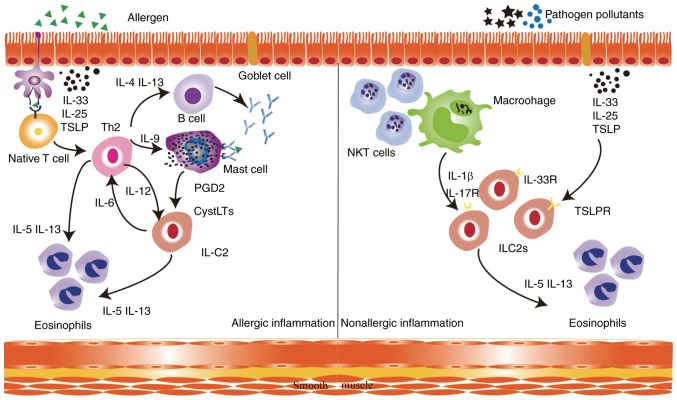
Figure 1.
Physiopathology of asthma. In allergic asthma, dendritic cells present allergens to naive T lymphocytes to induce Th2 cells, which produce IL-4 to induce IgE switching in B cells. The released IgE molecules bind to FceR1 on mast cell surfaces. CysLTs and PGD2, which are secreted by activated mast cells, are activators of ILC2s. ILC2s support Th2 cells by inducing a type 2 response, airway eosinophilia and mucous hypersecretion. In non-allergic eosinophilic asthma, air pollutants and pathogens induce the release of epithelium-derived and macrophage-derived cytokines, including IL-33, IL-25, TSLP and IL-1β, which activate ILC2s in an antigen-independent manner via their respective receptors. This leads to the secretion of type 2 cytokines by ILC2s, including high amounts of IL-5 and IL-13, which leads to eosinophilia, mucous hypersecretion and airway hyperreactivity. DC, dendritic cells; IL, interleukin; ILC2, type 2 innate lymphoid cell; IL-5R, interleukin 5 receptor; Th, T helper; CysLTs, cysteinyl leukotrienes; PDG2, prostaglandin D2.