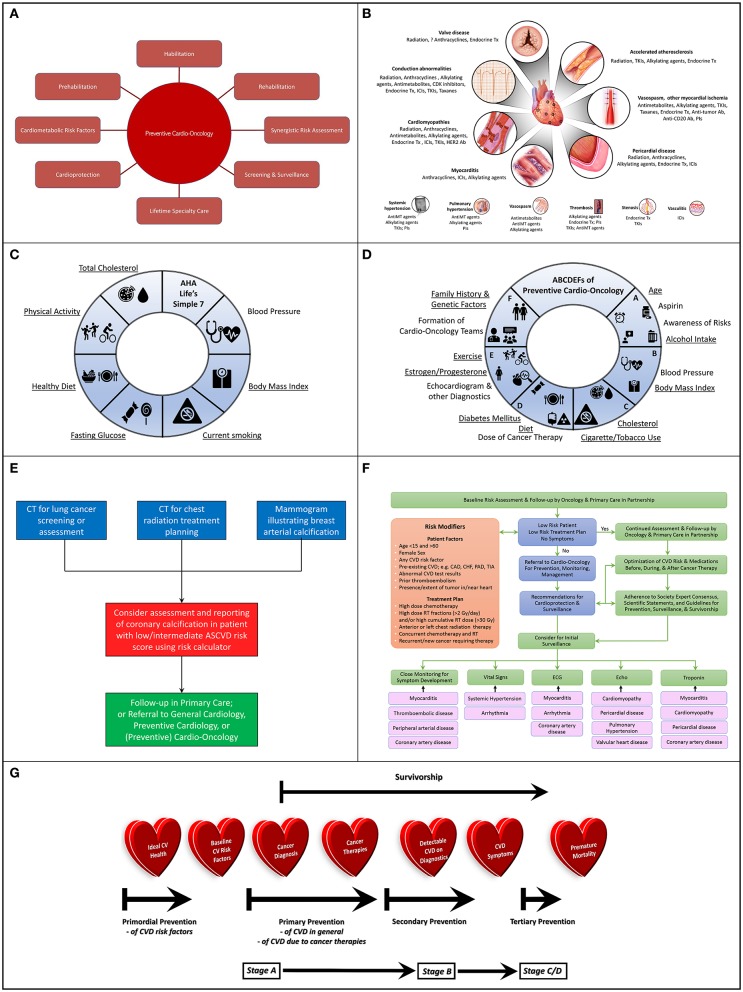
Figure 1.
(A) Potential Scope of Preventive Cardio-Oncology: Preventive Cardio-Oncology can potentially consist of prehabilitation, habilitation, and rehabilitation, with synergistic risk assessment in cardiology and oncology screening tests, as well as optimization of cardiometabolic risk factors (pre-existing, or consequential from cancer/therapies), in addition to adequate cardioprotection in the setting of cancer therapy, with appropriate screening and surveillance guided by lifetime specialty care. (B) Cardiovascular Toxic Effects of Cancer Therapies: A wide spectrum of cancer therapeutics can injure or aggravate a variety of components of the cardiac (top) and vascular (bottom) system, knowledge of which can assist with vigilant monitoring, prevention if possible, and appropriate diagnosis if present. (C) American Heart Association (AHA) Life's Simple 7: Seven different domains can guide conceptualization and realization of Ideal Cardiovascular Health, recognizing specific factors (underlined) that underlie risk of development of both CVD and cancer. (D) ABCDEFs of Preventive Cardio-Oncology: A proposed ABCDEF approach to prevention of CVD and cancer in the general population and in those with a prior history of cancer addresses all seven factors in the AHA Life's Simple 7, as well as other characteristics that can contribute to CVD, cancer (new or recurrent), or both (underlined), with expansion of a previously published ABCDE algorithm (1, 2) to include Family History and Genetic Factors and Formation of Cardio-Oncology Teams to prevent or mitigate the impact of these multiple hits and risk factors relevant to the development of CV toxicities from cancer therapies. (E) Algorithm for Synergistic Screening in Preventive Cardio-Oncology: Patients presenting for screening or assessment for cancer could also be considered for simultaneous or subsequent CV screening and reporting, particularly if the initial imaging test is of the chest, with radiology teams scheduling or reading chest x-rays or chest CTs contacting patients' ordering clinician to consider CV assessment and reporting in tandem, or with ordering clinician teams (primary care, oncology, cardiology, cardio-oncology, preventive cardio-oncology) also requesting assessment and reporting of CV findings when ordering chest x-rays or CTs for patients at low/intermediate risk for CVD, especially for patients with any previous cancers who received radiation therapy or chemotherapy with drugs that associate with coronary artery atherosclerosis or thrombosis. (F) Algorithm for Risk Assessment and Follow-up: Initial assessment of patients in oncology can occur with the oncologist in partnership with primary care, with those patients at low risk continuing to be followed predominantly in oncology and primary care, while other patients can be referred to (preventive) cardio-oncology for recommendations on additional screening and preventive measures prior to, during, and after cancer therapies, recognizing that close monitoring for symptoms, abnormal vitals, or findings on lab testing, ECG, or Echo can help guide the need for more advanced testing related to potential cardiotoxicities; various specific cardiotoxicities may benefit most from particular initial monitoring methods (black arrows), e.g., myocarditis from ICIs may first manifest with symptoms with or without changes in the ECG or troponin (which can further be assessed with cardiac MRI), while VEGFI toxicity most commonly manifests as hypertension; high risk determinants are adapted from (3). (G) Preventive Cardio-Oncology Paradigm Shift: Efforts at prevention in Cardio-Oncology may need to be shifted earlier than traditionally implemented or currently considered; in typical Preventive Cardiology, primordial prevention targets the general population prior to development of risk factors for CVD, such as hypertension or diabetes; primordial prevention in Preventive Cardio-Oncology, if truly merging Preventive Cardiology and Cardio-Oncology, could benefit from maintaining this place of primordial prevention on the prevention spectrum; as such, indeed, primordial prevention would remain in the general population before cancer is diagnosed; at the time of cancer diagnosis, individuals in the general population would then become cancer survivors, with a focus on primary prevention for those with CV risk factors, then secondary prevention following cancer therapy, especially once structural heart disease is visible on imaging and manifested with signs or symptoms; with advanced CVD, tertiary prevention would be in effect, in hopes to optimize quality while delaying premature mortality. CAD, coronary artery disease; CHF, congestive heart failure; CV, cardiovascular; CVD, cardiovascular disease; Echo, echocardiogram; ECG, electrocardiogram; Gy, Gray; ICIs, immune checkpoint inhibitors; PAD, peripheral artery disease; RT, radiation therapy; TIA, transient ischemic attack; VEGFI, vascular endothelial growth factor inhibitor (a tyrosine kinase inhibitor).