ABSTRACT
Background
A trial in Burkina Faso compared the cost-effectiveness of 4 specialized nutritious foods (SNFs) used to prevent stunting and wasting in children aged 6–23 mo.
Objectives
This article explores differences in SNF use that may have influenced effectiveness, specifically in relation to consumption by the recipient child and by any other person (i.e., sharing), other diversion from the recipient child, preparation, storage, and hygiene.
Methods
Subsamples from a geographically clustered, longitudinal trial with random assignment to Corn Soy Blend Plus with oil (CSB+ w/oil), Corn Soy Whey Blend with oil (CSWB w/oil), Super Cereal Plus (SC+), or ready-to-use supplementary food (RUSF) were selected for in-depth interviews, in-home observations, and focus group discussions.
Results
Sharing was common in all arms, with the highest reported in SC+ (73%) and highest observed in CSWB w/oil (36%). Some reported giving the ration away (highest in SC+ at 17%) or using it for other purposes (highest in CSWB w/oil at 17%). The recipient child was observed consuming the ration in 49% of households on average (38–60% by arm in CSB+ w/oil and RUSF, respectively). Qualitative reports of bitterness and spoilage emerged in the CSWB w/oil arm. Most observed households (excluding RUSF) did not prepare porridge daily as instructed (35–46% by arm). Household water samples showed either high-risk or unsafe contamination with Escherichia coli (72–78% by arm). Low percentages were observed handwashing (both child and server) before consuming the porridge.
Conclusions
The SNFs were not prepared or served as intended and diversion from the recipient was common. Storage conditions may have resulted in spoilage of the ration containing whey before reaching recipients. This article provides context about factors that may have influenced the effectiveness of these SNFs. Programming and household use of SNFs are as important as their nutrient composition. This trial was registered at clinicaltrials.gov as NCT02071563.
Keywords: supplementary feeding, children under 5, corn–soy blend, lipid-based nutrient supplements, stunting, wasting, specialized nutritious food, Burkina Faso
Introduction
It is well known that the first 2 y of life is a critical period for prevention of growth faltering through adequate complementary feeding (1–5). A range of complementary feeding strategies, including use of specialized nutritious foods (SNFs), have been shown to improve growth outcomes and reduce child stunting in food-insecure settings (6, 7). But these findings show either modest improvements or mixed evidence, with declining rates of growth still observed among groups that receive food supplementation (8–16). There is growing consensus that supplementary feeding programs providing SNFs must account for the feeding and preparation behaviors within the household that may influence how much and in what way the products are consumed and thus their effectiveness (17). These factors are wide-ranging and may vary both across and within regions; understanding these context-specific factors can result in more effective programming (18, 19).
A recent trial in Burkina Faso also observed growth faltering (declines in z scores over time) among children who received supplementary foods monthly from age ∼6 mo to 23 mo (I. Cliffer, L. Nikiema, B. Langlois, A. Zeba, Y. Shen, H. Lanou, D. Suri, F. Garanet, K. Chui, S. Vosti, S. Walton, I. Rosenberg, P. Webb, B. Rogers; Tufts University). The trial compared 4 specialized nutritious foods (SNFs) used for prevention of stunting and wasting: Corn Soy Blend Plus with oil (CSB+ w/oil); Corn Soy Whey Blend with oil (CSWB w/oil); Super Cereal Plus (SC+); and ready-to-use supplementary food (RUSF). The study found that although the foods differed in terms of cost-effectiveness—with CSB+ w/oil emerging as the most cost-effective and CSWB w/oil as the least—none prevented declines in linear growth over time or fundamentally altered growth trajectories (Ilana R Cliffer et al., unpublished results, Tufts University). These findings raise 2 important questions: 1) why did the SNFs fail to prevent growth faltering, and 2) why did the SNF with added whey protein and enhanced micronutrient profile perform relatively less well than the other SNFs (20, 21)? This article provides insight into factors that may have influenced the effectiveness of the SNFs used in this blanket supplementary feeding program in Burkina Faso. Specifically, this article explores differences in consumption, sharing and diversion, preparation, and storage and hygiene of the SNFs.
Methods
Study design, population, and setting
This article describes data collected on subsamples of recipient households participating in a 4-pronged, geographically clustered, longitudinal trial (NCT02071563) with random assignment to receive CSB+ w/oil, CSWB w/oil, SC+, or RUSF. The rations were calculated to provide the recipient child with ∼500 kcal/d if prepared as directed. Rations were premeasured to the correct amounts before distribution. In the dry season, the fortified blended foods (FBFs) were prepackaged. Owing to logistical constraints in the rainy season, however, they were measured on site as they were “scooped” from bulk form. The RUSF was always provided in prepackaged sachets. At each month of distribution, it was recorded whether the ration was received or the caregiver missed the distribution. A total of 18 possible distributions were planned for all the products. Along with the monthly ration, caregivers were given instructions and provided with cooking demonstrations on how to prepare the food that they received. For those who received CSB+ w/oil or CSWB w/oil, a key aspect was the provision of additional fortified oil, to be prepared in the ratio of 30 g oil to 100 g flour, so that all 4 rations were comparable in caloric density. In addition, caregivers were instructed to feed the foods only to the target child at appropriate frequencies throughout the day, and to maintain proper hygiene while doing so. Key themes of social and behavior change communication messaging related to the rations included: its purpose, quantities to consume, hygienic precaution in preparation, consumption and storage, and culinary preparations (FBF arms). Instruction was provided to each caregiver at the initial distribution. Table 1 provides details about the nutrient composition of the study foods and the ration quantities provided.
TABLE 1.
Nutrient composition and ration sizes1
| Nutrient composition | CSB+ w/oil (per ∼500 kcal) | SC+ (per 500 kcal) | CSWB w/oil (per ∼500 kcal) | RUSF (per 500 kcal) |
|---|---|---|---|---|
| Water, g | 7.86 | 10.82 | 0 | 13.7 |
| Energy, kcal | 483.15 | 500 | 487.92 | 500 |
| Protein, g | 9.66 | 18.02 | 12.91 | 10 |
| Total lipid (fat), g | 26.52 | 10.19 | 27.72 | 15 |
| Carbohydrate, g | 51.28 | 82.9 | 46.96 | 51 |
| Total dietary fiber, g | 3.75 | 5.3 | 4.8 | 0 |
| Total sugars, g | 2.05 | 19.66 | 3.82 | 22 |
CSB+ w/oil, Corn Soy Blend Plus with oil; CSWB w/oil, Corn Soy Whey Blend with oil; RUSF, ready-to-use supplementary food; SC+, Super Cereal Plus.
The study took place through an existing blanket supplementary feeding program called “Victoire sur la Malnutrition,” run by ACDI/VOCA and Save the Children in Sanmatenga Province, Burkina Faso from 2014 to 2016. The foods were distributed by community volunteers at 48 designated food distribution points. Social and behavior change communication was delivered through a Care Group model: health and nutrition promoters trained lead mothers (a group leader selected from a block of 10–12 households) who then trained their group of recipient caregivers. A total of 6112 children aged ∼6 mo were enrolled on a rolling basis and followed for 18 mo to assess the comparative effectiveness and cost-effectiveness of the products for prevention of stunting and wasting. CSB+ w/oil served as the reference group in the effectiveness and cost-effectiveness evaluation. Study participants were not paid for their participation but received 2 bars of soap as a thank you gift after their participation in the study. The study protocol was approved by the Tufts University Institutional Review Board and the Ethics Committee for Health Research in Burkina Faso. The study reporting adheres to the CONSORT guidelines. A conceptual framework and a more detailed description of the study's methods, including the CONSORT guidelines for cluster-randomized trials, will be provided in a separate article reporting the main findings (I. Cliffer, L. Nikiema, B. Langlois, A. Zeba, Y. Shen, H. Lanou, D. Suri, F. Garanet, K. Chui, S. Vosti, S. Walton, I. Rosenberg, P. Webb, B. Rogers; Tufts University).
Data collection and sampling
This study used a mix of quantitative and qualitative data collection methods. Structured interviews, in-home observations, and qualitative focus group discussions were conducted among separate subsamples of participating households by trained enumerators who were paid by the study. Participants were selected for in-depth interviews or in-home observations using preassigned random numbers in a 3-stage process. First, random numbers were generated to identify a subset of mothers of recipient children from the larger sample. Then, the subset was randomly assigned to either an interview or an in-home observation. Lastly, participants were randomly assigned a time-period at which the interview would take place relative to their length of time in the program to ensure there was an even spread of interviews over the program exposure time. Households that received an in-home observation were also interviewed in their home at the end of the observation. Six food distribution points were selected purposively per study arm and focus group discussions were conducted with recipient caregivers from the catchment area once per site. Focus group discussion participants were chosen purposively based on geographic proximity and did not include those who were selected for either an interview or an in-home observation. There were no predetermined hypotheses about meaningful effect sizes, therefore sample sizes were chosen based on feasibility: 400 households per arm for in-depth interviews and 50 per arm for in-home observations. With sample sizes of 400 per arm for the in-depth interviews, detectable effect sizes ranged from 7 to 10 percentage points depending on the baseline proportion of the 400 households represented.
Interviews conducted among caregivers collected information on their personal experiences learning about, collecting, and using the rations. This included training and instructions received for ration use; accessibility and transport to the distribution site; sufficiency of ration quantities; sharing of the ration (i.e., consumption by anyone other than the recipient child) within and outside the household; preparation and feeding; consumption; and handling and storage. When possible, porridge samples of CSB+ w/oil, CSWB w/oil, and SC+ were collected to estimate the amount of oil contained, and water samples were collected from all interviewed or observed households and tested for Escherichia coli levels. In-home observations were conducted among participating households over a 4-d period for households to become accustomed to the presence of the female enumerator and to reduce the likelihood that they would alter their behavior because of her presence. The observations were conducted in 12-h time blocks, from 06:00 to 18:00 on each of the 4 d. The interviews lasted 30–45 min and were conducted after the in-home observation was completed.
The purpose of the observations was to directly capture habitual behaviors that might not be reported or might differ from what was reported by participants during interviews or focus groups. During observations, data about preparation and consumption and other uses of the ration within the household (e.g., how often was the ration prepared, who consumed the ration, under what hygienic conditions was the ration prepared and consumed, who consumes leftovers) were recorded on a structured paper form that listed each of the activities with 30-min time intervals in a grid format. Focus group discussions with caregivers were centered on the following experiences: barriers to following preparation and serving instructions; use of the ration, including consumption, sharing, and selling; acceptability of the ration by the child; and perceived opportunity costs and advantages regarding participation in the program. Focus group discussions were conducted in the local language of the participants and administered by 1 enumerator while another took notes. All focus groups were recorded with the permission of the participants.
Data analysis
Survey and observation data were collected by trained enumerators on paper forms and were double-entered and compared for inconsistencies in a CSPro (version 6) database (22). All quantitative data were cleaned and analyzed using Stata version 13 (StataCorp). In reporting in-home observation findings, we reference household-days, meaning the total number of observation days contributed by all households combined. Descriptive frequencies and percentages were calculated. Statistical significance for differences across study arms for the interview data was evaluated at the 0.05 level using Pearson's chi-square test for categorical variables and 1-factor ANOVA for continuous variables. Adjusted estimates for the differences across study arms were obtained through logistic regression models that controlled for potential confounders identified through the descriptive summary of household characteristics. However, because there were no formal a priori hypotheses or model-building processes, these analyses are exploratory. Statistical significance was not tested for in-home observations because these data served more of a qualitative purpose and owing to the low sample sizes.
All focus group records were translated into French and transcribed by the enumerators and then translated into English by external translators. Translated focus groups were checked for accuracy by comparison with recordings by members of the data collection team. Transcripts were then imported into QSR International's NVivo 12 software for analysis. Data were analyzed using an inductive approach, by which text was reviewed line-by-line and categorized into emergent themes. Two analysts read the transcripts independently and discussed possible themes. One of the analysts then took the lead coding the data into themes and subthemes. Periodically the 2 analysts coded together, resolving any disagreements through discussion.
Results
A total of 1654 interviews (84% response rate), 209 in-home observations (93% response rate), and 23 focus group discussions were completed. Nonresponse was mostly due to out-of-country travel or relocation out of the area. Table 2 displays a descriptive summary of household characteristics for the interviewed study sample. Characteristics were similar across study arms, with some variation in level of education, number of children <5 y, and wealth (Table 2). The differences identified in Table 2 were included in adjusted analyses. Of the interviewed households, porridge samples were collected from 51% (excluding the RUSF arm) and water samples were collected from 99.6%. The mean number of distributions received throughout the study among the interviewed sample was 17 overall and across all 4 study arms.
TABLE 2.
Household characteristics of the interviewed sample1
| CSB+ w/oil (n = 430) | CSWB w/oil (n = 418) | SC+ (n = 385) | RUSF (n = 421) | Total (n = 1654) | |
|---|---|---|---|---|---|
| Age of mother,* y | 26.00 ± 6.22 | 26.13 ± 6.44 | 27.15 ± 6.60 | 25.79 ± 6.34 | 26.26 ± 6.41 |
| Twin | 11 (3) | 16 (4) | 9 (2) | 22 (5) | 58 (4) |
| Highest level of education in the household* | |||||
| None | 110 (26) | 96 (23) | 53 (14) | 102 (25) | 361 (22) |
| Literate | 16 (4) | 22 (5) | 12 (3) | 14 (3) | 64 (4) |
| Primary | 243 (57) | 198 (48) | 171 (45) | 196 (47) | 808 (49) |
| Secondary | 51 (12) | 91 (22) | 136 (36) | 89 (22) | 367 (22) |
| Higher | 2 (0) | 0 (0) | 3 (1) | 3 (1) | 8 (0) |
| Other | 3 (1) | 8 (2) | 5 (1) | 9 (2) | 25 (2) |
| Number of children <5 y in household* | |||||
| ≤1 | 77 (18) | 79 (19) | 88 (23) | 65 (15) | 309 (19) |
| 2 | 138 (32) | 148 (35) | 156 (41) | 114 (27) | 556 (34) |
| 3 | 76 (18) | 78 (19) | 72 (19) | 91 (22) | 317 (19) |
| 4 | 60 (14) | 41 (10) | 33 (9) | 78 (19) | 212 (13) |
| ≥5 | 79 (18) | 72 (17) | 36 (9) | 73 (17) | 260 (16) |
| Household Food Insecurity Access Scale category | |||||
| Food secure | 176 (42) | 184 (45) | 154 (41) | 188 (45) | 702 (43) |
| Mildly insecure | 73 (17) | 70 (17) | 54 (14) | 71 (17) | 268 (17) |
| Moderately insecure | 105 (25) | 111 (27) | 104 (28) | 93 (22) | 413 (25) |
| Severely insecure | 69 (16) | 43 (11) | 64 (17) | 64 (15) | 240 (15) |
| Wealth quintiles2,* | |||||
| Lowest | 102 (24) | 64 (15) | 80 (21) | 85 (21) | 331 (20) |
| Mid-low | 84 (20) | 90 (22) | 81 (21) | 75 (18) | 330 (20) |
| Medium | 105 (25) | 90 (22) | 63 (17) | 65 (16) | 323 (20) |
| Mid-high | 71 (17) | 85 (20) | 72 (19) | 96 (23) | 324 (20) |
| Highest | 58 (14) | 86 (21) | 82 (22) | 90 (22) | 316 (19) |
Values are n (%) or mean ± SD. Percentages are out of the 1654 completed interviews—16% (318 of 1972) were not completed. CSB+ w/oil, Corn Soy Blend Plus with oil; CSWB w/oil, Corn Soy Whey Blend with oil; RUSF, ready-to-use supplementary food; SC+, Super Cereal Plus.
Derived from principal component analysis of household possessions.
P < 0.05 from Pearson's chi-square test (ANOVA test for age of mother).
Consumption: were the target recipients consuming the intended quantities of the foods?
Overall and within each arm, almost all caregivers reported that the recipient child normally consumed the ration. When asked about the most recent preparation, the percentages reporting that the recipient child consumed the ration were high and were slightly lower in the FBF (i.e., CSB+ w/oil, SC+, CSWB w/oil) arms than in the RUSF arm (Table 3). These estimates were similar in the adjusted analysis. Figure 1 shows observed consumption by day of observation. For each of the 4 d, observed consumption of the ration by the recipient child was lower than reported in all arms (Figure 1).
TABLE 3.
Descriptive statistics of the interviewed and observed households1
| CSB+ w/oil | CSWB w/oil | SC+ | RUSF | Total | |
|---|---|---|---|---|---|
| Reported, n | 430 | 418 | 385 | 421 | 1654 |
| How long ration lasted the previous month* | |||||
| All month with leftovers | 61 (14) | 42 (10) | 57 (15) | 66 (16) | 226 (14) |
| All month without leftovers | 81 (19) | 54 (13) | 65 (17) | 168 (40) | 368 (22) |
| Finished before end of month | 280 (65) | 311 (75) | 260 (68) | 181 (43) | 1032 (63) |
| Unknown | 6 (1) | 7 (2) | 3 (1) | 6 (1) | 22 (1) |
| Have given the ration to others* | 38 (9) | 49 (12) | 66 (17) | 55 (13) | 208 (13) |
| Have given the oil to others | 36 (8) | 29 (7) | n/a | n/a | 65 (8) |
| What else is the ration used for* | |||||
| No other purpose | 382 (89) | 349 (84) | 379 (98) | 397 (95) | 1507 (91) |
| Other family meals | 24 (6) | 49 (12) | 2 (1) | 1 (0) | 76 (5) |
| Other purpose | 23 (5) | 19 (5) | 4 (1) | 22 (5) | 68 (4) |
| What else is the oil used for | |||||
| No other purpose | 342 (80) | 326 (78) | n/a | n/a | 668 (79) |
| Other family meals | 72 (17) | 74 (18) | n/a | n/a | 146 (17) |
| Other purpose | 16 (4) | 17 (4) | n/a | n/a | 33 (4) |
| Recipient child consumed the ration the last time it was prepared/served* | 383 (91) | 389 (95) | 345 (94) | 415 (99) | 1532 (94) |
| Recipient child normally consumed the ration | 424 (99) | 412 (99) | 383 (99) | 418 (99) | 1637 (99) |
| How much the recipient child likes the ration* | |||||
| Hates | 1 (0) | 2 (0) | 2 (1) | 3 (1) | 8 (0) |
| Does not like | 17 (4) | 23 (6) | 36 (10) | 11 (3) | 87 (5) |
| Neutral | 14 (3) | 6 (1) | 14 (4) | 11 (3) | 45 (3) |
| Likes | 209 (49) | 176 (42) | 126 (34) | 189 (45) | 700 (43) |
| Loves a lot | 187 (44) | 209 (50) | 198 (53) | 203 (49) | 797 (49) |
| Observed, n | 50 | 55 | 51 | 53 | 209 |
| Ration present on all 4 d2 | 46 (92) | 27 (49) | 25 (49) | 28 (53) | 126 (60) |
| Gave the ration to other households | 1 (2) | 0 | 0 | 1 (4) | 2 (2) |
| Gave the fortified oil to other households | 0 | 0 | n/a | n/a | 0 |
| Gave the porridge to other households | 0 | 2 (7) | 0 | n/a | 2 (2) |
| Used oil for something other than porridge preparation | 18 (39) | 10 (37) | n/a | n/a | 28 (22) |
Values are n (%). Percentages are out of the 1654 completed interviews—16% (318 of 1972) were not completed. CSB+ w/oil, Corn Soy Blend Plus with oil; CSWB w/oil, Corn Soy Whey Blend with oil; RUSF, ready-to-use supplementary food; SC+, Super Cereal Plus.
Percentages of households where activity was observed happening at least once over the 4 d of observation, among households where ration was present on all 4 d. Statistical significance not tested owing to low n.
P < 0.05 from Pearson's chi-square test.
FIGURE 1.
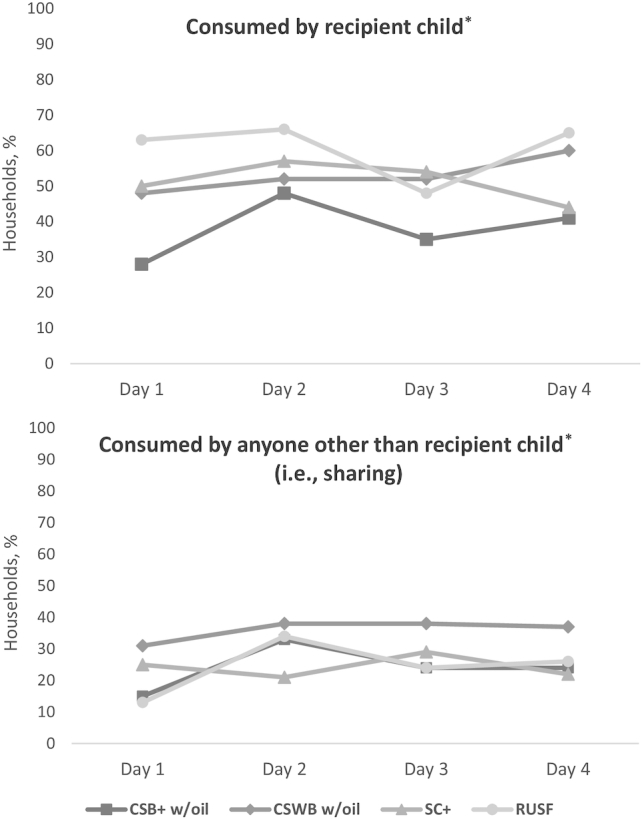
Observed consumption and sharing of the ration by day of observation. *Percentage ever observed among households where the ration was present (CSB+ w/oil: n = 46 on all days; CSWB w/oil: n = 29 on days 1–3 and n = 30 on day 4; SC+: n = 28 on days 1–3 and n = 27 on day 4; RUSF: n = 32 on days 1 and 2, n = 33 on day 3, and n = 31 on day 4). CSB+ w/oil, Corn Soy Blend Plus with oil; CSWB w/oil, Corn Soy Whey Blend with oil; RUSF, ready-to-use supplementary food; SC+, Super Cereal Plus.
It was commonly reported that the ration did not last the entire month as intended, with the highest percentage in the CSWB w/oil arm (Table 3). Among observed households, only 60% had the ration present on all 4 d of the observation, with the lowest in the CSWB w/oil and SC+ arms (Table 3). The percentage of household-days where the child was observed consuming the ration was highest in the RUSF arm (40%) and lowest in the CSWB w/oil arm (28%). Among households where the ration was observed to be present, the recipient child was observed consuming the ration in only 49% of households on average over the 4 d of observation (i.e., the mean of the percentages by day), with the highest in the RUSF arm and the lowest in the CSB+ w/oil arm (Figure 1).
Most caregivers reported that the recipient child either “likes” or “loves the ration a lot”, but a slightly higher percentage reported that the child “does not like” the ration in the SC+ arm (Table 3). In most of the focus group discussions, across all arms, it was described that the recipient child liked the ration a lot, but in some of the discussions, participants said that the recipient child did not accept the ration in any form. In the RUSF arm, refusal was only described in 1 focus group and only when the child was sick. In each of the FBF arms, this theme arose in 2 focus groups, and some offered explanations that included illness or vomiting, whereas others just said the child refused to eat it. A common theme in the CSWB w/oil and SC+ arms was that the child disliked or wouldn't eat the ration as a porridge but did like it in other forms (raw or as couscous).
In 2 separate focus group discussions in the CSWB w/oil arm, a theme arose that the ration was spoiled when they received it, tasted bitter, and could not be used. For example, in 1 of the focus groups a participant described:
Often, there are insects inside, and if we taste it, we find that it's too bitter-tasting. We can't use it to make porridge or couscous. We can only throw it out. (FGD #3, Respondent 3)
Another commented:
Last month, the flour they gave us could not be used, besides giving it to the animals. Even the animals don't want it. It's very bitter. (FGD #3, Respondent 6)
Others described how they were told to exchange the bad flour at the distribution site and how “now the flour is new” and “good.” In another focus group discussion, 1 woman detailed:
Since the beginning, the flour spoils because it spends a long time at the source… Most of the time, this flour expires before it reaches us. When you get this flour and return home, you will often find debris in it. At its starting place, the flour goes bad, before you receive it, and when you get it, it isn't edible, because often it smells bad and it is bitter. Then you have to leave this flour and get your own flour. (FGD #4, Respondent 3)
Sharing and diversion: were the target recipients receiving the food?
Sharing was defined as consumption of the ration by anyone other than the recipient child, as reported during the interview (either usually or the last time it was prepared) or observed in the home. Figure 2 shows the reported and observed percentages of sharing (at all and the mean over the 4 d of observation) by study arm. Sharing was reported in all study arms, with the lowest percentage in the RUSF arm and highest in the CSWB w/oil and SC+ arms (Figure 2). Overall, 66% of caregivers reported sharing. These figures remained consistent in the adjusted analysis. The most commonly reported reasons were other children need or want it (70%); the mother needs it for breastfeeding (21%); and moral obligation to share (22%).
FIGURE 2.
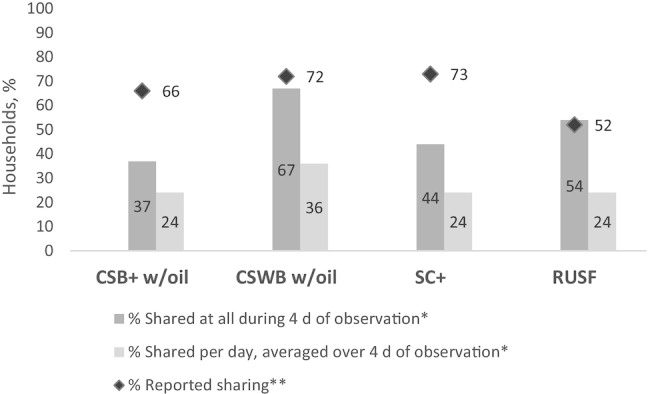
Reported and observed sharing of the ration. *Among the subsample of households that had an in-home observation, where the ration was present (CSB+ w/oil: n = 46 on all days; CSWB w/oil: n = 29 on days 1–3 and n = 30 on day 4; SC+: n = 28 on days 1–3 and n = 27 on day 4; RUSF: n = 32 on days 1 and 2, n = 33 on day 3, and n = 31 on day 4). **Percentage of nonmissing values (<5% missing in each arm). CSB+ w/oil, Corn Soy Blend Plus with oil; CSWB w/oil, Corn Soy Whey Blend with oil; RUSF, ready-to-use supplementary food; SC+, Super Cereal Plus.
Of the households where the ration was present, a total of 48% were observed sharing at least once over the course of the 4 d, with the lowest percentage in CSB+ w/oil and the highest in CSWB w/oil (Figure 2). On average across the 4 d of observation, observed sharing was highest in CSWB w/oil (36%) and similar among the other arms (Figure 2). Figure 1 displays the percentages of households that shared by day of observation, which does not appear to indicate alterations in behavior as households habituated to the enumerator's presence over the 4-d period.
In focus group discussions, the ration not lasting the full 30 d as intended was a common theme in the CSWB w/oil and RUSF arms. In CSWB w/oil, respondents said the ration did not last because it got shared or eaten by others, whereas in RUSF respondents said that the recipient child ate more than the recommended daily amount. Sharing of the ration was commonly described in all study arms, most often with siblings or other children. Some participants described a sense of moral obligation to share either with other children or with others who did not receive the ration:
You must take some of your ration to give to them, in this way, if one day you find yourself in the same situation, they will take some of their ration to give to you. (FGD #11, Respondent 1)
When you receive the ration, once you are at home, you have to share it. You can't say that this one isn't the beneficiary, so you won't give it to him. (FGD #18, Respondent 10)
Others talked about how older children in the household wanted the ration and would take it when the mother was out of the house:
If you don't give it to the little children, they can't get it, but the older children always have strategies to get the ration in case you're on a prolonged absence. (FGD #3, Respondent 5)
There was no reported selling of any of the ration in any of the study arms. A total of 13% of caregivers reported giving the ration to other households, with the highest percentage in the SC+ arm, consistent with the adjusted analysis. In the CSB+ w/oil and CSWB w/oil arms, smaller percentages reported having given the oil away (Table 3). There was no observed giving away of the (unprepared) CSB+ w/oil, CSWB w/oil, SC+, or oil rations to other households. Two households were observed giving away the RUSF, and 2 were observed giving away porridge in the CSWB w/oil arm (Table 3). When prompted about selling in focus group discussions, participants adamantly explained that they did not sell. None indicated having ever sold or exchanged the ration.
In the SC+ and RUSF arms, almost no one reported using the ration for other purposes. The CSB+ w/oil and CSWB w/oil arms had higher percentages reporting they used the ration for other family meals or other purposes, with the highest percentage in the CSWB w/oil arm. These relations persisted in the adjusted analysis. Similar percentages (∼20%) in the CSB+ w/oil and CSWB w/oil arms reported using the fortified oil for other family meals or other purposes (Table 3). The percentages observed using oil for other purposes in the CSB+ w/oil and CSWB w/oil arms were higher than reported (Table 3).
Preparation: were recipient households preparing the food as intended? (FBF arms)
Analysis of porridge samples collected during the interviews showed mean quantities of total fat per 100 g dry matter to be 12.9 g in CSB+ w/oil, 13.9 g in CSWB w/oil, and 5.0 g in SC+ (less than indicated on the specification for SC+). The mean quantities of added oil per 100 g dry matter in CSB+ w/oil and CSWB w/oil were 7.3 g and 6.3 g, respectively, far lower than the recommended 30 g/100 g which caregivers were instructed to add. Among the observed porridge preparation occasions, ingredients were observed to be measured most of the time in the CSB+ w/oil and CSWB w/oil arms, but only on some occasions in the SC+ arm (Figure 3).
FIGURE 3.
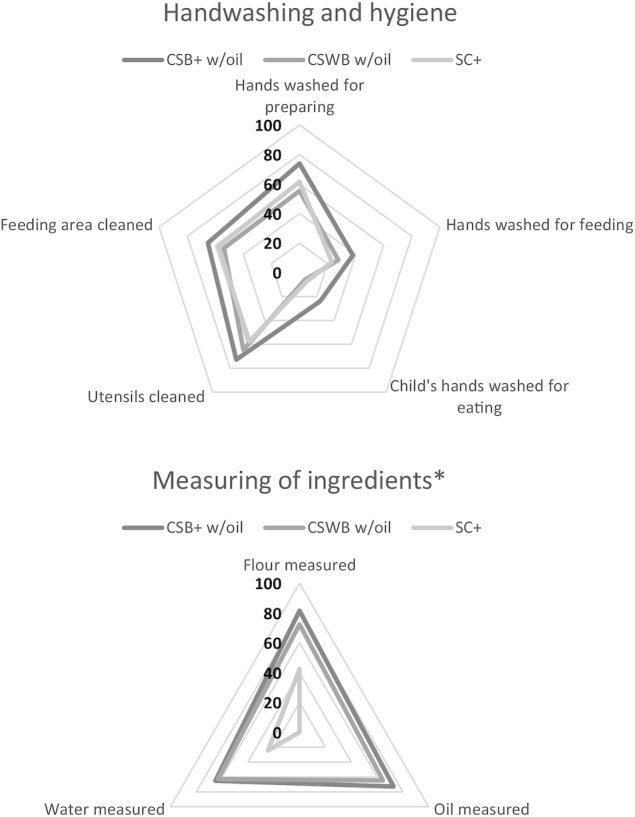
Gaps in handwashing and measuring of ingredients observed during porridge preparations. *SC+ not delivered with oil, so oil measured is not applicable. CSB+ w/oil, Corn Soy Blend Plus with oil; CSWB w/oil, Corn Soy Whey Blend with oil; SC+, Super Cereal Plus.
In the FBF arms, among households where the ration was present, less than half were observed preparing the porridge on average over the 4 d of observation, i.e., the means of the percentages by day were 35%, 48%, and 46% in the CSB+ w/oil, CSWB w/oil, and SC+ arms, respectively. A common theme in focus group discussions was the opportunity costs of preparing or serving the ration. In all study arms (including RUSF), it was often described that there was difficulty preparing or serving the ration 3 times/d as instructed because it interfered with other activities. Some in the FBF arms described how they could not comply if they were away from the home, particularly during the rainy season when they were working in the fields:
There are times when you have to go away from morning until night. If you make it for the child in the morning, you can only make it for him in the evening, because you aren't there at noon. (FGD #4, Respondent 3)
We often want to give it 3 times a day, but often we can't do it. Since often we're in a rush to go somewhere else. (FGD #23, Respondent 2)
Others, however, expressed that it did not interfere with other activities and that they had no problem following the recommendations.
Storage and hygiene
Most household water samples showed unsafe or high-risk contamination with E. coli, with similar percentages across the study arms (72–78%). During the observed porridge preparations, the recommended handwashing and cleaning practices were followed most of the time, but handwashing before feeding was followed less (Figure 3). Almost all ration storage was observed to be indoors, off the floor, and sealed or covered, or kept in the original container with some differences between arms (Table 4). The unadjusted and adjusted percentages were consistent.
TABLE 4.
Storage of the ration observed during interviews1
| CSB+ w/oil | CSWB w/oil | SC+ | RUSF | Total | |
|---|---|---|---|---|---|
| Ration storage observed,*n | 430 | 418 | 385 | 421 | 1654 |
| Yes | 301 (70) | 220 (53) | 233 (61) | 279 (66) | 1033 (63) |
| No, there is no more food | 95 (22) | 169 (41) | 130 (34) | 90 (21) | 484 (29) |
| Refuse/cannot access food | 33 (8) | 130 (34) | 17 (4) | 51 (12) | 128 (8) |
| Where the ration was stored, n | 301 | 220 | 233 | 279 | 1033 |
| Indoors2 | 297 (99) | 219 (100) | 232 (100) | 277 (99) | 1025 (99) |
| Outdoors in the shade2 | 0 (0) | 2 (1) | 0 (0) | 1 (0) | 3 (0) |
| Outdoors not in the shade2 | 0 (0) | 0 (0) | 0 (0) | 1 (0) | 1 (0) |
| Off the floor | 211 (70) | 164 (75) | 163 (70) | 194 (70) | 732 (71) |
| On the floor* | 19 (6) | 32 (15) | 19 (8) | 27 (10) | 97 (9) |
| Hanging* | 7 (2) | 12 (5) | 4 (2) | 27 (10) | 50 (5) |
| Sealed/covered* | 252 (84) | 176 (80) | 183 (79) | 203 (73) | 814 (79) |
| Unsealed/open | 11 (4) | 12 (5) | 5 (2) | 4 (1) | 32 (3) |
| Kept in the original container* | 228 (76) | 134 (61) | 203 (87) | 193 (69) | 758 (73) |
| Other | 44 (15) | 48 (22) | 53 (23) | 62 (22) | 207 (20) |
Values are n (%). Percentages are out of the 1654 completed interviews—16% (318 of 1972) were not completed. CSB+ w/oil, Corn Soy Blend Plus with oil; CSWB w/oil, Corn Soy Whey Blend with oil; RUSF, ready-to-use supplementary food; SC+, Super Cereal Plus.
Statistical significance not tested owing to exceedingly low variability.
P < 0.05 from Pearson's chi-square test.
Difficulty maintaining proper hygiene was a common theme across all arms in the focus group discussions. In several, participants explained that they did not have the means to buy soap. Some said that they used ash or lye or just water to wash hands when soap was not available. With regard to storage, it was described in only 1 focus group in each arm that they did not have good sealed containers. In a few focus groups in the CSB+ w/oil and CSWB w/oil arms, participants described that they needed good covers and containers or that insects got inside when they stored the ration.
Discussion
This study found that the 4 SNFs delivered in this intervention were not always used as intended or instructed, which could partly explain their limited effectiveness. Sharing and other diversion of the foods was common across all arms in this study, and many other studies have found similarly high levels (23–26). In a real-world context, sharing within and sometimes across households is largely unavoidable, especially among other children in the household with whom caregivers feel a sense of moral obligation to share. There is a common perception that RUSF is not shared because it is perceived as medicine (27). In this study, however, we saw that sharing was common among all 4 arms, including RUSF. This appears to vary in the literature. Another mass supplementation program also found similar sharing of RUSF (28), but another study in Ethiopia assessing treatment of moderate acute malnutrition found that RUSF was shared in only 2% of households (29). We did not see any evidence of corruption or selling of the SNFs for monetary gain in this study. No caregivers reported or were observed selling any of the SNFs. Because quantities delivered and distributed were closely monitored, there was little chance that the SNFs were diverted at the distribution site before distribution.
We found that children were not consuming as much of the SNF as intended and that there were challenges to preparing or serving the ration 2–3 times daily as instructed. Although we did not measure the quantity consumed when the child was eating the ration, we did observe that it was not consumed daily, contrary to the recommendation to feed the foods 2–3 times/d. This finding has been replicated in other studies showing that children do not consume the intended quantities of supplementary foods (30, 31). These studies have shown, for both lipid-based nutrient supplements and FBF products, that children are not likely to consume the intended doses (30, 31). But they may be more likely to consume lipid-based nutrient supplements than FBF, as was consistent in our study with slightly higher percentages of recipient children observed consuming the ration in the RUSF arm. The challenge of ration preparation or serving interfering with other activities was described by caregivers in all arms in this study. But this challenge may be more context specific. In another study that explored the relation between time spent in agriculture and dietary diversity, the direction of association varied depending on context and socioeconomic status (32).
The reports of bitterness and spoilage in the CSWB w/oil arm may partly explain the higher sharing and low consumption by the recipient children, even though caregivers reported that their children liked the ration during the interviews. We would expect to see more sharing if the SNF was not liked, as may have been the case for the CSWB w/oil arm (i.e., if the child does not want to eat the ration, then logically it will be shared more). The bitter taste may have resulted from the storage conditions in Burkina Faso. Before conducting this study, each of the 4 foods was tested for acceptability among the recipient population, and all 4 foods were deemed acceptable (33). Each of the products used in food aid programs has specified temperatures at which it should be stored; often Burkina Faso and likely other recipient countries experience much higher temperatures. When storage time was not considered, other studies have found that CSB with dairy protein was not perceived as bitter, and that products with dairy were actually perceived as having an overall sweet taste (31, 34). In organoleptic lab tests conducted by North Carolina State University, however, professional tasters agreed that CSWB that had been stored in Burkina Faso for ≥10 mo was bitter, whereas newer batches of the same product did not have the same bitter, stale, and fishy aftertaste. This points to the importance of conducting accelerated shelf-life studies on all new products, replicating the actual in-country temperatures and storage conditions (35). Other researchers may consider this in future studies of the effectiveness of SNF products, and directly assess whether differences exist among SNF products in terms of acceptability after prolonged periods of storage under extreme heat or other local conditions.
Analysis of porridge samples in CSB+ w/oil and CSWB w/oil indicated lower fat content than would be expected if preparation recommendations were followed. A 2011 report recommended a target ratio of 30 g added oil per 100 g CSB in order to achieve a fat content closer to that of RUSF, but this was not achieved in this program (36). A previous study found that with targeted and intensive social and behavior change communication, it is possible for caregivers to achieve a higher oil:CSB ratio, closer to the target, in prepared porridge (37). The ViM program did include a standard social and behavior change communication component about porridge preparation; however, this study shows that more intensive communication may be necessary if caregivers are expected to achieve the target oil-to-flour ratios. But we do not yet know how preparation of porridge at this ratio affects child growth outcomes. If recipients in the CSB+ w/oil and CSWB w/oil arms had consumed the porridge exactly as instructed with the quantities of oil that were programmed, we might reasonably expect they would have performed comparatively better than they did. Irrespective of the oil:CSB ratio, if the ration is not being consumed, it will of course not be effective.
Food consumption alone does not equate to adequate health and nutritional status or wholly explain growth faltering; other environmental factors, such as hygiene practices and prevalence of infections, also have an impact (38–40). In this program, the foods were delivered with social and behavior change communication encouraging hygienic preparation, consumption, and storage of the ration (e.g., handwashing with soap, cleaning of the feeding area, washing of all utensils, storage in sealed containers). But these behaviors alone may not overcome the risk of contaminated drinking water that was observed in this study. Across all study arms, the majority of household water was contaminated with levels of E. coli that were either unsafe or high risk. This finding indicates the potential presence of concurrent, repeated, or subclinical infections or environmental enteric dysfunction which may help explain why provision of SNFs did not have more dramatic effects in improving nutritional status in these settings (40, 41).
In our primary analysis we found the CSWB w/oil arm to be less effective than CSB+ w/oil, but it does not seem likely that this is due to nutrient composition (CSWB w/oil differs from CSB+ w/oil by the addition of whey protein concentrate). The higher levels of sharing and reports of bitter taste may partly explain the lower effectiveness in the CSWB w/oil arm. Other studies have found differences in effectiveness of SNFs, but relatively few have examined reasons for this other than the composition and nutrient profile of the foods, or how effectiveness could be improved by methods other than adjusting ingredients in the food product; further research is needed in this area (16, 42). More studies are now addressing water and sanitation/hygiene in nutritional interventions and the role of environmental enteric dysfunction on growth outcomes (40, 43). Future analyses should evaluate water and sanitation/hygiene behaviors with respect to anthropometric outcomes. In preliminary analyses, we did not find significant associations between any of the behaviors assessed in this article and stunting or wasting. In addition, multisectoral approaches are now being considered. The US Agency for International Development's multisectoral nutrition strategy considers combinations of interventions that include both nutrition-specific and nutrition-sensitive components such as family planning, food safety, nutrition-sensitive agriculture, girls’ and women's education, and economic strengthening, livelihoods, and social protection (44).
There are some limitations to this study. These findings are specific to the context of a blanket supplementary feeding program in Burkina Faso and may differ in other settings. Self-reported data may not be an accurate reflection of true behavior, because caregivers may have overreported what they thought was “good” behavior and underreported what they thought was “bad” behavior. We included in-home observations to get a better understanding of household behaviors, but it is possible that households may have altered their behavior due to the presence of an observer. We included 4 d of observation per household to limit this effect but did not see any evidence that the behavior had changed over the course of the observation.
These findings underscore an important message: the approach used in programming and the household use of SNFs matter at least as much as the composition of the products. We need more evidence of effective programming actions surrounding delivery of food aid as well as multisectoral interventions to address the prevention of stunting and wasting. Future studies could investigate the effectiveness of addressing some of the factors identified in this article, e.g., testing the effect of different ration sizes (or addition of family rations, vouchers, or cash) on household sharing and whether that affects growth outcomes and cost-effectiveness. Better programming requires more attention to barriers to correct food preparation, and drivers of food consumption including cultural norms related to sharing within the household.
ACKNOWLEDGEMENTS
We specifically thank Benoit Sawadogo from Institut de Recherche en Sciences de la Santé for his data management in the field. In addition, we thank Jocelyn Boiteau, Lindsey Green, and Adeline Kologo of Tufts University for their administrative support throughout the study and Nicole Masozera for her assistance with qualitative data analysis. The authors’ responsibilities were as follows—LN, ANZ, HBL, FG, and IRC: conducted the research; BLR, PW, and SMW: designed the research; BKL, IRC, DJS, and YS: analyzed the data and wrote the paper; BLR: had primary responsibility for the final content; and all authors: read and approved the final manuscript.
Notes
Supported by the Office of Food for Peace, Bureau for Democracy, Conflict, and Humanitarian Assistance, US Agency for International Development, under the terms of contract no. AID-OAA-C-16-00020 (to PW).
Author disclosures: The authors report no conflicts of interest.
The opinions expressed herein are those of the authors and do not necessarily reflect the views of the US Agency for International Development.
All quantitative data used for the publication of this article will be publicly available through the USAID Development Data Library: https://data.usaid.gov. In addition, the study protocol and data can be made available by the corresponding author upon request.
Abbreviations used: CSB+ w/oil, Corn Soy Blend Plus with oil; CSWB w/oil, Corn Soy Whey Blend with oil; FBF, fortified blended food; RUSF, ready-to-use supplementary food; SC+, Super Cereal Plus; SNF, specialized nutritious food.
References
- 1. Victora CG, de Onis M, Hallal PC, Blossner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125:e473–80. [DOI] [PubMed] [Google Scholar]
- 2. Dewey KG, Vitta BS. Strategies for ensuring adequate nutrient intake for infants and young children during the period of complementary feeding. [Internet] Insight: ensuring adequate nutrition. Alive&Thrive Technical Brief (7) Washington (DC): Alive&Thrive; 2013; [cited 2018 July 11]. Available from: https://www.aliveandthrive.org/wp-content/uploads/2018/07/Insight-Issue-7_Ensuring-Adequate-Nutrition.pdf. [Google Scholar]
- 3. Dewey KG. The challenge of meeting nutrient needs of infants and young children during the period of complementary feeding: an evolutionary perspective. J Nutr. 2013;143:2050–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. WHO. Complementary feeding. [Internet] Geneva: WHO; 2016; [cited 2018 July 11]. Available from: http://www.who.int/nutrition/topics/complementary_feeding/en/. [Google Scholar]
- 5. 1,000 Days. Homepage—1,000 Days. [Internet] Washington (DC): 1,000 Days, 2010; [cited 2018 July 11]. Available from: https://thousanddays.org/. [Google Scholar]
- 6. Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, Haider BA, Kirkwood B, Morris SS, Sachdev H et al.. What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371:417–40. [DOI] [PubMed] [Google Scholar]
- 7. Imdad A, Yakoob MY, Bhutta ZA. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health. 2011;11:S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stephenson KB, Agapova SE, Divala O, Kaimila Y, Maleta KM, Thakwalakwa C, Ordiz MI, Trehan I, Manary MJ. Complementary feeding with cowpea reduces growth faltering in rural Malawian infants: a blind, randomized controlled clinical trial. Am J Clin Nutr. 2017;106:1500–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Christian P, Shaikh S, Shamim AA, Mehra S, Wu L, Mitra M, Ali H, Merrill RD, Choudhury N, Parveen M et al.. Effect of fortified complementary food supplementation on child growth in rural Bangladesh: a cluster-randomized trial. Int J Epidemiol. 2015;44:1862–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bhandari N, Bahl R, Nayyar B, Khokhar P, Rohde JE, Bhan MK. Food supplementation with encouragement to feed it to infants from 4 to 12 months of age has a small impact on weight gain. J Nutr. 2001;131:1946–51. [DOI] [PubMed] [Google Scholar]
- 11. Isanaka S, Nombela N, Djibo A, Poupard M, Van Beckhoven D, Gaboulaud V, Guerin PJ, Grais RF. Effect of preventive supplementation with ready-to-use therapeutic food on the nutritional status, mortality, and morbidity of children aged 6 to 60 months in Niger: a cluster randomized trial. JAMA. 2009;301:277–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr. 2008;4:24–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huybregts L, Houngbe F, Salpeteur C, Brown R, Roberfroid D, Ait-Aissa M, Kolsteren P. The effect of adding ready-to-use supplementary food to a general food distribution on child nutritional status and morbidity: a cluster-randomized controlled trial. PLoS Med. 2012;9:e1001313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Islam MM, Khatun M, Peerson JM, Ahmed T, Mollah MAH, Dewey KG, Brown KH. Effects of energy density and feeding frequency of complementary foods on total daily energy intakes and consumption of breast milk by healthy breastfed Bangladeshi children. Am J Clin Nutr. 2008;88(1):84–94. [DOI] [PubMed] [Google Scholar]
- 15. Panjwani A, Heidkamp R. Complementary feeding interventions have a small but significant impact on linear and ponderal growth of children in low- and middle-income countries: a systematic review and meta-analysis. J Nutr. 2017;147:2169S–78S. [DOI] [PubMed] [Google Scholar]
- 16. Kristjansson E, Francis D, Liberato S, Greenhalgh T, Welch V, Jandu MB, Batal M, Rader T, Noonan E, Janzen L et al.. Supplementary feeding for improving the health of disadvantaged infants and children: what works and why? 3ie Systematic Review Summary 5. London: 3ie (International Initiative for Impact Evaluation); 2016. [Google Scholar]
- 17. Iuel-Brockdorf AS, Ouedraogo A, Ritz C, Draebel TA, Ashorn P, Filteau S, Michaelsen KF. Feeding behaviors during home-based treatment of moderate acute malnutrition using corn-soy blends or lipid-based nutrient supplements. Matern Child Nutr. 2017;13:e12399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harding KL, Aguayo VM, Webb P. Factors associated with wasting among children under five years old in South Asia: implications for action. PLoS One. 2018;13:e0198749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rogers B, Webb P, Wanke C, Sadler K, Masterson AR, Bagriansky J, Schlossman N, Narayan A, Tilahun J. Selection and use of US Title II food aid products in programming contexts. Food Nutr Bull. 2011;32(3 Suppl):S152–65. [DOI] [PubMed] [Google Scholar]
- 20. Schlossman N. Delivering improved nutrition: dairy ingredients in food aid products. Food Nutr Bull. 2016;37(Suppl 1):S6–13. [DOI] [PubMed] [Google Scholar]
- 21. Suri DJ, Moorthy D, Rosenberg IH. The role of dairy in effectiveness and cost of treatment of children with moderate acute malnutrition: a narrative review. Food Nutr Bull. 2016;37(2):176–85. [DOI] [PubMed] [Google Scholar]
- 22. US Census Bureau. Integrated System for Survey Analysis 6.0. Census and Survey Processing System (CSPro). Suitland (MD): US Census Bureau; 2014. [Google Scholar]
- 23. Osendarp S, Rogers B, Ryan K, Manary M, Akomo P, Bahwere P, Belete H, Zeilani M, Islam M, Dibari F et al.. Ready-to-use foods for management of moderate acute malnutrition: considerations for scaling up production and use in programs. Food Nutr Bull. 2015;36:S59–64. [DOI] [PubMed] [Google Scholar]
- 24. Abbeddou S, Hess SY, Yakes Jimenez E, Some JW, Vosti SA, Guissou RM, Ouedraogo J-B, Brown KH. Comparison of methods to assess adherence to small-quantity lipid-based nutrient supplements (SQ-LNS) and dispersible tablets among young Burkinabe children participating in a community-based intervention trial. Matern Child Nutr. 2015;11(Suppl 4):90–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Iuel-Brockdorf AS, Draebel TA, Ritz C, Fabiansen C, Cichon B, Brix Christensen V, Yameogo C, Oummani R, Briend A, Michaelsen KF et al.. Evaluation of the acceptability of improved supplementary foods for the treatment of moderate acute malnutrition in Burkina Faso using a mixed method approach. Appetite. 2016;99:34–45. [DOI] [PubMed] [Google Scholar]
- 26. Tadesse E, Berhane Y, Hjern A, Olsson P, Ekström EC. Perceptions of usage and unintended consequences of provision of ready-to-use therapeutic food for management of severe acute child malnutrition. A qualitative study in southern Ethiopia. Health Policy Plan. 2015;30:1334–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Karakochuk C, Van Den Briel T, Stephens D, Zlotkin S. Treatment of moderate acute malnutrition with ready-to-use supplementary food results in higher overall recovery rates compared with a corn-soya blend in children in southern Ethiopia: an operations research trial. Am J Clin Nutr. 2012;96:911–16. [DOI] [PubMed] [Google Scholar]
- 28. Grellety E, Shepherd S, Roederer T, Manzo ML, Doyon S, Ategbo EA, Grais RF. Effect of mass supplementation with ready-to-use supplementary food during an anticipated nutritional emergency. PLoS One. 2012;7:e44549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Karakochuk CD, van den Briel T, Stephens D, Zlotkin S. Food sharing practices in households receiving supplemental foods for the treatment of moderate acute malnutrition in Ethiopian children. J Hunger Environ Nutr. 2015;10:343–55. [Google Scholar]
- 30. Ashorn U, Alho L, Arimond M, Dewey KG, Maleta K, Phiri N, Phuka J, Vosti SA, Zeilani M, Ashorn P. Malawian mothers consider lipid-based nutrient supplements acceptable for children throughout a 1-year intervention, but deviation from user recommendations is common. J Nutr. 2015;145:1588–95. [DOI] [PubMed] [Google Scholar]
- 31. Iuel-Brockdorf AS, Draebel TA, Fabiansen C, Cichon B, Christensen VB, Yameogo C, Ritz C, Frahm Olsen M, Friis H. Acceptability of new formulations of corn-soy blends and lipid-based nutrient supplements in Province du Passoré, Burkina Faso. Appetite. 2015;91:278–86. [DOI] [PubMed] [Google Scholar]
- 32. Komatsu H, Malapit HJL, Theis S. Does women's time in domestic work and agriculture affect women's and children's dietary diversity? Evidence from Bangladesh, Nepal, Cambodia, Ghana, and Mozambique. Food Policy. 2018;79:256–70. [Google Scholar]
- 33. Saleh N. ViM beneficiary taste tests of Title II food aid products Sanmantenga Province, Burkina Faso: a report prepared for the Food Aid Quality Review. [Internet] Boston (MA): Tufts University's Friedman School of Nutrition Science and Policy; 2013; [cited 2018 July 11]. Available from: http://foodaidquality.org/sites/default/files/publications/ViMfullversion-min.pdf. [Google Scholar]
- 34. Kehlet U, Kæstel P, Hausner H, Bredie WLP, Allesen-Holm BH. Sensory characteristic of corn soya blend and the effects of milk protein replacement. Afr J Food Sci. 2011;5:200–7. [Google Scholar]
- 35. Schlossman N, Johnson Q, Wood L, Coglianese N, Santoso V, Koeppel L. Accelerated shelf life studies: methods and results relating to new and upgraded food aid products. [Internet] Washington (DC): USAID; 2015; [cited 2018 July 11]. Available from: https://foodaidquality.org/sites/default/files/publications/Accelerated%20Shelf%20Life%20Studies%20Methods%20and%20Results%20Relating%20to%20New%20and%20Upgraded%20Food%20Aid%20Products.pdf. [Google Scholar]
- 36. Webb P, Lorge Rogers B, Rosenberg I, Schlossman N, Wanke C, Bagriansky J, Sadler K, Johnson Q, Tilahun J, Reese Masterson A et al.. Improving the nutritional quality of U.S. food aid: recommendations for changes to products and programs. [Internet] Boston (MA): Tufts University; 2011; [cited 2018 July 11]. Available from: https://pdf.usaid.gov/pdf_docs/pnadz841.pdf. [Google Scholar]
- 37. Rogers BL, Wilner LB, Maganga G, Walton SM, Suri DJ, Langlois BK, Chui KKH, Boiteau JM, Vosti SA, Webb P. Program changes are effective and cost-effective in increasing the amount of oil used in preparing corn soy blend porridge for treatment of moderate acute malnutrition in Malawi. Matern Child Nutr. 2017;13:e12393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Crane RJ, Berkley JA. Progress on growth faltering. Lancet Glob Health. 2017;5:e125–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ngure FM, Reid BM, Humphrey JH, Mbuya MN, Pelto G, Stoltzfus RJ. Water, sanitation, and hygiene (WASH), environmental enteropathy, nutrition, and early child development: making the links. Ann N Y Acad Sci. 2014;1308:118–28. [DOI] [PubMed] [Google Scholar]
- 40. Israel M, Albert J, Annis J. Toward a hygienic environment for infants and young children: a review of the literature. [Internet] Washington (DC): USAID/WASHPaLS Project; 2018; [cited 2018 July 11]. Available from: https://www.tetratech.com/en/documents/toward-a-hygienic-environment-for-infants-and-young-children-a-review-of-the-literature. [Google Scholar]
- 41. Black RE, Brown KH, Becker S. Effects of diarrhea associated with specific enteropathogens on the growth of children in rural Bangladesh. Pediatrics. 1984;73(6):799–805. [PubMed] [Google Scholar]
- 42. Lazzerini M, Rubert L, Pani P. Specially formulated foods for treating children with moderate acute malnutrition in low- and middle-income countries. Cochrane Database Syst Rev. 2013;(6):CD009584. [DOI] [PubMed] [Google Scholar]
- 43. Humphrey JH, Jones AD, Manges A, Mangwadu G, Maluccio JA, Mbuya MNN, Moulton LH, Ntozini R, Prendergast AJ, Stoltzfus RJ et al.. The Sanitation Hygiene Infant Nutrition Efficacy (SHINE) trial: rationale, design, and methods. Clin Infect Dis. 2015;61:S685–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. USAID Multi-Sectoral Nutrition Strategy 2014–2025. [Internet] Washington (DC): USAID; 2014; [cited 2018 July 11]. Available from: https://www.usaid.gov/sites/default/files/documents/1867/USAID_Nutrition_Strategy_5-09_508.pdf. [Google Scholar]


