Abstract
Objective:
Circadian dysregulation plays an important role in the etiology of mood disorders. Evening chronotype is frequent in these patients. However, prospective studies about the influence of chronotype on mood symptoms have reached unclear conclusions in patients with bipolar disorder (BD). The objective of this study was to investigate relationship between chronotype and prognostic factors for BD.
Methods:
At the baseline, 80 euthymic BD patients answered a demographic questionnaire and clinical scales to evaluate anxiety, functioning and chronotype. Circadian preference was measured using the Morningness-Eveningness Questionnaire, in which lower scores indicate eveningness. Mood episodes and hospitalizations were evaluated monthly for 18 months.
Results:
Among the BD patients, 14 (17.5%) were definitely morning type, 35 (43.8%), moderately morning, 27 (33.7%) intermediate (neither) and 4 (5%) moderately evening. Eveningness was associated with obesity or overweight (p = 0.03), greater anxiety (p = 0.002) and better functioning (p = 0.01), as well as with mood episodes (p = 0.04), but not with psychiatric hospitalizations (p = 0.82). This group tended toward depressive episodes (p = 0.06), but not (hypo)mania (p = 0.56).
Conclusion:
This study indicated that evening chronotype predicts a poor prognostic for BD. It reinforces the relevance of treating rhythm disruptions even during euthymia to improve patient quality of life and prevent mood episodes.
Keywords: Chronotype, circadian rhythm, bipolar disorder, prognosis
Introduction
Circadian dysregulation can play an important role in the etiology of mood disorders1 and is highly prevalent among those who suffer from mood disorders. In fact, sleep alterations are one of the most important diagnostic criteria for these disorders. Patients with bipolar disorder (BD) show more circadian alterations, even in drug-naïve individuals and independently of mood status. They usually have more irregular sleep and social patterns, abnormal melatonin and cortisol secretion and mutations in clock genes.2
Evening chronotype is often associated with mood disorders.3,4 A large cohort study showed that depressive and anxiety disorders are associated with late circadian preference, even adjusting for sociodemographic and sleep-related factors.5 Eveningness is more common in adult BD patients. However, studies about the influence of chronotype on mood symptoms have shown conflicting results.1 Thus, more prospective studies are necessary.
The objective of this study was to investigate relationship between chronotype and prognostic factors for BD, including anxiety, functioning, mood episodes and hospitalizations.
Methods
A total of 80 euthymic BD patients were selected from four Brazilian institutions and were evaluated monthly for 18 months. At baseline, the euthymic condition of all participants was confirmed by the Hamilton Depression Rating Scale (HAM-D) and the Young Mania Rating Scale (YMRS) (i.e., HAM-D scores < 7 and YMRS < 8). Three psychiatrists blinded to participant chronotype verified the occurrence of mood episodes and hospitalizations monthly for 18 months. HAM-D scores > 7 or YMRS scores > 8 indicated depressive or (hypo)mania episodes, respectively.
The weight, height, waist, hip and neck circumference of each patient were measured, and body mass index (BMI) was calculated. BMI was used to classify patients as eutrophic (17.5-24.9) or overweight/obese (≥ 25). Waist values > 94 cm in men and > 80 cm in women indicated change. The recommended waist-hip ratio was less than 0.9 in men and 0.85 in women.6 Neck circumference greater than 40 cm in men and 37 cm in women suggested an increased risk of obstructive sleep apnea-hypopnea syndrome.7
The Hamilton Anxiety Rating Scale (HAM-A) and the Functioning Assessment Short Test (FAST) were applied to evaluate anxiety and functioning levels, respectively. The HAM-A includes 14 items that are scored from 0 to 4. In this study, we defined patients as anxious when they scored 18 or more on this scale.8 The FAST, which verifies BD patient functioning in the last 15 days, consists of 24 items that are divided into six categories: autonomy, working, cognition, finances, interpersonal relationships and leisure. Higher scores suggest lower functionality. A cutoff point has not been set.9
Psychiatrists assessed the patients’ chronotype using the Morningness-Eveningness Questionnaire (MEQ). The sum of all scores was converted into a five‐point MEQ scale as follows: ‘definitely morning type’, score 70-86; ‘moderately morning type’, score 59-69; ‘intermediate (neither) type’, score 42-58; ‘moderately evening type’, score 31-41; and ‘definitely evening type’, score 16-30.
The local ethics committee evaluated and approved the study. All patients participated voluntarily, giving written informed consent.
The statistical analyses were performed with SPSS version 24.0. Chronotype was analyzed as a continuous variable in most of the analyses. The Mann-Whitney test was used to determine associations between chronotype and categorical variables, such as gender, smoking, obesity/overweight, etc. Variations in anxiety and functioning levels (other continuous variables) were analyzed according to chronotype with nonparametric linear regression. Logistic regression was used to evaluate the relationship between circadian preference and prognostic measures, which were defined as the occurrence of mood episodes and psychiatric hospitalizations (dichotomous variables).
Results
Most patients were female (n=49; 61.3%), and the age range was 20 to 68 years (mean: 42.4±12.7). BD-I was the most prevalent diagnosis (n=69; 86.3%). The majority (n=55, 68.7%) had at least one psychiatric hospitalization, and 37 (46.2%) had three or more hospitalizations. The mean HAM-D and YMRS scores were 0.54±1.3 and 0.53±1.3, respectively.
The majority of the patients were overweight or obese (78.8%), had abnormal waist circumference (81.3%) and increased waist-hip ratio (77.5%). Thirty-five patients (43.7%) had increased neck circumference.
Among the patients, 14 (17.5%) were definitely morning type, 35 (43.8%), moderately morning, 27 (33.7%) intermediate (neither) and 4 (5%) moderately evening. No definitely evening individuals were identified. The mean MEQ score was 61.05±1.1.
Overweight/obese patients had lower MEQ scores, which suggests eveningness (Mann-Whitney, p = 0.03). There were no MEQ score differences with respect to gender (Mann-Whitney, p = 0.36), age (Correlation, p = 0.14), smoking (Mann-Whitney, p = 0.58), alcohol use (Mann-Whitney, p = 0.52), disorder duration (Correlation, p = 0.28), increased waist size (Mann-Whitney, p = 0.16), increased waist-hip ratio (Mann-Whitney, p = 0.85) or increased neck circumference (Mann-Whitney, p = 0.26) (Table 1).
Table 1. Sociodemographic, anthropometric and clinical data according to chronotype.
| Variables/categories | Mean MEQ | Standard error | p-values |
|---|---|---|---|
| Sociodemographic data | |||
| Gender | |||
| Male | 60.1 | 1.6 | 0.36* |
| Female | 61.6 | 1.5 | |
| Smoking | |||
| Yes | 62.3 | 2.7 | 0.58* |
| No | 60.7 | 1.2 | |
| Alcohol use | |||
| Yes | 57.8 | 4.4 | 0.52* |
| No | 61.4 | 1.1 | |
| Anthropometric data | |||
| BMI | |||
| Normal | 65.4 | 2.6 | 0.03* † |
| Increased | 59.8 | 1.1 | |
| Waist | |||
| Normal | 64.6 | 1.8 | 0.16* |
| Increased | 60.2 | 1.2 | |
| Waist-hip ratio | |||
| Normal | 61.3 | 2.3 | 0.85* |
| Increased | 60.9 | 1.2 | |
| Neck circumference | |||
| Normal | 61.8 | 1.4 | 0.26* |
| Increased | 59.6 | 1.7 | |
| Prospective data | |||
| Mood episodes in general | |||
| Present | 58.5 | 1.7 | 0.04†‡ |
| Absent | 63.0 | 1.4 | |
| Depressive episodes | |||
| Present | 56.7 | 2.2 | 0.06ठ|
| Absent | 62.1 | 1.2 | |
| (Hypo)manic episodes | |||
| Present | 60.0 | 2.1 | 0.56‡ |
| Absent | 61.4 | 1.3 | |
| Psychiatric hospitalizations | |||
| Present | 60.5 | 2.2 | 0.82‡ |
| Absent | 61.1 | 1.3 |
BMI = body mass index; MEQ = Morningness-Eveningness Questionnaire.
Mann-Whitney test;
statistically significant;
logistic regression;
trend to significance.
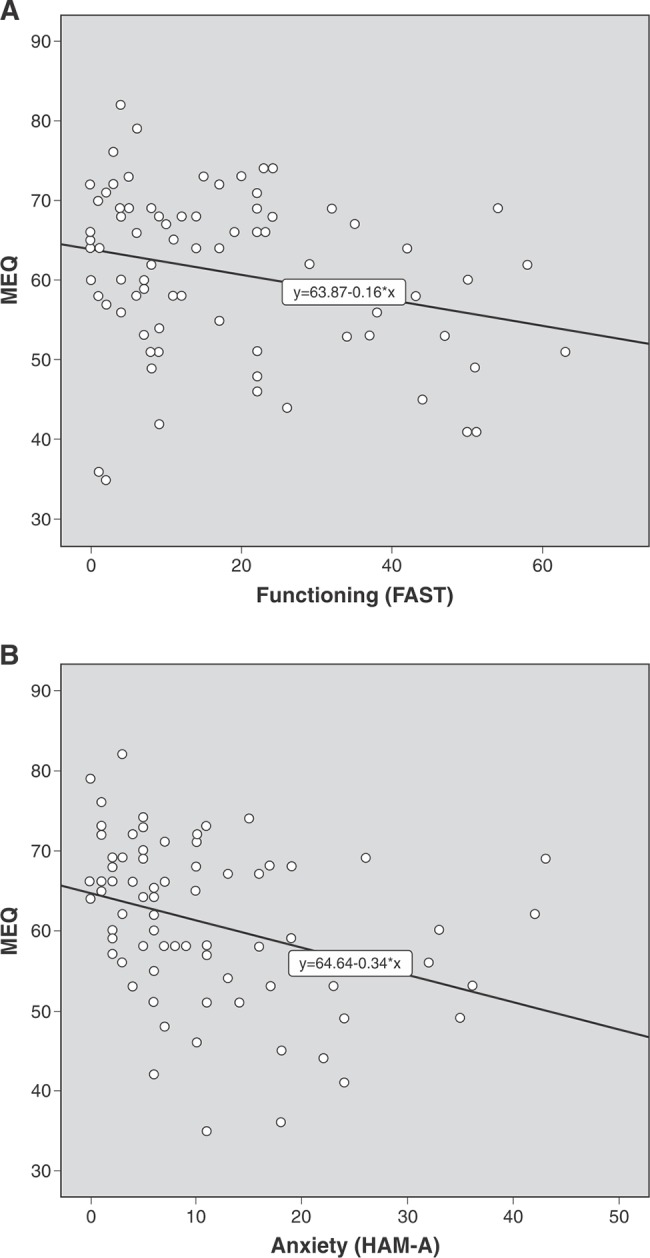
Patients with higher MEQ scores had lower levels of anxiety (nonparametric linear regression, R = 0.34, p = 0.002) and better functioning (nonparametric linear regression, R = 0.26, p = 0.01). Thus, eveningness was associated with higher anxiety and lower functioning (Figure 1).
Figure 1. Linear regression predicting anxiety levels (A) and functioning (B) according to chronotype in bipolar disorder patients. FAST = Functioning Assessment Short-Test; HAM-A = Hamilton Anxiety Rating Scale; MEQ = Morningness-Eveningness Questionnaire.
There was an evident relationship between mood episodes and eveningness (logistic regression, p = 0.04). Eveningness tended to be associated with depressive episodes (logistic regression, p = 0.06), but not (hypo)manic episodes (logistic regression, p = 0.56). There was no relationship between psychiatric hospitalizations and chronotype (logistic regression, p = 0.82) (Table 1).
Discussion
This is probably the first study to prospectively evaluate the effects of chronotype on the course of BD for 18 months. Eveningness predicted a poor prognosis for these patients in cross-sectional and longitudinal evaluation. Thus, the results of this study contribute to a broader understanding of BD and better clinical management.
Deregulation of biological rhythms is common in BD patients, even among those not taking psychoactive medications and independent of mood state.1 Previous reports have suggested that there is an association between evening chronotype, lower pineal gland volume, lower secretion of nocturnal melatonin, sleep-wake disorders, inappropriate dietary habits, poorer quality of life, greater losses in interpersonal relationships, and cognitive and behavioral dysfunction.10,11
Although the literature indicates that eveningness is common in BD,5,6 there were few such patients in the present sample. Most patients came from university outpatient clinics. Perhaps the emphasis given in medical appointments and group psychotherapy to sleep hygiene habits and sleep/wake regularity could have contributed to this fact.
In this study, eveningness was associated with increased anxiety levels, poor functioning and more mood episodes. Inflammatory processes could be a mediator of this relationship.12 A recent study with a shorter duration (48 weeks) found a relationship between circadian dysfunction and shorter intercrisis period.13 Although further research is necessary, strategies that contribute to circadian rhythm regulation may be able to improve the prognosis of BD patients.
In the present sample, evening chronotype BD patients had a higher BMI. Similarly, in the general population, evening chronotype is associated with higher BMI and inappropriate dietary behavior.14 It is possible that genetic factors, such as CLOCK 3111T/C SNP, mediate the relationship between chronotype and obesity.15 Among carriers of risk allele C, those with evening chronotype were found to have a higher mean body weight.
This study has certain limitations that should be considered. Rhythm parameters were based only on the participants’ subjective impressions, which reduces the reliability of the reported data. The use of objective instruments such as actigraphy could provide more information and reduce information bias.
Not surprisingly, eveningness was associated with other poor prognostic factors at baseline. Perhaps one or more of these factors, such as BMI or anxiety, could have influenced the results and have been predictive of future mood episodes.
A larger sample and a longer follow-up time might provide more solid conclusions. Only 80 patients were evaluated, and this sample was not representative of the Brazilian population. Some relationships had only limited statistical significance, such as the association between depressive episodes and eveningness. Despite this study’s originality and important results, 18 months is a very short time to evaluate mood episodes and their repercussions on BD.
In conclusion, according to the results of this study, evening type in BD indicates poor prognosis due to its association with greater anxiety, lower functioning and more mood episodes. These findings reinforce the relevance of researching and treating rhythm disruptions in BD patients, even during euthymia, to improve their quality of life and prevent mood episodes.
Disclosure
The authors report no conflicts of interest.
Acknowledgements
The authors would like to thank the psychiatrists who referred patients to this study and the four involved institutions.
Footnotes
How to cite this article: Melo MC, Garcia RF, Araújo CF, Luz JH, Bruin PF, Bruin VM. Chronotype in bipolar disorder: an 18-month prospective study. Braz J Psychiatry. 2020;42:68-71. http://dx.doi.org/10.1590/1516-4446-2019-0489
References
- 1.Melo MC, Abreu RL, Linhares VB, Neto, de Bruin PF, de Bruin VM. Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med Rev. 2017;34:46–58. doi: 10.1016/j.smrv.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Takaesu Y. Circadian rhythm in bipolar disorder: a review of the literature. Psychiatry Clin Neurosci. 2018;72:673–82. doi: 10.1111/pcn.12688. [DOI] [PubMed] [Google Scholar]
- 3.Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Vartiainen E, Partonen T. Circadian preference links to depression in general adult population. J Affect Disord. 2015;188:143–8. doi: 10.1016/j.jad.2015.08.061. [DOI] [PubMed] [Google Scholar]
- 4.Muller MJ, Cabanel N, Olschinski C, Jochim D, Kundermann B. Chronotypes in patients with nonseasonal depressive disorder: distribution, stability and association with clinical variables. Chronobiol Int. 2015;32:1343–51. doi: 10.3109/07420528.2015.1091353. [DOI] [PubMed] [Google Scholar]
- 5.Antypa N, Vogelzangs N, Meesters Y, Schoevers R, Penninx BW. Chronotype associations with depression and anxiety disorders in a large cohort study. Depress Anxiety. 2016;33:75–83. doi: 10.1002/da.22422. [DOI] [PubMed] [Google Scholar]
- 6.Worl Health Organization (WHO). Waist circumference and waist-hip ratio: report of a WHO expert consultation. Vol. 2011. Geneva, Switzerland: 2008 Dec 8-11. [Google Scholar]
- 7.Joshipura K, Muñoz-Torres F, Vergara J, Palacios C, Pérez CM. Neck circumference may be a better alternative to standard anthropometric measures. J Diabetes Res. 2016;2016:6058916. doi: 10.1155/2016/6058916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 9.Cacilhas AA, Magalhães PV, Ceresér KM, Walz JC, Weyne F, Rosa AR, et al. Validity of a short functioning test (FAST) in Brazilian outpatients with bipolar disorder. Value Health. 2009;12:624–7. doi: 10.1111/j.1524-4733.2008.00481.x. [DOI] [PubMed] [Google Scholar]
- 10.Ng TH, Chung KF, Lee CT, Yeung WF, Ho FY. Eveningness and its associated impairments in remitted bipolar disorder. Behav Sleep Med. 2016;14:650–64. doi: 10.1080/15402002.2015.1065407. [DOI] [PubMed] [Google Scholar]
- 11.Carpenter JS, Abelmann AC, Hatton SN, Robillard R, Hermens DF, Bennett MR, et al. Pineal volume and evening melatonin in young people with affective disorders. Brain Imaging Behav. 2017;11:1741–50. doi: 10.1007/s11682-016-9650-2. [DOI] [PubMed] [Google Scholar]
- 12.Mondin TC, de Azevedo Cardoso T, Moreira FP, Wiener C, Oses JP, de Mattos Souza LD, et al. Circadian preferences, oxidative stress and inflammatory cytokines in bipolar disorder: a community study. J Neuroimmunol. 2016;301:23–9. doi: 10.1016/j.jneuroim.2016.10.012. [DOI] [PubMed] [Google Scholar]
- 13.Takaesu Y, Inoue Y, Ono K, Murakoshi A, Futenma K, Komada Y, et al. Circadian rhythm sleep-wake disorders predict shorter time to relapse of mood episodes in euthymic patients with bipolar disorder: a prospective 48-week study. J Clin Psychiatry. 2018;79:pii: 17m11565. doi: 10.4088/JCP.17m11565. doi: https://10.4088/JCP.17m11565. [DOI] [PubMed] [Google Scholar]
- 14.Arora T, Taheri S. Associations among late chronotype, body mass index and dietary behaviors in young adolescents. Int J Obes (Lond). 2015;39:39–44. doi: 10.1038/ijo.2014.157. [DOI] [PubMed] [Google Scholar]
- 15.Ruiz-Lozano T, Vidal J, de Hollanda A, Canteras M, Garaulet M, Izquierdo-Pulido M. Evening chronotype associates with obesity in severely obese subjects: interaction with CLOCK 3111T/C. Int J Obes (Lond). 2016;40:1550–7. doi: 10.1038/ijo.2016.116. [DOI] [PubMed] [Google Scholar]


