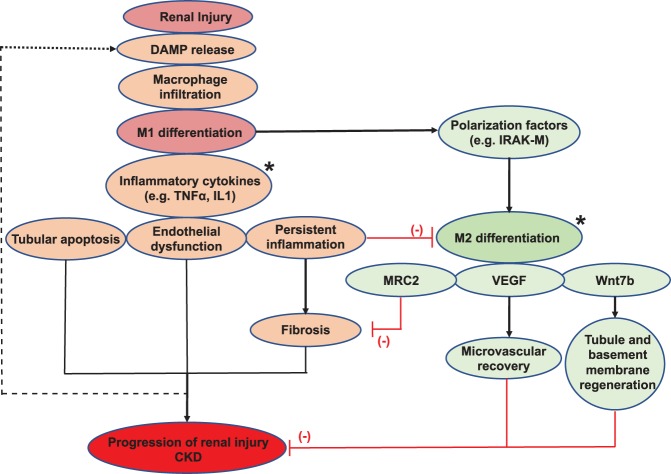
Fig. 1.
A schematic overview of macrophages in progression of renal injury. The initial renal damage leads to the release of chemotactic factors, inducing macrophage infiltration and subsequent differentiation to the M1 phenotype. M1 macrophages release multiple inflammatory cytokines, which drive tubular injury, endothelial dysfunction, and inflammation, leading to fibrosis and progression of renal injury toward chronic kidney disease (CKD) if left unchecked. In the normal course of healing, macrophages shift to the M2 phenotype and participate in the repair process through production of VEGF and Wnt7b (favoring microvascular recovery and parenchymal regeneration respectively, red lines) and surface expression of mannose receptor C type 2 (MRC2) to reduce the progression of fibrosis (red lines) and stimulate fibrolysis. M2 differentiation is favored by polarizing factors produced by M1 macrophages, such as IL-1 receptor-associated kinase M (IRAK-M), and inhibited by persistent inflammation favoring M1 polarization. Modulation of macrophage function or polarization state by genetic or cytokine approaches (*potential therapeutic targets) offers new potential therapeutic strategies for improving outcomes in kidney disease. DAMP, damage-associated molecular patterns.