Abstract
Objective
This study aimed to assess the prevalence and predictors of non-adherence to antihypertensive medication among patients with hypertension attending various healthcare settings in Islamabad, Pakistan.
Methods
A questionnaire-based cross-sectional study was conducted in selected healthcare facilities between September 2017 and December 2018. The study was conducted in primary, secondary and tertiary healthcare settings in Islamabad, Pakistan. Medication adherence was assessed using the eight-item Morisky Medication Adherence Scale (MMAS-8). Sociodemographic and clinical data of recruited patients were collected through a structured questionnaire. Binary logistic regression analysis was performed to determine covariates significantly associated with medication adherence and blood pressure control.
Results
A total of 776 hypertensive patients were invited and 741 (95%) completed the questionnaire. The mean ± SD age of participants was 53.6±12.6 years; 284 patients (38.3%) had high adherence, 178 (24%) had moderate adherence and 279 (37.7%) were non-adherent to the prescribed antihypertensive therapy. Binary regression analysis revealed that old age (OR 1.783 [95% CI: 1.172–2.712]; P=0.013), being educated (OR 2.018 [95% CI: 1.240–3.284]; P=0.036), entitlement to free medical care (OR 1.369 [95% CI: 1.009–1.859]; P=0.044), treatment duration (OR 2.868 [95% CI: 1.913–4.299]; P=0.001), number of medications (OR 1.973 [95% CI: 1.560–2.495]; P=0.001), presence of any comorbidity (OR 2.658 [95% CI: 1.836–3.848]; P=0.001) and blood pressure control (OR 3.103 [95% CI: 2.268–4.247]; P=0.001) were significantly associated with good adherence. Similarly, age (OR 1.998 [95% CI: 1.313–3.040]; P=0.004), entitlement to free medical care (OR 1.498 [95% CI: 1.116–2.010]; P=0.007), treatment duration (OR 1.886 [95% CI: 1.143–3.113]; P=0.013), presence of any comorbidity (OR 1.552 [95% CI: 1.123–2.147]; P=0.008) and adherence level (OR 3.103 [95% CI: 2.268–4.247]; P=0.001) had significant association with controlled blood pressure. The following were the main reasons for non-adherence to prescribed antihypertensive medication: “don’t feel need for regular use“ (24.7%), “Carelessness“ (13.4%) and “adverse effects“ (11.2%).
Conclusion
The prevalence of non-adherence to antihypertensive medications was high in the study population and poor medication adherence could potentially explain poor blood pressure control. Evidence-based targeted interventions on both medication adherence and blood pressure control should be introduced and implemented for better treatment outcomes.
Keywords: cross-sectional study, adherence, hypertension, Asia, antihypertensives, blood pressure control, Pakistan
Introduction
Hypertension is a significant global health challenge and a leading cause of morbidity and mortality. Persistently elevated blood pressure may lead to stroke, myocardial infarction, congestive heart failure, renal failure and blindness.1,2 In 2010, 1.3 billion people in the world were suffering from hypertension, with an annual increase rate of 2.5%.3 According to the World Health Organization (WHO) report published in 2013, the global prevalence of hypertension was 40%.4 Annually, 9.4 million people die from either hypertension or its related complications worldwide.4 Hypertension control is a significant healthcare challenge for both developing and developed countries. In Australia and the USA, the control rate for hypertension was 24% and 35%, respectively, in 2014–15.5 Hypertension control was even worse in Asia, with India and China having control rates of 7.9%6 and 5.7%,7 respectively. A meta-analysis published in 2018 in Pakistan revealed that the overall pooled prevalence of hypertension in Pakistan was 26.3% (25.93–26.75%); subgroup analysis revealed that the urban prevalence of hypertension was higher at 26.6% (21.80–31.42%) as compared to the rural prevalence at 21.1% (10.18–31.87%). Similarly, the pooled prevalence was 24.9% (19.70–30.28%) in males and 24.7% (16.76–32.76%) in females.8
Poor adherence is a critical barrier to treatment success9–11 leading to worsening of disease, increased hospitalization rate and longer hospital stays. The estimated overall global prevalence of non-adherence to antihypertensive therapy is around 30%.12 In the USA, 5% of avoidable hospital admissions are due to poor medication adherence,13 costing approximately $100 billion annually14 in the form of both direct and indirect losses.
Optimal adherence to prescribed antihypertensive therapy may result in substantial reductions in the incidence of myocardial infarction (20–25%), heart failure (>50%) and stroke (35–40%).15,16 Various barriers to antihypertensive medication adherence have been previously identified and reported in the literature. These include cost of medication, lack of education, forgetfulness, unavailability, too much medication, fear of addiction and possible side effects, and dissatisfaction with the therapy.17 Therefore, addressing these barriers is necessary to improve medication adherence.
This study aims to evaluate and compare the degree of medication adherence in hypertensive patients in primary, secondary and tertiary healthcare settings in Islamabad. Previously, three studies were conducted in different tertiary care hospitals in Pakistan to evaluate adherence to medication in hypertensive patients. Of these three studies, two used unvalidated questionnaires to assess medication adherence and had too small sample sizes to draw any meaningful conclusions.18,19 The largest study of the three was conducted in 2005 in the city of Karachi in a large tertiary care private hospital, and consisted of 460 hypertensive patients. The Morisky, Green, Levine Medication Adherence Questionnaire20 was used to assess adherence.17 Hypertension is managed primarily in primary care. In Pakistan, 85% of patients visit primary healthcare facilities for treatment, whereas only 15% of patients visit tertiary care hospitals.21,22 To date, no study has been conducted in Pakistan to assess the degree of medication adherence among hypertensive patients attending primary and secondary care. To fill this research gap, this study was designed to gather a better understanding of the prevalence of and barriers to medication adherence across all three tiers (primary, secondary and tertiary) of Pakistan's healthcare system. The results of this study could inform policy makers to help develop policies with the aim of improving medication adherence for hypertensive patients in Pakistan.
Materials and Methods
Ethics Statement
The study was approved by Quaid-i-Azam University Bioethics Committee (vide letter no. BFC-FBS-QAU-2018-108 dated 23/10/2018.) In addition, ethical approval was obtained from the bioethical committees/administrations of the respective healthcare settings where the study was conducted (vide letter no. F.1-1/2015/ERB/SZABMU dated 28/08/2017 and no. CDA/DHS-14(1) (63)/2018/1077 dated: 09/10/2018). A licensing agreement to use the copyrighted MMAS-8 was obtained from Donald E. Morisky (294 Lindura Court, Las Vegas, NV 89138-4632, USA; dmorisky@gmail.com). Both informed and written consent was sought from each participant using a consent form before enrollment in the study. Survey confidentiality and anonymity were assured to all enrolled participants.
Study Settings
This was a multicentre study conducted in one primary, one secondary and one tertiary healthcare setting in Islamabad, the capital of Pakistan. This study was conducted in all three tiers of Pakistan’s healthcare system to enable generalization of the data to the Pakistani population.
Study Design and Participants
This was a cross-sectional study including 741 hypertensive patients. The study took place between September 2017 and December 2018. Eligibility criteria included: all patients who were diagnosed with essential hypertension at any time; aged 18 years and above; on at least one antihypertensive medication for the past 6 months; able to communicate in Urdu language; and attending one of the participating healthcare facilities. Hypertensive patients with other comorbidities were also included in our study. Pregnant women, patients with mental disorders such as dementia, and those who could not communicate in Urdu, which is the national language of Pakistan, were not included in this study.
Data Collection
To assess medication adherence, the Urdu version of the eight-item Morisky Medication Adherence Scale (MMAS-8) was used.23–25 Since Urdu is the national language and is the most widely spoken and understood language in Pakistan, a validated Urdu translation of MMAS-826 was used to measure medication adherence. The MMAS-8 score can range between 0 and 8. Participants who scored 8 on MMAS-8 were considered “adherent”, participants with a score between 6 and <8 were considered “moderately adherent” and participants with an MMAS-8 score <6 were considered “non-adherent” to their prescribed therapy.25 A separate standardized data collection form was used to gather patients' sociodemographic data, medical and medication history, and reason for non-adherence. The questionnaires were piloted on 50 patients to test the acceptability of the questions.
Outcome Measures and Covariates
The primary and secondary outcome measures were optimal medication adherence and optimal blood pressure control, respectively. The target for controlled blood pressure was defined in accordance with NICE treatment guidelines for the management of hypertension 2011.27 For patients who were under 80 years of age, blood pressure <140/90 mmHg was considered controlled, whereas for patients aged 80 years or above, blood pressure <150/90 mmHg was considered controlled. Similarly, for the patients with both hypertension and diabetes mellitus, blood pressure <140/80 mmHg, and for patients with kidney, eye and cerebrovascular damage, blood pressure <130/80 mmHg was considered controlled. The covariates were age, gender, entitlement status, marital status, level of education, profession, smoking, number of antihypertensive medications used, duration of therapy and presence of comorbidities.
Statistical Analysis
Statistical analyses were performed using SPSS version 21.0. The alpha level of significance for all statistical tests was 0.05. Binary logistic regression analysis using the default entry method was conducted to identify predictors associated with medication adherence and blood pressure control. For the purposes of binary regression analysis, the patients were divided into two categories, ie either adherent or non-adherent, rather than three categories, ie good adherence, moderate adherence and non-adherence, on the basis of their MMAS-8 score. Patients who had an MMAS-8 score ≥6 were categorized as adherent and patients who had an MMAS-8 score <6 were categorized as non-adherent. Correlation and Hosmer–Lemeshow Goodness of Fit tests were performed to select the best prediction model.
Results
Patient Characteristics
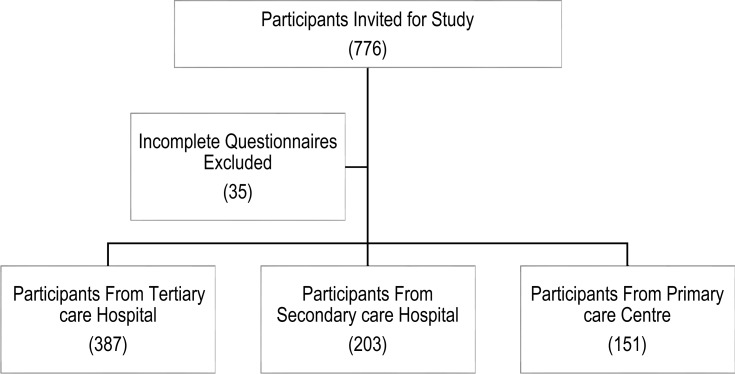
A total of 768 hypertensive patients using at least one antihypertensive medication were invited to participate, of whom 741 patients participated in the study (Figure 1). Of these 741 patients, 389 (52.5%) were male and 352 (47.5%) were female. The mean age of participants was 53.6±12.6 years. More than one-third of the participants (286, 38.6%) were obese. At least one comorbidity was present in 205 patients (27.7%) (Table 1). The majority of participants were on a single antihypertensive drug (303, 40.9%) and the mean number of antihypertensive medications used was 1.7. The mean duration of therapy was 5.7 years and the majority of participants had a duration of therapy <5 years (498, 67.2%). The mean MMAS-8 score was 6.17±1.8; 462 patients (62.3%) scored >6 and adherence was categorized as either good or moderate, whereas 279 patients (37.6%) scored <6 and were categorized as poor adherents. The mean systolic blood pressure was 148±18.6 mmHg and mean diastolic blood pressure was 92±10.7 mmHg. The mean systolic blood pressure was 145±19 mmHg in patients with good medication adherence, 148±18 mmHg in patients with moderate adherence and 152±18 mmHg in patients with low medication adherence. Similarly, the mean diastolic blood pressure was 90±11 mmHg in patients with good medication adherence, 92±11 mmHg in patients with moderate adherence and 95±10 mmHg in patients with low medication adherence (Table 2).
Figure 1.
Flowchart showing the participants from each healthcare setting.
Table 1.
Characteristics of Patients Included in This Study
| Patient Characteristics | Total Study Population (N=741) | ||
|---|---|---|---|
| N | % | ||
| Gender | Male | 389 | 52.5 |
| Female | 352 | 47.5 | |
| Age | Mean ± SD | 53.6±12.6 | |
| ≥60 years | 256 | 34.5. | |
| 40–59 years | 343 | 46.3 | |
| ≤40 years | 142 | 19.2 | |
| Marital status | Married | 632 | 85.3 |
| Unmarried/divorced/widowed | 109 | 14.7 | |
| BMI | Overweight | 286 | 38.6 |
| Normal | 411 | 55.5 | |
| Underweight | 44 | 5.9 | |
| Smoking | Non-smokers | 585 | 78.9 |
| Smokers | 104 | 14 | |
| Ex-smokers | 52 | 7 | |
| Educational level | Graduate and above | 122 | 16.5 |
| Secondary and higher secondary | 262 | 35.4 | |
| Primary and below | 163 | 22 | |
| Uneducated | 194 | 26.2 | |
| Profession | Officers/higher management | 78 | 10.5 |
| Clerical staff | 62 | 8.4 | |
| Workers/labourers | 148 | 20 | |
| Self-employed | 15 | 2 | |
| Retired/unemployed | 140 | 18.9 | |
| Housewives | 298 | 40.2 | |
| Entitlement status | Entitled | 303 | 40.9 |
| Non-entitled | 438 | 59.1 | |
| Treatment duration | Mean ± SD | 5.7±5.9 | |
| ≤5 years | 498 | 67.2 | |
| 6–9 years | 73 | 9.9 | |
| ≥10 years | 170 | 22.9 | |
| No. of antihypertensive drugs | Mean ± SD | 1.7±0.68 | |
| 1 | 303 | 40.9 | |
| 2 | 340 | 45.9 | |
| 3 | 97 | 13.1 | |
| 4 | 1 | 0.1 | |
| Comorbidity | Yes | 536 | 72.3 |
| No | 205 | 27.7 | |
| Specific comorbidity | Patients with DM | 125 | 16.9 |
| Patients with CHD | 63 | 8.50 | |
| Patients with CHF | 06 | 0.80 | |
| Patients with hyperlipidaemia | 169 | 22.8 | |
| Blood pressure | Controlled | 357 | 48.2 |
| Uncontrolled | 384 | 51.8 | |
Abbreviations: BMI, body mass index; DM, diabetes mellitus; CHD, coronary heart disease; CHF, congestive heart failure.
Table 2.
Mean SBP and DBP Stratified by Adherence Level
| Adherence Level | Mean SBP (mmHg) | Mean DBP (mmHg) |
|---|---|---|
| Good adherence | 145±19 | 90±11 |
| Moderate adherence | 148±18 | 92±11 |
| Low adherence | 152±18 | 95±10 |
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure.
Factors Associated with Medication Adherence
Patients were categorized into adherent, moderately adherent and non-adherent on the basis of their MMAS-8 score. In terms of level of care, univariate analysis found that patients attending the tertiary care hospital had a higher rate of medication adherence (169/387, 43.6%) compared to secondary care (79/203, 38.90%) and the primary care centre (36/151, 23.8%) (Table 3).
Table 3.
Medication Adherence Level in Different Healthcare Settings
| Healthcare Setting | No. of Patients, N | Adherent, N (%) | Moderate Adherence, N (%) | Non-Adherence, N (%) |
|---|---|---|---|---|
| Tertiary care hospital | 387 | 169 (43.66) | 90 (23.26) | 128 (33.07) |
| Secondary care hospital | 203 | 79 (38.90) | 47 (23.15) | 77 (37.93) |
| Primary care centre | 151 | 36 (23.8) | 41 (27.15) | 74 (49.0) |
| Overall | 741 | 284 (38.3) | 178 (24.0) | 279 (37.7) |
Notes: The level of adherence was measured through the eight-item Morisky Medication Adherence Scale (MMAS-8). Use of the MMAS is protected by US copyright laws. Permission for use is required. A licensing agreement is available from: Donald E. Morisky, ScD, ScM, MSPH. Use of the ©MMAS is protected by US copyright and registered trademark laws. Permission for use is required. A licensing agreement is available from: Donald E. Morisky, 294 Lindura Court, Las Vegas, NV 89138-4632; dmorisky@gmail.com. The scale’s questions are available in the originally published article.23
Table 4 shows the results of binary regression analysis for factors predicting medication adherence. Older age (OR 1.783 [95% CI: 1.172–2.712]), being educated (OR 2.018 [95% CI: 1.240–3.284]) and longer treatment duration increased the odds of being adherent (OR 2.868 [95% CI: 1.913–4.299]). Married patients were more likely to be adherent to the antihypertensive therapy than unmarried/divorced/widowed patients (OR 1.25 [95% CI: 0.827–1.890]). Patients who were entitled to free medical care were more likely to be adherent to prescribed antihypertensive therapy than patients who were non-entitled (OR 1.369 [95% CI: 1.009–1.859]). The odds of being adherent increased by 1.973 [95% CI: 1.560–2.495] times with every unit increase in number of antihypertensive medications. Similarly, patients who had comorbidity were more likely to be adherent to the antihypertensive therapy than the patients who had no comorbidity (OR 2.658 [95% CI: 1.836–3.848]). Patients with controlled blood pressure were three times more likely to be adherent than those with uncontrolled blood pressure (OR 3.103 [95% CI: 2.268–4.247]). Male patients were more likely to be adherent than female patients (OR 1.134 [95% CI: 0.842–1.527]).
Table 4.
Binary Logistic Regression Analysis for Factors Predicting Medication Adherence
| Parameter | Non-Adherent, N (%) | Adherent, N (%) | OR | 95% CI for OR Lower–Upper |
P-value |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 138 (39.2) | 214 (60.8) | 1 | ||
| Male | 141 (36.2) | 248 (63.8) | 1.134 | 0.842–1.527 | 0.407 |
| Age | |||||
| 18–40 years | 68 (48.6) | 72 (51.4) | 1 | ||
| 41–59 years | 122 (35.5) | 222 (64.5) | 1.719 | 1.154–2.559 | |
| ≥60 years | 89 (34.6) | 168 (65.4) | 1.783 | 1.172–2.712 | 0.013* |
| Marital status | |||||
| Married | 233 (36.9) | 399 (63.1) | 1 | ||
| Unmarried/divorced/widowed | 46 (42.2) | 63 (57.8) | 0.800 | 0.529–1.209 | 0.289 |
| Educational level | |||||
| Uneducated | 85 (43.8) | 109 (56.2) | 1 | ||
| Primary or below | 65 (39.9) | 98 (60.1) | 1.176 | 0.770–1.794 | |
| Secondary and higher secondary | 95 (36.3) | 167 (63.7) | 1.371 | 0.938–2.003 | |
| Graduate and above | 34 (27.9) | 88 (72.1) | 2.018 | 1.240–3.284 | 0.036* |
| BMI | |||||
| Obese | 109 (38.1) | 177 (61.9) | 1 | ||
| Normal weight | 157 (38.2) | 254 (61.8) | 0.996 | 0.730–1.359 | |
| Underweight | 13 (29.5) | 31 (70.5) | 1.468 | 0.736–2.928 | 0.523 |
| Profession | |||||
| Retired/unemployed | 53 (37.9) | 87 (62.1) | 1 | ||
| Housewives | 113 (37.9) | 185 (62.1) | 1.003 | 0.663–1.517 | |
| Officers | 23 (29.5) | 55 (70.5) | 1.461 | 0.851–2.507 | |
| Clerical staff | 23 (37.1) | 39 (62.9) | 1.036 | 0.588–1.824 | |
| Worker/labourer | 58 (39.2) | 90 (60.8) | 0.948 | 0.632–1.420 | |
| Self-employed | 9 (60) | 6 (40) | 0.407 | 0.141–1.174 | 0.376 |
| Entitlement status | |||||
| Non-entitled | 178 (40.6) | 260 (59.4) | 1 | ||
| Entitled | 101 (33.3) | 202 (66.7) | 1.369 | 1.009–1.859 | 0.044* |
| Smoking status | |||||
| Non-smoker | 222 (37.9) | 363 (62.1) | 1 | ||
| Smoker | 40 (38.5) | 64 (61.5) | 0.979 | 0.637–1.503 | |
| Ex-smoker | 17 (32.7) | 35 (67.3) | 1.259 | 0.689–2.301 | 0.743 |
| Treatment duration | |||||
| ≤5 years | 221 (44.4) | 277 (55.6) | 1 | ||
| 6–9 years | 21 (28.8) | 52 (71.2) | 1.976 | 1.155–3.379 | |
| ≥10 years | 37 (21.8) | 133 (78.2) | 2.868 | 1.913–4.299 | 0.0001* |
| No. of medications | |||||
| 1 | 151 (49.8) | 152 (50.2) | |||
| 2 | 107 (31.5) | 233 (68.5) | |||
| 3 | 20 (20.6) | 77 (79.4) | 1.973 | 1.560–2.495 | 0.0001* |
| Comorbidities | |||||
| No | 233 (43.5) | 303 (56.5) | 1 | ||
| Yes | 46 (22.4) | 159 (77.6) | 2.658 | 1.836–3.848 | 0.0001* |
| BP control | |||||
| Uncontrolled | 192 (50.0) | 192 (50.0) | 1 | ||
| Controlled | 87 (24.4) | 270 (75.6) | 3.103 | 2.268–4.247 | 0.0001* |
Note: *P<0.05.
Abbreviations: BMI, body mass index; BP, blood pressure.
Factors Associated with Optimal Blood Pressure Control
Univariate analysis revealed that the rate of blood pressure control was 63.7% among patients who had high medication adherence, compared to 50% among patients with moderate adherence and 31.2% among patients who had low adherence to prescribed antihypertensive medication (Table 5). The rate of blood pressure control was 44% in patients attending the tertiary care hospital, 56% in patients attending the secondary care hospital and 49% in patients attending the primary healthcare setting. The overall rate of blood pressure control was 48% (Table 6).
Table 5.
Adherence Level Among Hypertensive Patients Stratified by Blood Pressure Control
| Adherence Level | Blood Pressure | Total Study Population | ||
|---|---|---|---|---|
| N | % | Total (%) | ||
| High adherence | Controlled | 181 | 63.7 | 284 (38.3) |
| Uncontrolled | 103 | 36.3 | ||
| Moderate adherence | Controlled | 89 | 50 | 178 (24) |
| Uncontrolled | 89 | 50 | ||
| Low adherence | Controlled | 87 | 31.2 | 279 (37.7) |
| Uncontrolled | 192 | 68.8 | ||
Table 6.
Level of Blood Pressure Control in Different Healthcare Settings
| Healthcare Setting | Total No. of Patients | BP Controlled BP, N (%) | % | Uncontrolled BP, N (%) | % |
|---|---|---|---|---|---|
| Tertiary care hospital | 387 | 169 (44) | 44 | 218 (56) | 56 |
| Secondary care hospital | 203 | 113 (56) | 56 | 90 (44) | 44 |
| Primary care centre | 151 | 74 (49) | 49 | 77 (51) | 51 |
| Overall | 741 | 356 (48) | 48 | 385 (52) | 52 |
Abbreviation: BP, blood pressure.
The results of binary regression analysis showed that age, entitlement status for free medical care, treatment duration, presence of any comorbidity and adherence level had significant associations with controlled blood pressure. The results of binary regression analysis further revealed that the odds of controlled blood pressure were approximately three times greater in patients who were adherent to their prescribed antihypertensive therapy than in patients who were non-adherent (OR 3.103 [95% CI: 2.268–4.247]). Similarly, the odds of controlled blood pressure were 1.179 times greater in males than in females (OR 1.179 [95% CI: 0.883–1.574]). Older age (≥60 years) (OR 1.998 [95% CI: 1.313–3.040]), being educated (OR 1.5 [95% CI: 0.956–2.377]), being an officer (OR 1.5 [95% CI: 0.923–2.516]) and longer treatment duration (OR 1.4 [95% CI: 1.010–2.031]) increased the odds of controlled blood pressure. The odds of controlled blood pressure were 1.213 times greater in unmarried/divorced/widowed patients than in married patients (OR 1.213 [95% CI: 0.807–1.822]). The odds of controlled blood pressure were 1.5 times greater in patients who had entitlement to free medical care than in who did not have entitlement to free medical care (OR 1.498 [95% CI: 1.116–2.010]). The number of medications had an inverse relationship with controlled blood pressure with every unit increase in number of medications (OR 0.884 [95% CI: 0.716–1.091]). The odds of controlled blood pressure were 1.5 times greater in patients who had comorbidity than in patients who had no comorbidity (OR 1.552 [95% CI: 1.123–2.147]) (Table 7).
Table 7.
Binary Logistic Regression Analysis for Factors Predicting Controlled Blood Pressure
| Parameter | Uncontrolled BP, N (%) | Controlled BP, N (%) | OR | 95% CI for OR Lower-Upper | P-value |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 190 (54.0) | 162 (46.0) | 1 | ||
| Male | 194 (49.9) | 195 (50.1) | 1.179 | 0.883–1.574 | 0.264 |
| Age | |||||
| 18–40 years | 86 (61.4) | 54 (38.6) | 1 | ||
| 41–59 years | 184 (53.5) | 160 (46.6) | 1.385 | 0.927–2.068 | |
| ≥60 years | 114 (44.4) | 143 (55.6) | 1.998 | 1.313–3.040 | 0.004* |
| Marital status | |||||
| Married | 332 (52.5) | 300 (47.5) | 1 | ||
| Unmarried/divorced/widowed | 52 (47.7) | 57 (52.3) | 1.213 | 0.807–1.822 | 0.352 |
| Education | |||||
| Uneducated | 112 (57.7) | 82 (42.3) | 1 | ||
| Primary or below | 79 (48.5) | 84 (51.5) | 1.452 | 0.955–2.208 | |
| Secondary and higher secondary | 135 (51.5) | 127 (48.5) | 1.285 | 0.884–1.868 | |
| Graduate and above | 58 (47.5) | 64 (52.5) | 1.507 | 0.956–2.377 | 0.227 |
| BMI | |||||
| Obese | 152 (53.1) | 134 (46.9) | 1 | ||
| Normal weight | 216 (52.6) | 195 (47.4) | 1.024 | 0.757–1.386 | |
| Underweight | 16 (36.4) | 28 (63.6) | 1.985 | 1.029–3.828 | 0.113 |
| Profession | |||||
| Housewives | 165 (55.4) | 133 (44.6) | 1 | ||
| Officers | 35 (44.9) | 43 (55.1) | 1.524 | 0.923–2.516 | |
| Clerical staff | 33 (53.2) | 29 (46.8) | 1.090 | 0.630–1.887 | |
| Worker/labourer | 77 (52.0) | 71 (48.0) | 1.144 | 0.771–1.698 | |
| Retired/unemployed | 65 (46.4) | 75 (53.6) | 1.431 | 0.957–2.142 | |
| Self-employed | 9 (60.0) | 6 (40.0) | 0.827 | 0.287–2.382 | 0.407 |
| Entitlement status | |||||
| Non-entitled | 245 (55.9) | 193 (44.1) | 1 | ||
| Entitled | 139 (45.9) | 164 (54.1) | 1.498 | 1.116–2.010 | 0.007* |
| Smoking status | |||||
| Non-smoker | 301 (51.5) | 284 (48.5) | 1 | ||
| Smoker | 58 (55.8) | 46 (44.2) | 0.841 | 0.553–1.279 | |
| Ex-smoker | 25 (48.1) | 27 (51.9) | 1.145 | 0.649–2.019 | 0.615 |
| Treatment duration | |||||
| ≤5 years | 276 (55.4) | 222 (44.6) | 1 | ||
| 6–9 years | 29 (39.7) | 44 (60.3) | 1.886 | 1.143–3.113 | |
| ≥10 years | 79 (46.5) | 91 (53.5) | 1.432 | 1.010–2.031 | 0.013* |
| No. of medications | |||||
| 1 | 156 (51.5) | 147 (48.5) | |||
| 2 | 168 (49.4) | 172 (50.6) | |||
| 3 | 59 (60.8) | 38 (39.2) | 0.884 | 0.716–1.091 | 0.250 |
| Comorbidities | |||||
| No | 294 (54.9) | 242 (45.1) | 1 | ||
| Yes | 90 (43.9) | 115 (56.1) | 1.552 | 1.123–2.147 | 0.008* |
| Medication adherence level | |||||
| Non-adherent | 192 (68.8) | 87 (31.2) | 1 | ||
| Adherent | 192 (41.6) | 270 (58.4 | 3.103 | 2.268–4.247 | 0.0001* |
Note: *P<0.05.
Abbreviations: BMI, body mass index; BP, blood pressure.
Reasons for Non-Adherence/Moderate Adherence
Multiple reasons for moderate/non-adherence were reported by the patients. Of 457 hypertensive patients, 408 (89%) who had either moderate adherence or non-adherence responded to the question on the reasons for non-adherence. About one-quarter of the patients (24.7%) responded that they “don’t feel a need for regular use” as they take their medicines only when they feel any symptom of hypertension. Carelessness was the second most frequently cited reason for moderate/non-adherence (13.4%). Adverse effects to antihypertensive medications were also cited by 46 patients (11.2%) (Table 8).
Table 8.
Reasons “In Patient’s View” for Either Non-Adherence or Moderate Adherence to Prescribed Antihypertensive Therapy
| Sr. | Reason | n (%) |
|---|---|---|
| No. of Respondents (n=408) | ||
| 1 | Don't feel need for regular use | 101 (24.7) |
| 2 | Carelessness | 55 (13.4) |
| 3 | Adverse effect | 46 (11.2) |
| 4 | Forgetfulness | 40 (9.8) |
| 5 | Lack of education | 40 (9.8) |
| 6 | Travelling | 35 (8.6) |
| 7 | Tired of taking medication | 31 (7.6) |
| 8 | Fear of addiction | 24 (5.9) |
| 9 | Unaffordable | 19 (4.7) |
| 10 | Unavailability | 16 (3.9) |
Discussion
Medication adherence, predictors of medication adherence and its association with controlled blood pressure, as well as the reasons for medication non-adherence, were investigated in this study. Patient groups with poor blood pressure control were identified. This study could potentially help medical practitioners to design patient-specific interventions targeting these patients, including patient counselling, providing entitlement to free medical care and helping policy makers develop policies to ensure better therapeutic outcomes. Overall, 37.7% of hypertensive patients attending primary, secondary and tertiary healthcare settings in Islamabad were non-adherent. There was a significant association between medication adherence and blood pressure control. “Don’t feel need for regular use”, “Carelessness” and “adverse effects” were the main reasons for non-adherence among hypertensive patients.
Previous studies conducted in Pakistan have reported higher rates of non-adherence to antihypertensive therapy, ranging between 51% and 82%18,19, compared to our study. This difference may be due to the use of unvalidated questionnaires to assess medication adherence and very small sample sizes (89 and 32). The use of unvalidated questionnaires may have resulted in overestimation of non-adherence. However, one study, conducted in the metropolitan city of Karachi, Pakistan,17 was the only research study that used a validated questionnaire, ie the Morisky, Green, Levine Medication Adherence Questionnaire. Our study reported less medication adherence than was reported in the previous study conducted in Karachi, ie 77%. This difference may be due to the different methods used to estimate adherence, as it has been reported in a meta-analysis that MMAS-8 reports less adherence compared to other questionnaires used for the estimation of medication adherence. This is because MMAS-8 makes it possible to obtain a more in-depth picture of adherence, where the participants do not feel forced to claim to be adherent.28 Various studies conducted in different Asian countries, ie China, Hong Kong, Saudi Arabia, UAE and Iran, using MMAS-8 have also reported similar poor adherence to prescribed antihypertensive therapy, supporting our results.15,29–35
The WHO estimates the prevalence of non-adherence among patients with chronic diseases to be between 52% and 74%, defined by ≥80% cut-off.36
In this study, we found no significant correlation between gender and medication adherence. This finding is consistent with previously reported studies, including a study in Pakistan.17,30,31,37,38 In contrast, there are studies that have found a significant correlation between gender and medication adherence.29,32 Age was found to be significantly associated with medication adherence in our study, with better adherence observed in older patients. This finding is consistent with another study from Pakistan,17 as well as with a number of international studies.29,39–42 However, other studies have shown either no correlation with age43,44 or an inverse correlation with increasing age when it comes to the use of antihypertensives.45
In our opinion, this negative correlation may be due to loss of memory, non-availability of any caregiver or deteriorated health of the patients. On the other hand, the increased medication adherence in older patients may be due to either increased severity of the condition, which forced the patient to be adherent, or strong family support for older people in Pakistani society. Studies have reported a positive relationship between family support and medication adherence.46,47
The level of education of the participants was also found to be significantly associated with medication adherence in our study. There was a positive correlation between medication adherence and the level of education. This is in contrast to what has been reported previously in studies conducted in different Asian countries, as most of the previous studies using MMAS-8 have found no significant correlation between level of education and medication adherence.17,29–31,37 Increased medication adherence in educated patients may be due to increased awareness about the disease. This is in line with previous research which showed the significant relationship between formal education and medication adherence.48,49
The number of medications had a significant correlation with medication adherence. Medication adherence increases when the patient is using more than one medication to control blood pressure. This finding is in contrast to previously reported studies, which found no significant correlation between number of medications and medicationadherence.17,29–31,37,38 In our opinion, the increased medication adherence in patients who use more than one medication to control their blood pressure may be due to an increased severity of symptoms in these patients, which compels these patients to remain adherent with their prescribed medications.
Similarly, presence of comorbidity also had strong a correlation with medication adherence. Mixed findings have been reported in the literature regarding the association between presence of comorbidity and medication adherence. Some studies support our finding,29,38 whereas other studies found no significant correlation between presence of comorbidity and medication adherence.17,31,37 No significant correlation was found between gender, marital status, BMI, smoking or employment status and medication adherence.
For blood pressure control, the age of the patient was found to have a significant correlation with controlled blood pressure. We found that patients aged ≥60 years had better blood pressure control than patients who were under 60 years of age. This finding is in contrast to previously reported studies, which found the opposite result.29,50 This better control of blood pressure could be due to better medication adherence in elderly patients and increased self-care in old age.
This study also highlighted various self-reported reasons for medication non-adherence/moderate adherence among Pakistani patients. These reasons included “no need for regular use”, carelessness, adverse effects of medication, forgetfulness, lack of education, travelling, tired of taking medicines, fear of addiction, unaffordability and unavailability. A previous study, also conducted in Pakistan, reported misperception, no need for medications, ineffectiveness, forgetfulness, unavailability and adverse effects of medications as the main reasons for non-adherence in hypertensive patients.19 A study conducted in India revealed that forgetfulness, blood pressure assumed to be normal and non-availability were the main reasons for non-adherence.51 Similarly, a study conducted in Bangladesh reported that forgetfulness, feeling well/no need for medication use and busy schedule were the three main reasons for non-adherence.52 In another study conducted in Bangladesh, forgetfulness, busy schedule and boredom were reported as the three main factors for medication non-adherence in hypertensive patients.53 All of these South Asian studies showed that forgetfulness, feeling well/no need for medicines were the major reasons for medication non-adherence in hypertensive patients.
Implications for Clinical Practice
The findings of this study have critical implications for healthcare practitioners and policy makers. There is a clear need to design and implement different interventions with the aim of improving medication adherence among patients. In this study, we have identified different predictors for medication adherence, such as age, level of education, entitlement/insurance status, treatment duration, number of antihypertensive medications and presence of comorbidities. Hence, any intervention targeting any of these predictors could be helpful in improving medication adherence. Effective strategies to improve medication adherence can be achieved through better communications between the physician and patient and can help to improve medication adherence. Interventions have to be patient specific in order to be successful. Patient-related factors such as gender, culture, health beliefs and knowledge about disease should be kept in mind when designing any intervention for improving medication adherence. Limited local evidence is available on the effectiveness of interventions to improve medication adherence among hypertensive patients in Pakistan. However, internationally, effective interventions to improve medication adherence include educational programmes involving both patients and family members, in the form of individual instructions or group classes; regular monitoring of blood pressure at home; providing entitlement to free medical care; simplifying the dosing regimen; and behavioural interventions, such as memory aids and synchronizing therapeutic activities with the daily routine, eg taking medications before a shower or after prayer.54,55 The existing literature has demonstrated that interventions aimed at improving health literacy, using communication technologies such as mobile applications and sending SMS reminders, electronic medication reconciliation and motivational interviewing can improve medication adherence and may have positive effects on treatment outcomes.56–63
Study Limitations
There are a few limitations to our study findings. This study was conducted in only one city in Pakistan; therefore, the findings may not be generalizable to other cities, towns and villages. Self-administered questionnaires were used in this research to assess medication adherence, which may lead to under- or overestimation of results. This questionnaire required recall of previous events, which may lead to recall bias, especially in older patients or those who had been on antihypertensive treatment for many years. However, MMAS-8 has very well-documented reliability and validity in assessing medication adherence. In this study, comorbidity was recorded as a dichotomous outcome (present/not present); however, the number and nature of comorbidities, which could potentially affect medication adherence and treatment outcome, were not recorded. Future studies should collect data focusing on the number and nature of comorbidities, and their impact on medication adherence.
Conclusion
Adherence to prescribed antihypertensive medications was suboptimal in hypertensive patients attending different healthcare settings in Islamabad, Pakistan. This suboptimal medication adherence was associated with poor blood pressure control. Keeping in view the predictors of good blood pressure control identified in this study, targeted interventions should be introduced and implemented for better treatment outcomes.
Acknowledgments
The authors thank Professor Donald E. Morisky, Department of Community Health Sciences, UCLA Fielding School of Public Health, Los Angeles, United States, for granting us permission to use the copyrighted MMAS-8. Use of the ©MMAS is protected by US copyright and registered trademark laws. Permission for use is required. A licensing agreement is available from: Donald E. Morisky, 294 Lindura Court, Las Vegas, NV 89138-4632; dmorisky@gmail.com.
Disclosure
The authors declare that they have no conflicts of interest.
References
- 1.Kokubo Y, Iwashima Y. Higher blood pressure as a risk factor for diseases other than stroke and ischemic heart disease. Hypertension. 2015;66(2):254–259. doi: 10.1161/HYPERTENSIONAHA.115.03480 [DOI] [PubMed] [Google Scholar]
- 2.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1· 25 million people. Lancet. 2014;383(9932):1899–1911. doi: 10.1016/S0140-6736(14)60685-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mills KT, Bundy JD, Kelly TN, et al. Global burden of hypertension: analysis of population-based studies from 89 countries. J Hypertens. 2015;33:e2. doi: 10.1097/01.hjh.0000469726.59998.cc [DOI] [Google Scholar]
- 4.W.H.O report on global prevalence of hypertension published on World Health Day; 2013. Available from: https://apps.who.int/iris/bitstream/handle/10665/79059/WHO_DCO_WHD_2013.2_eng.pdf;jsessionid=F638668E0D914847E4B72CCAFB90BC63?sequence=1. Accessed July27, 2019.
- 5.Mohan S, Campbell NR. Hypertension management. Hypertension. 2009;53(3):450–451. doi: 10.1161/HYPERTENSIONAHA.108.127076 [DOI] [PubMed] [Google Scholar]
- 6.Prenissl J, Manne-Goehler J, Jaacks LM, et al. Hypertension screening, awareness, treatment, and control in India: a nationally representative cross-sectional study among individuals aged 15 to 49 years. PLoS Med. 2019;16(5):e1002801. doi: 10.1371/journal.pmed.1002801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1· 7 million adults in a population-based screening study (China PEACE million persons project). Lancet. 2017;390(10112):2549–2558. doi: 10.1016/S0140-6736(17)32478-9 [DOI] [PubMed] [Google Scholar]
- 8.Shah N, Shah Q, Shah AJ. The burden and high prevalence of hypertension in Pakistani adolescents: a meta-analysis of the published studies. Arch Public Health. 2018;76(1):20. doi: 10.1186/s13690-018-0265-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khatib R, Schwalm J-D, Yusuf S, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One. 2014;9(1):e84238. doi: 10.1371/journal.pone.0084238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jaam M, Hadi MA, Kheir N, et al. A qualitative exploration of barriers to medication adherence among patients with uncontrolled diabetes in Qatar: integrating perspectives of patients and health care providers. Patient Prefer Adherence. 2018;12:2205. doi: 10.2147/PPA.S174652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jaam M, Ibrahim MIM, Kheir N, Hadi MA, Diab MI, Awaisu A. Assessing prevalence of and barriers to medication adherence in patients with uncontrolled diabetes attending primary healthcare clinics in Qatar. Prim Care Diabetes. 2018;12(2):116–125. doi: 10.1016/j.pcd.2017.11.001 [DOI] [PubMed] [Google Scholar]
- 12.Cramer J, Benedict A, Muszbek N, Keskinaslan A, Khan Z. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract. 2008;62(1):76–87. doi: 10.1111/j.1742-1241.2007.01630.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levy G, Zamacona MK, Jusko WJ. Developing compliance instructions for drug labeling. Clin Pharmacol Ther. 2000;68(6):586–591. doi: 10.1067/mcp.2000.110976 [DOI] [PubMed] [Google Scholar]
- 14.Gibaldi M. Failure to comply: a therapeutic dilemma and the bane of clinical trials. J Clin Pharmacol. 1996;36(8):674–682. doi: 10.1002/jcph.1996.36.issue-8 [DOI] [PubMed] [Google Scholar]
- 15.Li YT, Wang HH, Liu KQ, et al. Medication adherence and blood pressure control among hypertensive patients with coexisting long-term conditions in primary care settings: a cross-sectional analysis. Medicine. 2016;95(20). doi: 10.1097/MD.0000000000004864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jalal Z, Antoniou S, Taylor D, Paudyal V, Finlay K, Smith F. South Asians living in the UK and adherence to coronary heart disease medication: a mixed-method study. Int J Clin Pharm. 2019;41(1):122–130. doi: 10.1007/s11096-018-0760-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hashmi SK, Afridi MB, Abbas K, et al. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS One. 2007;2(3):e280. doi: 10.1371/journal.pone.0000280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahmed N, Abdul Khaliq M, Shah SH, Anwar W. Compliance to antihypertensive drugs, salt restriction, exercise and control of systemic hypertension in hypertensive patients at Abbottabad. J Ayub Med Coll Abbottabad. 2008;20(2):66–69. [PubMed] [Google Scholar]
- 19.Ali M, Hameed J, Zia MH, Masood RA, Shahzad A. Patient compliance in systemic hypertension and to identify causes of non-compliance. J Islam Int Med Coll. 2013:48. [Google Scholar]
- 20.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007 [DOI] [PubMed] [Google Scholar]
- 21.Meghani ST, Sehar S, Punjani NS. Comparison and analysis of health care delivery system: pakistan versus China. Int J Endorsing Health Sci Res. 2014;2:46–50. [Google Scholar]
- 22.Islam A. Health sector reform in Pakistan: future directions. J Pak Med Assoc. 2002;52(4):174–182. [PubMed] [Google Scholar]
- 23.Morisky DE, Ang A, Krousel‐Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–354. doi: 10.1111/j.1751-7176.2008.07572.x [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Berlowitz DR, Foy CG, Kazis LE, et al. Effect of intensive blood-pressure treatment on patient-reported outcomes. N Engl J Med. 2017;377(8):733–744. doi: 10.1056/NEJMoa1611179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: response to authors. J Clin Epidemiol. 2011;64(3):255–257. doi: 10.1016/j.jclinepi.2010.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saleem F, Hassali MA, Akmal S, et al. Translation and validation study of Morisky Medication Adherence Scale (MMAS): the Urdu version for facilitating person-centered healthcare in Pakistan. Int J Pers Cent Med. 2012;2(3):384–390. [Google Scholar]
- 27.National Institute for Health and Care Excellence (NICE) [Internet]. Manchester, UK: Hypertension in adults: diagnosis and management NICE guidelines [CG127]; August 2011. [reviewed October 2013]. Available from: https://www.nice.org.uk/guidance/cg127. Accessed December31, 2019. [Google Scholar]
- 28.Nielsen JØ, Shrestha AD, Neupane D, Kallestrup P. Non-adherence to anti-hypertensive medication in low-and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens. 2017;31(1):14. doi: 10.1038/jhh.2016.31 [DOI] [PubMed] [Google Scholar]
- 29.Khayyat SM, Khayyat SMS, Alhazmi RSH, Mohamed MM, Hadi MA. Predictors of medication adherence and blood pressure control among Saudi hypertensive patients attending primary care clinics: a cross-sectional study. PLoS One. 2017;12(1):e0171255. doi: 10.1371/journal.pone.0171255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky medication adherence scale. PLoS One. 2013;8(4):e62775. doi: 10.1371/journal.pone.0062775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kang CD, Tsang PP, Li WT, et al. Determinants of medication adherence and blood pressure control among hypertensive patients in Hong Kong: a cross-sectional study. Int J Cardiol. 2015;182:250–257. doi: 10.1016/j.ijcard.2014.12.064 [DOI] [PubMed] [Google Scholar]
- 32.Han WP, Hong SA, Tiraphat S. Factors related to medication adherence among essential hypertensive patients in tertiary hospitals in Yangon, Myanmar. J Public Health Dev. 2015;13(2):43–56. [Google Scholar]
- 33.Shaik SA, Alsuwailem A, Alhargan A, et al. Medications adherence level and its associated factors among hypertensive patients at a major referral hospital, in Riyadh, KSA. Asian J Med Sci. 2016;7(4):24–30. doi: 10.3126/ajms.v7i4.14085 [DOI] [Google Scholar]
- 34.Fahey M, Abdulmajeed A, Sabra K. Measurement of adherence to anti-hypertensive medication as perceived by doctors and patients. Qatar Med J. 2006;2006(1):16. doi: 10.5339/qmj.2006.1.16 [DOI] [Google Scholar]
- 35.Saadat Z, Nikdoust F, Aerab-Sheibani H, et al. Adherence to antihypertensives in patients with comorbid condition. Nephrourol Mon. 2015;7(4). doi: 10.5812/numonthly. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Organization WH. Adherence to long-term therapies: evidence for action. 2003. https://apps.who.int/iris/bitstream/handle/10665/42682/9241545992.pdf. Accessed July 27, 2019. [Google Scholar]
- 37.Yue Z, Li C, Weilin Q, Bin W. Application of the health belief model to improve the understanding of antihypertensive medication adherence among Chinese patients. Patient Educ Couns. 2015;98(5):669–673. doi: 10.1016/j.pec.2015.02.007 [DOI] [PubMed] [Google Scholar]
- 38.Al-Ramahi R. Adherence to medications and associated factors: a cross-sectional study among Palestinian hypertensive patients. J Epidemiol Glob Health. 2015;5(2):125–132. doi: 10.1016/j.jegh.2014.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hassan N, Hasanah C, Foong K, et al. Identification of psychosocial factors of noncompliance in hypertensive patients. J Hum Hypertens. 2006;20(1):23. doi: 10.1038/sj.jhh.1001930 [DOI] [PubMed] [Google Scholar]
- 40.Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. CMAJ. 1999;160(1):31–37. [PMC free article] [PubMed] [Google Scholar]
- 41.Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. Am J Public Health. 1996;86(12):1805–1808. doi: 10.2105/AJPH.86.12.1805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–362. doi: 10.1097/01.hco.0000126978.03828.9e [DOI] [PubMed] [Google Scholar]
- 43.Inkster ME, Donnan P, MacDonald T, Sullivan F, Fahey T. Adherence to antihypertensive medication and association with patient and practice factors. J Hum Hypertens. 2006;20(4):295. doi: 10.1038/sj.jhh.1001981 [DOI] [PubMed] [Google Scholar]
- 44.Youssef R, Moubarak I. Patterns and determinants of treatment compliance among hypertensive patients. 2002. [PubMed] [Google Scholar]
- 45.Gryglewska B. How can we improve the effectiveness of treatment in elderly hypertensives? Blood Press. 2005;14(sup2):46–49. doi: 10.1080/08038020500428740 [DOI] [PubMed] [Google Scholar]
- 46.Olowookere AJ, Olowookere SA, Talabi AO, Etonyeaku AC, Adeleke OE, Akinboboye OO. Perceived family support and factors influencing medication adherence among hypertensive patients attending a Nigerian tertiary hospital. Ann Trop Med Public Health. 2015;8(6):241. doi: 10.4103/1755-6783.162668 [DOI] [Google Scholar]
- 47.Marín-Reyes F, Rodríguez-Morán M. Family support of treatment compliance in essential arterial hypertension. Salud Publica Mex. 2001;43(4):336–339. doi: 10.1590/S0036-36342001000400010 [DOI] [PubMed] [Google Scholar]
- 48.Setiati S, Sutrisna B. Prevalence of hypertension without anti-hypertensive medications and its association with social demographic characteristics among 40 years and above adult population in Indonesia. Acta Med Indones. 2005;37(1):20–25. [PubMed] [Google Scholar]
- 49.Taibanguay N, Chaiamnuay S, Asavatanabodee P, Narongroeknawin P. Effect of patient education on medication adherence of patients with rheumatoid arthritis: a randomized controlled trial. Patient Prefer Adherence. 2019;13:119. doi: 10.2147/PPA.S192008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jahangiry L, Ghanbari J, Farhangi MA, Sarbakhsh P, Ponnet K. Predictors of poor blood pressure control among Iranian hypertensive patients. BMC Res Notes. 2017;10(1):668. doi: 10.1186/s13104-017-2971-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mallya SD, Kumar A, Kamath A, Shetty A, Mishra S. Assessment of treatment adherence among hypertensive patients in a coastal area of Karnataka, India. Int J Community Med Public Health. 2017;3(8):1998–2003. [Google Scholar]
- 52.Hussanin S, Boonshuyar C, Ekram A. Non-adherence to antihypertensive treatment in essential hypertensive patients in Rajshahi, Bangladesh. Anwer Khan Mod Med Coll J. 2011;2(1):9–14. doi: 10.3329/akmmcj.v2i1.7465 [DOI] [Google Scholar]
- 53.Ekram AS, Hussain SM, Boonshuyar C. Preliminary report on non-adherence to antihypertensive treatment in essential hypertensive patients: a community based survey. J Teachers Assoc. 2008;21(2):112–117. [Google Scholar]
- 54.Fenerty SD, West C, Davis SA, Kaplan SG, Feldman SR. The effect of reminder systems on patients’ adherence to treatment. Patient Prefer Adherence. 2012;6:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jin J, Sklar GE, Oh VMS, Li SC. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269. doi: 10.2147/TCRM.S1458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gwadry-Sridhar FH, Manias E, Lal L, et al. Impact of interventions on medication adherence and blood pressure control in patients with essential hypertension: a systematic review by the ISPOR medication adherence and persistence special interest group. Value Health. 2013;16(5):863–871. doi: 10.1016/j.jval.2013.03.1631 [DOI] [PubMed] [Google Scholar]
- 57.Conn VS, Ruppar TM, Chase J-AD, Enriquez M, Cooper PS. Interventions to improve medication adherence in hypertensive patients: systematic review and meta-analysis. Curr Hypertens Rep. 2015;17(12):94. doi: 10.1007/s11906-015-0606-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Palacio AM, Uribe C, Hazel-Fernandez L, et al. Can phone-based motivational interviewing improve medication adherence to antiplatelet medications after a coronary stent among racial minorities? A randomized trial. J Gen Intern Med. 2015;30(4):469–475. doi: 10.1007/s11606-014-3139-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kamal AK, Muqeet A, Farhat K, et al. Using a tailored health information technology-driven intervention to improve health literacy and medication adherence in a Pakistani population with vascular disease (Talking Rx)–study protocol for a randomized controlled trial. Trials. 2016;17(1):121. doi: 10.1186/s13063-016-1244-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zomahoun HTV, Guenette L, Gregoire J-P, et al. Effectiveness of motivational interviewing interventions on medication adherence in adults with chronic diseases: a systematic review and meta-analysis. Int J Epidemiol. 2016;46(2):589–602. [DOI] [PubMed] [Google Scholar]
- 61.Vollmer WM, Feldstein A, Smith D, et al. Use of health information technology to improve medication adherence. Am J Manag Care. 2011;17(12):SP79. [PMC free article] [PubMed] [Google Scholar]
- 62.Jalal ZS, Smith F, Taylor D, Patel H, Finlay K, Antoniou S. Pharmacy care and adherence to primary and secondary prevention cardiovascular medication: a systematic review of studies. Eur J Hosp Pharm. 2014;21(4):238–244. doi: 10.1136/ejhpharm-2014-000455 [DOI] [Google Scholar]
- 63.Jalal ZS, Smith F, Taylor D, Finlay K, Patel H, Antoniou S. Impact of pharmacy care upon adherence to cardiovascular medicines: a feasibility pilot controlled trial. Eur J Hosp Pharm. 2016;23(5):250–256. doi: 10.1136/ejhpharm-2015-000790 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- W.H.O report on global prevalence of hypertension published on World Health Day; 2013. Available from: https://apps.who.int/iris/bitstream/handle/10665/79059/WHO_DCO_WHD_2013.2_eng.pdf;jsessionid=F638668E0D914847E4B72CCAFB90BC63?sequence=1. Accessed July27, 2019.