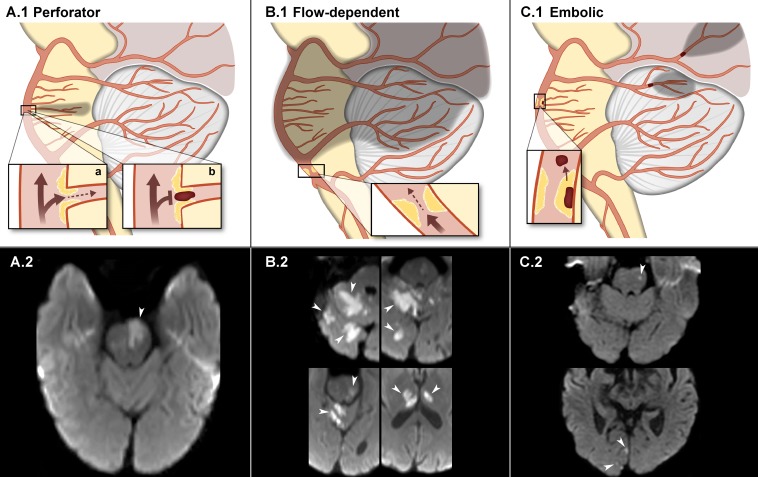
Figure 2.
Stroke mechanisms of ISBAS (infarction depicted in shadows). Schematic representation in the upper row and diffusion-weighted images depicting each stroke category in the lower row. (A.1) Deep pontine stroke secondary to an unstable plaque localised in the origin of a perforator. The stroke may occur due to decreased flow (a) or in situ thrombosis (b). (A.2) Midbrain stroke (arrow) due to occlusion of a BA perforator. (B.1) Flow-dependent/hypoperfusion stroke secondary to decreased blood flow in the mid and distal BA. The atherosclerotic plaque is located in the proximal segment. (B.2) Multiple strokes affecting the cerebellum, midbrain and thalami (arrows) in the setting of a flow-dependent high-grade stenosis. (C.1) Artery-to-artery thromboembolic occlusion of distal SCA and PCA branches secondary to a plaque rupture in the mid-basilar segment. (C.2) Thromboembolic strokes (arrows) in the left midbrain and right occipital lobe. BA, basilar artery; ISBAS, isolated symptomatic basilar artery stenosis; PCA, posterior cerebral artery; SCA, superior cerebellar artery.