‐only arm: n = 15 Average cluster size: 15.07 children Sample size justification and outcome used: not reported Unit of allocation: schools Missing data handling: participants with missing data were excluded from analyses Reported limitations: 1. Only about half of all families screened returned a baseline questionnaire; 2. Some outcomes were reported by caregivers; 3. Screening was made available to all kindergarten students, but the findings are based on a convenience sample; and 4. The intervention was short term (4 weeks) Randomization ratio and stratification: ˜ 1:1; stratification not reported Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (Intervention group)
Child‐only arm (control group)
Although not reporting by intervention arm, the study authors do provide additional information on the overall study sample
Recruitment methods: 4 rural counties out of 10 in West Virginia, whose staff indicated interest in rural health and education, were randomly chosen and invited to participate. It is unclear whether the 29 schools that were randomized were the total number of schools within these counties, or whether a proportion of schools were recruited. A short description of the program was provided to teachers and children, and then a booklet consisting of a caregiver consent form and the screening intake form was sent home with the children Inclusion criteria: cluster: school located in 1 of 4 randomly chosen rural counties; participants: children enrolled in kindergarten (aged 4 to 6 years) and caregivers Exclusion criteria: not reported Age of participating children at baseline: 4 to 6 years (kindergarten) Total number randomized by relevant group: total across both study arms: n = 437. Samples per arm were not reported and therefore were estimated: child + caregiver arm: n = 219; child‐only arm: n = 219 Baseline imbalances between relevant groups: baseline characteristics not reported by study arm Total number analyzed by relevant group: child + caregiver arm: n = 24; child‐only arm: n = 26 Attrition by relevant group: attrition was not reported and cannot be calculated because study authors did not report the number of children by intervention arm at baseline Description of sample for baseline characteristics reported above: children included in the analysis (child + caregiver arm: n = 24; child‐only arm: n = 26) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline and 4 weeks (end of intervention)
The following instrument was used to measure outcomes relevant to this review at 1 week, 2 weeks, 3 weeks, and 4 weeks (end of intervention)
Children's height and weight were measured at baseline and were used to calculate prevalence of overweight or obesity based on the CDC age‐ and gender‐specific growth charts. However, measurements do not appear to have been repeated at the end of the intervention |
|
| Identification |
Study name: Coronary Artery Risk Detection in Appalachian Communities (CARDIAC)—Kinder Country: USA Setting: homes in rural West Virginia Types of reports: published journal article Comments: used only one report: Cottrell 2005 Author's name: Lesley Cottrell Email: lcottrell@hsc.wvu.edu Conflicts of interest: not reported Sponsorship source: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk |
Quote: "randomization was conducted at school level..." (p 357) Judgment comment: the method used to generate the random sequence was not reported |
| Allocation concealment | Unclear risk | Judgment comment: methods to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged 4 to 6 years, so their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. However, steps were measured by pedometer and are unlikely to have been influenced by lack of blinding. Fruit and vegetable intake was measured by caregiver report and may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgment comment: attrition rates were not reported and could not be calculated because the study authors did not report the number of children by intervention arm at baseline. However, 88.5% (386/436) of children screened (with consent) and 75.4% (153/203) of children who returned the baseline questionnaire did not have complete data and were excluded from analyses |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Data on child steps were reported in a format that could be entered into meta‐analysis. However, the format in which dietary outcome data were reported lacked clarity, and we could not retrieve the relevant data from study authors. Due to our lack of confidence in the dietary data, we did not extract them |
| Recruitment bias | High risk | Judgment comment: schools were randomized before recruitment of participants |
| Baseline imbalance | Unclear risk | Judgment comment: the study authors did not report on similarities and differences between intervention arms or clusters |
| Loss of clusters | Unclear risk | Judgment comment: loss of clusters was not reported. However, nearly 90% of screened children did not have complete data from the intervention and were excluded from the analysis, so it is possible that some clusters could have been lost |
| Incorrect analysis | Low risk | Quote: "a repeated measures multivariate analysis of covariance (MANCOVA) was used to evaluate differences between the groups based on children's average steps across the four‐week period while controlling for potential clustering effects related to school enrollment" (p 598) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Crespo 2012a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to compare the independent and combined effects of changes in home/family environments and changes in school/community environments to prevent and control childhood obesity among Latinos" (quote) Study period: recruitment: August 2003 to January 2004 and again from May 2004 to December 2004; final assessment: 3 years after baseline assessment Total number of arms: 4 Description of intervention arms: 1. School/community‐level intervention and individual/family‐level intervention (child + caregiver); 2. School/community‐level intervention (child only); 3. Individual/family‐level intervention (not eligible); 4. No intervention control (not eligible) Number of clusters per arm: child + caregiver arm: n = 3; child‐only arm: n = 3; individual/family‐level arm: n = 3; no intervention control arm: n = 4 Average cluster size: 62.15 children Sample size justification and outcome used: it is unclear whether sample size calculations were conducted before the study. The study authors presented post‐hoc power calculations relative to the sample of participants analyzed at the final, end‐of‐intervention assessment (analysis sample = 441 children) using BMI as the outcome. The calculation was done relative to hypothesized effect sizes based on a 3‐year assessment, with effect based on data from a prior study in a similar population (average BMI change = 1.99 kg/m2). The study authors considered the no‐treatment control arm relative to the child + caregiver arm and assumed that the child‐only intervention would account for one‐third of the observed change (0.66 kg/m2) and the caregiver component would be responsible for two‐thirds of the change (1.33 kg/m2). Using an estimated standard deviation of 2.02 kg/m2, the standardized effect sizes were hypothesized to be 0.66 for a caregiver‐only main effect and 0.33 for the child‐only intervention main effect. An intracluster correlation (ICC) calculated for this study of 0.016 was used to account for school clustering. Based on this information and a significance level of 0.05 (2‐sided), the study authors determined that power was 80% to detect the child‐only intervention main effect and 97% to detect a caregiver‐only main effect Unit of allocation: school Missing data handling: all available data were used. Therefore, even when a participant had missing data at 1 or more time points, available data for other time points were included in the analysis Reported limitations: 1. High rates of attrition; 2. Survey measures were self‐reported by parents, and a measure of social desirability, which could have been used to adjust for self‐report bias, was not included in the survey; 3. Some measures, such as child physical activity, consisted of a single parent self‐report item rather than more valid objective measures (e.g. accelerometry) Randomization ratio and stratification: ˜ 1:1:1:1; stratification not reported Participant compensation or incentives: parent‐child dyads were given USD 20 after completing the baseline assessment |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although not reporting by intervention arm, study authors do provide additional information on the overall study sample
Recruitment methods: project staff contacted schools in the target region to describe the study, determine whether inclusion criteria were met, and obtain consent to participate. Thirteen of the 25 schools contacted met the criteria and agreed to participate. Caregivers were recruited at the schools through presentations and through fliers sent home with students Inclusion criteria: cluster: school in one of the target school districts, Latino enrollment ≥ 70%, defined attendance boundaries (no charter or magnet schools), no obesity‐related programs or additional physical education training for teachers within the past 4 years, willing to be randomized to experimental condition; participants: children entering kindergarten, first grade, or second grade; caregivers, self‐identified as Latino, living within school attendance boundaries; caregivers able to read in English or Spanish and willing to be randomized to experimental condition, intending to live in the area for at least 1 year Exclusion criteria: cluster: not reported; participants: children on a medically prescribed restricted diet or with a condition that limited physical activity Age of participating children at baseline: kindergarten to third grade (estimated to be 4 to 9 years old) Total number randomized by relevant group: total across all study arms: n = 808; child + caregiver arm: n = 165; child‐only arm: n = 218. These numbers appear to correspond to all children enrolled in the randomized classes Baseline imbalances between relevant groups: not reported Total number analyzed by relevant group: 1‐year assessment (child + caregiver arm: n = 145, child‐only arm: n = 196); 2‐year assessment (child + caregiver arm: n = 119, child‐only arm: n = 154); end of intervention (child + caregiver arm: n = 83, child‐only arm: n = 128) Attrition by relevant group: attrition rates were calculated by summing the number of participants who refused data collection, were lost to follow‐up, or were dropped, and dividing this by the number of children randomized. Attrition rates at 1‐year assessment: child + caregiver arm: 1.8% (3/165), child‐only arm: 1.4% (3/218); attrition rates at end of intervention: child + caregiver arm: 32.7% (54/165), child‐only arm: 28.4% (62/218) Description of sample for baseline characteristics reported above: all children included in analysis as reported in Crespo 2012b: child + caregiver arm: n = 163, child‐only arm: n = 216 |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 1 year, 2 years, and 3 years (end of intervention)
Study authors describe the 1‐year assessment as "immediate 1‐year post‐intervention" and the 2‐year and 3‐year assessments as "follow‐up" assessments. However, given that intervention activities continue for the entire 3‐year duration, we have determined to consider the 1‐year and 2‐year assessments to have taken place during the intervention, and the 3‐year assessment to represent the end of the intervention. |
|
| Identification |
Study name: Aventuras para Niños Country: USA Setting: South Bay region of San Diego County, California, adjacent to the US−Mexico border Types of reports: published journal articles Comments: used the following reports: (1) Crespo 2012b, (2) Elder 2010, (3) Ayala 2010. Publications for this study report different sample sizes, and CONSORT diagrams differ in the Crespo 2012b and Ayala 2010 publications. To the extent possible, we report numbers from the primary outcome paper (Crespo 2012b) Author's name: John P Elder Email: jelder@mail.sdsu.edu Conflicts of interest: "The authors have no conflicts of interest to disclose" (quote) Sponsorship source: National Heart, Lung and Blood Institute. Additional support was provided to individual authors by the Centers for Disease Control and Prevention, the American Cancer Society, the National Institute of Diabetes and Digestive and Kidney Diseases, and the National Heart, Lung and Blood Institute |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk |
Quote: "…schools were the unit of randomization" (Crespo 2012b, p 86) Judgment comment: the method used to generate the random sequence was not reported |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged approximately 4 to 9 years, so their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: outcome assessors were blinded to height and weight measurements: "measurement staff were blinded to participants' study condition" (quote; Crespo 2012b, p 90). Data for other outcomes (including dietary intake) were measured by caregiver report and may or may not have been influenced by lack of blinding. Study authors noted risk of social desirability bias as a study limitation |
| Incomplete outcome data All outcomes | High risk | Judgment comment: using data from the primary outcome paper (Crespo 2012b), we calculated attrition rates by summing the number of participants who refused data collection, were lost to follow‐up, or were dropped, and dividing this by the number of children randomized. At 1‐year assessment, total attrition was 1.1% (9/808) for the study overall and 1.0% (4/383) for the 2 relevant study arms. Differential attrition for the relevant study arms was 1.8% (3/165 vs 1/218). The analysis included 88% (145/165) of those in the child + caregiver arm and 90% (196/218) of those in the child‐only arm. Taking the same approach to calculate attrition for the end‐of‐intervention (3‐year) assessment, total attrition was 30.4% (246/808) for the study overall and 30.3% (116/383) for the 2 relevant study arms. Differential attrition for the relevant study arms was 4.3% (54/165 vs 62/218). The analysis included 50% (83/165) of those in the child + caregiver arm and 59% (128/218) of those in the child‐only arm |
| Selective reporting | Unclear risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Dietary and anthropometric outcomes were reported in a format that could be entered into meta‐analysis. Although physical activity and sedentary behavior outcomes were measured and reported completely, they did not align with those analyzed in this review |
| Recruitment bias | Low risk | Quote: "randomization of schools to study conditions took place immediately after all participants completed baseline measures" (Crespo 2012b, p 86) |
| Baseline imbalance | Unclear risk | Judgment comment: study authors did not report on similarities and differences between intervention arms or clusters |
| Loss of clusters | Low risk | Judgment comment: no clusters were lost |
| Incorrect analysis | Low risk | Quote: "...all models adjusted for clustering at the school level. With one exception, the intraclass correlations (ICC) for the outcome measures ranged from 0 to 0.019. These ICCs were well within the range anticipated by the study based on published estimates of other school‐based studies...The lone exception was number of snacks consumed per day with an ICC of 0.095" (Crespo 2012b, p 86) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
De Bock 2013a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "to assess whether a participatory parent‐focused approach using parents as agents of behavioral change enhances the efficacy of a preschool physical activity intervention" (quote) Study period: randomization: August 2008; data collection start date: September 2008; data collection end date: May 2010 Total number of arms: 2 Description of intervention arms: 1. Preschool physical activity program and participatory intervention (child + caregiver); 2. Preschool physical activity program (child only) Number of clusters per arm: child + caregiver arm: n = 19; child‐only arm: n = 20 Average cluster size: 21.18 children Sample size justification and outcome used: to detect a difference of 19.05 accelerometry counts per 15 seconds (0.5 standard deviation) between the child + caregiver arm and the child‐only arm, with 90% power and a 5% probability of a type 1 error, 504 children in 24 schools were required. Estimate of standard deviation (38.1 counts per 15 seconds) came from unpublished data from pilot studies with children aged 4 to 5 years. Study authors conservatively estimated an intracluster correlation (ICC) of 0.1 (design effect = 3). Recruitment aimed to enroll 280 children per arm (560 children total) to account for an anticipated 10% loss‐to‐follow‐up rate Unit of allocation: preschools Missing data handling: "in all models, missing data of outcomes were imputed by a cross‐sectional regression imputation approach" (quote). Age, gender, and measurement time were used as predictors in imputation analyses; 14.6% of anthropometry data and 31% of physical activity data were imputed using this approach. The pattern of missing physical activity monitoring data did not differ between the 2 arms. Missing data between children with and without physical activity monitoring differed only with respect to immigrant background. Sensitivity analyses were used to assess the effects of missing data Reported limitations: 1. Children were sampled from preschools that voluntarily applied for a state‐sponsored physical activity program, which may have reduced generalizability; 2. Absence of children on measurement days may have introduced post‐randomization selection bias; 3. Difficult to attribute intervention effects to specific components due to site‐level adaptations; 4. The study did not include a control group that received no intervention; 5. Intervention facilitators were involved in the process evaluation, which might have biased these results Randomization ratio and stratification: 1:1, stratified by school socioeconomic status (low, middle, high) and location (rural, non‐rural) Participant compensation or incentive: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although not reporting by intervention arm, study authors do provide additional information on the overall study sample
Recruitment methods: all preschools that applied for the state‐sponsored physical activity program were approached about participating. Details on recruitment were not reported Inclusion criteria: cluster: participation in an existing, state‐sponsored physical activity program; participants: children aged 4 to 6 years and caregivers Exclusion criteria: cluster: fewer than 15 children participating in the state‐sponsored physical activity program or without an external physical activity teacher in the area; participants: not reported Age of participating children at baseline: 4 to 6 years (preschool) Total number randomized by relevant group: total across both study arms: n = 826; child + caregiver arm: n = 441; child‐only arm: n = 385 Baseline imbalances between relevant group: the child + caregiver arm had larger group sizes than the child‐only arm (mean cluster size 23 vs 19). No other significant differences in baseline characteristics were observed between study arms Total number analyzed by relevant group: child + caregiver arm: n = 433; child‐only arm: n = 376 Attrition by relevant group: attrition rates were calculated as the number of children whose schools withdrew consent divided by the number of children randomized: child + caregiver arm: 1.8% (8/441), child‐only arm: 2.3% (9/385). Data for all other children were available or imputed Description of sample for baseline characteristics reported above: total sample analyzed (n = 809) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 6 months (end of intervention), and 1 year (follow‐up)
The study authors note that 6‐month data were collected "shortly before the end of intervention" |
|
| Identification |
Study name: Ene mene fit Country: Germany Setting: preschools in Baden‐Württemberg, Germany Types of reports: published protocol; published journal article; trial registration Comments: used the following reports: (1) De Bock 2010, (2) De Bock 2013b, (3) Trial registration (Clinicaltrials.gov NCT00987532) Author's name: Freia De Bock Email: freia.debock@medma.uni‐heidelberg.de Conflicts of interest: "the authors declare that they have no competing interests" (quote) Sponsorship source: Landesstiftung Baden‐Wurttemberg |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk |
Quote: "preschools were randomized (1:1) after stratification for aggregate SES [socioeconomic status] and geographic location (urban vs rural) using sealed opaque envelopes" (De Bock 2013b, p 65) Judgment comment: the method used to generate the random sequence was not reported |
| Allocation concealment | Low risk | Quote: "preschool assignment was blinded through the use of sequentially numbered, sealed envelopes" (De Bock 2010, p 53) |
| Blinding of participants and personnel All outcomes | Low risk |
Quote: "due to the participatory nature of the study, it was not possible to blind participants and study personnel" (De Bock 2010, p 53 to 54) Judgement comment: given that children were 4 to 6 years of age, their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Low risk |
Quote: "outcome assessors were blinded to group allocation as suggested for prospective randomized open trials with blinded evaluation" (De Bock 2013b, p 65) Judgment comment: height and weight were measured and physical activity was assessed by accelerometer |
| Incomplete outcome data All outcomes | High risk | Judgment comment: we calculated attrition rates as the number of children whose schools withdrew consent divided by the number of children randomized. Total attrition in the 2 relevant study arms was 2.1% (17/826). Differential attrition was 0.5% (8/441 vs 9/385). Additionally, 3 schools in the child + caregiver arm did not receive the intervention because the teachers disliked the measurements. However, the study authors did not report overall how many participants were lost to follow‐up or withdrew from the study. Missing data (31% of physical activity data and 14.6% of anthropometry data) were imputed for analyses. Sensitivity analyses to assess the effects of missing data on outcomes found that the direction of effects remained the same for all outcomes, but only the reduction in sedentary behavior and the increase in general perceived health remained significant |
| Selective reporting | Low risk | Judgment comment: the trial was registered and the protocol was published. Expected outcomes were pre‐specified and were addressed in the article |
| Recruitment bias | Unclear risk | Judgment comment: it is unclear whether children were recruited before or after randomization |
| Baseline imbalance | Unclear risk |
Quote: "except for larger group sizes in the intervention arm (mean cluster size 23 (15–50) vs 19 (9–46)), there were no differences in baseline characteristics between the study arms" (De Bock 2013b, p 67) Judgment comment: study authors did not report on similarities and differences between clusters |
| Loss of clusters | High risk | Judgment comment: study authors reported that 1 preschool in each study arm withdrew consent after randomization. A further 3 schools in the child + caregiver arm did not receive the intervention because teachers disliked the measurements |
| Incorrect analysis | Low risk | Quote: "the core model assumed a linear change of the outcomes with time and included two normally distributed random effects (one at the preschool level and one at the child level) to adjust for clustering in the data due to the hierarchic sampling scheme" (De Bock 2013b, p 67) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: study authors reported that "absence of children on measurement days may have introduced post‐randomization selection bias" (quote; De Bock 2013b, p 72). Children without physical activity measurements were more likely to have an immigrant background. However, "the possible oversampling of a low‐risk population (without immigrant background) would rather lead to an underestimation of effect size, and is very unlikely to change the direction of effect" (quote; De Bock 2013b, p 72) |
De Bourdeaudhuij 2002.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "… to determine whether changes in fat intake and in psychosocial determinants could be found as a result of tailored nutrition education aiming at reducing fat, and whether this intervention is more effective when two family members participate in the intervention study compared with an intervention directed to an individual family member" (quote) Study period: not reported Total number of arms: 3 Description of intervention arms: 1. Family‐based condition including adolescent and an adult (child + caregiver); 2. Adolescent‐only condition (child only); 3. Adult‐only condition (not eligible) Number of clusters per arm: child + caregiver arm: n = 19; child‐only arm: n = 16; adult‐only condition: n = 17 Average cluster size: 3.33 children Sample size justification and outcome used: not reported Unit of allocation: class Missing data handling: not reported Reported limitations: 1. Selection bias due to oversampling of mothers and adolescents with lower fat intake levels; 2. Intervention did not include all possible family members; 3. Only short‐term intervention impacts were assessed; 4. Self‐reported measures were used to assess intervention outcomes; 5. Long interval between screening of participants and provision of tailored feedback may have contributed to dropout; 6. Intervention focused only on fat intake reduction and did not emphasize the importance of a simultaneous reduction in energy intake Randomization ratio and stratification: ˜ 1:1:1, with more classes randomized to the child + caregiver arm because a lower response rate was expected for this group Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: no information reported on recruitment of study schools or classes. Researchers report that there were 2 secondary schools in the study, and that 52 classes with students aged 15 to 18 years were included. A letter explaining the study and seeking consent (tailored to each study arm) was provided to caregivers and adolescents. Participants were made aware of only their own study condition Inclusion criteria: cluster: class in 1 of 2 selected secondary schools; participants: children aged 15 to 18 years and caregivers Exclusion criteria: not reported Age of participating children at baseline: 15 to 18 years Total number randomized by relevant group: child + caregiver arm: n = 55; child‐only arm: n = 71. Total number across all study arms not reported because the ineligible study arm included caregivers but not children Baseline imbalances between relevant groups: significant differences were not reported, but the child + caregiver arm had 75% (33/44) female adolescent participants and the child‐only arm had 60% (30/50) female participants Total number analyzed by relevant group: diet outcome (child + caregiver arm: n = 44 dyads; child‐only arm: n = 50) Attrition by relevant group: attrition rates were calculated by summing the number of dyads who dropped out and dividing this by the number randomized: child + caregiver arm: 20% (11/55); child‐only arm: 30% (21/71). Study authors report that dyads dropped out of the child + caregiver arm “mainly because only the adolescent or the parent was willing to complete the post‐test questionnaire" (quote) Description of sample for baseline characteristics reported above: all participants who completed both baseline and post‐test questionnaires |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline and at 10 weeks (end of intervention)
|
|
| Identification |
Study name: not reported Country: Belgium Setting: secondary schools in Flanders, Belgium Types of reports: published journal article Comments: used only 1 report: De Bourdeaudhuij 2002 Author's name: Ilse De Bourdeaudhuij Email: ilse.debourdeaudhuij@ugent.be Conflicts of interest: not reported Sponsorship source: Ghent University and the Flemish Fund for Scientific Research |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk |
Quote: "the classes were randomized in three groups before recruitment" (p 437) Judgment comment: however, the method used to generate the random sequence was not reported |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk |
Quote: "participants were only aware of their own study condition, not of the other conditions" (p 437) Judgment comment: however, it is possible that children or caregivers or both from different classes could have spoken about the intervention |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: dietary data were measured by self‐report and may or may not have been influenced by lack of blinding. No information was provided on whether or not study staff were blinded |
| Incomplete outcome data All outcomes | High risk | Judgment comment: we calculated attrition rates by summing the number of dyads who dropped out and dividing this by the number randomized. Total attrition in the overall study was 21% (37/173) and from the 2 relevant study arms was 25.4% (32/126). Differential attrition between relevant study arms was 10% (11/55 vs 21/71). No significant differences in baseline characteristics were found between dropouts and participants with complete data |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Percentage of total energy from fat intake was reported incompletely and could not be entered into meta‐analysis. We could not retrieve the relevant data from study authors |
| Recruitment bias | High risk | Quote: "the classes were randomized in three groups before recruitment" (p 437) |
| Baseline imbalance | Unclear risk | Judgment comment: study authors did not report on similarities and differences between intervention arms or clusters |
| Loss of clusters | Unclear risk | Judgment comment: study authors did not report whether any clusters were lost |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Dietsch 1990.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "...to test the effectiveness of a school‐based parent program (SPP) as an adjunct to a school‐based program (SMART) for 7th grade students on dietary changes in adults and their adolescent children over a one year period" (quote) Study period: study start: January 1987; study end: January 1988 Total number of arms: 2 Description of intervention arms: 1. School‐based intervention and parent intervention (child + caregiver); 2. School‐based intervention (child only) Number of clusters per arm: 3 Average cluster size: 15 children Sample size justification and outcome used: not reported Unit of allocation: school Missing data handling: participants with missing data were excluded from the main analysis, but a number of methods were applied to assess potential attrition biases and threats to internal and external validity. First, the study author assessed differences between those who dropped out and those who stayed in the study, and found few differences. Second, she kept all dropouts in the post‐test analyses and used their pre‐test scores. This resulted in similar findings Reported limitations: 1. Selection bias, as participants were different than non‐participants and caregivers knew the details of the intervention to which they would be allocated (“the study attracted primarily White, highly educated, health conscious individuals with high incomes” [quote]); 2. High attrition rate Randomization ratio and stratification: 1:1, stratified by socioeconomic status (low, medium, high) Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: caregivers of students in sixth, seventh, and eighth grades at Project SHARP schools were sent a recruitment letter. Those interested returned a printed form or requested more information. A second letter was sent to all interested caregivers describing the relevant intervention arm in greater detail and asking them to sign an agreement to participate and a waiver regarding physical activity. Only seventh grade children were eligible if they had a caregiver participating in the SMART Parent Program; they were enrolled only if their caregiver provided data at both of the first 2 health status assessments Inclusion criteria: cluster: unclear sampling approach, but junior high schools in the Greater Los Angeles area (2 low socioeconomic status [SES], 2 middle SES, and 2 high SES) participating in the Project SHARP program; participants: seventh grade students and caregivers (Note: the child‐only intervention was for seventh grade students, but caregivers of students in the sixth and eighth grades were invited to participate to increase the number of participating caregivers. Because the sample of caregivers was not restricted to those with children in the study, caregiver outcomes were not extracted) Exclusion criteria: not reported Age of participating children at baseline: sixth to eighth grade (estimated to be 10 to 14 years old) Total number randomized by relevant group: adolescents were not randomized and all received the school‐based intervention; only caregivers were randomized. Adolescents with caregivers in the SMART Parent Program: across both study arms: n = 90; child + caregiver arm: n = 31; child‐only arm: n = 59 Baseline imbalances between relevant groups: not reported Total number analyzed by relevant group: total number analyzed for relevant outcomes was not reported but was assumed to be those with data at the final assessment: child + caregiver arm: n = 20 children; child‐only arm: n = 47 Attrition by relevant group: children were considered in the sample only if their caregiver had data at the second caregiver health status assessment (child + caregiver arm: n = 31; child‐only arm: n = 59). Attrition rates were calculated as those for whom matched baseline and post‐test data were not available, divided by children considered in the sample: child + caregiver arm: 35.5% (11/31); child‐only arm: 20.3% (12/59). Description of sample for baseline characteristics reported above: children with caregivers with data at the second health status assessment: child + caregiver arm: n = 31; child‐only arm: n = 59. Caregiver sample included individuals without a participating child |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline and 9 months (end of intervention)
Data for caregivers' dietary intake also were collected but could not be used for this review because the caregiver sample had different inclusion criteria than the child sample |
|
| Identification |
Study name: SMART Parent Program Country: USA Setting: junior high schools in the Greater Los Angeles area Types of reports: PhD thesis Comments: used only 1 report: Dietsch 1990 Author's name: Barbara J Dietsch Email: bdietsc@wested.org Conflicts of interest: not reported Sponsorship source: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Judgment comment: a method for randomization was not reported. However, the trial author did note that "six junior high schools were stratified by socioeconomic status (low, medium, or high), matched, and assigned randomly from matched pairs to intervention or control conditions" (quote; p 37) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, children were aged 10 to 14 years, and their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: dietary data were measured by self‐report and may or may not have been influenced by lack of blinding. No information was provided on whether or not study staff were blinded |
| Incomplete outcome data All outcomes | High risk | Judgment comment: the trial author considered children to be in the sample only if their caregiver had data at the second caregiver health status assessment "Time 2" (child + caregiver arm: n = 31; child‐only arm: n = 59). We calculated attrition rates as those for whom matched baseline and end‐of‐intervention data were not available, divided by children considered in the sample. Total attrition was 25.6% and differential attrition was 15.2% (11/31 vs 12/59) |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Child dietary outcomes were reported incompletely, and not all could be entered into meta‐analysis. We could not retrieve relevant data from the study author |
| Recruitment bias | High risk | Judgment comment: recruitment of caregivers occurred after cluster‐randomization |
| Baseline imbalance | Unclear risk | Judgment comment: the number of clusters was low (n = 6), and study authors did not report similarities or differences between clusters. They did report the characteristics of caregivers at baseline, and the 2 arms appear to have been relatively balanced |
| Loss of clusters | Unclear risk | Judgment comment: the trial author did not report whether any clusters were lost |
| Incorrect analysis | High risk | Judgment comment: the study author did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Ducheyne 2014a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "… the primary aim of this present study was to evaluate the effects of a cycle training course on cycling skills in Belgian children from the fourth grade of elementary school within 1 week after the intervention and at 5 months follow‐up… A second aim of the study was to examine the effects of a cycle training course, with and without parental involvement, on levels of cycling to school and on parental attitudes towards cycling" Study period: baseline assessment: March 2012; endpoint assessment: April 2012; follow‐up assessment: October 2012 Total number of arms: 3 Description of intervention arms: 1. Child intervention plus parent condition (child + caregiver); 2. Child intervention (child only); 3. No intervention control (not eligible) Number of clusters per arm: 1 Average cluster size: 43.33 children Sample size justification and outcome used: not reported Unit of allocation: school Missing data handling: cycling skill data were analyzed for children who completed the practical cycling test at the 3 time points (117/130). For all other research questions, data were analyzed for children who returned parental questionnaires at the 3 time points (94/130). Study authors did not report doing sensitivity analyses to determine the effect of dropouts or missing data Reported limitations: 1. Only 3 schools were included in the study; 2. Ability to generalize is constrained by the inclusion of only children in the fourth grade; 3. Randomization of children was limited to randomization by schools (the clusters); 4. Researchers who scored children on the practical cycling test were not blinded; 5. No manipulation check was done on parental involvement; and 6. Cycling to school levels was proxy reported by parents Randomization ratio and stratification: 1:1:1, stratification not reported Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: 5 elementary schools in Flanders, Belgium, were selected at random. Letters were sent to principals inviting schools to take part. Three schools agreed to participate; 2 declined due to lack of time Inclusion criteria: cluster: not reported; participants: fourth grade students and caregivers Exclusion criteria: not reported Age of participating children at baseline: fourth grade (estimated to be 8 to 10 years old) Total number randomized by relevant group: total across all study arms: n = 130. Samples per arm were not reported and therefore were estimated: child + caregiver arm: n = 43; child‐only arm: n = 43 Baseline imbalances between relevant groups: significant differences were not reported, but the child + caregiver arm had 41.2% (14/34) boys, 90.6% children of normal weight, and 94.1% (32/34) children of higher socioeconomic status (SES) compared to the child‐only arm, which had 48% (12/25) boys, 79.2% children of normal weight, and 68% (17/25) children of higher SES Total number analyzed by relevant group: level of cycling to school and parental attitudes toward cycling (child + caregiver arm: n = 42, child‐only arm: n = 36) Attrition by relevant group: not reported and cannot be calculated because study authors did not report the number of children by intervention arm at baseline Description of sample for baseline characteristics reported above: children whose caregivers completed the questionnaire at all 3 time points (child + caregiver arm: n = 34, child‐only arm: n = 25) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 1 month (end of intervention), and 6 months (follow‐up)
Parents reported children's height and weight at baseline, and this was used to calculate body mass index. However, collection of height and weight measurements does not appear to have been repeated at subsequent assessments. |
|
| Identification |
Study name: not reported Country: Belgium Setting: primary schools in Flanders, Belgium Types of reports: published journal article Comments: used only 1 report: Ducheyne 2014b, as well as unpublished information provided by study authors (Cardon 2018 [pers comm]) Author's name: Fabian Ducheyne; corresponding author Greet Cardon Email: Greet.Cardon@UGent.be Conflicts of interest: not reported Sponsorship source: Lifeline Campaign of the Research Foundation—Flanders (FWO) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Judgment comment: schools were randomized by coin toss (Cardon 2018 [pers comm]) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged approximately 8 to 10 years, so their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | High risk | Judgment comment: for the practical cycling test, the "three researchers were not blinded for the condition they were testing" (quote Ducheyne 2014b, p 51). Parental report was used to assess child body mass index (BMI) |
| Incomplete outcome data All outcomes | High risk | Judgment comment: we calculated attrition by dividing the number of children with complete data at all time points by the number of children randomized with consent. Total attrition (including participants in a third non‐relevant study arm) was 10% (13/130) for the cycling test and 27.7% (36/130) for the questionnaire (used to assess cycling behavior and parental attitudes toward cycling). Because the original sample size in each study arm was not reported, it was not possible to calculate total attrition in the 2 relevant study arms nor differential attrition. Analyses were conducted on children with data at all time points |
| Selective reporting | Unclear risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Although a physical activity outcome was measured and reported completely, it did not align with those analyzed in this review |
| Recruitment bias | Unclear risk | Judgment comment: it is unclear whether children were recruited before or after randomization |
| Baseline imbalance | Unclear risk |
Quote: "...there were no significant differences in SES [socioeconomic status] levels between the three schools and all three school were within the same region" (Ducheyne 2014b, p 59) Judgment comment: among participating children, significance testing does not appear to have been done. However, weight status and SES appear to be somewhat high among children in the child + caregiver arm compared to those in the child‐only arm. Analyses were adjusted for age at baseline and distance from school |
| Loss of clusters | Low risk | Judgment comment: this is not relevant because there was only 1 cluster per arm |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | High risk | Judgment comment: there was only 1 cluster per intervention arm |
Frenn 2013a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to examine the feasibility and initial efficacies of parent‐ and/or child‐focused online interventions and variables correlated with child body mass index percentile change" (quote) Study period: not reported Total number of arms: 4 Description of intervention arms: 1. Both parent and child online condition (child + caregiver); 2. Child online condition (child only); 3. Parent online condition (not eligible); 4. No intervention control (not eligible) Number of clusters per arm: child + caregiver arm: n = 2; child‐only arm: n = 1; parent‐only: n = 2; no intervention control: n = 1 Average cluster size: 10.33 children Sample size justification and outcome used: this was a pilot study. No sample size justification was given and study authors noted that the study was not adequately powered to examine between‐group differences in the 3 primary outcome variables: body mass index (BMI) percentile, physical activity, and dietary fat intake. Using the data collected, study authors calculated the sample sizes needed for future research Unit of allocation: classroom Missing data handling: an on‐protocol analysis was used rather than intention‐to‐treat. All children assigned completed the online program and their data were analyzed in line with the arm to which they were randomized. Nine parents assigned to complete online modules did not. Data for 4 of these dyads were analyzed as if they were assigned to the child‐only arm rather than to the child + caregiver arm. Data for 5 of these dyads were analyzed as if they were assigned to the "usual class control" arm (i.e. no intervention) rather than to the parent‐only arm. Caregivers and children with missing data were not included in the analysis Reported limitations: 1. A large number of caregivers did not respond to the invitation to participate; 2. Requirement of Internet access was a barrier to some caregivers' participation; 3. Some caregivers appeared to be confused regarding the request for their height and weight information and did not provide usable data to calculate caregiver BMI Randomization ratio and stratification: 2:1:2:1; stratification not reported Participant compensation or incentives: children who returned completed consents were entered into a drawing for small gifts, regardless of whether consent was provided or withheld. Child/caregiver dyads were offered US dollar (USD) 25 for completing intervention components or USD 10 for completing only the measures |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although not reporting by intervention arm, study authors did provide additional information on the overall study sample and noted that children were from low‐ and middle‐income households and attended urban schools
Recruitment methods: at one school, the study was explained to parents as they waited for parent‐teacher conferences. In the other 2 schools, the project was explained to students, and packets with return postage were sent home to parents Inclusion criteria: cluster: not reported; participants: child in fifth, seventh, or eighth grade and caregiver Exclusion criteria: not reported Age of participating children at baseline: fifth, seventh, or eighth grade (estimated to be 9 to 14 years old) Total number randomized by relevant group: total across all study arms: n = 62; child + caregiver arm: n = 15; child‐only arm: n = 18 Baseline imbalances between relevant groups: not reported Total number analyzed by relevant group: based on data presented in the CONSORT diagram (which contains inconsistencies): child BMI percentile (child + caregiver arm: n = 2, child‐only arm: n = 14); caregiver BMI (child + caregiver arm: n = 2, child‐only arm: n = 2) Attrition by relevant group: based on data presented in the CONSORT diagram (which contains inconsistencies), attrition rates were calculated by summing those who were lost to follow‐up and, for the child + caregiver arm, those whose parents discontinued participation: child + caregiver arm: 33.3% (5/15); child‐only arm: 16.7% (3/18) Description of sample for baseline characteristics reported above: not reported |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | No end‐of‐intervention data were collected in this study. The following instruments were used to measure outcomes relevant to this review at baseline and 6 to 9 months
|
|
| Identification |
Study name: Project FUN Country: USA Setting: urban schools in the Midwest Types of reports: published journal article Comments: used only 1 report: Frenn 2013b, as well as unpublished information provided by the study authors (Frenn 2018 [pers comm]). The CONSORT diagram includes discrepancies (numbers for analysis and attrition do not add up to total enrollment) Author's name: Marilyn Frenn Email: marilyn.frenn@marquette.edu Conflicts of interest: "the authors report no actual or potential conflicts of interest" (quote) Sponsorship source: Regrier Faculty Award |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Judgment comment: randomization of schools was determined by coin toss. Selection and randomization of classrooms at each school also was determined by coin toss (Frenn 2018 [pers comm]) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: participants were not blinded, and knowledge of the intervention may or may not have influenced children's performance. Because the intervention was delivered online, blinding of personnel is not a concern |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Height and weight were measured. Other relevant outcomes were measured by self‐report. These outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgment comment: based on data presented in the trial's CONSORT diagram (which contains inconsistencies), we calculated attrition rates by summing those who were lost to follow‐up and those whose parents discontinued participation, and dividing this by the number of children randomized. Total attrition was 24.2% for both the study overall (15/62) and the 2 relevant study arms (8/33). Differential attrition for the 2 relevant arms was 16.6% (5/15 vs 3/18) |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Dietary, physical activity, and anthropometric outcomes were reported incompletely and could not be entered into meta‐analysis. We were not able to retrieve relevant data from the study authors |
| Recruitment bias | High risk | Judgment comment: randomization occurred before recruitment |
| Baseline imbalance | Unclear risk | Judgment comment: study authors reported that no significant differences were found between study arms with respect to age, race, gender, or weight status. Between the 2 clusters in the child + caregiver arm, the study authors did not report whether there were similarities or differences |
| Loss of clusters | Low risk | Judgment comment: no clusters were lost (Frenn 2018 [pers comm]) |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | High risk | Judgment comment: of the relevant intervention arms, 1 had 1 cluster and the other had 2. The study authors reported that the sample size was not sufficient to examine between‐group differences in the outcomes of interest. Also, "an on‐protocol analysis was used" (quote; p 69), so if a caregiver in the child + caregiver group did not want to participate in the online program but was willing to complete the assessments, data for the dyad were analyzed with the child‐only data or with data from the no‐intervention control arm |
Haerens 2006a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to evaluate the effects of a middle school physical activity and healthy eating intervention, including an environmental and computer‐tailored component, and to investigate the effects of parental involvement" (quote) Study period: baseline: September 2003; final assessment: May to June 2005 Total number of arms: 3 Description of intervention arms: 1. School‐based intervention with parental support (child + caregiver); 2. School‐based intervention (child only); 3. No intervention control (not eligible) Number of clusters per arm: 5 Average cluster size: 189.33 children Sample size justification and outcome used: to detect a 0.3‐change in body mass index (BMI) and a 10‐minutes‐per‐day change in total physical activity with 80% power and an alpha level of 0.05, 300 children per group were needed. Study authors sought larger samples to account for possible dropout and to support subgroup analyses Unit of allocation: schools Missing data handling: to account for missing data on physical activity outcomes, "intention‐to‐treat analyses were conducted by carrying the last observation forward" (quote). However, the number analyzed differs from the baseline sample, and the reason why is not explained. For BMI and dietary intake analyses, study authors did not report how missing data were handled. In data provided by the study authors, the distinct sample sizes used to assess baseline to 1‐year outcomes vs baseline to 2‐year outcomes suggest that data were analyzed based on matched pairs Reported limitations: 1. Randomization at the school level may have contributed to clustering of outcomes (but this was considered in analyses); 2. Considerable gender differences were evident across study arms (accounted for in analyses); 3. Intervention period was too short to observe sustained behavior change; 4. Accelerometers were used only in a subsample of seventh graders; 5. Quality of implementation and parental involvement was not objectively evaluated; 6. It was not possible to isolate the effects of specific intervention components; 7. After 2 school years, there was a relatively high percentage of dropouts (25%); 8. Self‐reported diet and physical activity measures are subject to reporting errors Randomization ratio and stratification: 1:1:1; stratification not reported Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: to obtain a sample of 15 of the 65 Flemish technical and vocational schools in West Flanders, Belgium, the research team contacted principals of 23 of the schools by phone; 8 declined participation. Following phone contact, principals were sent more information by mail, and a meeting with the research team was arranged. Parents of all seventh and eighth grade students in the 15 participating schools received an informed consent form to provide authorization for their child to participate in measurements Inclusion criteria: cluster: random sample of 15 of the 65 schools with technical and vocational education in West Flanders, Belgium; participants: seventh or eighth grade students and caregivers Exclusion criteria: not reported Age of participating children at baseline: seventh to eighth grade (estimated to be 11 to 14 years old) Total number randomized by relevant group: total across all study arms: n = 2840; child + caregiver arm: n = 1194, child‐only arm: n = 911 Baseline imbalances between relevant groups: at baseline, no significant differences were reported between study arms Total number analyzed by relevant group: the number analyzed differs for each measure. Data provided by the corresponding author: total kcal at 9‐month assessment (child + caregiver arm: n = 1070, child‐only arm: n = 678) and at end of intervention (child + caregiver arm: n = 902, child‐only arm: n = 635); % kcal from fat at 9‐month assessment (child + caregiver arm: n = 970, child‐only arm: n = 563) and at end of intervention (child + caregiver arm: n = 738, child‐only arm: n = 514); fruit intake at 9‐month assessment (child + caregiver arm: n = 1064, child‐only arm: n = 691) and at end of intervention (child + caregiver arm: n = 902, child‐only arm: n = 580); soft drink intake at 9‐month assessment (child + caregiver arm: n = 1087, child‐only arm: n = 660) and at end of intervention (child + caregiver arm: n = 934, child‐only arm: n = 595); water intake at 9‐month assessment (child + caregiver arm: n = 1086, child‐only arm: n = 660) and at end of intervention (child + caregiver arm: n = 932, child‐only arm: n = 595); total physical activity at 9‐month assessment (child + caregiver arm: n = 1081, child‐only arm: n = 676) and at end of intervention (child + caregiver arm: n = 883, child‐only arm: n = 632); MVPA and light physical activity at 9‐month assessment (child + caregiver arm: n = 70, child‐only arm: n = 52) and at end of intervention (not reported or provided for relevant study arms); BMI Z score at 9‐month assessment (child + caregiver arm: n = 1127, child‐only arm: n = 882) and at end of intervention (child + caregiver arm: n = 980, child‐only arm: n = 768); prevalence of overweight/obesity at 9‐month assessment (child + caregiver arm: n = 1129, child‐only arm: n = 888) and at end of intervention (child + caregiver arm: n = 1080, child‐only arm: n = 907) Attrition by relevant group: attrition rates were calculated by dividing the number of children missing data at the assessment time point by the number of children randomized with consent. Rates differed by outcomes and are based on unpublished information provided by the study authors. Dietary outcomes, 9‐month assessment: child + caregiver arm: 11.6% (139/1194), child‐only arm: 24.8% (226/911), end of intervention: not reported or provided by relevant study arms; self‐reported physical activity, 9‐month assessment: child + caregiver arm: 9.4% (70/1194), child‐only arm: 7.4% (68/911), end of intervention: not reported or provided by relevant study arms; accelerometers: not reported or provided by relevant study arms; BMI, 9‐month assessment: child + caregiver arm: 7.0% (78/1194), child‐only arm: 8.0% (73/911), end of intervention: child + caregiver arm: 18.7% (223/1194), child‐only arm: 20.0% (182/911) Description of sample for baseline characteristics reported above: for female, age, socioeconomic status: children with parental consent and baseline data (child + caregiver arm: n = 1194; child‐only arm: n = 911); child diet: (child + caregiver arm: n = 1055; child‐only arm: n = 685) (Haerens 2007a); total physical activity: (child + caregiver arm: n = 1124; child‐only arm: n = 843) (Haerens 2007b) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | All data used in this systematic review were provided by the study authors. The following instruments were used to measure outcomes relevant to this review at baseline, 9 months, and 21 months (end of intervention)
|
|
| Identification |
Study name: not reported Country: Belgium Setting: schools with technical and vocational education in West Flanders, Belgium Types of reports: published journal articles Comments: used the following reports: (1) Haerens 2006b, (2) Haerens 2006c, (3) Haerens 2007a, and (4) Haerens 2007b, as well as unpublished information provided by the corresponding author (Haerens 2019 [pers comm]) Author's name: Leen Haerens Email: leen.haerens@ugent.be Conflicts of interest: "the author(s) declare that they have no competing interests" (quote) Sponsorship source: Policy Research Centre Sport, Physical Activity and Health, funded by the Flemish government |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk |
Quote: "...schools were then randomly assigned to the intervention or control conditions..." (Haerens 2007b, p 259)…" Judgment comment: randomization was computer generated (Haerens 2019 [pers comm]) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged 11 to 14 years, and their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Height and weight were measured. Dietary outcomes were measured by self‐report, and physical activity was measured by accelerometer. Body mass index (BMI) and dietary outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk |
Judgment comment: we calculated attrition rates by dividing the number of children missing data at the assessment time point by the number of children randomized with consent. Rates differed by outcomes and are based on unpublished information provided by the study authors (Haerens 2019 [pers comm]). At the midpoint assessment, total attrition in the relevant study arms was 17.3% (365/2105) for dietary outcomes, 6.6% (138/2105) for self‐reported total physical activity, and 7.2% (151/2105) for BMI. Differential attrition was 13.2% (139/1194 vs 226/911) for dietary outcomes, 2.0% (70/1194 vs 68/911) for self‐reported total physical activity, and 1.0% (78/1194 vs 73/911) for BMI. Data on attrition in the relevant study arms were not available for accelerometer‐assessed outcomes; however, study authors noted that of the 258 children chosen for accelerometry assessment, the parents of 22 children withheld permission and data were missing for 24 children at baseline and for 21 children at the 1‐year assessment. At the end‐of‐intervention assessment, attrition was not available for the relevant study arms for any outcome except BMI. For BMI, total attrition for the relevant study arms was 19.2% (405/2105) and differential attrition was 1.3% (223/1194 vs 182/911) At each time point and for each outcome, analyses were conducted on matched paired data, reducing the sample sizes. At the end‐of‐intervention assessment, “Drop‐out analyses comparing baseline characteristics of pupils participating and not participating at follow‐up showed few significant differences…Pupils not participating at follow‐up were significantly older and consumed significantly more soft drinks then pupils participating at follow‐up” (quote; Haerens 2006b, p 916) |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Dietary, physical activity, and anthropometric outcome data were provided by the study authors in a format that could be entered into meta‐analysis. However, some physical activity outcome data could not be retrieved for the end‐of‐intervention assessment and could not be entered into the meta‐analysis |
| Recruitment bias | Unclear risk | Judgment comment: it is unclear whether participants were recruited to the trial after schools (clusters) had been randomized |
| Baseline imbalance | Unclear risk | Judgment comment: significant baseline differences were not reported, but the child + caregiver arm appeared to have had more girls and fewer participants from lower socioeconomic status households than the child‐only arm. However, "analyses were adjusted for baseline values, age, and socio‐economic status" (quote; Haerens 2006c, p 850). The study authors did not report on similarities and differences between clusters |
| Loss of clusters | Low risk | Judgment comment: no clusters were lost |
| Incorrect analysis | Low risk | Quote: "linear mixed models on 1‐ and 2‐year post‐intervention values, with intervention assignment and gender entered as factors, were used to evaluate the intervention effects. School was nested within condition to take into account school variance" (quote; Haerens 2006c, p 850) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Hopper 1992a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to compare the effect of including versus not including a family‐participation component in a school‐based program to develop children's heart‐healthy exercise and nutrition habits" (quote) Study period: baseline data collection: January 18, 1990; final assessment: April 3, 1990 Total number of arms: 3 Description of intervention arms: 1. School‐ and home‐based condition (child + caregiver); 2. School‐only condition (child only); 3. No intervention control (not eligible) Number of clusters per arm: 2 Average cluster size: 22 children Sample size justification and outcome used: not reported Unit of allocation: class Missing data handling: children with missing data on dietary outcomes were excluded from the analysis Reported limitations: 1. Observed associations may be attributable to demographic or environmental differences between classes; 2. Effect of parental involvement may be confounded by intervention rewards; 3. There was no control group to assess changes in parental outcomes Randomization ratio and stratification: 1:1:1; stratified by class (fifth grade, sixth grade) Participant compensation or incentives: for the child + caregiver arm, participating family members received a t‐shirt. Families also received weekly points for completing nutrition and exercise activities. Stickers and other incentives were awarded weekly, contingent on family participation |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: overall recruitment methods were not reported. However, parents of children assigned to the child + caregiver arm were contacted by letter and phone and were invited to a baseline assessment session and orientation meeting Inclusion criteria: cluster: not reported; participants: fifth or sixth grade students and caregivers Exclusion criteria: not reported Age of participating children at baseline: fifth to sixth grade (estimated to be 9 to 12 years old) Total number randomized by relevant group: total across all study arms: n = 132; child + caregiver arm: n = 45; child‐only arm: n = 43 Baseline imbalances between relevant groups: no significant differences in any of the individual measured variables were observed between the child + caregiver arm and the child‐only arm Total number analyzed by relevant group: dietary intake (n = 43 child + caregiver arm, n = 41 child‐only arm) Attrition by relevant group: attrition rates were calculated by dividing the number of children missing data at the post‐test assessment by the number of children assigned to the intervention arm (all of whom have baseline data): child + caregiver arm: 4.4% (2/45); child‐only arm: 4.7% (2/43). This calculation was based on unpublished information provided by the study authors Description of sample for baseline characteristics reported above: children with data for both baseline and endpoint assessments; caregivers with baseline data (child + caregiver arm, n = 9; child‐only arm, data not collected) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | All data used in this systematic review were provided by the study authors. The following instruments were used to measure outcomes relevant to this review at baseline and at 2.5 months (end of intervention)
Data for caregivers' dietary intake also were collected but could not be used for this review because data were collected only from caregivers in the child + caregiver arm and not from those in the child‐only arm |
|
| Identification |
Study name: not reported Country: USA Setting: primary schools in California Types of reports: published journal article Comments: used only 1 report: Hopper 1992b, as well as unpublished information provided by the study authors (Gruber 2018 [pers comm]) Authors' names: Chris A Hopper and Mary B Gruber Email: chris.hopper@humboldt.edu and mary.gruber@humboldt.edu Conflicts of interest: not reported Sponsorship source: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Judgment comment: study authors confirmed that classes were randomly assigned to 1 of 3 treatment conditions. Classes were block‐randomized by grade, so that each condition had 1 fifth grade and 1 sixth grade class. Randomization was performed manually by drawing teachers' names from a box (Gruber 2018 [pers comm]) |
| Allocation concealment | Low risk | Judgment comment: treatment assignments were made by randomly drawing teachers' names written on slips of paper of equal size (Gruber 2018 [pers comm]) |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged 9 to 12 years, and their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Dietary outcomes were measured by self‐report and may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | Low risk | Judgment comment: we calculated attrition rates by dividing the number of children missing data at the post‐test assessment by the number of children assigned to the intervention arm (all of whom had baseline data). Total attrition in the relevant study arms was 4.5% (4/88) and differential attrition was 0.3% (2/45 vs 2/43). Analyses were conducted on matched paired data (Gruber 2018 [pers comm]) |
| Selective reporting | Unclear risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Dietary and anthropometric outcome data were provided by the study authors in a format that could be entered into meta‐analysis |
| Recruitment bias | Unclear risk | Judgment comment: after receiving consent from teachers, classes were randomly assigned to 1 of 3 treatment conditions. It is unclear whether consent was obtained from participants before or after randomization |
| Baseline imbalance | Unclear risk | Judgment comment: study authors reported that treatment groups did not differ significantly by sex, grade level, age, or any baseline outcome measures. Study authors did not report on similarities and differences between clusters |
| Loss of clusters | Low risk | Judgment comment: no clusters were lost (Gruber 2018 [pers comm]) |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Ievers Landis 2005.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "to provide 1‐year outcomes for a randomized controlled trial of a behavioral−educational intervention for the primary prevention of osteoporosis among 247 preadolescent girls" (quote) Study period: recruitment: August 1998 to December 2000; post‐test assessment: December 1999 to May 2001 Total number of arms: 3 Description of intervention arms: 1. Behavioral intervention for girls and their mothers (child + caregiver); 2. Behavioral intervention for girls (child only); 3. No intervention control (not eligible) Number of clusters per arm: total: 30; not reported per study arm Average cluster size: 13.17 children Sample size justification and outcome used: power calculations appear to have been conducted post‐hoc. The trial authors reported that using the final sample size from the primary outcome paper (n = 247), the intraclass correlation coefficient (ICC) for the calcium outcome, and an effect size of 0.44 for dietary calcium intake and weight‐bearing physical activity, the study had 85% power to detect differences. It is not clear which 2 study arms were compared for the power calculation Unit of allocation: Girl Scout troop Missing data handling: only participants who participated in the baseline and 1‐year assessment and for whom trial authors had complete data were analyzed Reported limitations: 1. Outcomes were measured via self‐report; 2. Study staff were not blinded to study assignment; 3. Sampling issues may have limited the generalizability of the findings Randomization ratio and stratification: 1:1:1, following block randomization (for each sequentially recruited group of 6 troops, random number blocks were used to assign 2 troops to each study arm); stratification not reported Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although not reported by intervention arm, study authors do provide additional information on the overall study sample
Recruitment methods: information about the project was distributed to troop leaders through their service unit directors and the council newspaper. Thirty‐eight eligible troop leaders expressed interest in participating Inclusion criteria: cluster: Girl Scout troop of Lake Erie Council with at least 6 girls that met the age criteria; participants: preadolescent girls aged 8 to 11 years who had not yet undergone menarche and caregivers Exclusion criteria: history of cancer, severe asthma requiring steroid treatment, medical condition that may have influenced bone development, a known disorder of dietary behavior Age of participating children at baseline: 8 to 11 years Total number randomized by relevant group: total across all study arms: n = 395. Samples per arm were not reported and therefore were estimated: child + caregiver arm: n = 563; child‐only arm: n = 563 Baseline imbalances between relevant groups: not reported Total number analyzed by relevant group: child + caregiver arm: n = 94; child‐only arm: n = 73. Numbers may have been lower at some assessments Attrition by relevant group: attrition was not reported and cannot be calculated because study authors did not report the number of children per intervention arm at baseline Description of sample for baseline characteristics reported above: children with baseline physical activity data (child + caregiver arm: n = 94, child‐only arm: n = 71) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | No end‐of‐intervention data were collected in this study. The following instruments were used to measure outcomes relevant to this review at baseline and at 1 year
No information or data were available regarding the 2‐year and 3‐year follow‐up assessments |
|
| Identification |
Study name: Osteoporosis Prevention Project Country: USA Setting: Girl Scout troops in the Lake Erie Council area Types of reports: published journal article Comments: used only 1 report: Ievers Landis 2005. We also identified a second publication related to this study, but it did not provide additional information relevant to this review. Of note, however, the second publication reported a larger number of clusters and a different sample size. We did not receive clarification from study authors on this inconsistency and therefore report only values from the primary outcome paper. Additionally, the study authors noted that “additional assessments were conducted for 2‐ and 3‐year follow‐ups.” (quote) However, we could not locate reports of the findings at these time points Author's name: Carolyn E Ievers‐Landis Email: not reported Conflicts of interest: not reported Sponsorship source: "the study was supported by grant AR‐20618 from the Northeast Ohio Multipurpose Arthritis Center and by the Elizabeth Severance Prentice Foundation, awarded to the principal investigator (C. Kent Kwoh). We also acknowledge support by grant NIH M01‐RR0080 awarded to the General Clinical Research Center" (quote) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Quote: "for each sequentially recruited group of six troops, statistically generated random number blocks were used to assign to troops to each of the three arms..." (p 157) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk |
Quote: "girls, mothers, and troop leaders were masked to their group membership assignment..." (p 158) Judgment comment: however, "due to the nature of the project, there was no masking of the study facilitators or of those assessing the participants" (quote; p 158), and this may or may not have influenced performance |
| Blinding of outcome assessment All outcomes | Unclear risk |
Quote: "...due to the nature of the project, there was no masking of the study facilitators or of those assessing the participants" Judgment comment: physical activity outcomes were assessed using an interviewer‐administered questionnaire and may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgement comment: we calculated attrition rates by dividing the number of children who did not complete the 1‐year assessment by the total sample of eligible girls. Total attrition (including participants in a third “non‐relevant” study arm) was 27.3% (108/395). Because the original sample size in each study arm was not reported, it is not possible to calculate total attrition in the 2 relevant study arms nor differential attrition. In addition to the children who did not complete the 1‐year assessment, an additional 40 girls were dropped from data analysis because of missing data. The final analysis was conducted on the 247 girls with complete data |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Although weight‐bearing physical activity was measured and reported completely, total physical activity was not reported and could not be entered into the meta‐analysis. We were unable to retrieve relevant data from the study authors |
| Recruitment bias | High risk | Judgment comment: recruitment occurred following randomization of Girl Scout troops |
| Baseline imbalance | Unclear risk | Judgment comment: similarities and differences beyond baseline calcium intake and weight‐bearing physical activity between relevant intervention arms and clusters were not reported |
| Loss of clusters | Unclear risk | Judgment comment: study authors did not report whether any clusters were lost |
| Incorrect analysis | Low risk | Quote: "given the high ICC for both of our primary outcomes and for the method of randomization (i.e. cluster‐randomization), HLMs were used in all analyses to control for the clustering at the troop level using [hierarchical linear/logistic models] for Windows 5.05 (Raudenbush, Bryk, & Congdon, 2001)" (p 159 to 160) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Kirks 1982a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to assess the effects of a parent nutrition education program on nutrition education outcomes in young children" (quote) Study period: 1979‐1980 school year Total number of arms: 3 Description of intervention arms: 1. School‐based intervention for children with concurrent parent education (child + caregiver); 2. School‐based intervention for children (child only); 3. No intervention control (not eligible) Number of clusters per arm: 1 Average cluster size: 140.33 children Sample size justification and outcome used: not reported Unit of allocation: school Missing data handling: the number of cases for each outcome differed due to missing data. This suggests that pair‐wise deletion was used rather than list‐wise deletion (i.e. complete case analysis) Reported limitations: 1. Small sample size and non‐random distribution of student ability limits generalizability Randomization ratio and stratification: 1:1:1; effort to match by socioeconomic status, location, quality of teachers and staff, and similarity of resources Participant compensation or incentives: none provided |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: not reported Inclusion criteria: cluster: not reported; participants: kindergarten, first, second, or third grade students and caregivers Exclusion criteria: not reported Age of participating children at baseline: kindergarten to third grade (estimated to be 4 to 9 years old) Total number randomized by relevant group: total across all study arms: n = 421; child + caregiver arm: n = 176; child‐only arm: n = 140 Baseline imbalances between relevant groups: not reported Total number analyzed by relevant group: dietary outcomes (child + caregiver arm: n = 51; child‐only arm: n = 50) Attrition by relevant group: attrition rates were calculated by dividing the number of children without dietary intake data at the post‐test assessment by the number of participating children in each study arm: child + caregiver arm: 71.0% (125/176); child‐only arm: 64.3% (90/140) Description of sample for baseline characteristics reported above: not reported |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 4 months (end of intervention), and 5 years
|
|
| Identification |
Study name: not reported Country: USA Setting: northern California Types of reports: published journal articles Comments: used the following reports: (1) Kirks 1982b, (2) Kirks 1986, as well as unpublished information provided by the study authors (Fischer 2019 [pers comm]) Author's name: Barbara A Kirks Email: not available Conflicts of interest: not reported. However, the study authors noted, "the first author has been the ongoing nutrition consultant for the school district in which our study was done" (quote) Sponsorship source: California State Department of Education |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk |
Quote: "…three schools were matched and randomly assigned to one of three groups" (Kirks 1986, p 203) Judgement comment: however, the method used to generate the random sequence was not reported |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged approximately 4 to 9 years, so their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Dietary intake was reported by caregivers, and outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgment comment: we calculated attrition rates by dividing the number of children without dietary intake data at the post‐test assessment by the number of participating children in each study arm. Total attrition was 35.9% (151/421) for the study overall and 68.0% (215/316) for the 2 relevant study arms. Differential attrition for the relevant study arms was 6.7% (125/176 vs 90/140). Dietary data were not collected at baseline, and analyses considered only children with data at the post‐test assessment (or, for the follow‐up assessment, only children with data at the 5‐year follow‐up time point) |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Fruit intake, vegetable intake, dietary diversity, and dietary quality outcomes were reported incompletely and could not be entered into the meta‐analysis. We could not retrieve relevant data from the study authors |
| Recruitment bias | Unclear risk | Judgment comment: it is unclear whether participants were recruited before or after randomization |
| Baseline imbalance | High risk | Judgment comment: study authors did not report on similarities and differences between intervention arms. However, the study authors noted that one of the classes involved in the study was "exceptional" (quote; Kirks 1982b, p 139), and it would have been better if the treatment groups were truly matched |
| Loss of clusters | Low risk | Judgment comment: this is not relevant because there was only 1 cluster per arm |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | High risk | Judgment comment: only 1 cluster was reported per intervention arm |
Lin 2017a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: this study aims "to evaluate the short‐ and long‐term effects of two behavioral interventions based on the HAPA [Health Action Process Approach] on F&V [fruit and vegetable] intake compared to a ‘no treatment’ control condition. The first intervention only targeted adolescents; while the second intervention also included mothers to investigate the incremental effects of involving family members..." (quote) Study period: September 2015 to March 2016 Total number of arms: 3 Description of intervention arms: 1. Intervention for mothers and children (child + caregiver); 2. Intervention for children (child only); 3. No intervention control (not eligible) Number of clusters per arm: 16 Average cluster size: 58.77 children Sample size justification and outcome used: "power analysis suggested that recruiting 464 participants at baseline in each group (1392 total) would provide 95% power to detect a medium‐sized difference (d = .40) in outcomes between groups, assuming a 10% dropout rate and a design effect of 2.24. With an estimated average class size of 29, students from 48 schools were randomly selected from the 66 eligible schools and invited to participate in the trial" (quote) The outcome used for this analysis was mean fruit and vegetable intake Unit of allocation: high schools Missing data handling: multiple imputation was used to handle missing data Reported limitations: 1. Most outcome measures were developed for this study and have not been validated before; 2. Fruit and vegetable intake was measured using a retrospective, self‐report instrument, and the test‐retest reliability of the instrument was not examined; 3. The findings may not generalize to Western countries due to differences between Eastern and Western cultures; 4. The findings may not generalize to other age groups; 5. Home and school food environments may be important determinants of adolescent fruit and vegetable intake but were not considered in the design of this study Randomization ratio and stratification: 1:1:1; stratified by educational district and gender of students in the schools (no high schools in Iran are mixed‐gender) Participant compensation or incentives: pool tickets were provided as compensation |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: a list of high schools was provided by the Organization for Education in Qazvin. Sixty‐six high schools were identified as potential candidates for recruitment; 48 of these schools were "randomly selected" (quote) and were invited to participate. All schools agreed to participate; 1537 students from these schools were invited to take part in the trial, of whom 1455 (94.7%) agreed. It is not reported how adolescents were recruited within schools Inclusion criteria: cluster: high school in Qazvin that was not already involved with a nutritional program; participant: adolescent attending high school and possessing the ability to understand Persian language Exclusion criteria: cluster: current involvement in a nutrition program; participant: not reported Age of participating children at baseline: 13 to 18 years Total number randomized by relevant group: total across all study arms: n = 215; child + caregiver arm: n = 94; child‐only arm: n = 59 Baseline imbalances between relevant groups: study authors report demographic characteristics of participants in the 3 groups to be "similar"; no significant differences were identified for the following variables: age, mother's education, monthly household income, or sex Total number analyzed by relevant group: "all available data were analyzed" (quote). At the 1‐month follow‐up, this appears to be all adolescents with consent except those lost to follow‐up: child + caregiver arm: n = 502; child‐only arm: n = 456. At the 6‐month follow‐up, this appears to be all adolescents with consent except those lost to follow‐up (as indicated above) plus those who dropped out: child + caregiver arm: n = 493; child‐only arm: n = 449 Attrition by relevant group: attrition rates were calculated by summing the number of adolescents who were lost to follow‐up (by the 1‐month post‐intervention assessment) or dropped out (by the 6‐month assessment) and dividing this number by the total number of consented adolescents: child + caregiver arm: 3.3% (17/510); child‐only arm: 2.8% (13/462) Description of sample for baseline characteristics reported above: consented children (child + caregiver arm: n = 510; child‐only arm: n = 462) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 1 month (end of intervention), and 6 months (follow‐up)
|
|
| Identification |
Study name: not reported Country: Islamic Republic of Iran Setting: high schools in Qazvin, Iran Types of reports: published journal article; trial registration Comments: used the following reports: (1) Lin 2017, and (2) trial registration (Clinicaltrials.gov registration number: NCT02405611), as well as unpublished information provided by Amir Pakpour, the corresponding author (Pakpour 2019 [pers comm]) Author's name: Amir Pakpour Email: apakpour@qums.ac.ir; pakpour_amir@yahoo.com Conflicts of interest: "no potential conflict of interest was reported by the authors" (quote) Sponsorship source: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Quote: "an independent statistician used a computer‐generated list of random numbers to randomise schools to the three arms" (p 1453) |
| Allocation concealment | Low risk | Quote: "an independent statistician used a computer‐generated list of random numbers to randomise schools to the three arms" (p 1453) |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants was provided, and it is unclear whether personnel who delivered the intervention were blinded. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Given that the children were aged 13 to 18 years, their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk |
Quote: "all research assistants and statisticians were blinded to group allocation" (p 1453) Judgment comment: no information on how blinding was done was reported. Although fruit and vegetable intake was self‐reported by adolescents, the reports were checked against parental reports of intake and the level of agreement was found to be "fair" (quote; p 1456). These data may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | Low risk | Judgment comment: we calculated attrition rates by dividing the number of dropouts and participants lost to follow‐up by the number of participating children at baseline. Total attrition was 2.9% (42/1455) for the study overall and 3.1% (30/972) for the 2 relevant study arms. Differential attrition for the 2 relevant study arms was 0.5% (17/510 vs 13/462) |
| Selective reporting | Low risk | Judgment comment: the trial was registered. Expected outcomes were pre‐specified and were addressed in the article |
| Recruitment bias | Low risk | Quote: "after baseline assessment, the participating schools were randomly allocated…" (p 1452) |
| Baseline imbalance | Unclear risk | Judgment comment: study authors report that the following characteristics were "similar" (quote; p 1457) across study arms: age, mother's education, monthly household income, sex, number of classes, and average number of students in the classes. Whether there were differences between clusters of the same arm is not reported |
| Loss of clusters | Low risk | Judgment comment: no clusters were lost (Pakpour 2019 [pers comm]) |
| Incorrect analysis | Low risk | Quote: "several mulilevel linear mixed models with three levels (clustered in schools and repeated measures in person) were used to examine the efficacy of the intervention(s)" (p 1457) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: no other sources of bias were detected |
Luepker 1996a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "to assess the outcomes of health behavior interventions, focusing on the elementary school environment, classroom curricula, and home programs, for the primary prevention of cardiovascular disease" (quote) Study period: the Child and Adolescent Trial for Cardiovascular Health (CATCH) II (trial): data collection start date: fall 1991; data collection end date: spring 1994; CATCH III (follow‐up study): first follow‐up: spring 1995; final follow‐up: spring 1997 Total number of arms: 3 Description of intervention arms: 1. School‐based program plus a family‐based program (child + caregiver); 2. School‐based program (child only); 3. No intervention control (not eligible) Number of clusters per arm: child + caregiver arm: n = 28 (7 per field center); child‐only arm: n = 28 (7 per field center); no intervention control arm: n = 40 (10 per field center) Average cluster size: 53.19 children Sample size justification and outcome used: a power of 92% to detect a 0.13‐mmol/L (5.1‐mg/dL) mean difference in serum cholesterol concentration between intervention arms together (child + caregiver arm and child‐only arm) and the “control” arm. Power calculations assumed a standard deviation of 28 mg/dL and were performed for a 1‐sided type I error rate of 0.025. Study authors estimated that each school would have 4 classes of 25 students each, and that approximately 20% of students would refuse consent. As noted above, the primary individual outcome was serum cholesterol concentration. There also were 2 primary outcomes at the school level: total fat and sodium content of food served in school cafeterias and the amount of physical education time that students spend in MVPA Unit of allocation: school, with each field center contributing equal numbers per arm Missing data handling: individual‐level measurements were done only on children who gave a blood sample at baseline and completed lipid assessment at follow‐up (4019/5106). Children who left the district before the end of the study were tracked within a 100‐mile radius and underwent measurements to enable analysis according to the intention‐to‐treat principle Reported limitations: 1. The study may not have been adequately powered for a population intervention given the ambitious targeted endpoint for differential changes in blood cholesterol between conditions; 2. Participation rates in blood draws were moderate; 3. The intensity of the intervention was limited by the public school context; 4. The intervention did not encompass other community stakeholders and dimensions that may influence children’s health behaviors Randomization ratio and stratification: 7:7:10 Participant compensation or incentives: in the child + caregiver arm, small rewards were used as participation incentives |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although not reporting by intervention arm, study authors do provide additional information on the overall study sample
Recruitment methods: the study team sent school district superintendents a letter describing the project and inviting their district to participate. This was usually followed by a meeting between a school district representative, one of the principal investigators, and the site intervention co‐ordinator, at which a brief video about CATCH was shown and the study was described. Schools were recruited based on their distance to one of the study centers, ethnic diversity, food service potential for intervention, commitment to offering at least 90 minutes of physical education per week, and willingness to be randomly assigned to treatment or control Inclusion criteria: cluster: school following recruitment outlined below; participant: third grade students and caregivers Exclusion criteria: not reported Age of participating children at baseline: third grade (estimated to be 7 to 9 years old) Total number randomized by relevant group: cohort for the trial was defined as the 5106 children who provided total cholesterol measurement at baseline; child + caregiver arm: n = 1506; child‐only arm: n = 1483 Baseline imbalances between relevant groups: there were no significant differences by condition at baseline for any of the relevant variables Total number analyzed by relevant group: the number analyzed differs for each measure. The total number analyzed for diet and anthropometric measures relate to change data. The total number analyzed for physical activity and sedentary time measures relate to data available for that time point (no baseline data available). Data were provided by the corresponding author: child total kcal intake; % total energy intake from fat; % total energy intake from saturated fat; % total energy intake from carbohydrate; % total energy intake from protein; sodium intake at end of intervention (child + caregiver arm: n = 353; child‐only arm: n = 356) and at 5.5‐year follow‐up (child + caregiver arm: n = 406; child‐only arm: n = 378); water intake at end of intervention (child + caregiver arm: n = 85; child‐only arm: n = 97) and at 5.5‐year follow‐up (not reported or provided for relevant study arms); total PA, MVPA, light PA, and sedentary behavior at end of intervention (child + caregiver arm: n = 1032; child‐only arm: n = 1016), at 3.5‐year follow‐up (child + caregiver arm: n = 1255; child‐only arm: n = 1257), at 4.5‐year follow‐up (child + caregiver arm: n = 1258; child‐only arm: n = 1245), and at 5.5‐year follow‐up (child + caregiver arm: n = 1092; child‐only arm: n = 1063); BMI Z score at end of intervention (child + caregiver arm: n = 1177; child‐only arm: n = 1176) and at 5.5‐year follow‐up (child + caregiver arm: n = 1081; child‐only arm: n = 1061); prevalence of overweight/obesity at end of intervention (child + caregiver arm: n = 1185; child‐only arm: n = 1181) and at 5.5‐year follow‐up (child + caregiver arm: n = 1092; child‐only arm: n = 1071) Attrition by relevant group: overall: 78.7% (4019/5106); child + caregiver arm: 78.7% (1185/1506); child‐only arm: 79.6% (1181/1483). Note: the attrition rate for the primary outcome (total cholesterol) was higher than the general attrition rate (provided here) Description of sample for baseline characteristics reported above: data on diet, physical activity, and anthropometric characteristics were provided by the corresponding author: total kcal, % energy intake from fat, % energy intake from saturated fat, % energy intake from carbohydrate, % energy intake from protein, sodium intake (child + caregiver arm: n = 400; child‐only arm: n = 558), water intake (child + caregiver arm: n = 170; child‐only arm: n = 156), BMI Z score (child + caregiver arm: n = 1481; child‐only arm: n = 1501), prevalence of overweight/obesity (child + caregiver arm: n = 1506; child‐only arm: n = 1483). The sample for other measures includes all 5106 children enrolled in the study |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | All data used in this systematic review were provided by the study authors The following instruments were used to measure outcomes relevant to this review at baseline, 2.5 years (end of intervention), and 5.5 years (follow‐up)
The following instruments were used to measure outcomes relevant to this review at 2.5 years (end of intervention), 3.5 years (follow‐up), 4.5 years (follow‐up), 5.5 years (follow‐up)
|
|
| Identification |
Study name: Child and Adolescent Trial for Cardiovascular Health (CATCH) Country: USA Setting: primary schools in cities in 4 geographically diverse states: San Diego, California; New Orleans, Louisiana; Minneapolis, Minnesota; and Austin, Texas Types of reports: published journal articles Comments: multi‐site trial with large collaborative group and multiple principal investigators. Used the following reports: (1) Luepker 1996b; (2) Lytle 1994; (3) Lytle 1996; (4) Nader 1996; (5) Nader 1999; (6) Perry 1992; (7) Perry 1997; and (8) Zucker 1995, as well as unpublished information provided by Henry Feldman, the senior project statistician (Feldman 2018 [pers comm]) Author's name: Henry A Feldman Email: henry.feldman@childrens.harvard.edu Conflicts of interest: not reported Sponsorship source: National Heart, Lung and Blood Institute of the National Institutes of Health |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Judgment comment: trial authors took the list of 24 enrolled schools at each site and attached a computer‐generated random number to each school (unpublished information provided by trial authors) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Although children began the intervention in the third grade, given the duration of the intervention and follow‐up assessments, their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Dietary intake was reported by 24‐hour recall, physical activity was self‐reported, and height and weight were measured. Given the self‐reported nature of diet and physical activity data, these outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgment comment: trial authors defined the CATCH cohort as those with a total cholesterol measurement at baseline (n = 5106). Following their guidance, we calculated attrition rates by dividing the number of children with data at the fifth grade assessment by the number of children in the CATCH cohort. Rates differed by outcomes and are based on unpublished information provided by the study authors. Total attrition (general for the study) was 21.3% (1087/5106) for the study overall and 20.8% (623/2989) for the two relevant study arms. Differential attrition in the 2 relevant study arms was 0.9% (321/1506 vs 302/1483). For total cholesterol, the primary endpoint, total attrition was 22.9% (1170/5106) for the study overall and 22.7% (678/2989) for the 2 relevant study arms. Differential attrition in the 2 relevant study arms for total cholesterol was 1.7% (354/1506 vs 324/1483). For BMI Z score, total attrition was 21.3% (636/2989) for the 2 relevant study arms, and differential attrition in the 2 relevant study arms was 1.1% (329/1506 vs 307/1483). For prevalence of overweight and obesity, total attrition was 20.8% (623/2989) for the 2 relevant study arms, and differential attrition in the 2 relevant study arms was 0.9% (321/1506 vs 302/1483). For physical activity, total attrition was 31.5% (941/2989) for the 2 relevant study arms, and differential attrition in the 2 relevant study arms was 11.0% (474/1506 vs 486/1483). For dietary outcomes, data were collected from “a random subsample of 30 students per school at both baseline and follow‐up” (quote; Luepker 1996a, p 770); thus attrition was not calculated. Analyses were restricted to children with paired data. Sensitivity analyses were planned to address issues of missing data, but the approach used was not reported and may have differed between different analyses |
| Selective reporting | Low risk | Judgment comment: outcomes for this large trial were specified and published a priori. Dietary, physical activity, and anthropometric outcome data were provided by the study authors in a format that could be entered into meta‐analysis |
| Recruitment bias | Low risk | Quote: "randomization occurred after all baseline measurements were completed" (Luepker 1996b, p 769) |
| Baseline imbalance | Unclear risk |
Quote: "among the 96 schools measured at baseline, there were no significant differences in the study conditions for all relevant variables, including environmental, behavioral, psychosocial, and risk factor data, ensuring equivalency among groups" (Luepker 1996b, p 771) "...there were no significant differences in nutrient intake by treatment group at baseline" (Lytle 1996, p 468) Judgment comment: study authors did not report on similarities or differences between clusters |
| Loss of clusters | Low risk | Quote: "all 96 schools maintained their participation in their allocated treatment condition during the 3‐year study period" (Luepker 1996b, p 771) |
| Incorrect analysis | Low risk | Quote: “individual‐level measures were analyzed by mixed‐model analysis of covariance (ANCOVA) with the follow‐up value as the dependent variable, the CATCH intervention group as the independent variable, and the baseline value as a covariate... School‐level measures were analyzed by repeated measures ANCOVA with the CATCH intervention group as the independent variable" (Luepker 1996b, p 770) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Perry 1988a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: to compare the efficacy of a school‐based program vs a home‐based program on elementary students' dietary fat and sodium intake Study period: baseline data collection: spring of 1985 (second grade); post‐test data collection (third grade): spring of 1986 Total number of arms: 4 Description of intervention arms: 1. School‐based program plus a home‐based program (child + caregiver); 2. School‐based program (child only); 3. Home‐based program (not eligible); 4. No intervention control (not eligible) Number of clusters per arm: child + caregiver arm: n = 8; child‐only arm: n = 8; home‐based arm: n = 8; no intervention control arm: n = 7 Average cluster size: 72.58 children Sample size justification and outcome used: not reported Unit of allocation: school Missing data handling: not reported Reported limitations: 1. The 24‐hour dietary recall method is known to have high variability and can be subject to response bias; 2. The Home Team intervention (administered to families in the child + caregiver arm) requires investigation with a longer follow‐up period, with other behaviors, with other socioeconomic groups, and with differing age groups; 3. This study was conducted in predominantly well‐educated, white, middle‐class communities in Minnesota and North Dakota, and the findings may not be generalizable to other groups Randomization ratio and stratification: ˜ 1:1; schools were blocked by state and were randomized to 1 of the 4 conditions Participant compensation or incentives: in the child + caregiver arm, hats, magnifying glasses, and stickers were used as participation incentives. Families who completed the program also were eligible to win a trip to Disneyworld |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although study authors do not report data on race/ethnicity or household income/socioeconomic status by intervention arm, they note, "The study population was predominantly Caucasian and middle class" (quote) Recruitment methods: not reported Inclusion criteria: cluster: elementary school in 4 urban public school districts in Minnesota and North Dakota; participant: child enrolled in second grade at a participating school and caregiver Exclusion criteria: not reported Age of participating children at baseline: second grade (estimated to be 6 to 8 years old) Total number randomized by relevant group: total across all study arms: n = 2250 second grade students at participating schools. Samples per arm were not reported and therefore were estimated: child + caregiver arm: n = 563; child‐only arm: n = 563 Baseline imbalances between relevant groups: significant differences were not reported Total number analyzed by relevant group: at each time point, 30 children at each school were selected randomly to provide an overnight urine sample and 15 additional children at each school were selected randomly to provide a urine sample plus 24‐hour dietary recall. Diet data relevant to this review are based on the samples that provided urine plus 24‐hour dietary recall data. At post‐test: child + caregiver arm: n = 77; child‐only arm: n = 68 Attrition by relevant group: not reported, and cannot be calculated for each relevant arm Description of sample for baseline characteristics reported above: children with baseline and post‐test data; total: n = 1839; child + caregiver arm: n = 512; child‐only arm: n = 391 |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | No end‐of‐intervention data were collected in this study. The following instruments were used to measure outcomes relevant to this review at baseline, 1‐year (follow‐up), and 2‐year (follow‐up) time points
The following instruments were used to measure outcomes relevant to this review at baseline and at the 1‐year follow‐up time point
|
|
| Identification |
Study name: Minnesota Home Team Country: USA Setting: urban schools in Minnesota and North Dakota Types of reports: published journal articles Comments: used 4 reports: (1) Crocket 1989; (2) Luepker 1988; (3) Perry 1988b; and (4) Perry 1989, as well as information provided by co‐investigator, Russell Luepker (Luepker [pers comm]) Author's name: Cheryl L Perry Email: cheryl.l.perry@uth.tmc.edu Conflicts of interest: not reported Sponsorship source: National Heart, Lung, and Blood Institute of the National Institutes of Health |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk |
Quote: "…schools were blocked by state and randomly assigned to one of four conditions" (Perry 1988b, p 1156) Judgment comment: however, the method used to generate the random sequence was not reported |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged approximately 6 to 8 years, so their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: there was no information on blinding of outcome assessors. Dietary intake was reported by an interviewer‐administered 24‐hour recall, and outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | Unclear risk |
Quote: "participation rates were notably high for all aspects of the study" (Perry 1988b, p 1158) Judgment comment: when all 4 intervention arms were considered together, "participation rates for the school survey and anthropometric measures were greater than 93 percent for all measures at both pretest and posttest" (quote; Perry 1988b, p 1158). However, the study authors did not report attrition rates by intervention arm, and we could not calculate these because a randomly selected subset of children completed the 24‐hour dietary recalls at each data collection time point |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Dietary outcomes were reported incompletely or for merged study arms, or were not reported for all study time points. The only outcome we extracted for this review was sodium intake at the 1‐year follow‐up assessment. We were unable to retrieve additional outcome data from the study authors. Therefore, not all outcome data could be entered into meta‐analysis |
| Recruitment bias | Unclear risk | Judgment comment: study authors did not describe recruitment or consent. However, they noted that "the assigned education program was given to all third grade students who were enrolled in the participating schools" (quote; Perry 1988b, p 1157), and that "at each survey time, students enrolled in the appropriate grade in all 31 schools took part in the school surveys..." (quote; Perry 1988b, p 1158) |
| Baseline imbalance | Unclear risk | Judgment comment: not reported; however, the distribution of female:male students was similar across study arms, as was the distribution of children by age, height, and weight |
| Loss of clusters | High risk |
Judgment comment: 1 cluster (school) dropped out of the study after randomization Quote: "one school in one school district withdrew from the study due to commitments to a previously developed nutrition education program" (Perry 1988b, p 1156) |
| Incorrect analysis | Low risk | Quote: "to avoid such bias, design effects were estimated based on the observed intraclass correlation coefficients drawn from the data. These design effects were then used to adjust the mean‐square‐error terms in the ANOVAs to reflect properly any intraschool dependence in the data. Although this procedure provides only an approximation of the true intraclass correlation coefficients, it is far better than ignoring this potential source of bias" (Luepker 1988, p 238) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: study authors noted that self‐reported outcome measures are typically subject to response bias. However, "if this were true, the effect on the behavior index would be equivalent across all three treatment conditions, which was not the case" (quote; Perry 1988b, p 1159). We detected no other sources of bias |
Petchers 1987.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: " ... to test the impact of the Chicago Heart Healthy curriculum on pre‐adolescent students" and "to evaluate the efficacy of a parent‐participation component in conjunction with the student curriculum" (quote) Study period: 1982‐1983 school year Total number of arms: 3 Description of intervention arms: 1. School‐based curriculum with parent participation (child + caregiver); 2. School‐based program (child only); 3. No intervention control (not eligible) Number of clusters per arm: child + caregiver arm: n = 9; child‐only arm: n = 8; no intervention control arm: n = 9 Average cluster size: cannot be calculated Sample size justification and outcome used: not reported Unit of allocation: school Missing data handling: the number of cases for each outcome variable differed due to missing data. This suggests that pair‐wise deletion was used rather than list‐wise deletion (i.e. complete case analysis) Reported limitations: not reported Randomization ratio and stratification: 1:1:1, but 3 schools were guaranteed random assignment to the child + caregiver or child‐only arm because they participated in a heart‐health education project the previous year. Stratification was not reported Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although not reporting by intervention arm, study authors do provide additional information on the overall study sample
Recruitment methods: not reported Inclusion criteria: cluster: unclear sampling approach, but schools were from 5 school districts in northeast Ohio (2 rural, 1 suburban, 2 residential urban); participants: sixth grade students and caregivers Exclusion criteria: not reported Age of participating children at baseline: sixth grade (estimated to be 10 to 12 years old) Total number randomized by relevant group: the number of children randomized was not reported overall or by study arm. The total number reflects children who completed the study. The sample by study arm was estimated from this total. Across all study arms: n = 647; child + caregiver arm: n = 162; child‐only arm: n = 162 Baseline imbalances between relevant groups: not reported Total number analyzed by relevant group: not reported Attrition by relevant group: attrition was not reported and cannot be calculated because study authors did not report the number of children per intervention arm at baseline Description of sample for baseline characteristics reported above: not reported |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline and post‐test
Of note, study authors did not analyze all of the child + caregiver data together because some of the caregivers did not participate. However, this does not impact the findings of the present systematic review because this trial did not contribute any data |
|
| Identification |
Study name: not reported Country: USA Setting: schools in northeast Ohio Types of reports: published journal article Comments: used 1 report only: Petchers 1987 Author's name: Marcia K Petchers Email: not reported Conflicts of interest: not reported Sponsorship source: American Heart Association, Northeast Ohio Affiliate, Inc., and the Schoolsite Committee, with funds granted by the Northeast Ohio Affiliate, the Martha Holden Jennings Foundation, and the Cleveland Foundation |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | High risk | Quote: “…schools were assigned to treatment conditions using modified random assignment strategy…It should be noted that three schools in the sample participated as control groups in a heart health education project the previous year. As a result of their prior participation, they had been guaranteed participation by random assignment in one of the two curriculum conditions…The remaining schools were then randomly assigned to one of the three study conditions so that there were approximately equal numbers of schools in each condition" (p 451) |
| Allocation concealment | High risk | Judgment comment: the method used to conceal the allocation sequence was not described. However, 3 of the schools were guaranteed assignment to the child + caregiver or child‐only arm before randomization |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged approximately 10 to 12 years, and their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: there was no information on blinding of outcome assessors. Because all data were self‐reported by study participants, outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | Unclear risk | Judgment comment: attrition rates were not reported and could not be calculated because study authors did not report the number of children per intervention arm at baseline. The study authors noted that for different analyses, "the number of cases differs due to missing data" (quote; p 456) |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Although dietary and physical activity outcomes were measured, they were reported incompletely and did not align with outcomes analyzed in this review |
| Recruitment bias | Unclear risk | Judgment comment: study authors did not specify if the children were recruited before or after the schools were randomized |
| Baseline imbalance | Unclear risk | Judgment comment: study authors did not report on similarities and differences between intervention arms or clusters |
| Loss of clusters | Unclear risk | Judgment comment: trial authors did not report whether any clusters were lost |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Vandongen 1995.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "… to assess the impact of the programs on cardiovascular risk factors using a modified factorial design to examine fitness and nutrition programs alone and in combination and to compare the effects of school‐based and home‐based nutrition programs" (quote) Study period: recruitment start: beginning of 1990 school year; data collection end date: end of 1990 school year Total number of arms: 6 Description of intervention arms: 1. School and home nutrition program (child + caregiver); 2. School nutrition program (child only); 3. Fitness program (not eligible); 4. Fitness and school nutrition program (not eligible); 5. Home nutrition program (not eligible); 6. No intervention control (not eligible) Number of clusters per arm: 5 Average cluster size: 38.23 children Sample size justification and outcome used: sample size calculations were based on a pilot study in 10 schools with about 300 children. To detect a 5‐lap difference (standard deviation of 14) in the Leger run, with 80% power, an alpha level of 0.05, and allowance for failure to achieve both baseline and follow‐up measurements in around 20% of children, approximately 150 children per arm were needed. If a class size of 30 children was estimated, 30 schools were required Unit of allocation: school Missing data handling: not reported Reported limitations: 1. Girls who did not attend follow‐up tended to be less fit and to have higher blood pressure at baseline than girls who completed the study; 2. The proportion of children exceeding recommended cholesterol levels is probably underestimated because of the measurement instrument used (Reflotron) Randomization ratio and stratification: 1:1:1:1:1:1; stratified by socioeconomic status (each school was assigned to 1 of 5 socioeconomic strata, based on the Australian Bureau of Statistics ratings of postcodes) Participant compensation or incentives: for the child + caregiver arm, children had to bring completed homework to school and were rewarded. The reward was not described |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: no information on recruitment of study schools was reported. Within the selected schools, a letter explaining the study and seeking consent was sent to the parents of all children enrolled in sixth grade Inclusion criteria: cluster: not reported; participant: sixth grade student and caregiver Exclusion criteria: not reported Age of participating children at baseline: sixth grade (estimated to be 10 to 12 years old) Total number randomized by relevant group: total across all study arms: n = 1147; samples per arm were not reported and therefore were estimated: child + caregiver arm: n = 229; child‐only arm: n = 229 Baseline imbalances between relevant groups: significant between‐group differences were reported for some baseline variables, but study authors did not specify which variables or between which study arms Total number analyzed by relevant group: child + caregiver arm: n = 119; child‐only arm: n = 164 Attrition by relevant group: attrition was not reported and cannot be calculated as study authors did not report the number of children by intervention arm at baseline Description of sample for baseline characteristics reported above: all children with matched paired diet data (child + caregiver arm: n = 119; child‐only arm: n = 164) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline and at 9 months (end of intervention)
Data were analyzed and presented separately for boys and girls. Data also were analyzed by baseline level of cardiovascular risk |
|
| Identification |
Study name: Western Australian Schools Physical Activity and Nutrition Project (WASPAN) Country: Australia Setting: schools in Perth, Western Australia Types of reports: published journal articles Comments: used the following reports: (1) Vandongen 1995b, and (2) Burke 1996, as well as unpublished information provided by study authors (Gracey 2018 [pers comm]) Author's name: Robert Vandongen; corresponding author Valerie Burke (Gracey) Email: valerie.gracey@optusnet.com.au Conflicts of interest: not reported Sponsorship source: “this study was supported by a Program Grant from the National Health and Medical Research Council (Public Health Research and Development Committee)” (quote) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Judgment comment: within socioeconomic strata, schools were randomly allocated via computer‐generated random numbers (Gracey 2018 [pers comm]) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged 10 to 12 years, and their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk |
Quote: "restricted funding and limited availability of qualified personnel prevented the use of a team of assessors who were blinded to the intervention" (Vandongen 1995b, p 11) Judgment comment: data on dietary intake (our primary outcome) was measured by children's self‐report and may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | Unclear risk |
Quote: “dietary data at follow‐up were obtained from 83% of children, fitness data from 88%, blood pressure data from 96%, cholesterol levels from 96%, and anthropometry from 92%” (Vandongen 1995b, p 11) Judgment comment: however, attrition rates by intervention arm were not reported and could not be calculated because the study authors did not report the number of children by intervention arm at baseline |
| Selective reporting | Unclear risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Following conversions of reported data, we were able to enter them into meta‐analysis |
| Recruitment bias | Unclear risk | Judgment comment: it is unclear whether participants were recruited before or after randomization |
| Baseline imbalance | High risk |
Quote: "…there were significant between‐group differences in some baseline variables" (Vandongen 1995b, p 11) Judgment comment: study authors did not report on similarities and differences between clusters |
| Loss of clusters | Unclear risk | Judgment comment: study authors did not report whether any clusters were lost |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Voll 2013.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to determine whether parental involvement in a physical activity intervention delivered to children in‐school could result in positive behavior change in parents, as measured by increased physical activity and reduced sedentary behavior" (quote) Study period: baseline data collection start: February 2012; post‐test assessment: March 2012 Total number of arms: 2 Description of intervention arms: 1. School‐based screen time tracking with family homework (child + caregiver); 2. School‐based screen time tracking (child only) Number of clusters per arm: not reported Average cluster size: 5.38 children Sample size justification and outcome used: not reported Unit of allocation: school Missing data handling: only participants who completed baseline and post‐test assessments were included in the analysis Reported limitations: 1. Small sample size as a result of difficulties in recruitment and attrition; 2. Failure to collect demographic information; 3. Self‐selected participation Randomization ratio and stratification: not reported Participant compensation or incentives: participating children were entered into a drawing with physical activity−related prizes (e.g. jump ropes, basketballs, volleyballs, frisbees). To thank caregivers for participation, drawings were held for a massage gift certificate and a trigger point foam roller |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although not reporting by intervention arm, study authors did indicate that across the 2 intervention arms, 81% (22/27) of participants were female Recruitment methods: names of elementary schools in the Waterloo Region School District were randomly selected for recruitment. School principals were the first point of contact by phone or email, and this was followed up with a package of study materials and documentation. If the principal declined participation or contact could not be established after 1.5 weeks, another school was selected and contacted. Eight schools agreed to participate. Some schools had more than 1 eligible class (n = 14 classes). The researcher visited each school to give students a 10‐minute presentation on the study and to distribute cover letters and consent forms Inclusion criteria: cluster: school located within the Waterloo Region District School Board; participant: child enrolled in fourth/fifth, fifth, or fifth/sixth grade with a caregiver with a working email address Exclusion criteria: not reported Age of participating children at baseline: fourth to sixth grade (estimated to be 8 to 12 years old) Total number randomized by relevant group: total across all study arms: n = 43; samples per arm were not reported and therefore were estimated: child + caregiver arm: n = 22; child‐only arm: n = 22 Baseline imbalances between relevant groups: no significant differences were reported, but study authors note higher levels of physical activity in the child‐only arm Total number analyzed by relevant group: child physical activity score (child + caregiver arm: n = 11; child‐only arm: n = 5); caregiver physical activity score (child + caregiver arm: n = 12; child‐only arm: n = 6) Attrition by relevant group: attrition rates by intervention arm were not reported and cannot be calculated because study authors did not report the number of children by intervention arm at baseline Description of sample for baseline characteristics reported above: child physical activity score: those who completed measures at baseline and post‐test assessments (child + caregiver arm: n = 11; child‐only arm: n = 5); caregiver physical activity score: those who completed measures at baseline and post‐test assessments (child + caregiver arm: n = 12; child‐only arm: n = 6) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline and at 2 weeks (end of intervention)
|
|
| Identification |
Study name: Determining the "Spread of Effects" of Physical Activity Interventions From Children to Parents/Guardians Country: Canada Setting: primary schools in Waterloo Region, Ontario, Canada Types of reports: Masters thesis Comments: used 1 report only: Voll 2013 Author's name: Jess Voll Email: jess@greo.ca Conflicts of interest: not reported Sponsorship source: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Quote: "each classroom (or school, if more than one class per school wished to participate) was randomly assigned to the treatment or control group using random number generation in Microsoft Excel" (p 47) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: participating parents and children were informed that they would be assigned to 1 of 2 groups; however, the true purpose of the study was concealed until after the intervention. Although outcome data were collected via self‐report, concealment of the study hypothesis may have helped to minimize bias |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Because all data were self‐reported by study participants, outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgment comment: attrition rates by intervention arm were not reported and could not be calculated because the study author did not report the number of children by intervention arm at baseline. Overall, no data were available for 37.2% (16/43) of caregiver‐child dyads; this includes 15 dyads that provided no data and 1 dyad that withdrew data after they were informed of the true intent of the study. Matched baseline and post‐test data were not available for 62.8% (27/43) of children and 58.1% (25/43) of caregivers |
| Selective reporting | Unclear risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Physical activity scores for both children and caregivers were reported in a format that could be entered into meta‐analysis |
| Recruitment bias | Unclear risk | Judgment comment: it is unclear whether randomization occurred before or after recruitment. However, wording provided in the cover letter to caregivers suggests that they may not have been made aware of assignment before consenting to take part in the study |
| Baseline imbalance | Unclear risk | Judgment comment: study authors did not report on similarities and differences between intervention arms or clusters |
| Loss of clusters | High risk | Judgment comment: study authors did not report on whether any clusters were lost. However, given the very small number of participants and the high level of attrition and missing data, it is likely that clusters were lost |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | High risk | Judgment comment: study authors noted that some clusters (i.e. classrooms) had 1 or 2 study participants |
Wang 2007a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "this study used the combination of school education and family education to carry out nutrition education activities. By comparing the effects of different education methods, we (1) analyze the independent role of schools and families, [and] (2) analyze the combined effect of school and family...We followed up the changes of nutrition knowledge, attitude, and practice (KAP) before and after education in accordance with the epidemiological prospective study method" (quote) [Chinese‐English translation] Study period: 1 school term; dates not specified Total number of arms: 3 Description of intervention arms: 1. Nutrition education for children and their parents (child + caregiver); 2. Nutrition education for children (child only); 3. Nutrition education for parents (not eligible) Number of clusters per arm: 1 Average cluster size: 492.33 children Sample size justification and outcome used: to detect a 5% increase in intake of soy‐based food products with a power of 90% and an alpha level of 0.05, approximately 138 children were needed per group. In consideration of clustering, study authors aimed to include 50% more children than required per sample size calculation Unit of allocation: school Missing data handling: missing values were excluded from scoring and statistical analyses Reported limitations: 1. Children may not have fully understood the questionnaire and may not have paid attention, leading to mistakes and missing responses Randomization ratio and stratification: 1:1:1:1; no stratification Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: not reported Inclusion criteria: clusters: elementary school located in Xuzhou City (schools randomly chosen); participant: child enrolled in third, fourth, or fifth grade at a participating school and caregiver Exclusion criteria: not reported Age of participating children at baseline: third to fifth grade (estimated to be 7 to 11 years old) Total number randomized by relevant group: total across all study arms: n = 1477; child + caregiver arm: n = 391; child‐only arm: n = 322 Baseline imbalances between relevant groups: not reported Total number analyzed by relevant group: number analyzed differed by outcome variable but for this review was assessed as the number of children with "behavior" data at the end of the intervention and included the following: total: n = 1091; child + caregiver arm: n = 297; child‐only arm: n = 252 Attrition by relevant group: attrition rates differed by variable but for this review were calculated by dividing the number of children without "behavior" data (which includes the habit of eating breakfast and spending on or consuming various foods) at the end of the intervention by the number of children with data at baseline: child + caregiver arm: 24.0% (94/391); child‐only arm: 21.7% (70/322) Description of sample for baseline characteristics reported above: not applicable |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instrument was used to measure outcomes relevant to this review at baseline and at end of school term (end of intervention)
|
|
| Identification |
Study name: not reported Country: China Setting: elementary schools in Xuzhuo City, China Types of reports: published journal article and Masters thesis Comments: used the following reports: Wang 2007b, as well as a thesis by Zhao 2006 Author's name: Cannan Wang Email: wcnseu@126.com Conflicts of interest: not reported Sponsorship source: Jiangsu Province Preventive Medicine Scientific Research Fund |
|
| Notes | Chinese‐English data extraction was completed by Yuan Chi and Andrew Ying | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged approximately 7 and 11 years, and their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Because data were reported by study participants, outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgment comment: we calculated attrition rates by dividing the number of participating children without behavior data at the end of the intervention by the number of children with data at baseline. Total attrition was 26.1% (386/1477) for the study overall and 22.0% (164/713) for the 2 relevant study arms. Differential attrition for the 2 relevant study arms was 2.3% (94/391 vs 70/322) |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Although dietary outcomes were measured, they did not align with dietary outcomes analyzed in this review |
| Recruitment bias | Low risk | Judgment comment: randomization was carried out after participant recruitment but before baseline data collection |
| Baseline imbalance | Unclear risk | Judgment comment: not reported; however, the distribution of female‐to‐male students was similar across study arms, as was the distribution of children by grade |
| Loss of clusters | Low risk | Judgment comment: no clusters were lost |
| Incorrect analysis | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Werch 2003a.
| Methods |
Study design: randomized controlled trial Study grouping: parallel group Study aim: to examine “(1) the efficacy of a brief, tailored sport‐based consultation alone and in combination with an alcohol preventive consultation and a set of parent print materials, on influencing alcohol consumption, alcohol use risk and protective factors, and exercise habits; and (2) differential effects of the interventions on alcohol use and exercise among drinking and nondrinking youth, to estimate the potential of the strategies as future universal (primary) and selective (secondary) prevention interventions” (quote) Study period: baseline assessment: fall 2001; post‐test assessment: spring 2002 Total number of arms: 3 Description of intervention arms: 1. Sport and alcohol consultation and materials for parents (child + caregiver); 2. Sport and alcohol consultation (child only); 3. Sport consultation (not eligible) Sample size justification and outcome used: not reported Unit of allocation: individual child Missing data handling: not reported Reported limitations: 1. Post‐intervention data collection was limited to 1 assessment 3 months post intervention; 2. Despite use of within‐school random assignment, the child‐only arm had significantly greater negative alcohol consequences than the other arms at baseline; 3. Small sample size; 4. No study arm received no intervention Randomization ratio and stratification: 1:1:1; children were randomized within schools, and schools represented an inner city school, a suburban school, and a rural school Participant compensation or incentives: not reported |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Although not reporting by intervention arm, study authors do provide additional information on the overall study sample
Recruitment methods: not reported Inclusion criteria: participants: eighth grade students at participating school and caregivers Exclusion criteria: child unable to read and understand the baseline data collection instrument Age of participating children at baseline: eighth grade (estimated to be 12 to 14 years old) Total number randomized by relevant group: total across all study arms: n = 454; child + caregiver arm: n = 152; child‐only arm: n = 150 Baseline imbalances between relevant groups: there were no significant differences by condition at baseline, except significantly more adolescents in the child‐only arm had alcohol problems compared to adolescents in the child + caregiver arm Total number analyzed by relevant group: total: n = 444; child + caregiver arm: n = 150; child‐only arm: n = 146 Attrition by relevant group: attrition rates were calculated by dividing the number of dropouts by the number of participating children at baseline: child + caregiver arm: 1.3% (2/152); child‐only arm: 2.7% (4/150) Description of sample for baseline characteristics reported above: children with baseline data: child + caregiver arm: n = 152; child‐only arm: n = 150 |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | No end‐of‐intervention data were collected in this study. The following instrument was used to measure outcomes relevant to this review at baseline and 3 months after the intervention (follow‐up)
|
|
| Identification |
Study name: not reported Country: USA Setting: schools in northeast Florida Types of reports: published journal article Comments: used only 1 report: Werch 2003b, as well as unpublished information provided by the corresponding author (Werch 2018 [pers comm]) Author's name: Chudley Werch Email: cwerch@preventionpluswellness.com Conflicts of interest: not reported Sponsorship source: National Institute on Alcohol Abuse and Alcoholism |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Quote: "students were randomly assigned within schools by computer‐generated numbers..." (p 381) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Unclear risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged 12 to 14 years, and their performance may or may not have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Because physical activity was self‐reported by adolescents, outcomes may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | Low risk | Judgment comment: we calculated attrition rates by dividing the number of dropouts by the number of children of participating children at baseline. Total attrition was 2.2% (10/454) for the study overall and 2.0% (6/302) for the 2 relevant study arms. Differential attrition for the 2 relevant study arms was 1.4% (2/152 vs 4/150) |
| Selective reporting | Unclear risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Physical activity outcomes were reported in a format that could be entered into meta‐analysis |
| Recruitment bias | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Baseline imbalance | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Loss of clusters | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Incorrect analysis | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Comparability with individually randomized trials | Low risk | Judgment comment: not relevant. This was an individually randomized trial |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
Yeh 2018a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "... to determine the following: (1) the weight distribution of [preschoolers] in Head Start facilities in a Midwestern metropolitan area; (2) whether providing nutrition education with [African American preschoolers] and their [caregivers] could establish healthy eating habits, nutrition knowledge, and improve their weight status; and (3) whether replacing refined grain with whole grain products in all school meals could alter blood lipid levels" (quote) Study period: 2008‐2009 academic year Total number of arms: 3 Description of intervention arms: 1. Nutrition education for preschoolers and their caregivers (child + caregiver); 2. Nutrition education for preschoolers (child only); 3. No intervention control (not eligible) Number of clusters per arm: 2 Average cluster size: 33.83 children Sample size justification and outcome used: the sample size was determined based on previous publications regarding the number of students per study arm and by convenience sampling (unpublished information provided by the study authors) Unit of allocation: Head Start center Missing data handling: not reported Reported limitations: 1. Small sample size; 2. Intervention had modest intensity; 3. Did not collect dietary records to validate dietary changes; 4. May not have been adequately powered to detect change; 5. Some teachers or peers refused to try whole grain products in the meal, thereby reducing exposure through role modeling; 6. Children may not have had sufficient access to whole grain products at home; 7. Lack of co‐operation among some food service workers; 8. Short intervention period Randomization ratio and stratification: 1:1:1; stratification not reported Participant compensation or incentives: participants received US dollar (USD) 20 for completing the baseline questionnaire and USD 20 for completing the post‐intervention questionnaire. An additional USD 20 was provided to those who completed the blood sample |
|
| Participants |
Baseline characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
Recruitment methods: study investigators recruited parents during the schools' scheduled parent orientations. The study's goals, benefits and risks, confidentiality procedures, and incentive structure were explained, and parents were invited to consent to take part Inclusion criteria: cluster: participating Head Start program (additional information not provided); participant: child aged 3 to 5 years and a caregiver Exclusion criteria: not reported Age of participating children at baseline: 3 to 5 years (preschool) Total number randomized by relevant group: total across all study arms: n = 203; child + caregiver arm: n = 66, child‐only arm: n = 63. Study authors did not report how many children were enrolled in the randomized classes Baseline imbalances between relevant groups: at baseline, no significant differences were reported between study arms Total number analyzed by relevant group: BMI percentile (child + caregiver arm: n = 54, child‐only arm: n = 47) Attrition by relevant group: attrition rates were calculated as the number of children excluded from analysis divided by the number of children randomized based on unpublished information provided by the authors: child + caregiver arm: 18.2% (12/66); child‐only arm: 23.8% (15/63) Description of sample for baseline characteristics reported above: children with measurements at baseline and post‐test, that is, those included in analyses (child + caregiver arm: n = 54, child‐only arm: n = 47) |
|
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline and at 7 months (end of intervention)
|
|
| Identification |
Study name: Healthy Kids Healthy Lives (HKHL) Country: USA Setting: United Children and Family Head Start programs in Detroit, Michigan Types of reports: published journal article and Masters thesis Comments: used the following reports: (1) Akil 2013, and (2) Yeh 2018b, as well as unpublished information provided by the study authors (Yeh 2018c [pers comm]). For discrepancies between reports, we sought clarification from the study authors Author's name: Yulyu Yeh Email: yyeh@tamu.edu Conflicts of interest: "the authors declare that they have no conflict of interest" (quote) Sponsorship source: Office of the Vice President for Research, Wayne University |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Judgment comment: school names were placed in a bag, and the research co‐ordinator drew names (Yeh 2018c [pers comm]) |
| Allocation concealment | Unclear risk | Judgment comment: methods used to conceal the allocation sequence were not described |
| Blinding of participants and personnel All outcomes | Low risk | Judgment comment: no information on blinding of participants and personnel was provided. However, given the nature of the intervention, there would have been no way to blind participants and personnel. Also, the children were aged 3 to 5 years, so their performance was not likely to have been influenced by lack of blinding |
| Blinding of outcome assessment All outcomes | Unclear risk | Judgment comment: no information on blinding of outcome assessors was provided. Height and weight were measured. Therefore, body mass index (BMI) may or may not have been influenced by lack of blinding |
| Incomplete outcome data All outcomes | High risk | Judgment comment: we calculated attrition rates as the number of children excluded from analysis divided by the number of children randomized, based on unpublished information provided by the study authors. Total attrition was 19.2% (39/203) for the study overall and 20.9% (27/129) for the 2 relevant study arms. Differential attrition for the 2 relevant study arms was 5.6% (12/66 vs 15/63) (Yeh 2018c [pers comm]) |
| Selective reporting | High risk | Judgment comment: the trial was not registered and no protocol was cited that could be retrieved. Anthropometric data were reported in a format that could be entered into meta‐analysis, but dietary outcomes were not reported in a usable format, and we could not retrieve these data from the study authors |
| Recruitment bias | High risk | Judgment comment: randomization was carried out before participant recruitment (Yeh 2018c [pers comm]) |
| Baseline imbalance | Unclear risk | Judgment comment: study authors noted that, at baseline, "there was no difference in BMI among the three groups" (Yeh 2018b, p 555). They did not report on similarities and differences between clusters |
| Loss of clusters | Low risk | Judgment comment: no clusters were lost (Yeh 2018c [pers comm]) |
| Incorrect analysis | High risk | Judgment comment: study authors did not report adjusting for clustering in the analysis and did not report intraclass correlation coefficients (ICCs) |
| Comparability with individually randomized trials | Unclear risk | Judgment comment: information provided was insufficient to permit judgment |
| Other sources of bias | Low risk | Judgment comment: we detected no other sources of bias |
ABC: Activity Begins in Childhood.
ANCOVA: analysis of covariance.
BMI: body mass index.
CATCH: Child and Adolescent Trial for Cardiovascular Health.
CDC: Centers for Disease Control and Prevention.
CIHR: Canadian Institutes for Health Research.
DILQ: Day in the Life Questionnaire.
FV: fruits and vegetables.
ICC: intracluster correlation coefficient.
IPAQ: International Physical Activity Questionnaire.
LPA: light physical activity.
MANCOVA: multi‐variate analysis of covariance.
MVPA: moderate to vigorous physical activity.
PAQ‐C: Physical Activity Questionnaire for Older Children.
PE: physical education.
PROGRESS‐Plus: place of residence, race/ethnicity/culture/language, occupation, gender/sex, religion, education, socioeconomic status, social capital, personal characteristics associated with discrimination, features of relationships, and time‐dependent relationships.
RAPA: Rapid Assessment of Physical Activity questionnaire.
RCT: randomized controlled trial.
SD: standard deviation.
SES: socioeconomic status.
SSB: sugar‐sweetened beverage.
TIDieR: Template for Intervention Description and Replication.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Brannon 2018 | Ineligible study design: cross‐over trial without suitable first period data |
| DeVilliers 2009 | Ineligible control: no intervention received |
| Harrington 2005 | Ineligible study design: secondary analyses from a randomized controlled trial |
| Natale 2016 | Ineligible control: did not receive an eligible child‐only intervention |
| Regev 2012 | Ineligible outcomes |
| Russell Mayhew 2007 | Ineligible outcomes |
| Treu 2017 | Ineligible study design: experimental but not random or quasi‐random |
Characteristics of studies awaiting assessment [ordered by study ID]
Kobak 2016.
| Methods |
Study design: randomized controlled trial Study grouping: cross‐over design Study aim: the primary aim of this study was "to assess the amount and intensity of children’s physical and sedentary activity behavior during three separate simulated recess conditions: playing alone, with their parent participating, and with their friend participating" (quote) Study period: not known Total number of arms: not known Description of intervention arms: 1. Playing with a parent (child + caregiver); 2. Playing alone (child only); 3. Playing with a friend (not eligible) Sample size justification and outcome used: not known Unit of allocation: individual child Missing data handling: not known Reported limitations: 1. Most participating parents were fathers; 2. There are no other studies on this topic to compare or contrast the results; 3. The allotted amount of time was relatively short Randomization ratio and stratification: not relevant Participant compensation or incentives: children received USD 10 for completing each of 3 sessions (USD 30 total) |
| Participants |
Baseline characteristics Children acted as their own controls
Recruitment methods: 5 boys and 5 girls were recruited via fliers posted in the local community and a database of potential participants who had contacted the principal investigator regarding unrelated studies. These children were asked to choose a friend of the same biological sex to play with them. Once the friend was selected, research personnel contacted the friend's parent for consent for the friend to participate. If the parent agreed, the friend also became a participant in the study Inclusion criteria: not known Exclusion criteria: not known Age of participating children at baseline: not known Total number randomized by relevant group: 20 Baseline imbalances between relevant groups: not relevant Total number analyzed by relevant group: not relevant Attrition by relevant group: no attrition Description of sample for baseline characteristics reported above: all children with consent (n = 20) |
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at each assessment
Children's height and weight were measured at baseline, and this was used to calculate body mass index. However, collection of height and weight measurements was not repeated at subsequent assessments |
| Notes |
Author's name: Mallory Kobak Email: not known Country: USA Setting: Independence, Ohio Types of reports: PhD thesis Comments: used 1 report only: Kobak 2016 Conflicts of interest: not known Sponsorship source: not known |
NTR5755.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: this study aims "to investigate whether the dietary and physical activity behaviors of children between 9 and 12 years at the school participate in the intervention 'KERNgezond' is healthier if the parents of these children follow the E‐learning 'Making a healthy deal with your child,' compared to children whose parents only receive a folder about healthy diet and physical activity" (quote) Study period: September 2015 to December 2016 Total number of arms: not known Description of intervention arms: 1. KERNgezond intervention and caregiver e‐learning program (child + caregiver); 2. KERNgezond intervention (child only); possible other intervention arms Number of clusters per arm: not known Average cluster size: not known Sample size justification and outcome used: not known Unit of allocation: school Missing data handling: not known Reported limitations: not known Randomization ratio and stratification: not known Participant compensation or incentives: not known |
| Participants |
Baseline characteristics: not known Recruitment methods: not known Inclusion criteria: clusters: primary schools located in the northern part of province Limburg and participating in the "KERNgezond" program; participants: children in sixth and seventh grades whose parents are willing to participate Exclusion criteria: clusters: not known; participants: insufficient understanding of Dutch Age of participating children at baseline: sixth to seventh grade (9 to 12 years old) Total number randomized by relevant group: total across all study arms: n = 1500; sample size per eligible arm not reported Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm (Intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 5 months (end of intervention), and 1 year (follow‐up)
|
| Notes |
Author's name: Emilie Ruiter Email: e.ruiter@elg.umcn.nl Country: The Netherlands Setting: primary schools in Limberg, The Netherlands Types of reports: trial registration Comments: used the following report: (1) trial registration (Netherlands Trial Register: NTR5755) Conflicts of interest: not known Sponsorship source: Province Limburg, The Netherlands |
Ruiter 2015a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: this study aims "to investigate the effects of our web‐based parenting program entitled 'Making a healthy deal with your child' on dietary, sedentary, and physically active behavior among children 9–13 years of age who participate in the existing school‐based overweight prevention program entitled 'Scoring for Health'" (quote) Study period: January 2013 to December 2014 Total number of arms: 2 Description of intervention arms: 1. Scoring for Health intervention and caregiver e‐learning program (child + caregiver); 2. Scoring for Health intervention (child only); possible other intervention arms Number of clusters per arm: not known Average cluster size: not known Sample size justification and outcome used: 40% of children aged 9 to 13 living in this region of The Netherlands meet the Dutch standards for fruit and vegetable intake, SSB intake, and sedentary behavior. To detect an increase of 20% in the number of children who meet these standards 1 year after baseline (i.e. an increase from 40% to 60%), with 80% power and a 5% probability of a type 1 error, 161 children per arm were required. Estimate of intracluster correlation (ICC) was based on similar effectiveness studies and school‐based programs in children aged 9 to 13 years Unit of allocation: class Missing data handling: not known Reported limitations: 1. It is likely that more motivated parents will complete the e‐learning program; 2. Use of a within‐school design may result in contamination effects; 3. BMI was not included as a measure of effectiveness; 4. Outcomes were reported by children and parents Randomization ratio and stratification: 1:1; to control for school characteristics, randomization was performed centrally at the school grade level class and within schools, and groups were stratified by ethnicity Participant compensation or incentives: parents received euro (EUR) 30 and children received a small bottle of water for their participation |
| Participants |
Baseline characteristics: not known Recruitment methods: contacted principals of 11 schools in the Nijmegen region in The Netherlands that were participating in the Scoring for Health intervention for permission to invite parents of children to participate with their child. Envelopes included information on the study and passive informed consent forms for child and parent. The parental baseline questionnaire was sent home with children after they completed the baseline questionnaire in school. A reminder was sent to non‐responders after 3 weeks Inclusion criteria: clusters: schools in the Nijmegen region and participating in the "Scoring for Health" program; participants: children in fourth, fifth, or seventh grade whose parents are willing to participate Exclusion criteria: clusters: not known; participants: insufficient understanding of Dutch Age of participating children at baseline: fourth, fifth, or seventh grade (9 to 13 years old) Total number randomized by relevant group: 322 children anticipated Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review at baseline, 5 months (end of intervention), and 1 year (follow‐up)
Children's height and weight were measured at baseline, and this was used to calculate body mass index. However, collection of height and weight measurements was not repeated at subsequent assessments |
| Notes |
Author's name: Emilie Ruiter Email: e.ruiter@elg.umcn.nl Country: The Netherlands Setting: schools in Nijmegen region, The Netherlands Types of reports: trial registration; published protocol Comments: used the following reports: (1) Ruiter 2015b, and (2) trial registration (Netherlands Trial Register: NTR3938) Conflicts of interest: all study authors declare no competing interests, except for the fact that they have developed the e‐learning program entitled "Making a Healthy Deal With Your Child" Sponsorship source: The Netherlands Organization for Health Research and Development (ZonMw; project number 505010296015) |
Swindle 2017a.
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: this study will “test the impact of the enhanced implementation strategy of WISE on implementation and child health outcomes using a Hybrid Type III Cluster Randomized Trial and continuous formative evaluation" (quote) Study period: January 2018 to June 2020 Total number of arms: 2 Description of intervention arms: 1. Enhanced WISE strategy (child + caregiver); 2. Basic WISE strategy (child only) Number of clusters per arm: 6 Average cluster size: not known Sample size justification and outcome used: study authors based power calculations on data from the previous WISE study. For the present study, study authors reported that the design will provide 80% power to detect an effect of 0.40 (a half standard deviation) with a 5% probability of a type 1 error Unit of allocation: Head Start center Missing data handling: not known Reported limitations: not known Randomization ratio and stratification: 1:1; stratified by center size and key zip code characteristics (e.g. food insecurity, poverty) Participant compensation or incentives: not known |
| Participants |
Baseline characteristics: not known Recruitment methods: not known; all centers (n = 12) from the partnering Head Start agency will be randomized to implement the basic WISE strategy or the enhanced WISE strategy Inclusion criteria: clusters: centers within the partnering Head Start agency; participants: child enrolled in a participating center, aged 3 to 5 years Exclusion criteria: not known Age of participating children at baseline: 3 to 5 years Total number randomized by relevant group: 760 children anticipated Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments were used to measure outcomes relevant to this review twice yearly (time points not specified)
|
| Notes |
Author's name: Taren Swindle Email: tswindle@uams.edu Country: USA Setting: Head Start centers in Arkansas Types of reports: published protocol; trial registration Comments: used the following reports: (1) Swindle 2017, and (2) trial registration (Clinicaltrials.gov registration number NCT03075085) Conflicts of interest: "the authors declare that they have no competing interests" (quote) Sponsorship source: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, under award number K01 DK110141‐01 |
ICC: intracluster correlation coefficient.
RRS: resonance Raman spectroscopy.
SD: standard deviation.
TIDieR: Template for Intervention Description and Replication.
USD: United States dollar.
Characteristics of ongoing studies [ordered by study ID]
Armstrong 2019a.
| Trial name or title | Creating Healthy Habits Among Maryland Preschoolers (CHAMP) |
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: this study aims "to evaluate strategies to prevent health disparities by building wellness‐related habits of diet and physical activity into daily child care activities and extending the habits introduced in child care centers to caregivers" (quote) Study period: June 2016 to July 2019 Total number of arms: 3 Description of intervention arms: 1. Child care center−based wellness intervention plus a web‐based caregiver intervention (child + caregiver arm); 2. Child care center−based wellness intervention (child only); 3. No intervention control (not eligible) Number of clusters per arm: not known Average cluster size: not known Sample size justification and outcome used: study authors reported their intent to enroll 864 children across 54 child care centers (an average of 16 children per center). To calculate power and sample size estimates, study authors assumed a correlation of r = 0.5 between repeated measures of the same individual, accounted for a loss to follow‐up rate of 20%, and estimated an ICC of 0.03. Study authors reported that the expected sample size "will provide adequate power (> 0.8) to detect an effect as small as 0.27 standard deviations (SD) across outcomes" (quote). The estimate of intraclass correlation coefficient (ICC) was based on previous literature and was averaged across outcomes of interest (child body mass index, MVPA, fruit and vegetable intake, and willingness to try new foods) Unit of allocation: child care center Missing data handling: not known Reported limitations: not known Randomization ratio and stratification: 1:1:1; research staff matched centers into stratified groups of 3 based on similarity of center size, location, and racial/ethnic mix. Centers within the group of 3 are then randomized to 1 of the 3 conditions Participant compensation or incentives: caregivers and child care staff receive gift card compensation for completion of questionnaires, and caregivers receive additional gift card reimbursement for completion of the secondary measures. Liaisons working at each participating child care center receive gift card compensation for recruiting participants |
| Participants |
Baseline characteristics: not known Recruitment methods: child care centers in the state of Maryland that meet eligibility criteria were filtered for those located within 50 miles of the university and having more than 20 children enrolled. Eligible centers were contacted by the study team to describe the study, assess eligibility, and, if the center is interested, arrange a visit to the center to meet with the director and discuss the intervention and the evaluation. Eligible centers that express interest after this recruitment visit and within the recruitment time frame are invited to participate. Study staff and center liaisons create a recruitment plan for each center that involves print materials, a video on the program, presentations at back‐to‐school nights, and discussion with parents at drop‐offs and pick‐ups Inclusion criteria: cluster: licensed center serving low‐income communities with children aged 3 to 5 years enrolled, childcare staff must be at least 18 years old; participants: child attending participating child care center at least 3 days per week, aged 3 to 5 years, English‐speaking, caregiver anticipates that the child will be enrolled in the center through the spring, and the caregiver gives informed consent; caregiver eligibility criteria include being the child's primary caregiver, living with the child 4 or more days per week, basic English literacy, and being at least 18 years old Exclusion criteria: cluster: Head Start center, childcare staff cannot speak English; participants: child has health problems that would interfere with participation in physical activity or developmental delays that prevent assessment of key study outcomes Age of participating children at baseline: 3 to 5 years Total number randomized by relevant group: 864 children anticipated Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments are being used to measure outcomes relevant to this review
|
| Starting date | The study began in July 2016, and the trial was registered on April 12, 2017 |
| Contact information |
Author's name: Maureen Black Email: mblack@som.umaryland.edu |
| Notes |
Country: USA Setting: childcare centers in Maryland Types of reports: published protocol; trial registration Comments: used the following reports: (1) Armstrong 2019, and (2) trial registration (Clinicaltrials.gov registration number NCT03111264) Conflicts of interest: not known Sponsorship source: National Institute of Diabetes and Kidney Diseases, under award number 1R01DK107761‐01 |
Cunningham Sabo 2016.
| Trial name or title | Study name: Fuel for Fun |
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: factorial assignment Study aim: this study "builds on prior research to engage multiple sectors of the community to reduce the risk of childhood obesity by promoting healthful food and activity environments, policies and behaviors through: 1) developing and testing the efficacy of a 4th grade comprehensive school‐ and family‐based intervention, 2) applying this intervention to an afterschool setting, and 3) state‐wide program dissemination" (quote) Study period: not known Total number of arms: 4 (note: trial registration indicates 5 arms, including a no intervention control arm) Description of intervention arms: 1. School‐based intervention plus both family intervention and online parent‐based intervention (child + caregiver A); 2. School‐based intervention plus family intervention (child + caregiver B); 3. School‐based intervention plus online parent‐based intervention (child + caregiver C); 4. School‐based condition (child only) Number of clusters per arm: not known Average cluster size: not known Sample size justification and outcome used: power calculations sought to determine minimum sample sizes to detect a clinically relevant change at a power of 80% and a 5% probability of a type 1 error. Study authors based power calculations on data from prior studies with fourth grade Colorado students and their parents. Instead study authors reported sample sizes needed per group for 7 outcomes: child attitude (n = 50), child self‐efficacy (n = 108), child fruit and vegetable preference (n = 127), parent modeling (n = 64), parent self‐efficacy (n = 110), parent fruit and vegetable availability (n = 15), and parent eating competence (n = 105). They did not report the sample sizes needed to detect a change in the primary outcomes (fruit and vegetable consumption at school lunch and student activity level) nor in the secondary outcome (BMI) Unit of allocation: school Missing data handling: not known Reported limitations: 1. The target audience lacks diversity, therefore potentially limiting the generalizability of results; 2. Caregiver involvement will be indirect; 3. If teachers continue teaching fourth grade in participating schools, they will participate in more than 1 intervention arm, which could influence their involvement; 4. Long‐term follow‐up is not possible Randomization ratio and stratification: 1:1:1:1; 8 schools were matched on the percentage of students receiving free or reduced‐priced school meals before randomization Participant compensation or incentives: to motivate participation in the family component, family nights held at schools include a drawing for free cooking and activity prizes. As compensation or participation in accelerometry assessment, children will receive up to USD 25 in gift cards as compensation when they return their device and the device worn by their caregiver. Caregivers will receive e‐gift cards for each dietary recall that they complete and an e‐card and an e‐gift card pin for survey completion |
| Participants |
Baseline characteristics: not known; however, study authors note that the intervention schools will be "low‐to‐moderate income" (quote) Recruitment methods: not known Inclusion criteria: clusters: not known, although all schools were located in 2 districts in the same county in northern Colorado, USA; participants: child enrolled in fourth grade at a participating school and caregiver Exclusion criteria: not known Age of participating children at baseline: fourth grade (estimated to be 8 to 10 years old) Total number randomized by relevant group: total number of children randomized by relevant group has not yet been reported; however, study authors note that they anticipate recruiting 1320 to 1584 children and their parents Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm A (intervention group)
Child + caregiver arm B (intervention group)
Child + caregiver arm C (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments are being used to measure outcomes relevant to this review at baseline, 7 months (end of intervention), and 1 year (follow‐up)
|
| Starting date | The study began in July 2012, and the trial was registered on July 7, 2015 |
| Contact information |
Author's name: Leslie Cunningham‐Sabo Email: leslie.cunningham‐sabo@colostate.edu |
| Notes |
Country: USA Setting: schools in northern Colorado Types of reports: published protocol; trial registration Comments: used the following reports: (1) Cunningham‐Sabo 2016, and (2) trial registration (Clinicaltrials.gov registration number NCT02491294) Conflicts of interest: "the authors declare that they have no competing interests" (quote) Sponsorship source: National Institute of Food and Agriculture, US Department of Agriculture, under award number 2012‐68001‐19603 |
Kovalskys 2017a.
| Trial name or title | Study name: MINI SALTEN |
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "the main aim of MINI SALTEN is to assess the effects of a technology family‐based and PA school‐based intervention on (1) physical activity, and (2) quality of diet and eating behaviour in first grade children of the city of Buenos Aires. The specific aims are to (a) evaluate the effects of the intervention on children’s specific eating habits (fruit and vegetable consumption, energy intake, snack and breakfast quality), (b) evaluate progression of body mass index (BMI) over time, and (c) identify parental factors associated with changes in PA and in children’s quality of diet" (quote) Study period: July 2015 to November 2016 Total number of arm: 4 Description of intervention arms: 1. Active breaks intervention and virtual intervention (child + caregiver); 2. Active breaks intervention only (child only); 3. Virtual intervention only (not eligible); 4. No intervention control (not eligible) Number of clusters per arm: 3 Average cluster size: 35 Sample size justification and outcome used: "assuming approximately 50% participation rate, the aim is to enrol a minimum of 200 dyads, i.e. 50 per trial arm. Assuming an additional 20% attrition, it is expected to collect data on 160 dyads (40 per arm, an average of 13 per school)... the target sample size of N = 160 participants (40 in each of the four conditions) yields a 80% power to detect an effect size of 0.22... An effect size of 0.22 corresponds to a change of 5 min/day in moderate/vigorous PA (within‐cell SD = 11) and a change of 5.4 min/day of sedentary time (within‐cell SD = 12)..." Unit of allocation: school Missing data handling: not known Reported limitations: not known Randomization ratio and stratification: 1:1:1:1 Participant compensation or incentives: not known |
| Participants |
Baseline characteristics: not known Recruitment methods: not known Inclusion criteria: cluster: not known, although the Ministry of Education of the city of Buenos Aires, Argentina, pre‐selected a pool of eligible schools; participants: first grade student at participating school Exclusion criteria: cluster: not known; participants: children with severe intellectual difficulties, limitations to engage in physical activity, suffering from illnesses compromising nutrition or food selection, or taking medication known to affect body weight, or parents who do not have access to Internet or who have severe intellectual disabilities Age of participating children at baseline: first grade (estimated age: 6 years) Total number randomized by relevant group: 200 children anticipated Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments are being used to measure outcomes relevant to this review at baseline and at 1 year (end of intervention)
|
| Starting date | The study began in July 2015, and the trial was registered on March 14, 2016 |
| Contact information |
Author's name: Irina Kovalskys Email: ikovalskys@ilsi.org.ar |
| Notes |
Country: Argentina Setting: schools in Buenos Aires, Argentina Types of reports: published protocol; abstract; trial registration Comments: used the following reports: (1) Kovalskys 2017c, (2) Kovalskys 2017b, and (2) trial registration (ISRCTN58093412) Conflicts of interest: "the authors declare that they have no competing interests" (quote) Sponsorship source: Coca Cola Foundation |
NCT00065247.
| Trial name or title | Study name: Beat Osteoporosis: Nourish and Exercise Skeletons (BONES) Project |
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: "this study will implement and evaluate an after‐school program with exercise, education, and diet components designed to improve bone quality and muscle strength in early elementary school children” (quote) Study period: study start date: June 1999, study completion date: May 2004 Total number of arms: 3 Description of intervention arms: 1. The BONES Project plus a parent/caregiver component (child + caregiver); 2. The BONES Project (child only); 3. No intervention control (not eligible) Number of clusters per arm: not known Average cluster size: not known Sample size justification and outcome used: not known Unit of allocation: after‐school program Missing data handling: not known Reported limitations: not reported Randomization ratio and stratification: not known Participant compensation or incentives: not known |
| Participants |
Baseline characteristics: not known Recruitment methods: not known Inclusion criteria: clusters: after‐school programs in Massachusetts and Rhode Island, USA; participants: child aged 6 to 9 years, enrolled in a participating after‐school program, and living in Massachusetts or Rhode Island, USA Exclusion criteria: clusters: not known; participants: not known Age of participating children at baseline: 6 to 9 years Total number randomized by relevant group: 1500 children anticipated Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following relevant outcomes relevant to this review were measured at assessments (time points not specified)
|
| Starting date | The study began in June 1999, and the trial was registered on July 22, 2003 |
| Contact information |
Author's name: Christina Economos Email: christina.economos@tufts.edu Country: USA Setting: after‐school programs in Massachusetts and Rhode Island Types of reports: trial registration Comments: used the following report: (1) trial registration (Clinicaltrials.gov registration number NCT00065247) Conflicts of interest: not known Sponsorship source: National Institute of Child Health and Human Development (R01HD037752) |
| Notes |
NCT02809196.
| Trial name or title | Study name: Texts for Healthy Teens (T4HT): A Health Education Program for Adolescents |
| Methods |
Study design: randomized controlled trial Study grouping: factorial assignment Study aim: “the overall objective is to examine if participating in an SMS‐transmitted health educational program targeting a cluster of dietary factors over a period of weeks during the years of adolescence can induce durable changes toward more healthful dietary habits” (quote) Study period: study start date: June 2016, estimated study completion date: December 2017 Total number of arms: 9 Description of intervention arms: 1. Tailored SMS program implicating friend and mother (child + caregiver A); 2. Standardized SMS program implicating friend and mother (child + caregiver B); 3. Tailored SMS program implicating friend, not mother (child only A); 4. Standardized SMS program implicating friend, not mother (child only B); 5. Tailored SMS program implicating mother, not friend (child + caregiver arm C); 6. Standardized SMS program implicating mother, not friend (child + caregiver D); 7. Tailored SMS program not implicating mother or friend (child only C); 8. Standardized SMS program not implicating mother or friend (child only D); 9. No SMS program (not eligible) Number of clusters per arm: not relevant Average cluster size: not relevant Sample size justification and outcome used: not known Unit of allocation: child Missing data handling: not known Reported limitations: not known Randomization ratio and stratification: not known Participant compensation or incentives: not known |
| Participants |
Baseline characteristics: not known Recruitment methods: not known Inclusion criteria: participants: participating in the National Danish Birth Cohort and aged 14 to 15 years Exclusion criteria: participants: lacking information from maternal interviews 1 and 2 Age of participating children at baseline: 14 to 15 years Total number randomized by relevant group: 8000 children anticipated Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions | Child + caregiver arm A (intervention group)
Child‐only A (control group)
Child + caregiver arm B (intervention group)
Child‐only B (control group)
Child + caregiver arm C (intervention group)
Child‐only C (control group)
Child + caregiver arm D (intervention group)
Child‐only arm D (control group)
|
| Outcomes | The following relevant outcomes relevant to this review are being measured at baseline, 6 months, and 12 months
|
| Starting date | The study began in June 2016, and the trial was registered on June 22, 2016 |
| Contact information |
Author's name: Sjurdur Olsen Email: sfo@ssi.dk Country: Denmark Setting: any location in Denmark Types of reports: trial registration Comments: used the following report: (1) trial registration (Clinicaltrials.gov registration number NCT02809196) Conflicts of interest: not known Sponsorship source: not known |
| Notes |
NCT02942823.
| Trial name or title | Study name: Kids' Obesity Prevention Program (KOP) Part 2 |
| Methods |
Study design: randomized controlled trial Study grouping: parallel group Study aim: this study aims “to evaluate a motion‐controlled serious game regarding its acceptance and efficacy in a randomized controlled trial in parents of primary school children aged 9 to 12 years” (quote) Study period: October 2016 to April 2017 (estimated) Total number of arms: 2 Description of intervention arms: 1. Serious game playing + parental involvement (child + caregiver); 2. Serious game playing only (child only) Number of clusters per arm: not relevant Average cluster size: not relevant Sample size justification and outcome used: not known Unit of allocation: child Missing data handling: not known Reported limitations: not known Randomization ratio and stratification: 1:1 Participant compensation or incentives: not known |
| Participants |
Baseline characteristics: not known Recruitment methods: fourth grade students from a single school who received the original KOP intervention will be randomly allocated to an intervention group and a control group Inclusion criteria: participants: all fourth grade children from a single primary school Exclusion criteria: participants: children with massive linguistic difficulties (after study participation) Age of participating children at baseline: 9 to 12 years Total number randomized by relevant group: total number of children randomized by relevant group has not yet been reported; however, study authors note that they anticipate enrolling 34 participants Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments are being used to measure outcomes relevant to this review at baseline, 2 weeks, 4 weeks (follow‐up)
|
| Starting date | The study began in January 2016, and the trial was registered on October 24, 2016 |
| Contact information |
Author's name: Isabelle Mack Email: isabelle.mack@medizin.uni‐tuebingen.de |
| Notes |
Country: Germany Setting: primary school in Germany Types of reports: trial registration Comments: used the following report: (1) trial registration (Clinicaltrials.gov registration number NCT02942823) Conflicts of interest: not known Sponsorship source: not known |
Yin 2019a.
| Trial name or title | Study name: ¡Míranos! Look at Us, We Are Healthy! |
| Methods |
Study design: cluster‐randomized controlled trial Study grouping: parallel group Study aim: this study “will use a cluster randomized controlled design to test the efficacy of the ¡Míranos! intervention in preventing excessive weight gain and promoting the development of healthy habits in young children enrolled in Head Start" (quote) Study period: May 2018 to August 2021 (estimated) Total number of arms: 3 Description of intervention arms: 1. Combined center‐ and home‐based intervention (child + caregiver); 2. Center‐based intervention (child only); 3. Attention control arm offering Head Start−endorsed obesity prevention curriculum (not eligible) Number of clusters per arm: 4 Average cluster size: 37 (estimated) Sample size justification and outcome used: study authors based power calculations on data from a previous study with a similar center‐based intervention and home‐based intervention components. For the present study, study authors reported that “a sample size of 12 centers (i.e., 4 centers/group) with 29 children per center” (quote) was needed to detect a difference between the child + caregiver and child‐only arms and the attention control arm of 0.53 BMI units at a power of 80% and a 5% probability of a type 1 error, assuming an ICC of 0.003 and SD = 1.147. “The final sample size was increased to 37 (> 29/0.8) children per center (i.e. 37 × 12 = 444 children in total) to account for an attrition rate of 80%” (quote). Unit of allocation: Head Start center Missing data handling: study authors reported that participants with missing data will be compared with participants with complete data to assess any differences in demographic and outcome measures, using available data. If data are missing at random (MAR), standard computational algorithms will be used to generate appropriate parameter estimates using all available data. If the MAR assumption is in doubt, missing data will be imputed using the multiple imputations with chained equations approach. Specifically, missing values will be imputed by adjusting for time of measurement and demographics to create 10 imputed data sets. Effect sizes then will be combined using the Rubin’s rules Reported limitations: 1. Head Start staff will not be blinded to treatment assignment; 2. Data collection staff will not be blinded to treatment assignment Randomization ratio and stratification: 1:1:1; stratified by the organization overseeing each center and center enrollment size Participant compensation or incentives: to increase parental participation and compliance, incentives (up to USD 30) will be provided for completing daily logs (USD 3 per day) and parent surveys (USD 9 and raffles for a tricycle); staff members will receive cash incentives for their centers by participating in center‐wide wellness challenges |
| Participants |
Baseline characteristics: not known Recruitment methods: Head Start centers were selected from 2 organizations that joined the study as collaborators. Twelve centers were determined to meet the eligibility criteria and have been randomly assigned to 1 of the 3 treatment conditions (3 centers from organization A and 9 centers from organization B). Recruitment packets will be sent home with eligible children from each participating center. Children will receive a coloring book if their parents return a signed consent form agreeing or declining to participate in the study Inclusion criteria: clusters: full‐day center (more than 7 hours of care per day), at least 1 classroom enrolling children aged 3, agreement to modify center physical activity and nutrition policies, agreement not to participate in other health‐related studies; participants: child enrolled in a participating center, aged 3 years at baseline, parental consent, 1 child per family Exclusion criteria: not known Age of participating children at baseline: 3 years Total number randomized by relevant group: total number of children randomized by relevant group has not yet been reported; however, study authors note that they anticipate recruiting 444 children and their parents Baseline imbalances between relevant groups: not known Total number analyzed by relevant group: not known Attrition by relevant group: not known Description of sample for baseline characteristics reported above: not relevant |
| Interventions |
Intervention characteristics Child + caregiver arm (intervention group)
Child‐only arm (control group)
|
| Outcomes | The following instruments are being used to measure outcomes relevant to this review at baseline, 8 months (end of intervention), and 21 months (1‐year post‐intervention follow‐up)
|
| Starting date | The study began in May 2018, and the trial was registered on July 18, 2018 |
| Contact information |
Author's name: Zenong Yin Email: zenong.yin@utsa.edu |
| Notes |
Country: USA Setting: Head Start centers in San Antonio, Texas Types of reports: published protocol; trial registration Comments: used the following reports: (1) Yin 2019, and (2) trial registration (Clinicaltrials.gov registration number NCT03590834) Conflicts of interest: "the authors declare that they have no competing interests" (quote) Sponsorship source: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, under award number R01DK109323 |
BCT: behavior change technique.
BMI: body mass index.
CDC: Centers for Disease Control and Prevention.
FFQ: food frequency questionnaire.
GPAQ: Global Physical Activity Questionnaire.
ICC: intracluster correlation coefficient.
IPAQ: International Physical Activity Questionnaire.
MAR: missing at random.
MVPA: moderate to vigorous physical activity.
NHANES: National Health and Nutrition Examination Survey.
PA: physical activity.
SD: standard deviation.
SMS: short message service.
SSB: sugar‐sweetened beverage.
TIDieR: Template for Intervention Description and Replication.
WHO: World Health Organization.
Differences between protocol and review
Review information
An additional review author (US) joined the research team after publication of the protocol and participated in several research activities as described in the Contributions of authors section.
Types of interventions
In the protocol (Morgan 2017), we indicated that the control group had to receive the same intervention as the intervention group, with the exception of the caregiver component. However, we identified a few studies in which one group received a child intervention with some communication to caregivers and the other received the same child intervention as well as a robust caregiver intervention. An example of this is Alhassan 2018a, in which caregivers in both groups received newsletters, but in one arm they also participated in weekly dance classes with their daughters. Given important differences in the nature and dose of intervention activities directed at caregivers in the two arms, we determined that it was appropriate to include these interventions in this review. Therefore, we now indicate that a study could be eligible for inclusion if the control group intervention "did not include a component involving caregivers or included caregivers in only a marginal capacity," and we also note that intervention components across the groups must be "similar" (rather than "the same"), except for the caregiver component.
Types of outcome measures
In the protocol (Morgan 2017), we indicated that, with the exception of adverse effects, all of our outcomes would relate to change: change in children's dietary intake, change in children's physical activity levels, change in children's dietary quality, change in children's sedentary behavior, change in prevalence of overweight and obesity among children's BMI or weight‐for‐height parameter, change in caregiver's dietary intake, and change in caregiver's physical activity levels. When possible, we used change scores in our analyses; however, for many studies, change scores were not available and we used end values. To reduce possible confusion, we therefore have removed "change in" from the names of our outcome measures.
In the protocol (Morgan 2017), we did not stipulate which specific diet and physical activity outcomes would be the focus of this review. Therefore, before data extraction, we created a list of what we believed to be the most important outcomes, as well as outcomes measured in our included studies, and discussed each outcome as a team. Throughout this process, we additionally consulted with the Cochrane Nutrition Field. We list the specific diet and physical activity outcomes of interest in parentheses in the Methods section.
We pre‐specified that we would include dietary outcomes measured by validated instruments only. Because several studies included in our review were published more than 20 years ago, both measurement techniques and reporting expectations have changed over time, and we lacked criteria for definitively evaluating instrument validity and reliability; therefore we chose not to limit our inclusion to dietary outcomes measured by validated tools. In cases in which study authors specified whether the instruments that they used were validated, we included this information in the Characteristics of included studies. Additionally, in the protocol, we provided specific examples of measures that could be used to assess each primary and secondary outcome (Morgan 2017). Because most of these example measures were not used in studies included in this review, we removed these examples and replaced them with relevant categories of measurement instruments. For example, instead of specifying that we were interested in dietary intake “as measured by validated instruments such as the Automated Self‐Administered 24‐hour Dietary Recall for Children (Diep 2015), the Block Kids Food Frequency Questionnaire (Cullen 2008), or similar,” we now indicate that we were interested in dietary intake “as measured by instruments such as 24‐hour dietary recalls and food frequency questionnaires.”
We planned to include all primary and secondary outcomes, if addressed in included studies, in the "Summary of findings" tables. However, given the large number of specific dietary intake and physical activity behavior outcomes, we chose the seven primary outcomes that we believed to be most important from a clinical perspective: percentage of dietary intake from saturated fat, sodium intake, fruit and vegetable intake, and SSB intake; total physical activity; MVPA; and adverse effects. When data allowed, we pooled outcome statistics for studies’ end‐of‐intervention assessments, regardless of study length, for these tables.
In our protocol (Morgan 2017), we indicated that we would group time points across studies and suggested that we would group interventions with others of similar duration. Due to considerable heterogeneity in the duration of interventions, and because the dose delivered at a specific time point may be similar between studies of different duration, we chose to pool outcome statistics collected at time points during and at the end of the intervention. We describe our approach in the Data synthesis section.
Searching other resources
In the protocol (Morgan 2017), we indicated that we would email the contact author of each included study to ask for information about any other relevant trials of which they were aware. Due to the very large number of records screened through our database searches, as well as reviews of the reference lists of included studies and relevant systematic reviews, this was omitted.
Selection of studies
US and a research assistant participated in title and abstract screening.
Due to the very large number of records screened, we do not list in the Characteristics of excluded studies tables all studies for which we obtained the full‐text reports. Instead, we list only those that required discussion or author correspondence to reach consensus that the study should be excluded. A summary of decisions on all records is presented in the PRISMA diagram (Figure 1).
Data extraction and management
To make the most of the specific skills and knowledge of different review authors, we made slight modifications to who was involved in various aspects of data extraction and management. An additional review author (US) and a research assistant participated in data extraction. Rather than resolving discrepancies by discussion between the two extractors, EHM reviewed all extracted data and resolved discrepancies. When she had difficulty, she sought input from AS instead of RAS. For studies awaiting classification and ongoing studies, data extraction was carried out by only one review author (EHM).
We simplified and modified our approach to data extraction, including extracting information on all items on the template for intervention description and replication (TIDieR) (Hoffman 2014). We added extraction of information on child and caregiver diet, physical activity, and weight status at baseline. Although planned, we did not extract data on sample representativeness, reasons for withdrawal and exclusions, and caregiver comorbidities, as we believe that these study and sample characteristics are adequately addressed through other items.
We contacted the trial authors of only English language reports when reported information was unclear or contradictory, or when important details or data were missing.
In our protocol (Morgan 2017), we did not anticipate identifying studies in which the number of children randomized per arm would not be reported. To address this, we estimated these values using available information.
Although not pre‐specified, when data allowed, we prioritized within‐group change values for analyses. When both end values and change values were presented, we extracted both, so that we could utilize the end value data to calculate assumed risk for the "Summary of findings" tables.
Data synthesis
Studies included in our review often used different units to measure treatment effect for continuous outcomes, thereby necessitating the use of SMD to poll data. This method is appropriate only when data from all studies are provided in the form of end values or change values; when the unit of measurement differs across studies, change values and end values cannot be pooled with SMD. Therefore, to maximize our capacity for meta‐analysis for outcomes in which both the unit of measurement and the format of outcome statistics differ, we pooled data across studies with the same outcome statistic format with SMD and examined data presented in the alternate format separately. We now explain this approach in the text.
Subgroup analyses and investigation of heterogeneity
In our protocol (Morgan 2017), we specified that we would conduct subgroup analyses on interventions addressing diet only versus physical activity only versus both behaviors. Following publication of our protocol (Morgan 2017), we determined that because these align with our three comparisons and the overall organization of our review, they do not apply as subgroup analyses. We did, however, subgroup our data by time points, as discussed above.
Contributions of authors
Emily H Morgan (EHM) and Anel Schoonees (AS) conceptualized the review question.
EHM and AS developed the search strategy, with input from Marlyn Faure (MF) and Rebecca A Seguin (RAS).
EHM and AS implemented the search.
Urshila Sriram (US), EHM, MF, and RAS screened search results. AS, EHM, MF, and Research Assistant Heidi Van Deventer (HVD) searched other resources, with AS and HVD focusing on the reference lists of relevant reviews, and MF and EHM focusing on the reference lists of included studies.
EHM and AS organized retrieval of screened records.
EHM and US screened retrieved papers against the inclusion criteria. When consensus could not be reached, they sought input from AS.
EHM, AS, MF, US, and HVD extracted data from eligible trials. EHM reconciled discrepancies, with input from AS.
EHM, AS, MF, US, and HVD assessed the risk of bias of included studies. EHM and AS discussed initial determinations and made final judgments.
EHM wrote to the authors of eligible studies for additional information and data.
AS and EHM entered data into RevMan and analyzed and interpreted data (Review Manager 2014), with AS providing methodological insight and EHM providing content knowledge. AS and EHM assessed the quality of the evidence in GRADEpro.
EHM oversaw data management.
AS created the interactive map of included studies.
EHM, AS, MF, and RAS wrote the review: EHM and RAS wrote the Background; EHM and AS the Objectives; AS, EHM, and MF the Methods; EHM the Results; and RAS and EHM the Discussion and Authors' contributions. All authors read the complete review and provided critical content contributions.
EHM is the guarantor and has overall responsibility for this review.
Sources of support
Internal sources
-
Cornell University, USA.
Emily H Morgan and Rebecca A Seguin were partially supported by Cornell University through employment. Urshila Sriram was partially supported by Cornell University Graduate School and Engaged Cornell Program.
-
Stellenbosch University, South Africa.
Marlyn Faure was supported by Stellenbosch University through employment.
-
University of Vermont, USA.
Emily H Morgan was partially supported by the University of Vermont through employment.
External sources
-
Cochrane South Africa, Medical Research Council, South Africa.
Emily H Morgan received a Fellowship to travel to Stellenbosch University in 2018 to collaborate with co‐authors on this review.
-
Canadian Institutes of Health Research, Canada.
Urshila Sriram was partially supported by a Doctoral Foreign Study Award (award number DFS268523) from the Canadian Institutes of Health Research.
-
Department for International Development, UK.
Anel received funding support under project number 300342‐104.
Declarations of interest
Emily H Morgan (EHM) received funding from Cornell University to attend the World Health Organization (WHO)/Cochrane/Cornell University Summer Institute for Systematic Reviews in Nutrition for Global Policy Making, hosted by the Division of Nutritional Sciences, Cornell University, Ithaca, New York, USA, July 27 to August 7, 2015. Additionally, EHM was partially supported by a Fellowship from Cochrane South Africa, South African Medical Research Council, which is funded by the Effective Health Care Research Consortium. This Consortium is funded by UK aid from the UK Government for the benefit of developing countries (Grant 5242). This Fellowship financed EHM's travel to Stellenbosch University for two weeks in 2018 to facilitate collaboration. Additionally, EHM declares that she is part owner of a small business that sells hearing aids. EHM does not believe this poses any conflict but declares it as an interest in the medical/health field.
Anel Schoonees (AS) received a Developing Country Stipend in 2018 from Cochrane to attend the Cochrane Colloquium in Edinburgh, UK. This was not related to this review, but AS declares it in the interest of transparency.
Urshila Sriram—none known.
Marlyn Faure—none known.
Rebecca A Seguin—none known.
Disclaimer: the views expressed in this publication are those of the authors and do not necessarily reflect UK government policy.
New
References
References to studies included in this review
Adamo 2017a {published data only (unpublished sought but not used)}
- Adamo K. Queries re: Activity Begins in Childhood [personal communication]. Email to E Morgan, July 19, 2019.
- Adamo KB, Barrowman N, Naylor PJ, Yaya S, Harvey A, Grattan KP, et al. Activity Begins in Childhood (ABC)—inspiring healthy active behaviour in preschoolers: study protocol for a cluster randomized controlled trial. Trials 2014;15:305. [DOI: 10.1186/1745-6215-15-305; PMC4124151; PUBMED: 25073797] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adamo KB, Wasenius NS, Grattan KP, Harvey AL, Naylor PJ, Barrowman NJ, et al. Effects of a preschool intervention on physical activity and body composition. Journal of Pediatrics 2017;188:42‐9. [DOI: 10.1016/j.jpeds.2017.05.082; PUBMED: 28666535] [DOI] [PubMed] [Google Scholar]
- ISRCTN94022291. Activity begins in childhood—a study to inspire healthy active behaviour in preschoolers [Activity begins in childhood—a randomized controlled trial to inspire healthy active behaviour in preschoolers]. www.isrctn.com/ISRCTN94022291 (first received December 11, 2012). [DOI: 10.1186/ISRCTN94022291] [DOI]
Alhassan 2018a {published data only (unpublished sought but not used)}
- Alhassan S, Nwaokelemeh O, Greever CJ, Burkart S, Ahmadi M, Laurent CW, et al. Effect of a culturally‐tailored mother‐daughter physical activity intervention on pre‐adolescent African‐American girls' physical activity levels. Preventive Medicine Reports 2018;11:7‐14. [DOI: 10.1016/j.pmedr.2018.05.009; PMC6066471 ; PUBMED: 30065909] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkart S, Laurent CW, Alhassan S. Process evaluation of a culturally‐tailored physical activity intervention in African‐American mother‐daughter dyads. Preventive Medicine Reports 2017;8:88‐92. [DOI: 10.1016/j.pmedr.2017.08.002; PMC5577404 ; PUBMED: 28879073] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01588379. Mothers and girls dancing together trial (MAGNET) [Effects of an Afro‐centric dance program for African‐American daughters and mothers]. www.clinicaltrials.gov/ct2/show/NCT01588379 (first received April 25, 2012).
Baghurst 2014 {published data only (unpublished sought but not used)}
- Baghurst T, Eichmann K. Effectiveness of a child‐only and a child‐plus‐parent nutritional education program. International Journal of Child and Adolescent Health 2014;7(3):229‐37. [Google Scholar]
Cottrell 2005 {published data only (unpublished sought but not used)}
- Cottrell L, Spangler‐Murphy E, Minor V, Downes A, Nicholson P, Neal WA. A kindergarten cardiovascular risk surveillance study: CARDIAC‐Kinder. American Journal of Health Behavior 2005;29(6):595‐606. [DOI: 10.5555/ajhb.2005.29.6.595; PUBMED: 16336114] [DOI] [PubMed] [Google Scholar]
Crespo 2012a {published data only (unpublished sought but not used)}
- Ayala GX, Elder, JP, Campbell NR, Arredondo E, Baquero B, Crespo NC, et al. Longitudinal intervention effects on parenting of the Aventuras para Niños study. American Journal of Preventive Medicine 2010;38(2):154‐62. [DOI: 10.1016/j.amepre.2009.09.038; PMC2832210; PUBMED: 20117571] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespo NC, Elder JP, Ayala GX, Slymen DJ, Campbell NR, Sallis JF, et al. Results of a multi‐level intervention to prevent and control childhood obesity among Latino children: the Aventuras Para Niños Study. Annals of Behavioral Medicine 2012;43(1):84‐100. [DOI: 10.1007/s12160-011-9332-7; PMC4131843; PUBMED: 22215470] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder J. Queries re: Aventuras Para Niños [personal communication]. Email to E Morgan, October 25, 2018.
- Elder JP, Arredondo EM, Campbell N, Baquero B, Duerksen S, Ayala G, et al. Individual, family, and community environmental correlates of obesity in Latino elementary school children. Journal of School Health 2010;80(1):20‐30. [DOI: 10.1111/j.1746-1561.2009.00462.x; PMC4477683; PUBMED: 20051087] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Bock 2013a {published data only (unpublished sought but not used)}
- Bock F, Fischer JE, Hoffmann K, Renz‐Polster H. A participatory parent‐focused intervention promoting physical activity in preschools: design of a cluster‐randomized trial. BMC Public Health 2010;10:49. [DOI: 10.1186/1471-2458-10-49; PMC2835684; PUBMED: 20113522] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock F, Genser B, Raat H, Fischer JE, Renz‐Polster H. A participatory physical activity intervention in preschools: a cluster randomized controlled trial. American Journal of Preventive Medicine 2013;45(1):64‐74. [DOI: 10.1016/j.amepre.2013.01.032; PUBMED: 23790990] [DOI] [PubMed] [Google Scholar]
- NCT00987532. A participatory parental intervention promoting physical activity in preschools. clinicaltrials.gov/ct2/show/NCT00987532 (first received September 30, 2009).
De Bourdeaudhuij 2002 {published data only (unpublished sought but not used)}
- Bourdeaudhuij I, Brug J, Vandelanotte C, Oost P. Differences in impact between a family‐ versus an individual‐based tailored intervention to reduce fat intake. Health Education Research 2002;17(4):435‐49. [PUBMED: 12197589] [DOI] [PubMed] [Google Scholar]
Dietsch 1990 {published data only (unpublished sought but not used)}
- Dietsch BJ. Effectiveness of a School/Community‐based Health Promotion Program on Changes in Diet and Diet‐related Risk Factors for Cardiovascular Disease: Family Determinants of Change in Adolescents and Their Parents [PhD dissertation]. Los Angeles, CA: University of Southern California, 1990. [Google Scholar]
Ducheyne 2014a {published and unpublished data}
- Cardon G. Queries re: cycle training RCT [personal communication]. Email to E Morgan, May 30, 2018.
- Ducheyne F, Bourdeaudhuij I, Lenoir M, Cardon G. Effects of a cycle training course on children's cycling skills and levels of cycling to school. Accident Analysis & Prevention 2014;67:49‐60. [DOI: 10.1016/j.aap.2014.01.023; PUBMED: 24607594] [DOI] [PubMed] [Google Scholar]
Frenn 2013a {published and unpublished data}
- Frenn M. Follow‐up re: Project FUN [personal communication]. Email to E Morgan, June 25, 2018.
- Frenn M, Pruszynski JE, Felzer H, Zhang J. Authoritative feeding behaviors to reduce child BMI through online interventions. Journal for Specialists in Pediatric Nursing 2013;18(1):65‐77. [DOI: 10.1111/jspn.12008; PUBMED: 23289456] [DOI] [PubMed] [Google Scholar]
Haerens 2006a {published and unpublished data}
- Haerens L. Data [personal communication]. Email to E Morgan, February 26, 2019.
- Haerens L, Bourdeaudhuij I, Maes L, Cardon G, Deforche B. School‐based randomized controlled trial of a physical activity intervention among adolescents. Journal of Adolescent Health 2007;40(3):258‐65. [DOI: 10.1016/j.jadohealth.2006.09.028; PUBMED: 17321427] [DOI] [PubMed] [Google Scholar]
- Haerens L, Bourdeaudhuij I, Maes L, Vereecken C, Brug J, Deforche B. The effects of a middle‐school healthy eating intervention on adolescents' fat and fruit intake and soft drinks consumption. Public Health Nutrition 2007;10(5):443‐9. [DOI: 10.1017/S1368980007219652; PUBMED: 17411463] [DOI] [PubMed] [Google Scholar]
- Haerens L, Deforche B, Maes L, Cardon G, Stevens V, Bourdeaudhuij I. Evaluation of a 2‐year physical activity and healthy eating intervention in middle school children. Health Education Research 2006;21(6):911‐21. [DOI: 10.1093/her/cyl115; PUBMED: 17032704] [DOI] [PubMed] [Google Scholar]
- Haerens L, Deforche B, Maes L, Stevens V, Cardon G, Bourdeaudhuij I. Body mass effects of a physical activity and healthy food intervention in middle schools. Obesity 2006;14(5):847‐54. [DOI: 10.1038/oby.2006.98; PUBMED: 16855194] [DOI] [PubMed] [Google Scholar]
Hopper 1992a {published and unpublished data}
- Gruber MB. Queries re: completed RCT [personal communication]. Email to E Morgan, May 5, 2018.
- Hopper CA, Gruber MB, Munoz KD, Herb RA. Effect of including parents in a school‐based exercise and nutrition program for children. Research Quarterly for Exercise & Sport 1992;63(3):315‐21. [DOI: 10.1080/02701367.1992.10608748; PUBMED: 1513963] [DOI] [PubMed] [Google Scholar]
Ievers Landis 2005 {published data only (unpublished sought but not used)}
- Ievers‐Landis CE, Burant C, Drotar D, Morgan L, Trapl ES, Colabianchi N, et al. A randomized controlled trial for the primary prevention of osteoporosis among preadolescent girl scouts: 1‐year outcomes of a behavioral program. Journal of Pediatric Psychology 2005;30(2):155‐65. [DOI: 10.1093/jpepsy/jsi003; PUBMED: 15681310] [DOI] [PubMed] [Google Scholar]
- Landis C. Follow‐up re: RCT with Girl Scouts [personal communication]. Email to E Morgan, August 27, 2018.
Kirks 1982a {published and unpublished data}
- Fischer BA. Questions about your 1979 study [personal communication]. Email to E Morgan, February 27, 2019.
- Kirks BA, Hendricks DG, Wyse BW. Parent involvement in nutrition education for primary grade students. Journal of Nutrition Education 1982;14(4):137‐40. [DOI: 10.1016/S0022-3182(82)80156-8] [DOI] [Google Scholar]
- Kirks BA, Hughes C. Long‐term behavioral effects of parent involvement in nutrition education. Journal of Nutrition Education 1986;18(5):203‐6. [DOI: 10.1016/S0022-3182(86)80043-7] [DOI] [Google Scholar]
Lin 2017a {published and unpublished data}
- Lin CY, Scheerman JFM, Yaseri M, Pakpour AH, Webb TL. A cluster randomized controlled trial of an intervention based on the Health Action Process Approach for increasing fruit and vegetable consumption in Iranian adolescents. Psychology & Health 2017;32(12):1449‐68. [DOI: 10.1080/08870446.2017.1341516; PUBMED: 28681612] [DOI] [PubMed] [Google Scholar]
- NCT02405611. A multi‐component intervention on improving fruit and vegetable consumption in teenagers and their mothers. clinicaltrials.gov/ct2/show/NCT02405611 (first received March 25, 2015).
- Pakpour A. Queries about your HAPA intervention for adolescents [personal communication]. Email to E Morgan, November 11, 2019.
Luepker 1996a {published and unpublished data}
- Feldman H. Catch up [personal communication]. Email to E Morgan, December 17, 2018.
- Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. Outcomes of a field trial to improve children's dietary patterns and physical activity: the Child and Adolescent Trial for Cardiovascular Health (CATCH). JAMA 1996;275(10):768‐76. [DOI: 10.1001/jama.275.10.768; PUBMED: 8598593] [DOI] [PubMed] [Google Scholar]
- Lytle LA, Johnson CC, Bachman K, Wambsgans K, Perry CL, Stone EJ, et al. Successful recruitment strategies for school‐based health promotion: experiences from CATCH. Journal of School Health 1994;64(10):405‐9. [DOI: 10.1111/j.1746-1561.1994.tb03261.x] [DOI] [PubMed] [Google Scholar]
- Lytle LA, Stone EJ, Nichaman MZ, Perry CL, Montgomery DH, Nicklas TA, et al. Changes in nutrient intakes of elementary school children following a school‐based intervention: results from the CATCH Study. Preventive Medicine 1996;25(4):465‐77. [DOI: 10.1006/pmed.1996.0078; PUBMED: 8818069] [DOI] [PubMed] [Google Scholar]
- Nader PR, Sellers DE, Johnson CC, Perry CL, Stone EJ, Cook KC, et al. The effect of adult participation in a school‐based family intervention to improve children's diet and physical activity: the Child and Adolescent Trial for Cardiovascular Health. Preventive Medicine 1996;25(4):455‐64. [DOI: 10.1006/pmed.1996.0077; PUBMED: 8818068] [DOI] [PubMed] [Google Scholar]
- Nader PR, Stone EJ, Lytle LA, Perry CL, Osganian SK, Kelder S, et al. Three‐year maintenance of improved diet and physical activity: the CATCH cohort. Archives of Pediatrics & Adolescent Medicine 1999;153(7):695‐704. [DOI: 10.1001/archpedi.153.7.695; PUBMED: 10401802] [DOI] [PubMed] [Google Scholar]
- Perry CL, Parcel GS, Stone E, Nader P, McKinlay SM, Luepker RV, et al. The Child and Adolescent Trial for Cardiovascular Health (CATCH): overview of the intervention program and evaluation methods. Cardiovascular Risk Factors 1992;2(1):36‐44. [Google Scholar]
- Perry CL, Sellers DE, Johnson C, Pedersen S, Bachman KJ, Parcel GS, et al. The Child and Adolescent Trial for Cardiovascular Health (CATCH): intervention, implementation, and feasibility for elementary schools in the United States. Health Education & Behavior 1997;24(6):716‐35. [DOI: 10.1177/109019819702400607; PUBMED: 9408786] [DOI] [PubMed] [Google Scholar]
- Zucker DM, Lakatos E, Webber LS, Murray DM, McKinlay SM, Feldman HA, et al. Statistical design of the Child and Adolescent Trial for Cardiovascular Health (CATCH): implications of cluster randomization. Controlled Clinical Trials 1995;16(2):96‐118. [PUBMED: 7789139] [DOI] [PubMed] [Google Scholar]
Perry 1988a {published and unpublished data}
- Crocket SJ, Mullis R, Perry CL, Luepker RV. Parent education in youth‐directed nutrition interventions. Preventive Medicine 1989;18(4):475‐91. [DOI: 10.1016/0091-7435(89)90007-8; PUBMED: 2678093] [DOI] [PubMed] [Google Scholar]
- Luepker R. Queries re: MN Home Team [personal communication]. Email to E Morgan, February 28, 2019.
- Luepker RV, Perry CL, Murray DM, Mullis R. Hypertension prevention through nutrition education in youth: a school‐based program involving parents. Health Psychology 1988;7 Suppl:233‐45. [PUBMED: 3243221] [PubMed] [Google Scholar]
- Perry CL, Luepker RV, Murray DM, Hearn MD, Halper A, Dudovitz B, et al. Parent involvement with children's health promotion: a one‐year follow‐up of the Minnesota home team. Health Education Quarterly 1989;16(2):171‐80. [PUBMED: 2732061] [DOI] [PubMed] [Google Scholar]
- Perry CL, Luepker RV, Murray DM, Kurth C, Mullis R, Crocket S, et al. Parent involvement with children's health promotion: the Minnesota Home Team. American Journal of Public Health 1988;78(9):1156‐60. [PMC1349385; PUBMED: 3407811] [DOI] [PMC free article] [PubMed] [Google Scholar]
Petchers 1987 {published data only (unpublished sought but not used)}
- Petchers M. Heart Health [personal communication]. Email to E Morgan, May 18, 2018.
- Petchers MK, Hirsch EZ, Bloch BA. The impact of parent participation on the effectiveness of a heart health curriculum. Health Education Quarterly 1987;14(4):449‐60. [PUBMED: 3692866] [DOI] [PubMed] [Google Scholar]
Vandongen 1995 {published and unpublished data}
- Burke V, Thompson C, Taggart AC, Spickett EE, Beilin LJ, Vandongen R, et al. Differences in response to nutrition and fitness education programmes in relation to baseline levels of cardiovascular risk in 10 to 12‐year‐old children. Journal of Human Hypertension 1996;10 Suppl 3:S99‐106. [PUBMED: 8872838] [PubMed] [Google Scholar]
- Gracey V. Fitness and nutrition trial in children [personal communication]. Email to E Morgan, April 17, 2018.
- Vandongen R, Jenner DA, Thompson C, Taggart AC, Spickett EE, Burke V, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10‐ to 12‐year‐old children. Preventive Medicine 1995;24(1):9‐22. [DOI: 10.1006/pmed.1995.1003; PUBMED: 7740021] [DOI] [PubMed] [Google Scholar]
Voll 2013 {published data only (unpublished sought but not used)}
- Voll J. Determining the “Spread of Effects” of Physical Activity Interventions From Children to Parents/Guardians [Masters thesis]. Thunder Bay, ON: Lakeland University, 2012. [Google Scholar]
Wang 2007a {published data only}
- Wang C, Zhao H, Liu P, Ju P, He Z, Cong N. Effect of three ways of nutritional education on knowledge‐attitude‐behavior with nutrition in pupils. Wei Sheng Yan Jiu [Journal of Hygiene Research] 2007;36(1):85‐7. [PUBMED: 17424859] [PubMed] [Google Scholar]
- Zhao H. Intervention Study on Improvement of Knowledge, Attitude and Practice With Calcium Nutrition in Pupil [Masters thesis]. Nanjing, JS: Southeast University, 2006. [Google Scholar]
Werch 2003a {published and unpublished data}
- Werch C. New customer message on May 17, 2018 at 02:00 PM [personal communication]. Email to E Morgan, May 17, 2018.
- Werch C, Moore M, DiClemente CC, Owen DM, Jobli E, Bledsoe R. A sport‐based intervention for preventing alcohol use and promoting physical activity among adolescents. Journal of School Health 2003;73(10):380‐8. [PUBMED: 14727390] [DOI] [PubMed] [Google Scholar]
Yeh 2018a {published and unpublished data}
- Akil N. Evaluation of Effectiveness of Classroom‐based Nutrition Intervention on Changes in Eating Behavior in African American Parents/Caregivers and Their Children [Masters thesis]. Detroit, MI: Wayne State University, 2013. [Google Scholar]
- Yeh Y. Query re: study at Head Start sites in Detroit [personal communication]. Email to E Morgan, August 18, 2018.
- Yeh Y, Hartlieb KB, Danford C, Catherine Jen KL. Effectiveness of nutrition intervention in a selected group of overweight and obese African‐American preschoolers. Journal of Racial and Ethnic Health Disparities 2018;5(3):553‐61. [DOI: 10.1007/s40615-017-0399-0; PUBMED: 28699045 ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Brannon 2018 {published data only (unpublished sought but not used)}
- Brannon EE, Cushing CC, Walters RW, Crick C, Noser AE, Mullins LL. Goal feedback from whom? A physical activity intervention using an N‐of‐1 RCT. Psychology & Health 2018;33(6):701‐12. [DOI: 10.1080/08870446.2017.1385783; PUBMED: 28988493] [DOI] [PubMed] [Google Scholar]
- Cushing C. Query on your N‐of‐1 intervention [personal communication]. Email to E Morgan, October 9, 2019.
DeVilliers 2009 {published data only}
- Villiers A. RE: De Villiers et al 2009 [personal communication]. Email to A Schoonees, March 8, 2018.
- Villiers A, Steyn NP, Lambert EV, Fourie J. Preventing diabetes through a primary school‐based intervention—the healthkick program. Journal of Diabetes 2009;1(Suppl 1):A144. [DOI: 10.1111/j.1753-0407.2009.00020.x; onlinelibrary.wiley.com/doi/epdf/10.1111/j.1753‐0407.2009.00020.x] [DOI] [Google Scholar]
Harrington 2005 {published data only}
- Franklin F. Hi5+ study [personal communication]. Email to E Morgan, April 28, 2018.
- Harrington KF, Franklin FA, Davies SL, Shewchuk RM, Binns MB. Implementation of a family intervention to increase fruit and vegetable intake: the Hi5+ experience. Health Promotion Practice 2005;6(2):180‐9. [DOI: 10.1177/1524839904263681; PUBMED: 15855288] [DOI] [PubMed] [Google Scholar]
Natale 2016 {published data only}
- Natale R. Healthy Caregivers–Healthy Children (HC2): A Childcare Center–based Obesity Prevention Program [personal communication]. Email to A Schoonees, February 15, 2018.
- Natale RN, Messiah SE, Chang C, Sardinas K, Fitzgibbons J, Peraza S. Healthy caregivers‐healthy children: a primary prevention program with preschool children. Cardiology 2016;134(Suppl 1):71. [DOI: 10.1159/000447505; Abstract number 059; www.karger.com/Article/Pdf/447505] [DOI] [Google Scholar]
Regev 2012 {published data only}
- Regev D, Kedem D, Guttmann J. The effects of mothers' participation in movement therapy on the emotional functioning of their school‐age children in Israel. The Arts in Psychotherapy 2012;39(5):479‐88. [DOI: 10.1016/j.aip.2012.08.003] [DOI] [Google Scholar]
Russell Mayhew 2007 {published data only}
- Russell‐Mayhew S, Arthur N, Ewashen C. Targeting students, teachers and parents in a wellness‐based prevention program in schools. Eating Disorders 2007;15(2):159‐81. [DOI: 10.1080/10640260701190709; PUBMED: 17454075] [DOI] [PubMed] [Google Scholar]
Treu 2017 {published data only}
- Njike V. RE: Query re: ASCEND study [personal communication]. Email to A Schoonees, April 30, 2018.
- Treu JA, Doughty K, Reynolds JS, Njike VY, Katz DL. Advancing school and community engagement now for disease prevention (ASCEND). American Journal of Health Promotion 2017;31(2):143‐52. [DOI: 10.4278/ajhp.140820-QUAN-413; PUBMED: 26559709] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Kobak 2016 {published data only (unpublished sought but not used)}
- Kobak MS. The Experimental Effect of Parent Versus Peer Influence on Children's Physical Activity Behavior [Doctoral thesis]. Kent, OH: Kent State University College, 2016. [etd.ohiolink.edu/!etd.send_file?accession=kent1459775865&disposition=inline] [Google Scholar]
NTR5755 {published data only (unpublished sought but not used)}
- NTR5755. Strengthening parenting styles and practices in the existing intervention KERNgezond to prevent overweight and obesity in children [Strengthening parenting styles and practices in the existing intervention KERNgezond to prevent overweight and obesity in children, a cluster randomized controlled study]. www.trialregister.nl/trial/5640 (first received February 22, 2016).
Ruiter 2015a {published data only (unpublished sought but not used)}
- NTR3938. Strengthening parenting styles and practices in existing interventions to prevent overweight and obesity in children [Strengthening parenting styles and practices in existing interventions to prevent overweight and obesity in children, a cluster randomized study]. www.trialregister.nl/trial/3752 (first received April 7, 2013).
- Ruiter EL, Fransen GA, Molleman GR, Velden K, Engels RC. The effectiveness of a web‐based Dutch parenting program to prevent overweight in children 9‐13 years of age: study protocol for a two‐armed cluster randomized controlled trial. BMC Public Health 2015;15:148. [DOI: 10.1186/s12889-015-1394-1; PMC4335372; PUBMED: 25884190] [DOI] [PMC free article] [PubMed] [Google Scholar]
Swindle 2017a {published data only}
- NCT03075085. Developing and testing implementation strategies for evidence‐based obesity prevention in childcare. clinicaltrials.gov/ct2/show/NCT03075085 (first received February 20, 2017).
- Swindle T, Johnson SL, Whiteside‐Mansell L, Curran GM. A mixed methods protocol for developing and testing implementation strategies for evidence‐based obesity prevention in childcare: a cluster randomized hybrid type III trial. Implemention Science 2017;12(1):90. [DOI: 10.1186/s13012-017-0624-6; PMC5516351 ; PUBMED: 28720140] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Armstrong 2019a {published data only}
- Armstrong B, Trude ACB, Johnson C, Castelo RJ, Zemanick A, Haber‐Sage S, et al. CHAMP: a cluster randomized‐control trial to prevent obesity in child care centers. Contemporary Clinical Trials 2019;86:105849. [DOI: 10.1016/j.cct.2019.105849; PUBMED: 31525490] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT03111264. Building blocks for healthy preschoolers [Building blocks for healthy preschoolers: child care and family models]. clinicaltrials.gov/ct2/show/NCT03111264 (first received March 27, 2017).
Cunningham Sabo 2016 {published data only}
- Cunningham‐Sabo L, Lohse B, Smith S, Browning R, Strutz E, Nigg C, et al. Fuel for fun: a cluster‐randomized controlled study of cooking skills, eating behaviors, and physical activity of 4th graders and their families. BMC Public Health 2016;16:444. [DOI: 10.1186/s12889-016-3118-6; PMC4882848; PUBMED: 27230565] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02491294. Fuel for fun: cooking with kids plus parents and play (FFF) [Cooking with kids 2.0: plus parents and play]. clinicaltrials.gov/ct2/show/NCT02491294 (first received July 1, 2015).
Kovalskys 2017a {published data only (unpublished sought but not used)}
- ISRCTN58093412. More jumping and better eating at home and school [MINI SALTEN: study assessing the efficacy of a virtual intervention targeted to parents and aimed at preventing obesity in 6 year old children of public schools of Buenos Aires]. isrctn.com/ISRCTN58093412 (first received March 14, 2016).
- Kovalskys I, Indart Rougier P, Luciana L, Rauch Herscovici C, Gregorio MJ. MINI SALTEN: a case study on learnings from Argentina on outcomes and challenges. Annals of Nutrition & Metabolism 2017;71(Suppl 2):96‐7. [DOI: 10.1159/000480486] [DOI] [Google Scholar]
- Kovalskys I, Rausch Herscovici C, Indart Rougier P, Gregorio MJ, Zonis L, Orellana L. Study protocol of MINI SALTEN: a technology‐based multi‐component intervention in the school environment targeting healthy habits of first grade children and their parents. BMC Public Health 2017;17(1):401. [DOI: 10.1186/s12889-017-4327-3; PMC5420097 ; PUBMED: 28477624] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT00065247 {published data only (unpublished sought but not used)}
- Economos C. Query re: BONES [personal communication]. Email to E Morgan, October 11, 2019.
- NCT00065247. The BONES project: building healthy bones in children [Beat osteoporosis: nourish and exercise skeletons (BONES)]. clinicaltrials.gov/ct2/show/NCT00065247 (first received July 18, 2003).
NCT02809196 {published data only (unpublished sought but not used)}
- Frodi Olsen S. NCT02809196, 2014‐01, texts for healthy teens: a health education program for adolescents [personal communication]. Email to E Morgan, November 4, 2019.
- NCT02809196. Texts for healthy teens: a health education program for adolescents (T4HT) [A digital messaging education program for dietary behavior modification towards healthier lifestyle among Danish adolescents]. clinicaltrials.gov/ct2/show/NCT02809196 (first received June 20, 2016).
NCT02942823 {published data only (unpublished sought but not used)}
- Mack I. NCT02942823, KOP_2, Kids Obesity Prevention Program Part 2 [personal communication]. Email to E Morgan, October 10, 2019.
- NCT02942823. Kids obesity prevention program part 2 (KOP‐2). clinicaltrials.gov/ct2/show/NCT02942823 (first received October 19, 2016).
Yin 2019a {published data only (unpublished sought but not used)}
- NCT03590834. Míranos! program, a preschool obesity prevention RCT [Obesity prevention in Head Start: Míranos! program]. clinicaltrials.gov/ct2/show/NCT03590834 (first received June 27, 2018).
- Yin Z. Query re: Miranos! [personal communication]. Email to E Morgan, November 3, 2019.
- Yin Z, Ullevig SL, Sosa E, Liang Y, Olmstead T, Howard JT, et al. Study protocol for a cluster randomized controlled trial to test "¡Míranos! Look at Us, We Are Healthy!"—an early childhood obesity prevention program. BMC Pediatrics 2019;19(1):190. [DOI: 10.1186/s12887-019-1541-4; PMC6556954 ; PUBMED: 31179916] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abraham 2008
- Abraham H, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychology 2008;27(3):379‐87. [DOI: 10.1037/0278-6133.27.3.379; PUBMED: 18624603] [DOI] [PubMed] [Google Scholar]
Adamo 2014
- Adamo KB, Barrowman N, Naylor PJ, Yaya S, Harvey A, Grattan KP, et al. Activity Begins in Childhood (ABC)—inspiring healthy active behaviour in preschoolers: study protocol for a cluster randomized controlled trial. Trials 2014;15:305. [DOI: 10.1186/1745-6215-15-305; PMC4124151; PUBMED: 25073797] [DOI] [PMC free article] [PubMed] [Google Scholar]
Adamo 2017b
- Adamo KB, Wasenius NS, Grattan KP, Harvey AL, Naylor PJ, Barrowman NJ, et al. Effects of a preschool intervention on physical activity and body composition. Journal of Pediatrics 2017;188:42‐9. [DOI: 10.1016/j.jpeds.2017.05.082; PUBMED: 28666535] [DOI] [PubMed] [Google Scholar]
Afshin 2014
- Afshin A, Micha R, Khatibzadeh S, Mozaffarian D. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: a systematic review and meta‐analysis. American Journal of Clinical Nutrition 2014;100(1):278–88. [DOI: 10.3945/ajcn.113.076901; PUBMED: 24898241] [DOI] [PMC free article] [PubMed] [Google Scholar]
Akil 2013
- Akil N. Evaluation of Effectiveness of Classroom‐based Nutrition Intervention on Changes in Eating Behavior in African American Parents/Caregivers and Their Children [Masters thesis]. Detroit, MI: Wayne State University, 2013. [Google Scholar]
Alhassan 2018
- Alhassan S, Nwaokelemeh O, Greever CJ, Burkart S, Ahmadi M, Laurent CW, et al. Effect of a culturally‐tailored mother‐daughter physical activity intervention on pre‐adolescent African‐American girls' physical activity levels. Preventive Medicine Reports 2018;11:7‐14. [DOI: 10.1016/j.pmedr.2018.05.009; NCT01588379; PMC6066471 ; PUBMED: 30065909] [DOI] [PMC free article] [PubMed] [Google Scholar]
Armstrong 2019
- Armstrong B, Trude ACB, Johnson C, Castelo RJ, Zemanick A, Haber‐Sage S, et al. CHAMP: a cluster randomized‐control trial to prevent obesity in child care centers. Contemporary Clinical Trials 2019;86:105849. [DOI: 10.1016/j.cct.2019.105849; NCT03111264; PUBMED: 31525490] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ayala 2010
- Ayala GX, Elder JP, Campbell NR, Arredondo E, Baquero B, Crespo NC, et al. Longitudinal intervention effects on parenting of the Aventuras para Niños study. American Journal of Preventive Medicine 2010;38(2):154‐62. [DOI: 10.1016/j.amepre.2009.09.038; PMC2832210; PUBMED: 20117571] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barriuso 2015
- Barriuso L, Miqueleiz E, Albaladejo R, Villanueva R, Santos JM, Regidor E. Socioeconomic position and childhood‐adolescent weight status in rich countries: a systematic review, 1990–2013. BMC Pediatrics 2015;15:129. [DOI: 10.1186/s12887-015-0443-3; PMC4578240; PUBMED: 26391227] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bauman 2012
- Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW, et al. Correlates of physical activity: why are some people physically active and others not?. Lancet 2012;380(9838):258‐71. [DOI: 10.1016/S0140-6736(12)60735-1; PUBMED: 22818938] [DOI] [PubMed] [Google Scholar]
Bautista‐Castaño 2004
- Bautista‐Castaño I, Doreste J, Serra‐Majem L. Effectiveness of interventions in the prevention of childhood obesity. European Journal of Epidemiology 2004;19(7):617‐22. [PUBMED: 15461192] [DOI] [PubMed] [Google Scholar]
Beaglehole 2011
- Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non‐communicable disease crisis. Lancet 2011;377(9775):1438–47. [DOI: 10.1016/S0140-6736(11)60393-0; PUBMED: 15461192] [DOI] [PubMed] [Google Scholar]
Biswas 2015
- Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta‐analysis. Annals of Internal Medicine 2015;162(2):123‐32. [DOI: 10.7326/M14-1651] [DOI] [PubMed] [Google Scholar]
Black 2013
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, Onis M, et al. Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet 2013;382(9890):427‐51. [DOI: 10.1016/S0140-6736(13)60937-X] [DOI] [PubMed] [Google Scholar]
Blissett 2011
- Blissett J. Relationships between parenting style, feeding style and feeding practices and fruit and vegetable consumption in early childhood. Appetite 2011;57(3):826–31. [DOI: 10.1016/j.appet.2011.05.318; PUBMED: 21651932] [DOI] [PubMed] [Google Scholar]
Brown 2009
- Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. International Journal of Epidemiology 2009;38(3):791–813. [DOI: 10.1093/ije/dyp139; PUBMED: 19351697] [DOI] [PubMed] [Google Scholar]
Brown 2019
- Brown T, Moore THM, Hooper L, Gao Y, Zayegh A, Ijaz S, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews 2019, Issue 7. [DOI: 10.1002/14651858.CD001871.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burkart 2017
- Burkart S, Laurent CW, Alhassan S. Process evaluation of a culturally‐tailored physical activity intervention in African‐American mother‐daughter dyads. Preventive Medicine Reports 2017;8:88‐92. [DOI: 10.1016/j.pmedr.2017.08.002; PMC5577404 ; PUBMED: 28879073] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burke 1996
- Burke V, Thompson C, Taggart AC, Spickett EE, Beilin LJ, Vandongen R, et al. Differences in response to nutrition and fitness education programmes in relation to baseline levels of cardiovascular risk in 10 to 12‐year‐old children. Journal of Human Hypertension 1996;10 Suppl 3:S99‐106. [PUBMED: 8872838] [PubMed] [Google Scholar]
Buttitta 2014
- Buttitta M, Iliescu C, Rousseau A, Guerrien A. Quality of life in overweight and obese children and adolescents: a literature review. Quality of Life Research 2014;23(4):1117‐39. [DOI: 10.1007/s11136-013-0568-5; PUBMED: 24249217] [DOI] [PubMed] [Google Scholar]
Cardon 2018 [pers comm]
- Cardon G. Queries re: cycle training RCT [personal communication]. Email to E Morgan, May 30, 2018.
Chan 2011
- Chan DSM, Lau R, Aune D, Vieira R, Greenwood DC, Kampman E, et al. Red and processed meat and colorectal cancer incidence: meta‐analysis of prospective studies. PLoS ONE 2011;6(6):e20456. [DOI: 10.1371/journal.pone.0020456; PMC3108955; PUBMED: 21674008] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cheungpasitporn 2014
- Cheungpasitporn W, Thongprayoon C, O'Corragain OA, Edmonds PJ, Kittanamongkolchai W, Erickson SB. Associations of sugar‐sweetened and artificially sweetened soda with chronic kidney disease: a systematic review and meta‐analysis. Nephrology 2014;19(12):791‐7. [DOI: 10.1111/nep.12343; PUBMED: 25251417] [DOI] [PubMed] [Google Scholar]
Chung 2016
- Chung A, Backholer K, Wong E, Palermo C, Keating C, Peeters A. Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: a systematic review. Obesity Reviews 2016;17(3):276‐95. [DOI: 10.1111/obr.12360; PUBMED: 26693831] [DOI] [PubMed] [Google Scholar]
Clark 2007
- Clark HR, Goyder E, Bissell P, Blank L, Peters J. How do parents' child‐feeding behaviours influence child weight? Implications for childhood obesity policy. Journal of Public Health 2007;29(2):132–41. [DOI: 10.1093/pubmed/fdm012; PUBMED: 17442696] [DOI] [PubMed] [Google Scholar]
Cole 2000
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320(7244):1240‐3. [DOI: 10.1136/bmj.320.7244.1240; PUBMED: 10797032] [DOI] [PMC free article] [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation. Covidence. Version accessed March 18, 2019. Melbourne, AU: Veritas Health Innovation.
Craigie 2011
- Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity‐related behaviours from childhood to adulthood: a systematic review. Maturitas 2011;70(3):266–84. [DOI: 10.1016/j.maturitas.2011.08.005; PUBMED: 21920682] [DOI] [PubMed] [Google Scholar]
Crespo 2012b
- Crespo NC, Elder JP, Ayala GX, Slymen DJ, Campbell NR, Sallis JF, et al. Results of a multi‐level intervention to prevent and control childhood obesity among Latino children: the Aventuras Para Niños Study. Annals of Behavioral Medicine 2012;43(1):84‐100. [DOI: 10.1007/s12160-011-9332-7; PMC4131843; PUBMED: 22215470] [DOI] [PMC free article] [PubMed] [Google Scholar]
Crocket 1989
- Crocket SJ, Mullis R, Perry CL, Luepker RV. Parent education in youth‐directed nutrition interventions. Preventive Medicine 1989;18(4):475‐91. [DOI: 10.1016/0091-7435(89)90007-8; PUBMED: 2678093] [DOI] [PubMed] [Google Scholar]
Crockett 1995
- Crockett SJ, Sims LS. Environmental influences on children's eating. Journal of Nutrition Education 1995;27(5):235‐49. [DOI: 10.1016/S0022-3182(12)80792-8] [DOI] [Google Scholar]
Cullen 2008
- Cullen KW, Watson K, Zakeri I. Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. Journal of the American Dietetic Association 2008;108(5):862‐8. [DOI: 10.1016/j.jada.2008.02.015; PUBMED: 18442512] [DOI] [PubMed] [Google Scholar]
Cunningham‐Sabo 2016
- Cunningham‐Sabo L, Lohse B, Smith S, Browning R, Strutz E, Nigg C, et al. Fuel for fun: a cluster‐randomized controlled study of cooking skills, eating behaviors, and physical activity of 4th graders and their families. BMC Public Health 2016;16:444. [DOI: 10.1186/s12889-016-3118-6; NCT02491294; PMC4882848; PUBMED: 27230565] [DOI] [PMC free article] [PubMed] [Google Scholar]
Daniels 2009
- Daniels SR. Complications of obesity in children and adolescents. International Journal of Obesity 2009;33(Suppl 1):S60‐5. [DOI: 10.1038/ijo.2009.20; PUBMED: 19363511] [DOI] [PubMed] [Google Scholar]
Darmon 2008
- Darmon N, Drewnowski A. Does social class predict diet quality?. American Journal of Clinical Nutrition 2008;87(5):1107‐17. [PUBMED: 18469226] [DOI] [PubMed] [Google Scholar]
De Bock 2010
- Bock F, Fischer JE, Hoffmann K, Renz‐Polster H. A participatory parent‐focused intervention promoting physical activity in preschools: design of a cluster‐randomized trial. BMC Public Health 2010;10:49. [DOI: 10.1186/1471-2458-10-49; PMC2835684; PUBMED: 20113522] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Bock 2013b
- Bock F, Genser B, Raat H, Fischer JE, Renz‐Polster H. A participatory physical activity intervention in preschools: a cluster randomized controlled trial. American Journal of Preventive Medicine 2013;45(1):64‐74. [DOI: 10.1016/j.amepre.2013.01.032; PUBMED: 23790990] [DOI] [PubMed] [Google Scholar]
De Onis 2010
- Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. American Journal of Clinical Nutrition 2010;92(5):1257–64. [DOI: 10.3945/ajcn.2010.29786; PUBMED: 20861173] [DOI] [PubMed] [Google Scholar]
De Vet 2011
- Vet E, Ridder DT, Wit JB. Environmental correlates of physical activity and dietary behaviours among young people: a systematic review of reviews. Obesity Reviews 2011;12(5):e130‐42. [DOI: 10.1111/j.1467-789X.2010.00784.x; PUBMED: 20630024] [DOI] [PubMed] [Google Scholar]
Diep 2015
- Diep CS, Hingle M, Chen TA, Dadabhoy HR, Beltran A, Baranowski J, et al. The Automated Self‐Administered 24‐Hour Dietary Recall for Children, 2012 version, for youth aged 9 to 11 years: a validation study. Journal of the Academy of Nutrition and Dietetics 2015;115(10):1591‐8. [DOI: 10.1016/j.jand.2015.02.021; PMC4584168; PUBMED: 25887784] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinsa 2012
- Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M. Obesity and socioeconomic status in developing countries: a systematic review. Obesity Reviews 2012;13(11):1067‐79. [DOI: 10.1111/j.1467-789X.2012.01017.x; PMC3798095; PUBMED: 22764734] [DOI] [PMC free article] [PubMed] [Google Scholar]
Draper 2015
- Draper CE, Grobler L, Micklesfield LK, Norris SA. Impact of social norms and social support on diet, physical activity and sedentary behaviour of adolescents: a scoping review. Child: Care, Health and Development 2015;41(5):654‐67. [DOI: 10.1111/cch.12241; PUBMED: 25809525] [DOI] [PubMed] [Google Scholar]
Ducheyne 2014b
- Ducheyne F, Bourdeaudhuij I, Lenoir M, Cardon G. Effects of a cycle training course on children's cycling skills and levels of cycling to school. Accident Analysis & Prevention 2014;67:49‐60. [DOI: 10.1016/j.aap.2014.01.023; PUBMED: 24607594] [DOI] [PubMed] [Google Scholar]
Elder 2010
- Elder JP, Arredondo EM, Campbell N, Baquero B, Duerksen S, Ayala G, et al. Individual, family, and community environmental correlates of obesity in Latino elementary school children. Journal of School Health 2010;80(1):20‐30. [DOI: 10.1111/j.1746-1561.2009.00462.x; PMC4477683; PUBMED: 20051087] [DOI] [PMC free article] [PubMed] [Google Scholar]
Feldman 2018 [pers comm]
- Feldman H. Catch up [personal communication]. Email to E Morgan, December 17, 2018.
Fischer 2019 [pers comm]
- Fischer BA. Questions about your 1979 study [personal communication]. Email to E Morgan, February 27, 2019.
Forouzanfar 2016
- Forouzanfar MH, Afshin A, Alexander L, Anderson HR, Bhutta, ZA, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388(10053):1659‐724. [DOI: 10.1016/S0140-6736(16)31679-8; PUBMED: 27733284] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frenn 2013b
- Frenn M, Pruszynski JE, Felzer H, Zhang J. Authoritative feeding behaviors to reduce child BMI through online interventions. Journal for Specialists in Pediatric Nursing 2013;18(1):65‐77. [DOI: 10.1111/jspn.12008; PUBMED: 23289456] [DOI] [PubMed] [Google Scholar]
Frenn 2018 [pers comm]
- Frenn M. Follow‐up re: Project FUN [personal communication]. Email to E Morgan, June 25, 2018.
Gan 2015
- Gan Y, Tong X, Li L, Cao S, Yin X, Gao C, et al. Consumption of fruit and vegetable and risk of coronary heart disease: a meta‐analysis of prospective cohort studies. International Journal of Cardiology 2015;183:129‐37. [DOI: 10.1016/j.ijcard.2015.01.077; PUBMED: 25662075] [DOI] [PubMed] [Google Scholar]
GBD 2017 Diet Collaborators 2019
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2019;393(10184):1958‐72. [DOI: 10.1016/S0140-6736(19)30041-8; PUBMED: 30954305] [DOI] [PMC free article] [PubMed] [Google Scholar]
Golan 2004
- Golan M, Crow S. Parents are key players in the prevention and treatment of weight‐related problems. Nutrition Reviews 2004;62(1):39‐50. [PUBMED: 14995056] [DOI] [PubMed] [Google Scholar]
Golley 2011
- Golley RK, Hendrie GA, Slater A, Corsini N. Interventions that involve parents to improve children's weight‐related nutrition intake and activity patterns—what nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness?. Obesity Reviews 2011;12(2):114‐30. [DOI: 10.1111/j.1467-789X.2010.00745.x; PUBMED: 20406416] [DOI] [PubMed] [Google Scholar]
Gordon‐Larsen 2000
- Gordon‐Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics 2000;105(6):e83. [PUBMED: 10835096] [DOI] [PubMed] [Google Scholar]
Gracey 2018 [pers comm]
- Gracey V. Fitness and nutrition trial in children [personal communication]. Email to E Morgan, April 17, 2018.
Gruber 2018 [pers comm]
- Gruber MB. Queries re: completed RCT [personal communication]. Email to E Morgan, May 5, 2018.
Haerens 2006b
- Haerens L, Deforche B, Maes L, Cardon G, Stevens V, Bourdeaudhuij I. Evaluation of a 2‐year physical activity and healthy eating intervention in middle school children. Health Education Research 2006;21(6):911‐21. [DOI: 10.1093/her/cyl115; PUBMED: 17032704] [DOI] [PubMed] [Google Scholar]
Haerens 2006c
- Haerens L, Deforche B, Maes L, Stevens V, Cardon G, Bourdeaudhuij I. Body mass effects of a physical activity and healthy food intervention in middle schools. Obesity 2006;14(5):847‐54. [DOI: 10.1038/oby.2006.98; PUBMED: 16855194] [DOI] [PubMed] [Google Scholar]
Haerens 2007a
- Haerens L, Bourdeaudhuij I, Maes L, Vereecken C, Brug J, Deforche B. The effects of a middle‐school healthy eating intervention on adolescents' fat and fruit intake and soft drinks consumption. Public Health Nutrition 2007;10(5):443‐9. [DOI: 10.1017/S1368980007219652; PUBMED: 17411463] [DOI] [PubMed] [Google Scholar]
Haerens 2007b
- Haerens L, Bourdeaudhuij I, Maes L, Cardon G, Deforche B. School‐based randomized controlled trial of a physical activity intervention among adolescents. Journal of Adolescent Health 2007;40(3):258‐65. [DOI: 10.1016/j.jadohealth.2006.09.028; PUBMED: 17321427] [DOI] [PubMed] [Google Scholar]
Haerens 2019 [pers comm]
- Haerens L. Data [personal communication]. Email to E Morgan, February 26, 2019.
Hall 2009
- Hall JN, Moore S, Harper SB, Lynch JW. Global variability in fruit and vegetable consumption. American Journal of Preventative Medicine 2009;36(5):402–9.e5. [DOI: 10.1016/j.amepre.2009.01.029; PUBMED: 19362694] [DOI] [PubMed] [Google Scholar]
Hallal 2012
- Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U, for the Lancet Physical Activity Series Working Group. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380(9838):247–57. [DOI: 10.1016/S0140-6736(12)60646-1] [DOI] [PubMed] [Google Scholar]
He 2009
- He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. Journal of Human Hypertension 2009;23(6):363–84. [DOI: 10.1038/jhh.2008.144; PUBMED: 19110538] [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011c
- Higgins JPT, Deeks JJ (editors). Chapter 7: Selecting studies and collecting data. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hingle 2010
- Hingle MD, O'Connor TM, Dave JM, Baranowski T. Parental involvement in interventions to improve child dietary intake: a systematic review. Preventive Medicine 2010;51(2):103‐11. [DOI: 10.1016/j.ypmed.2010.04.014; PMC2906688; PUBMED: 20462509] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoffman 2014
- Hoffman TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI: 10.1136/bmj.g1687; PUBMED: 24609605] [DOI] [PubMed] [Google Scholar]
Hopper 1992b
- Hopper CA, Gruber MB, Munoz KD, Herb RA. Effect of including parents in a school‐based exercise and nutrition program for children. Research Quarterly for Exercise & Sport 1992;63(3):315‐21. [DOI: 10.1080/02701367.1992.10608748; PUBMED: 1513963] [DOI] [PubMed] [Google Scholar]
Hu 2014
- Hu D, Huang J, Wang Y, Zhang D, Qu Y. Fruits and vegetables consumption and risk of stroke: a meta‐analysis of prospective cohort studies. Stroke 2014;45(6):1613‐9. [DOI: 10.1161/STROKEAHA.114.004836] [DOI] [PubMed] [Google Scholar]
Huang 2014
- Huang C, Huang J, Tian Y, Yang X, Gu D. Sugar sweetened beverages consumption and risk of coronary heart disease: a meta‐analysis of prospective studies. Atherosclerosis 2014;234(1):11‐6. [DOI: 10.1016/j.atherosclerosis.2014.01.037; PUBMED: 24583500] [DOI] [PubMed] [Google Scholar]
Imamura 2015
- Imamura F, O'Connor L, Ye Z, Mursu J, Hayashino Y, Bhugathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta‐analysis, and estimation of population attributable fraction. BMJ 2015;351:h3576. [DOI: 10.1136/bmj.h3576; PMC4510779; PUBMED: 26199070] [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN58093412
- ISRCTN58093412. More jumping and better eating at home and school [MINI SALTEN: study assessing the efficacy of a virtual intervention targeted to parents and aimed at preventing obesity in 6 year old children of public schools of Buenos Aires]. isrctn.com/ISRCTN58093412 (first received March 14, 2016).
ISRCTN94022291
- ISRCTN94022291. Activity begins in childhood—a study to inspire healthy active behaviour in preschoolers [Activity begins in childhood—a randomized controlled trial to inspire healthy active behaviour in preschoolers]. www.isrctn.com/ISRCTN94022291 (first received December 11, 2012). [DOI: 10.1186/ISRCTN94022291] [DOI]
Jeon 2007
- Jeon CY, Lokken RP, Hu FB, Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care 2007;30(3):744–52. [DOI: 10.2337/dc06-1842; PUBMED: 17327354] [DOI] [PubMed] [Google Scholar]
Kader 2015
- Kader M, Sundblom E, Elinder LS. Effectiveness of universal parental support interventions addressing children's dietary habits, physical activity and bodyweight: a systematic review. Preventive Medicine 2015;77:52‐67. [DOI: 10.1016/j.ypmed.2015.05.005; PUBMED: 25981555] [DOI] [PubMed] [Google Scholar]
Kirks 1982b
- Kirks BA, Hendricks DG Wyse BW. Parent involvement in nutrition education for primary grade students. Journal of Nutrition Education 1982;14(4):137‐40. [DOI: 10.1016/S0022-3182(82)80156-8] [DOI] [Google Scholar]
Kirks 1986
- Kirks BA, Hughes C. Long‐term behavioral effects of parent involvement in nutrition education. Journal of Nutrition Education 1986;18(5):203‐6. [DOI: 10.1016/S0022-3182(86)80043-7] [DOI] [Google Scholar]
Kobes 2018
- Kobes A, Kretschmer T, Timmerman G, Schreuder P. Interventions aimed at preventing and reducing overweight/obesity among children and adolescents: a meta‐synthesis. Obesity Reviews 2018;19(8):1065‐79. [DOI: 10.1111/obr.12688; PUBMED: 29671938] [DOI] [PubMed] [Google Scholar]
Kovalskys 2017b
- Kovalskys I, Indart Rougier P, Luciana L, Rauch Herscovici C, Gregorio MJ. MINI SALTEN: a case study on learnings from Argentina on outcomes and challenges. Annals of Nutrition & Metabolism 2017;71(Suppl 2):96‐7. [DOI: ] [Google Scholar]
Kovalskys 2017c
- Kovalskys I, Rausch Herscovici C, Indart Rougier P, Gregorio MJ, Zonis L, Orellana L. Study protocol of MINI SALTEN: a technology‐based multi‐component intervention in the school environment targeting healthy habits of first grade children and their parents. BMC Public Health 2017;17(1):401. [DOI: 10.1186/s12889-017-4327-3; ISRCTN58093412; PMCID: PMC5420097 ; PUBMED: 28477624] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuczmarski 2002
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer‐Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC growth charts for the United States: methods and development. Vital and Health Statistics 2002;11(246):1‐190. [PUBMED: 12043359] [PubMed] [Google Scholar]
Lee 2012
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, for the Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non‐communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380(9838):219–29. [DOI: 10.1016/S0140-6736(12)61031-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2008
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews for Interventions. Chichester (UK): John Wiley & Sons, 2008. [Google Scholar]
Lin 2017
- Lin CY, Scheerman JFM, Yaseri M, Pakpour AH, Webb TL. A cluster randomized controlled trial of an intervention based on the Health Action Process Approach for increasing fruit and vegetable consumption in Iranian adolescents. Psychology & Health 2017;32(12):1449‐68. [DOI: 10.1080/08870446.2017.1341516; PUBMED: 28681612] [DOI] [PubMed] [Google Scholar]
Lindsay 2006
- Lindsay AC, Sussner KM, Kim J, Gortmaker SL. The role of parents in preventing childhood obesity. The Future of Children 2006;16(1):169‐86. [PUBMED: 16532663] [DOI] [PubMed] [Google Scholar]
Ling 2017
- Ling J, Robbins LB, Wen F, Zhang N. Lifestyle interventions in preschool children: a meta‐analysis of effectiveness. American Journal of Preventive Medicine 2017;53(1):102‐12. [DOI: 10.1016/j.amepre.2017.01.018; PUBMED: 28237633] [DOI] [PubMed] [Google Scholar]
Lobstein 2015
- Lobstein T, Jackson‐Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015;385(9986):2510‐20. [DOI: 10.1016/S0140-6736(14)61746-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lorenc 2013
- Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. Journal of Epidemiology and Community Health 2013;67(2):190‐3. [DOI: 10.1136/jech-2012-201257; PUBMED: 22875078] [DOI] [PubMed] [Google Scholar]
Loveman 2015
- Loveman E, Al‐Khudairy L, Johnson RE, Robertson W, Colquitt JL, Mead EL, et al. Parent‐only interventions for childhood overweight or obesity in children aged 5 to 11 years. Cochrane Database of Systematic Reviews 2015, Issue 12. [DOI: 10.1002/14651858.CD012008] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lozano 2012
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380(9859):2095–128. [DOI: 10.1016/S0140-6736(12)61728-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luepker 1988
- Luepker RV, Perry CL, Murray DM, Mullis R. Hypertension prevention through nutrition education in youth: a school‐based program involving parents. Health Psychology 1988;7 Suppl:233‐45. [PUBMED: 3243221] [PubMed] [Google Scholar]
Luepker 1996b
- Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. Outcomes of a field trial to improve children's dietary patterns and physical activity: the Child and Adolescent Trial for Cardiovascular Health (CATCH). JAMA 1996;275(10):768‐76. [DOI: 10.1001/jama.275.10.768; PUBMED: 8598593] [DOI] [PubMed] [Google Scholar]
Luepker [pers comm]
- Luepker R. Queries re: MN Home Team [personal communication]. Email to E Morgan, February 28, 2019.
Luttikhuis 2009
- Luttikhuis HO, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD001872.pub2] [DOI] [PubMed] [Google Scholar]
Lytle 1994
- Lytle LA, Johnson CC, Bachman K, Wambsgans K, Perry CL, Stone EJ, et al. Successful recruitment strategies for school‐based health promotion: experiences from CATCH. Journal of School Health 1994;64(10):405‐9. [DOI: 10.1111/j.1746-1561.1994.tb03261.x] [DOI] [PubMed] [Google Scholar]
Lytle 1996
- Lytle LA, Stone EJ, Nichaman MZ, Perry CL, Montgomery DH, Nicklas TA, et al. Changes in nutrient intakes of elementary school children following a school‐based intervention: results from the CATCH Study. Preventive Medicine 1996;25(4):465‐77. [DOI: 10.1006/pmed.1996.0078; PUBMED: 8818069] [DOI] [PubMed] [Google Scholar]
Malik 2010
- Malik VS, Popkin BM, Bray GA, Després J‐P, Willett WC, Hu FB. Sugar‐sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta‐analysis. Diabetes Care 2010;33(11):2477‐83. [DOI: 10.2337/dc10-1079; 20693348; PMC2963518] [DOI] [PMC free article] [PubMed] [Google Scholar]
Malik 2013
- Malik VS, Pan A, Willett WC, Hu FB. Sugar‐sweetened beverages and weight gain in children and adults: a systematic review and meta‐analysis. American Journal of Clinical Nutrition 2013;98(4):1084‐102. [DOI: 10.3945/ajcn.113.058362; PMC3778861; PUBMED: 23966427] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marmot 2007
- Marmot M, Atinmo T, Byers T, Chen J, Hirohata T, Jackson A, et al. Food, Nutrition, Physical activity, and the Prevention of Cancer: a Global Perspective. Washington DC: World Cancer Research Fund/American Institute for Cancer Research, 2007. [Google Scholar]
Mayén 2014
- Mayén A, Marques‐Vidal P, Paccaud F, Bovet P, Stringhini S. Socioeconomic determinants of dietary patterns in low‐ and middle‐income countries: a systematic review. American Journal of Clinical Nutrition 2014;100(6):1520‐31. [DOI: 10.3945/ajcn.114.089029; PUBMED: 25411287] [DOI] [PubMed] [Google Scholar]
McLean 2003
- McLean N, Griffin S, Toney K, Hardeman W. Family involvement in weight control, weight maintenance and weight‐loss interventions: a systematic review of randomised trials. International Journal of Obesity and Related Metabolic Disorders 2003;27(9):987‐1005. [DOI: 10.1038/sj.ijo.0802383; PUBMED: 12917703] [DOI] [PubMed] [Google Scholar]
Micha 2012
- Micha R, Michas G, Mozaffarian D. Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes—an updated review of the evidence. Current Atherosclerosis Reports 2012;14(6):515‐24. [DOI: 10.1007/s11883-012-0282-8; PMC3483430; PUBMED: 23001745] [DOI] [PMC free article] [PubMed] [Google Scholar]
Micha 2015
- Micha R, Khatibzadeh S, Shi P, Andrews KG, Engell RE, Mozzaffarian D, Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE). Global, regional, and national consumption of major food groups in 1990 and 2010: a systematic analysis including 266 country‐specific nutrition surveys worldwide. BMJ Open 2015;5(9):e008705. [DOI: 10.1136/bmjopen-2015-008705; PMC4593162; PUBMED: 26408285] [DOI] [PMC free article] [PubMed] [Google Scholar]
Michie 2011
- Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO‐RE taxonomy. Psychology and Health 2011;26(11):1479‐98. [DOI: 10.1080/08870446.2010.540664; PUBMED: 21678185] [DOI] [PubMed] [Google Scholar]
Michie 2013
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine 2013;46(1):81‐95. [DOI: 10.1007/s12160-013-9486-6; PUBMED: 23512568] [DOI] [PubMed] [Google Scholar]
Michie 2015
- Michie S, Wood CE, Johnson M, Abraham C, Francis JJ, Hardeman W. Behaviour change techniques: the development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technology Assessment 2015;19(99):1‐188. [DOI: 10.3310/hta19990; PMC4781650; PUBMED: 26616119] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mielke 2016
- Mielke GI, Brown WJ, Nunes BP, Silva ICM, Hallal PC. Socioeconomic correlates of sedentary behavior in adolescents: systematic review and meta‐analysis. Sports Medicine 2017;47(1):61‐75. [DOI: 10.1007/s40279-016-0555-4; PUBMED: 27260683] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mikkilä 2005
- Mikkilä V, Räsänen L, Raitakari O, Pietinen P, Viikari J. Consistent dietary patterns identified from childhood to adulthood: the cardiovascular risk in young Finns study. British Journal of Nutrition 2005;93:923‐31. [DOI: 10.1079/BJN20051418] [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2015
- Morris H, Skouteris H, Edwards S, Rutherford L. Obesity prevention interventions in early childhood education and care settings with parental involvement: a systematic review. Early Child Development and Care 2015;185(8):1283–313. [DOI: 10.1080/03004430.2014.991723] [DOI] [Google Scholar]
Mozaffarian 2009
- Mozaffarian D, Aro A, Willett WC. Health effects of trans‐fatty acids: experimental and observational evidence. European Journal of Clinical Nutrition 2009;63(Suppl 2):S5‐21. [DOI: 10.1038/sj.ejcn.1602973; PUBMED: 19424218] [DOI] [PubMed] [Google Scholar]
Nader 1996
- Nader PR, Sellers DE, Johnson CC, Perry CL, Stone EJ, Cook KC, et al. The effect of adult participation in a school‐based family intervention to improve children's diet and physical activity: the Child and Adolescent Trial for Cardiovascular Health. Preventive Medicine 1996;25(4):455‐64. [DOI: 10.1006/pmed.1996.0077; PUBMED: 8818068] [DOI] [PubMed] [Google Scholar]
Nader 1999
- Nader PR, Stone EJ, Lytle LA, Perry CL, Osganian SK, Kelder S, et al. Three‐year maintenance of improved diet and physical activity: the CATCH cohort. Archives of Pediatrics & Adolescent Medicine 1999;153(7):695‐704. [DOI: 10.1001/archpedi.153.7.695; PUBMED: 10401802] [DOI] [PubMed] [Google Scholar]
National Research Council 2004
- National Research Council, Institute of Medicine. Children's Health, the Nation's Wealth: Assessing and Improving Child Health. Washington DC: National Academies Press, 2004. [Google Scholar]
NCD Countdown 2030 Collaborators 2018
- NCD Countdown 2030 Collaborators. NCD Countdown 2030: worldwide trends in non‐communicable disease mortality and progress towards Sustainable Development Goal target 3.4. The Lancet 2018;392(10152):1072‐88. [DOI: 10.1016/s0140-6736(18)31992-5; PUBMED: 30264707] [DOI] [PubMed] [Google Scholar]
NCT00987532
- NCT00987532. A participatory parental intervention promoting physical activity in preschools. clinicaltrials.gov/ct2/show/NCT00987532 (first received September 30, 2009).
NCT01588379
- NCT01588379. Mothers and girls dancing together trial (MAGNET) [Effects of an Afro‐centric dance program for African‐American daughters and mothers]. clinicaltrials.gov/ct2/show/NCT01588379 (first received April 25, 2012).
NCT02405611
- NCT02405611. A multi‐component intervention on improving fruit and vegetable consumption in teenagers and their mothers. clinicaltrials.gov/ct2/show/NCT02405611 (first received March 25, 2015).
NCT02491294
- NCT02491294. Fuel for fun: cooking with kids plus parents and play (FFF) [Cooking with kids 2.0: plus parents and play]. clinicaltrials.gov/ct2/show/NCT02491294 (first received July 1, 2015).
NCT03075085
- NCT03075085. Developing and testing implementation strategies for evidence‐based obesity prevention in childcare. clinicaltrials.gov/ct2/show/NCT03075085 (first received February 20, 2017).
NCT03111264
- NCT03111264. Building blocks for healthy preschoolers [Building blocks for healthy preschoolers: child care and family models]. clinicaltrials.gov/ct2/show/NCT03111264 (first received March 27, 2017).
NCT03590834
- NCT03590834. Míranos! program, a preschool obesity prevention RCT [Obesity prevention in Head Start: Míranos! program]. clinicaltrials.gov/ct2/show/NCT03590834 (first received June 27, 2018).
Ng 2014
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980‐2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384(9945):766–81. [DOI: 10.1016/S0140-6736(14)60460-8; PMC4624264; PUBMED: 24880830] [DOI] [PMC free article] [PubMed] [Google Scholar]
Niemeier 2012
- Niemeier BS, Hektner JM, Enger KB. Parent participation in weight‐related health interventions for children and adolescents: a systematic review and meta‐analysis. Preventive Medicine 2012;55(1):3‐13. [DOI: 10.1016/j.ypmed.2012.04.021; PUBMED: 22575353] [DOI] [PubMed] [Google Scholar]
Nocon 2008
- Nocon M, Hiemann T, Müller‐Riemenschneider F, Thalau F, Roll S, Willich S. Association of physical activity with all‐cause and cardiovascular mortality: a systematic review and meta‐analysis. European Journal of Cardiovascular Prevention and Rehabilitation 2008;15(3):239–46. [DOI: 10.1097/HJR.0b013e3282f55e09; PUBMED: 18525377] [DOI] [PubMed] [Google Scholar]
NTR3938
- NTR3938. Strengthening parenting styles and practices in existing interventions to prevent overweight and obesity in children [Strengthening parenting styles and practices in existing interventions to prevent overweight and obesity in children, a cluster randomized study]. www.trialregister.nl/trial/3752 (first received April 7, 2013).
O'Connor 2009
- O'Connor TM, Jago R, Baranowski T. Engaging parents to increase youth physical activity: a systematic review. American Journal of Preventive Medicine 2009;37(2):141‐9. [DOI: 10.1016/j.amepre.2009.04.020; PUBMED: 19589450] [DOI] [PubMed] [Google Scholar]
Olshansky 2005
- Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A potential decline in life expectancy in the United States in the 21st century. New England Journal of Medicine 2005;352(11):1138–45. [DOI: 10.1056/NEJMsr043743; PUBMED: 15784668] [DOI] [PubMed] [Google Scholar]
Pakpour 2019 [pers comm]
- Pakpour A. Queries about your HAPA intervention for adolescents [personal communication]. Email to E Morgan, November 11, 2019.
Patrick 2005
- Patrick H, Nicklas TA. A review of family and social determinants of children's eating patterns and diet quality. Journal of the American College of Nutrition 2005;24(2):83–92. [PUBMED: 15798074] [DOI] [PubMed] [Google Scholar]
Pearson 2009
- Pearson N, Biddle SJ, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutrition 2009;12(2):267‐83. [DOI: 10.1017/S1368980008002589; PUBMED: 18559129] [DOI] [PubMed] [Google Scholar]
Perry 1988b
- Perry CL, Luepker RV, Murray DM, Kurth C, Mullis R, Crocket S, et al. Parent involvement with children's health promotion: the Minnesota Home Team. American Journal of Public Health 1988;78(9):1156‐60. [PMC1349385; PUBMED: 3407811] [DOI] [PMC free article] [PubMed] [Google Scholar]
Perry 1989
- Perry CL, Luepker RV, Murray DM, Hearn MD, Halper A, Dudovitz B, et al. Parent involvement with children's health promotion: a one‐year follow‐up of the Minnesota home team. Health Education Quarterly 1989;16(2):171‐80. [PUBMED: 2732061] [DOI] [PubMed] [Google Scholar]
Perry 1992
- Perry CL, Parcel GS, Stone E, Nader P, McKinlay SM, Luepker RV, et al. The Child and Adolescent Trial for Cardiovascular Health (CATCH): overview of the intervention program and evaluation methods. Cardiovascular Risk Factors 1992;2(1):36‐44. [Google Scholar]
Perry 1997
- Perry CL, Sellers DE, Johnson C, Pedersen S, Bachman KJ, Parcel GS, et al. The Child and Adolescent Trial for Cardiovascular Health (CATCH): intervention, implementation, and feasibility for elementary schools in the United States. Health Education & Behavior 1997;24(6):716‐35. [DOI: 10.1177/109019819702400607; PUBMED: 9408786] [DOI] [PubMed] [Google Scholar]
Popkin 2013
- Popkin BM, Adair LS, Ng SW. Now and then: the global nutrition transition: the pandemic of obesity in developing countries. Nutrition Reviews 2013;70(1):3–21. [DOI: 10.1111/j.1753-4887.2011.00456.x; NIHMS336201; PMC3257829] [DOI] [PMC free article] [PubMed] [Google Scholar]
Powles 2013
- Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013;3(12):e003733. [DOI: 10.1136/bmjopen-2013-003733] [DOI] [PMC free article] [PubMed] [Google Scholar]
Puder 2010
- Puder JJ, Munsch S. Psychological correlates of childhood obesity. International Journal of Obesity 2010;34(Suppl 2):S37‐43. [DOI: 10.1038/ijo.2010.238; PUBMED: 21151145] [DOI] [PubMed] [Google Scholar]
Pulgarón 2014
- Pulgarón ER. Childhood obesity: a review of increased risk for physical and psychological co‐morbidities. Clinical Therapeutics 2014;35(1):A18‐32. [DOI: 10.1016/j.clinthera.2012.12.014; PUBMED: 21151145] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Roberto 2015
- Roberto CA, Swinburn B, Hawkes C, Huang TT‐K, Costa SA, Ashe M, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. The Lancet 2015;385(9985):2400‐9. [10.1016/ S0140‐6736(14)61744‐X; PUBMED: 25703111] [DOI] [PubMed] [Google Scholar]
Ruiter 2015b
- Ruiter EL, Fransen GA, Molleman GR, Velden K, Engels RC. The effectiveness of a web‐based Dutch parenting program to prevent overweight in children 9‐13 years of age: study protocol for a two‐armed cluster randomized controlled trial. BMC Public Health 2015;15:148. [DOI: 10.1186/s12889-015-1394-1; PMC4335372; PUBMED: 25884190] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rychetnik 2002
- Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. Journal of Epidemiology and Community Health 2002;56(2):119‐27. [DOI: 10.1136/jech.56.2.119; PMC1732065; PUBMED: 11812811] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sameroff 2010
- Sameroff A. A unified theory of development: a dialectic integration of nature and nurture. Child Development 2010;81(1):6‐22. [DOI: 10.1111/j.1467-8624.2009.01378.x; PUBMED: 20331651] [DOI] [PubMed] [Google Scholar]
Scaglioni 2011
- Scaglioni S, Arrizza C, Vecchi F, Tedeschi S. Determinants of children's eating behavior. American Journal of Clinical Nutrition 2011;94(Suppl 6):2006S‐11S. [DOI: 10.3945/ajcn.110.001685.1; PUBMED: 22089441] [DOI] [PubMed] [Google Scholar]
Schultz 2010
- Schultz KF, Altman DG, Moher D, Consort Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Medicine 2010;8:18. [DOI: 10.1186/1741-7015-8-18; PMC2860339; PUBMED: 20334633] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Sharma 2006
- Sharma M. School‐based interventions for childhood and adolescent obesity. Obesity Reviews 2006;7(3):261‐9. [DOI: 10.1111/j.1467-789X.2006.00227.x; PUBMED: 16866974] [DOI] [PubMed] [Google Scholar]
Simmonds 2016
- Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta‐analysis. Obesity Reviews 2016;17(2):95‐107. [DOI: 10.1111/obr.12334; PUBMED: 26696565] [DOI] [PubMed] [Google Scholar]
Skouteris 2011
- Skouteris H, McCabe M, Swinburn B, Newgreen V, Sacher P, Chadwick P. Parental influence and obesity prevention in pre‐schoolers: a systematic review of interventions. Obesity Reviews 2011;12(5):315–28. [DOI: 10.1111/j.1467-789X.2010.00751.x; PUBMED: 20492538] [DOI] [PubMed] [Google Scholar]
Smith 2015
- Smith L, Gardner B, Hamer M. Childhood correlates of adult TV viewing time: a 32‐year follow‐up of the 1970 British Cohort Study. Journal of Epidemiology and Community Health 2015;69(4):309‐13. [DOI: 10.1136/jech-2014-204365] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sofi 2008
- Sofi F, Capalbo A, Cesari F, Abbate R, Gensini GF. Physical activity during leisure time and primary prevention of coronary heart disease: an updated meta‐analysis of cohort studies. European Journal of Cardiovascular Prevention & Rehabilitation 2008;15(3):247–57. [DOI: 10.1097/HJR.0b013e3282f232ac; PUBMED: 18525378] [DOI] [PubMed] [Google Scholar]
Solorzano 2010
- Solorzano CMB, McCartney CR. Obesity and the pubertal transition in girls and boys. Reproduction 2010;140(3):399‐410. [DOI: 10.1530/REP-10-0119; PMC2931339; PUBMED: 20802107] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stalsberg 2010
- Stalsberg R, Pedersen AV. Effects of socioeconomic status on the physical activity in adolescents: a systematic review of the evidence. Scandinavian Journal of Medicine and Science in Sports 2010;20(3):368‐83. [DOI: 10.1111/j.1600-0838.2009.01047.x; PUBMED: 20136763] [DOI] [PubMed] [Google Scholar]
Stice 2006
- Stice E, Shaw H, Marti CN. A meta‐analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychological Bulletin 2006;132(5):667‐91. [DOI: 10.1037/0033-2909.132.5.667; NIHMS10196; PMC1876697] [DOI] [PMC free article] [PubMed] [Google Scholar]
Swindle 2017
- Swindle T, Johnson SL, Whiteside‐Mansell L, Curran GM. A mixed methods protocol for developing and testing implementation strategies for evidence‐based obesity prevention in childcare: a cluster randomized hybrid type III trial. Implemention Science 2017;12(1):90. [DOI: 10.1186/s13012-017-0624-6; NCT03075085; PMC5516351 ; PUBMED: 28720140] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tandon 2012
- Tandon PS, Zhou C, Sallis JF, Cain KL, Frank LD, Saelens BE. Home environment relationships with children's physical activity, sedentary time, and screen time by socioeconomic status. International Journal of Behavioral Nutrition and Physical Activity 2012;9:88. [DOI: 10.1186/1479-5868-9-88; PMC3413573; PUBMED: 22835155] [DOI] [PMC free article] [PubMed] [Google Scholar]
Teegala 2009
- Teegala SM, Willett WC, Mozaffarian D. Consumption and health effects of trans fatty acids: a review. Journal of AOAC International 2009;92(5):1250‐7. [PUBMED: 19916363] [PubMed] [Google Scholar]
Thune 2001
- Thune I, Furberg AS. Physical activity and cancer risk: dose‐response and cancer, all sites and site‐specific. Medicine and Science in Sports and Exercise 2001;33(6 Suppl):S530–50. [PUBMED: 11427781] [DOI] [PubMed] [Google Scholar]
Tremblay 2014
- Tremblay MS, Gray CE, Akinroye K, Harrington DM, Katzmarzyk PT, Lambert EV, et al. Physical activity of children: a global matrix of grades comparing 15 countries. Journal of Physical Activity and Health 2014;11(Suppl 1):S113‐25. [DOI: 10.1123/jpah.2014-0177; PUBMED: 25426906] [DOI] [PubMed] [Google Scholar]
Tzioumis 2014
- Tzioumis E, Adair LS. Childhood dual burden of under‐ and overnutrition in low‐ and middle‐income countries: a critical review. Food and Nutrition Bulletin 2014;35(2):230‐43. [PMC4313560; PUBMED: 25076771] [DOI] [PMC free article] [PubMed] [Google Scholar]
UN General Assembly 2012
- UN General Assembly. Political declaration of the high‐level meeting of the General Assembly on the prevention and control of non‐communicable diseases. www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf (accessed January 16, 2017).
United Nations 2015
- United Nations. Transforming our world: the 2030 agenda for sustainable development. sustainabledevelopment.un.org/post2015/transformingourworld/publication (accessed March 21, 2019).
Van Lippevelde 2012
- Lippevelde W, Verloigne M, Bourdeaudhuij I, Brug J, Bjelland M, Lien N, et al. Does parental involvement make a difference in school‐based nutrition and physical activity interventions? A systematic review of randomized controlled trials. International Journal of Public Health 2012;57(4):673‐8. [DOI: 10.1007/s00038-012-0335-3; PUBMED: 22301709] [DOI] [PubMed] [Google Scholar]
Vandongen 1995b
- Vandongen R, Jenner DA, Thompson C, Taggart AC, Spickett EE, Burke V, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10‐ to 12‐year‐old children. Preventive Medicine 1995;24(1):9‐22. [DOI: 10.1006/pmed.1995.1003; PUBMED: 7740021] [DOI] [PubMed] [Google Scholar]
Wang 2007b
- Wang C, Zhao H, Liu P, Ju P, He Z, Cong N. Effect of three ways of nutritional education on knowledge‐attitude‐behavior with nutrition in pupils. Wei Sheng Yan Jiu [Journal of Hygiene Research] 2007;36(1):85‐7. [PUBMED: 17424859] [PubMed] [Google Scholar]
Wang 2014
- Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose‐response meta‐analysis of prospective cohort studies. BMJ 2014;349:g4490. [DOI: 10.1136/bmj.g4490; PMC4115152; PUBMED: 25073782] [DOI] [PMC free article] [PubMed] [Google Scholar]
Waters 2011
- Waters E, Silva‐Sanigorski A, Burford BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD001871.pub3] [DOI] [PubMed] [Google Scholar]
Werch 2003b
- Werch C, Moore M, DiClemente CC, Owen DM, Jobli E, Bledsoe R. A sport‐based intervention for preventing alcohol use and promoting physical activity among adolescents. Journal of School Health 2003;73(10):380‐8. [PUBMED: 14727390] [DOI] [PubMed] [Google Scholar]
Werch 2018 [pers comm]
- Werch C. New customer message on May 17, 2018 at 02:00 PM [personal communication]. Email to E Morgan, May 17, 2018.
WHO 2003
- World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of the Joint WHO/FAO Expert Consultation. World Health Organization: Geneva, 2003. [Google Scholar]
WHO 2010
- WHO. Global recommendations on physical activity for health. www.who.int/dietphysicalactivity/global‐PA‐recs‐2010.pdf (accessed February 12, 2019).
WHO 2013
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013‐2020. Geneva: World Health Organization, 2013. [Google Scholar]
WHO 2016
- World Health Organization. Report of the Commission on Ending Childhood Obesity. Geneva: World Health Organization, 2016. [Google Scholar]
WHO 2018
- WHO. Healthy diet: key facts. www.who.int/news‐room/fact‐sheets/detail/healthy‐diet (accessed February 12, 2019).
WHO Multicentre Growth Reference Study Group 2006
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/height‐for‐age, Weight‐for‐age, Weight‐for‐length, Weight‐for‐height and Body Mass Index‐for‐age: Methods and Development. Geneva: World Health Organization, 2006. [PUBMED: 16817681] 16817681 [Google Scholar]
Wilkinson 2011
- Wilkinson RG, Pickett K. The Spirit Level: Why Greater Equality Makes Societies Stronger. London, UK: Bloomsbury Press, 2011. [Google Scholar]
Wilmot 2012
- Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta‐analysis. Diabetologia 2012;55(11):2895–905. [DOI: 10.1007/s00125-012-2677-z; PUBMED: 22890825] [DOI] [PubMed] [Google Scholar]
Wu 2015
- Wu S, Ding Y, Wu F, Li R, Hu Y, Hou J, et al. Socio‐economic position as an intervention against overweight and obesity in children: a systematic review and meta‐analysis. Scientific Reports 2015;5:11354. [DOI: 10.1038/srep11354; PMC4481703; PUBMED: 26112253] [DOI] [PMC free article] [PubMed] [Google Scholar]
Xi 2015
- Xi B, Huang Y, Reilly KH, Li S, Zheng R, Barrio‐Lopez MT, et al. Sugar‐sweetened beverages and risk of hypertension and CVD: a dose–response meta‐analysis. British Journal of Nutrition 2015;113(5):709‐17. [DOI: 10.1017/S0007114514004383; PUBMED: 25735740] [DOI] [PubMed] [Google Scholar]
Yavuz 2015
- Yavuz HM, Ijzendoorn MH, Mesman J, Veek S. Interventions aimed at reducing obesity in early childhood: a meta‐analysis of programs that involve parents. Journal of Child Psychology and Psychiatry 2015;56(6):677–92. [DOI: 10.1111/jcpp.12330; PUBMED: 25292319] [DOI] [PubMed] [Google Scholar]
Ye 2012
- Ye EQ, Chacko SA, Chou EL, Kugizaki M, Liu S. Greater whole‐grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. Journal of Nutrition 2012;142(7):1304–13. [DOI: 10.3945/jn.111.155325; PUBMED: 22649266] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yeh 2018b
- Yeh Y, Hartlieb KB, Danford C, Catherine Jen KL. Effectiveness of nutrition intervention in a selected group of overweight and obese African‐American preschoolers. Journal of Racial and Ethnic Health Disparities 2018;5(3):553‐61. [DOI: 10.1007/s40615-017-0399-0; PUBMED: 28699045 ] [DOI] [PubMed] [Google Scholar]
Yeh 2018c [pers comm]
- Yeh Y. Query re: Study at Head Start sites in Detroit [personal communication]. Email to E Morgan, August 18, 2018.
Yin 2019
- Yin Z, Ullevig SL, Sosa E, Liang Y, Olmstead T, Howard JT, et al. Study protocol for a cluster randomized controlled trial to test "¡Míranos! Look at Us, We Are Healthy!"—an early childhood obesity prevention program. BMC Pediatrics 2019;19(1):190. [DOI: 10.1186/s12887-019-1541-4; NCT03590834; PMC6556954 ; PUBMED: 31179916] [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2007
- Young KM, Northern JJ, Lister KM, Drummond JA, Brien WH. A meta‐analysis of family‐behavioral weight‐loss treatments for children. Clinical Psychology Review 2007;27(2):240‐9. [DOI: 10.1016/j.cpr.2006.08.003; PUBMED: 17070638] [DOI] [PubMed] [Google Scholar]
Zhao 2006
- Zhao H. Intervention Study on Improvement of Knowledge, Attitude and Practice With Calcium Nutrition in Pupil [Masters thesis]. Nanjing, JS: Southeast University, 2006. [Google Scholar]
Zucker 1995
- Zucker DM, Lakatos E, Webber LS, Murray DM, McKinlay SM, Feldman HA, et al. Statistical design of the Child and Adolescent Trial for Cardiovascular Health (CATCH): implications of cluster randomization. Controlled Clinical Trials 1995;16(2):96‐118. [PUBMED: 7789139] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Morgan 2017
- Morgan EH, Schoonees A, Faure M, Seguin RA. Caregiver involvement in interventions for improving children's dietary intake and physical activity behaviors. Cochrane Database of Systematic Reviews 2017, Issue 2. [DOI: 10.1002/14651858.CD012547] [DOI] [PMC free article] [PubMed] [Google Scholar]


