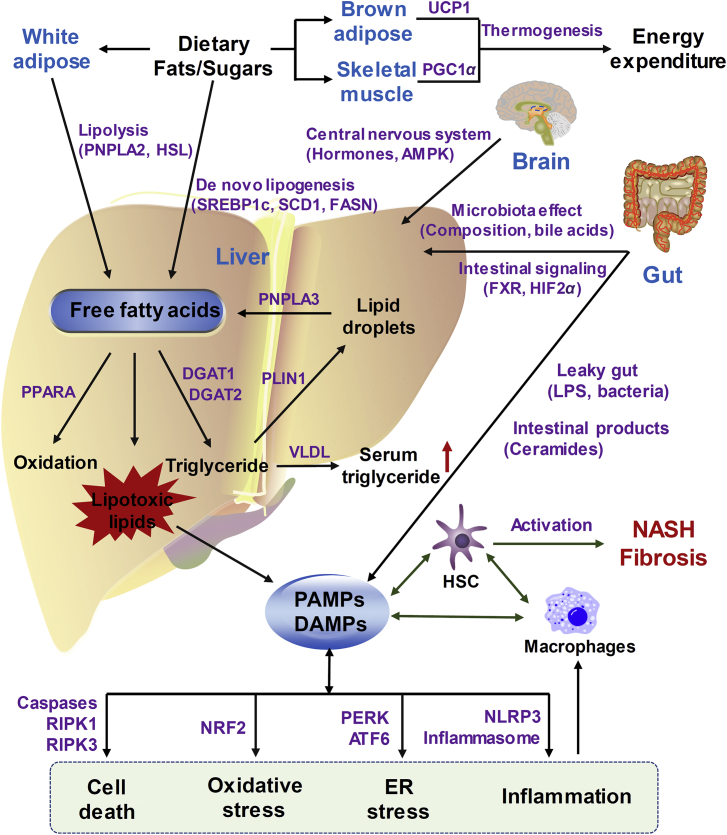
Figure 1.
Proposed “multiple organs-multiple hits” model for explaining the NAFLD/NASH pathogenesis. “Multiple organs-multiple hits” model describes how the crosstalk between liver and other tissues/non-liver cells (gut, brown/white adipose, skeletal muscle, brain and macrophages) promotes NASH progression. Free fatty acids, sourced from either adipose lipolysis or hepatic lipid droplets or de novo lipogenesis from dietary fats/sugars, overload the liver. Then, fatty acids could be degraded by fatty acid β-oxidation and triglyceride secreted from liver to serum, or can be converted to lipotoxic lipids when the disposal pathways of fatty acids are saturated. Lipotoxic lipids could then cause oxidative stress, ER stress, inflammation and possibly cell death. Non-liver organs can also contribute directly or indirectly to NASH progression. During NAFLD progress, changes in gut microbiota composition or intestinal lipids modulation signaling, can yield toxic microbiota products, or even forms leaky gut to release LPS or bacteria, all of which could be PAMPs or DAMPs and enter the liver via the portal vein. All the PAMPs and/or DAMPs generated from liver, gut or macrophages can work together to activate HSC and cause liver fibrosis. Energy balance could be regulated by the central nervous system via food intake or central hormones/signaling, as well as by brown adipose or skeletal muscle that helps burn adipose fat via thermogenesis or energy expenditure, thus indirectly decrease the overloaded burden of hepatic fatty acids and alleviate NAFLD.