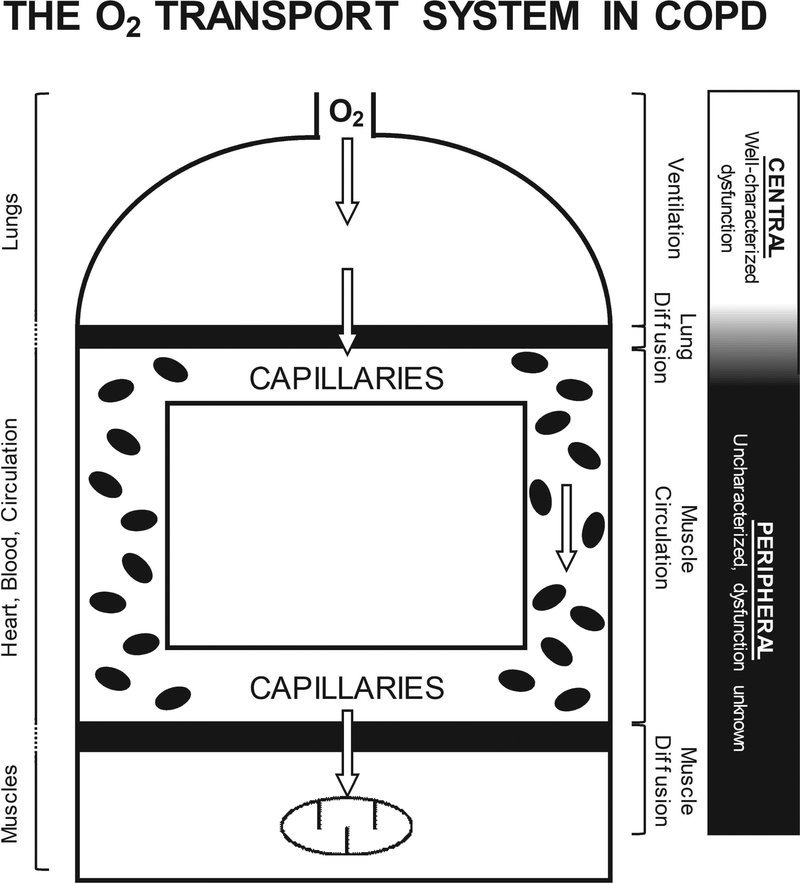
Figure 1. Schematic of the O2 transport system in COPD.
An illustration of the principal structures (lungs, heart, blood, circulation, and muscles) and associated functions (ventilation, lung diffusion, muscle circulation, and muscle diffusion) integrated in the transport of O2 from air to muscle. Patients with COPD demonstrate characterized central O2 transport dysfunction (i.e. ventilation and lung diffusion), which has been considered the primary mechanism responsible for the diminished exercise capacity in these patients. Importantly, previous studies have predominantly utilized exercise modalities that recruit a large muscle mass in the face of the marked lung dysfunction in patients with COPD (e.g. cycle ergometry), which would accentuate the influence of central O2 transport on exercise capacity, while masking peripheral dysfunction. However, peripheral O2 transport (i.e. muscle circulation and muscle diffusion) has yet to be comprehensively assessed in patients with COPD, when the central cardiopulmonary limitations to exercise capacity are minimized. Such an assessment is essential for a better understanding of the functional consequences of peripheral maladaptations with COPD and the identification of novel therapeutic targets, beyond the lungs, ultimately, facilitating the optimization of treatment and improving exercise capacity in patients with COPD.