Abstract
Background
Feline osteoarthritis (OA) is a common cause of long-standing pain and physical dysfunction. Performing a physical examination of a cat is often challenging. There is a need for disease-specific questionnaires or the so-called clinical metrology instruments (CMIs) to facilitate diagnosis and evaluation of treatment of feline OA. The CMI provides the owners an assessment of the cat’s behavioural and lifestyle changes in the home environment. The purpose of the study was to evaluate readability, internal consistency, reliability and discriminatory ability of four CMIs.
Methods
This is a prospective, cross-sectional study with 142 client-owned cats. Feline OA was diagnosed based on medical history, orthopaedic examination and radiography.
Results
The results indicate that all four instruments have sound readability, internal consistency, are reliable over time and have good discriminatory ability. Preliminary cut-off values with optimal sensitivity and specificity were suggested for each instrument. The osteoarthritic cats showed significant changes in behavioural response to pain during orthopaedic examination, compared with sound cats.
Conclusion
The results indicate that all four questionnaires make an important contribution in a clinical setting, and that the cat’s behavioural response to pain during physical examination should be a parameter to take into account as a possible indication of chronic pain.
Keywords: feline, chronic pain, clinical metrology instruments, owner assessment, pressure mat technique, sensitivity
Introduction
Feline osteoarthritis (OA) is a common disorder in older cats characterised by long-standing pain and physical dysfunction.1–6 Even though it is a common disease, OA is still underdiagnosed and undertreated in cats.7 Currently the method for diagnosing OA is based on a combination of information from the cat owner, the cat’s medical history, and findings from the physical and orthopaedic examination and radiography. The orthopaedic examination in a feline patient is often challenging. OA frequently affects bilateral joints,5 6 and few cats show single limb lameness as a clinical sign.2–4 In addition, cats undergoing examination at a veterinary clinic often have a stress response,8 9 which can make the clinical manifestations of long-standing pain difficult to recognise. This has, appropriately, led to owner involvement in the assessment process. The onset of OA-related changes in the cat’s behaviour and activities of everyday living is gradual and frequently interpreted as effects of normal ageing.1 6 10–13 Thus, clinical metrology instruments (CMIs) have been developed. CMIs are questionnaires designed to measure the sensory and affective effects of pain. CMIs have been developed for use as a diagnostic aid in clinical practice and as outcome measurements in clinical research.
Currently, there are several disease-specific CMIs available for behavioural assessment of pain in cats.14 15 The main goals of CMIs for feline OA are to determine when OA-associated pain is present (discriminatory ability) and to detect treatment-associated improvement (responsiveness validity). One of the major challenges in developing valid tools has been the strong placebo effect, as recently highlighted by Gruen et al.16 17 This makes it difficult to assess responsiveness validity, as strong responses can be seen with placebo alone. ‘The Owner Behaviour Watch’ (OBW) is a disease-specific instrument that has been used in cats with OA. It was determined that changes in behaviour occurred in each of four domains: general activity, mobility, temperament and grooming.10 This early work provided good evidence of face validity and showed that assessment of cats in the home environment is an important diagnostic aid. The results were later corroborated by Sul et al,18 although the lack of a placebo group makes interpretation of the results difficult. A study by Zamprogno et al 13 showed that behaviours relating to activity differed between musculoskeletally normal cats with no signs of pain and osteoarthritic cats. They also identified essential items or question topics, which were assembled in the so-called ‘Zamprogno Question Bank’ (ZQB). The information was later used to construct ‘The Feline Musculoskeletal Pain Index’ (FMPI), an instrument that has undergone reliability and validity testing.19–22 ‘The Feline Physical Function Formula’ (FPFF) is a recently developed CMI, based on the OBW, and focuses on physical function.23 Pain questionnaires for cats are still under development, and more information regarding their readability, internal consistency, discriminatory ability, reliability and cut-off values for diagnostic screening is needed. Therefore, the aims of the present study were the following:
To analyse the readability and internal consistency of four CMIs: FMPI, OBW, ZQB and FPFF.
To test the repeatability of each CMI by measuring test–retest reliability over time.
To evaluate the discriminatory ability of the CMIs by comparing sound and osteoarthritic cats.
To establish preliminary cut-off values for each CMI, with optimal sensitivity and specificity.
Materials and methods
Animals
Cats were recruited from patient databases at local animal hospitals (Skara and Uppsala, Sweden). The search in the database was based on the diagnosis ‘osteoarthritis’ in appendicular joints or orthopaedic conditions in the appendicular locomotor apparatus. They were also referred from primary care veterinarians, or self-referred from students, staff and the general public. All the participating cats were client-owned cats. Kinetic data were collected using a pressure-sensitive mat technique. These data are not presented in this paper.
Inclusion and exclusion criteria
Cats between one year and 14 years old, of either sex, or any breed other than Scottish fold were recruited. The Scottish fold breed was excluded due to osteochondrodysplasia, an inheritable disease which affects the synovial joints. Cats were excluded if they had concomitant disease other than OA, or a temperament that rendered them difficult to handle. Cats that were on any treatment for OA or other disease with either a registered pharmaceutical, nutraceutical or a therapeutic diet with alleged effect on OA were also excluded.
Overall study outline
The study was designed as a prospective, cross-sectional clinical study. Potential study subjects were screened using information from the cat owner, the cat’s medical history, and findings from physical and orthopaedic examination (table 1), and in some cases blood sampling and radiography. Cats were designated as osteoarthritic based on positive findings from the orthopaedic examination and radiography. The radiographic criteria used were marginal or periarticular osteophytes, subchondral bone sclerosis, subchondral bone lysis and cyst-like lesions, articular mineralisations, increased volume of the soft tissue opacity structures of the joint, and remodelling of joint shape.5 24–26
Table 1.
Contribution of the cat’s medical history, orthopaedic examination and radiography to the overall diagnosis as osteoarthritic, uncertain diagnosis or sound
| Screening of potential study objects | Overall diagnosis | ||
| Medical history | Orthopaedic examination | Radiography | |
| Osteoarthritis | Osteoarthritis | Osteoarthritis | Osteoarthritis |
| Normal/Uncertain | Osteoarthritis | Osteoarthritis | Osteoarthritis |
| Osteoarthritis | Osteoarthritis | Uncertain | Uncertain |
| Osteoarthritis | Sound | Not radiographed | Sound |
| Sound | Sound | Not radiographed | Sound |
Physical and orthopaedic examination
Each cat underwent a physical examination, performed by the same veterinarian (SS), who also evaluated the cat’s body condition score (BCS) according to a 9-point system.27 28 The examination included the axial and appendicular skeleton, as well as evaluation of muscle symmetry. Appendicular joints were evaluated regarding periarticular thickening, joint effusion, crepitation and range of motion (graded from 0=no clinical signs to 3=severe findings). Pain reactions during the evaluation of the axial and appendicular skeleton were graded according to Zamprogno et al.13 The pain response for each joint was graded as follows: 0=no resentment; 1=mild withdrawal, mild resistance to manipulation; 2=moderate withdrawal, body tenses, may orient to site, may vocalise or increase vocalisation; 3=orients to site, forcible withdrawal from manipulation, may vocalise, hiss or bite; and 4=tries to escape or prevent manipulation, bites or hisses, marked guarding of site. The total score a joint could get at the orthopaedic examination was 16 points. As an additional scoring, the highest pain response that was elicited in a single joint during the orthopaedic examination was given as an overall grading of behavioural response to pain in each cat.
Blood sample and radiography
After the physical examination was concluded, a blood sample was collected according to the flow chart in figure 1. (The 58 cats that contributed data from a previous study29 were not blood-sampled.) Cats that had creatinine, blood urea nitrogen, alanine aminotransferase, alkaline phosphatase, albumin and haemoglobin values within the normal reference range were sedated and underwent radiographic examination. Cats that did not have blood values within the normal reference range did not undergo radiography. Cats were sedated with a combination of medetomidine (50 µg/kg; Sedator vet, 1 mg/ml; Dechra Veterinary Products) and butorphanol (0.4 mg/kg; Dolorex vet, 10 mg/ml; Intervet). The appendicular joints that were found to be affected on the orthopaedic examination were radiographed. The radiographs were assessed by a board-certified radiologist. Sedation was reversed with atipamezole (125 µg/kg; Atipam vet, 5 mg/ml; Dechra Veterinary Products). Cats that had no indicators of osteoarthritic disease in their medical history or orthopaedic examination were enrolled as normal controls and were not radiographed. The cats that were diagnosed with OA were required to have findings on both the orthopaedic examination and radiography supporting the diagnosis. The ones that did not have positive findings on radiographs yet have positive findings on orthopaedic examination were deemed as uncertain (table 1).
Figure 1.
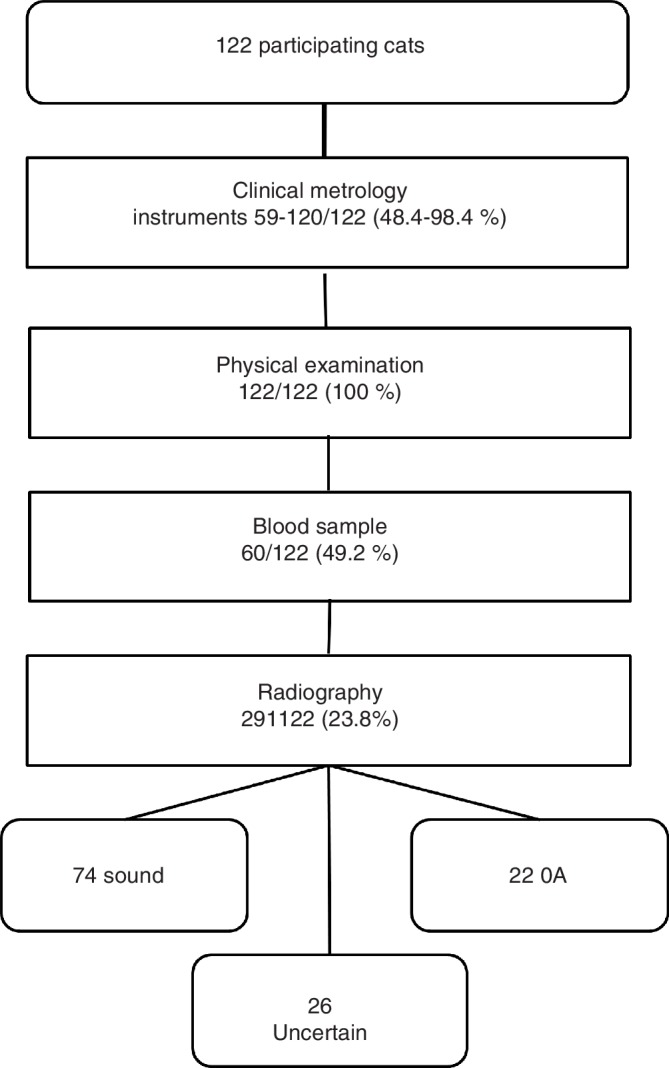
Flow chart describing the chronological order of examinations and the number of cats subjected to each examination. OA, osteoarthritis.
Clinical metrology instruments
Four CMIs, available at the time and suitable for feline degenerative joint disease, were evaluated in the present study. ‘The Owner Behaviour Watch’ consists of four questions regarding the domains general activity, mobility, temperament and grooming, and one comprehensive question regarding the cat’s overall ability to perform certain tasks. The owner is asked to rate the cat’s change in ability, compared with a normal cat, from 0 to 10 for each question. A score of 0 indicates a normal ability and 50 is the maximum total score.10 18 ‘The Feline Musculoskeletal Pain Index’ consists of 17 specific questions where the owner rates the cat’s ability to perform various tasks on a Likert scale.30 It also contains three comprehensive questions regarding the cat’s level of pain and general quality of life. Each question is scored from −1 to 4 and the total maximum score is 80.19–22 The original set of questions was used by Zamprogno et al.13 ‘The Zamprogno Question bank’, consisting of 18 questions, was also evaluated. The answers were scored on a Likert scale from 0 to 4, with a total maximum score of 72. The design of ‘The Feline Physical Function Formula’ was based on the OBW instrument. It consists of 16 questions, requiring binary answers, with a total maximum score of 12.23 For further details, see the individual publications.
The notes on how to fill out the FMPI was presented to the cat owner with the concomitant questionnaire. The questionnaires (FPFF, OBW and ZQB) were presented in a randomised order. The CMIs that were originally published in English (all but the FPFF) were translated from English to Swedish and back-translated by an official translation company. The forward and backward translations were made by different translators with experience of medical terms. The final versions were then reviewed by a third independent official translator that made a statement regarding the consistency of the translation. The owners filled out the CMIs in the same quiet room as the physical examination was performed. The owners were instructed verbally on how to complete each questionnaire and then presented with paper copies of the CMIs. The owners had access to qualified staff at all times that could answer any questions regarding the CMIs. Paper copies of the CMIs were later posted in prepaid envelopes to the cat owners, 1–39 months after the first occasion, to test reliability. The owners did not have access to the previously filled in questionnaires. The same owners who previously filled in the questionnaires were asked to fill out the CMIs again provided that the cat’s state of health or disease had not changed. CMIs’ ease of use was assessed by the number of CMIs that were filled out in the correct way the first time the cat owners were presented with them.
Data processing and statistical analysis
All data were entered into a database (Microsoft Excel), and all statistical analyses were done using R V.3.4.1.31 Statistical comparison between the three groups of cats regarding the descriptive parameters was made using Kruskal-Wallis and Fisher’s exact test. Pearson’s correlation coefficient was calculated to describe the reliability between the test results over time. Analysis of variance test of the difference between the overall diagnosis for each cat and the total score on the CMI was done to estimate the instrument’s discriminatory ability, for example, to estimate to what degree related questions score equally but still contribute unique information to the total score of the instrument. Receiver operating characteristic (ROC) curves were plotted, as sensitivity versus 1-specificity, in order to calculate the AUC.32 The ROC curve illustrates the diagnostic accuracy of the test, and the AUC illustrates how well a test parameter can distinguish between sound and OA cats. Cronbach’s α was analysed as a measurement of the instrument’s internal consistency. Data are presented as mean±sd.
Results
Animals
One hundred and forty-two client-owned cats were recruited. Of these, 56 were sound cats from a previous data set,29 contributing information regarding CMIs, and physical and orthopaedic examination. Out of the other 86 cats, 20 cats were excluded based on the results from orthopaedic examination (seven cats due to luxated coxofemoral joint, three cats due to neurological disease, one cat due to congenital malformation of the spinal column, three cats due to treatment with nutraceuticals or therapeutic diets, and six cats due to insufficient cooperative abilities). Six cats of the 66 were not blood-sampled due to insufficient cooperative ability. They still contributed data from the CMIs and physical and orthopaedic examination.
Twelve (20.0 per cent) of the remaining 60 cats that were blood-sampled had creatinine values exceeding the upper limit of the reference range for normal cats (70–160 μmol/l) and were therefore excluded from the study. Nineteen cats were not radiographed because they either lacked findings on the orthopaedic examination or had other blood values outside the reference range. Twenty-nine cats had positive findings on the orthopaedic examination, presenting 93 of 464 (20.0 per cent) joints with abnormal findings on physical examination. These 29 cats were radiographed, and one cat was deemed radiographically normal and six assessed as having uncertain findings on radiography. Twelve of the 29 (41.4 per cent) radiographed cats had visually apparent gait abnormalities. The present study included a total of 122 cats, divided into 74 sound, 26 with uncertain diagnosis and 22 with OA.
Data from 122 cats were analysed; 83 (68.0 per cent) of these cats were domestic shorthaired or longhaired and 39 (32.0 per cent) cats were purebred. Eleven different breeds were represented among the purebred cats. Fifty-four (44.3 per cent) of the 122 cats were female and 68 (55.7 per cent) were male. Of the participating 122 cats, eight (6.6 per cent) were entire and the rest were neutered. The mean age was 6.8±3.6 years. The mean weight of the cats was 5.2±0.9 kg. The cats had a mean BCS of 6.2±1.4 on a 9-point scale. Fifty-seven (46.7 per cent) of the participating cats had an indoor lifestyle only, and 65 (53.3 per cent) cats spent their time both indoor and outdoor. There was no statistical difference between the groups regarding the variables male/female, spayed/neutered, or indoors only or indoor and outdoor lifestyle. There was a significant difference in the variables age and weight between the groups sound, uncertain and OA, respectively (table 2). Results from the orthopaedic examination showed a significant difference in the behavioural response to pain between the three groups, respectively (table 3).
Table 2.
Median and mean±sd for weight and age of the three groups of cats and statistical comparisons
| Sound | Uncertain | Osteoarthritis | P value* | ||||
| Mean±sd | Median | Mean±sd | Median | Mean±sd | Median | ||
| Age (years) | 5.0±2.8 | 4.0 | 9.0±3.0 | 9.5 | 10.0±2.4 | 10.0 | 0.0004 |
| Weight (kg) | 4.7±1.3 | 4.8 | 6.0±2.1 | 5.5 | 6.0±2.0 | 5.6 | 0.002 |
*Kruskal-Wallis comparison based on median values, between sound cats, cats with uncertain diagnosis and cats with osteoarthritis, respectively.
Table 3.
Fisher’s comparison of demographic parameters for the three diagnostic groups
| Variable | Sound | Uncertain | OA | Comparison |
| Proportion | Proportion | Proportion | P value | |
| Male | 0.570 | 0.460 | 0.640 | 0.470 |
| Female | 0.430 | 0.540 | 0.360 | 0.470 |
| Spayed or neutered | 0.910 | 0.960 | 1.000 | 0.470 |
| Indoors* | 0.470 | 0.500 | 0.450 | 0.940 |
| Outdoors† | 0.530 | 0.500 | 0.550 | 0.9400 |
| Behavioural response to pain 0 | 0.950 | 0.420 | 0.450 | 0.0005 |
| Behavioural response to pain 1 | 0.027 | 0.120 | 0.410 | 0.0005 |
| Behavioural response to pain 2 | 0 | 0.270 | 0.091 | 0.0005 |
| Behavioural response to pain 3 | 0.014 | 0.077 | 0 | 0.0005 |
| Behavioural response to pain 4 | 0.014 | 0.120 | 0.045 | 0.0005 |
| Variable | Sound mean ± sd | Uncertain mean ± sd | OA mean ± sd | Comparison P value |
| Orthopaedic examination | 0±0 | 9.1±10.0 | 14.1±6.9 | 0.0005 |
Behavioural response to pain (0–4) was significantly different between the three groups (P=0.0005). Student’s t test comparison between sound and OA as well as sound and uncertain cats for orthopaedic examination scores (maximum score 16 points/joint for 19 joints).
*Indoors only.
†Combined indoors and outdoors.
OA, osteoarthritis.
Readability and internal consistency of the CMIs
The number of cat owners, for each cat’s diagnostic category, that filled out each CMI on the first test occasion is presented in table 4. The FMPI, FPFF and ZQB instruments were filled out correctly in more than 97.8 per cent of the cases. The OBW instrument by Bennett and Morton10 was filled out correctly by 51 of 88 (58.0 per cent) cat owners. In the cases where the cat owners did not fill out the last question correctly in this CMI, the CMI was analysed without this question. The four CMIs had values of Cronbach’s α in the range of 0.80–0.91 (table 5). Cronbach’s α in the range of 0.70–0.95 is generally considered to have an acceptable reliability.30
Table 4.
Number of cat owners, for each cat’s diagnostic category, that filled out each CMI on the first test occasion
| Category | FMPI | OBW | ZQB | FPFF |
| Sound | 23 | 46 | 48 | 73 |
| Uncertain | 18 | 21 | 22 | 26 |
| OA | 18 | 21 | 21 | 21 |
| Total number of cats | 59 | 88 | 91 | 120 |
CMI, clinical metrology instrument; FMPI, Feline Musculoskeletal Pain Index; FPFF, Feline Physical Function Formula; OA, osteoarthritis; OBW, Owner Behaviour Watch; ZQB, Zamprogno Question Bank.
Table 5.
Number of cat owners that answered the four CMIs on the first and second test occasions
| CMI | Test occasion 1 | Test occasion 2 | Response rate (%) | Pearson’s correlation coefficient |
| FMPI | 59 | 22 | 37.3 | 0.72 |
| OBW | 88 | 37 | 42.0 | 0.72 |
| ZQB | 91 | 45 | 49.5 | 0.73 |
| FPFF | 120 | 67 | 55.8 | 0.66 |
Pearson’s correlation coefficient guidelines for interpretation: 0–0.3, weak positive linear relationship; 0.3–0.7, moderate positive linear relationship; 0.7–1.0, strong positive linear relationship.31
CMI, clinical metrology instrument; FMPI, Feline Musculoskeletal Pain Index; FPFF, Feline Physical Function Formula; OBW, Owner Behaviour Watch; ZQB, Zamprogno Question Bank.
Repeatability of the CMIs
Of the 122 cat owners, four of the responding owners’ answers were excluded on the second test occasion due to the cat’s treatment with nutraceuticals or therapeutic diets being initiated after the first time the owner filled out the CMI. The response rate varied from 37.3 per cent to 55.8 per cent for the various CMIs (table 5). The time between the first and the second test occasions was on average 546 (±781) days. Pearson’s correlation showed a strong positive linear relationship for three of the CMIs, except for FPFF for which the correlation was moderately strong.
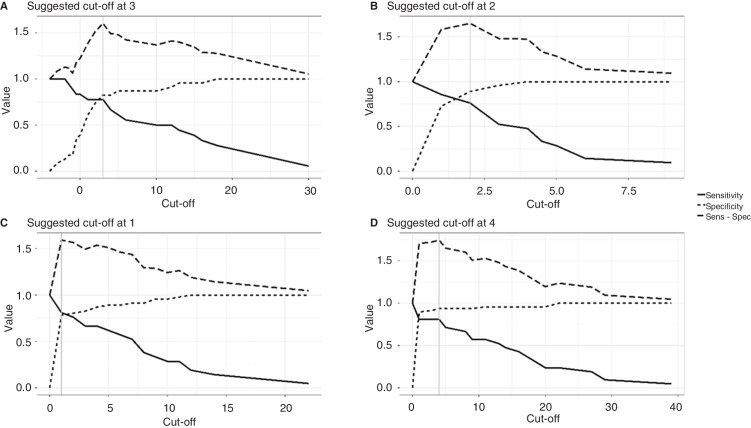
Discriminatory ability, cut-off values, and optimal sensitivity and specificity of the CMIs
The diagnostic accuracy estimated with AUC ranged from 0.79 to 0.87, which is considered good (table 6, figure 2).
Table 6.
Parameters illustrating test performance of the four CMIs
| CMI analysis | ANOVA P value | AUC | Cut-off | Cronbach’s α |
| FMPI (n=59) | 0.00014 | 0.79 | 3 | 0.91 |
| OBW (n=88) | 1.2 x 10−6 | 0.82 | 1 | 0.88 |
| ZQB (n=91) | 8.2 x 10−8 | 0.87 | 4 | 0.91 |
| FPFF (n=120) | 1.9 x 10−12 | 0.87 | 2 | 0.80 |
Cut-off is based on total score.
ANOVA, analysis of variance; CMIs, clinical metrology instruments; FMPI, Feline Musculoskeletal Pain Index; FPFF, Feline Physical Function Formula; OBW, Owner Behaviour Watch; ZQB, Zamprogno Question Bank.
Figure 2.
Cut-off values, sensitivity and specificity graphically illustrated for the four clinical metrology instruments. The x axis shows the instrument’s total maximum score, while the y axis shows the index value for sensitivity and specificity: (a) Feline Musculoskeletal Pain Index cut-off value=3 (−4 to 80); (b) Feline Physical Function Formula (FPFF) cut-off value=2 (0–12); (c) Owner Behaviour Watch (OBW) cut-off value=1 (0–50); and (d) Zamprogno Question Bank (ZQB) cut-off value=4 (0–72).
Discussion
The results indicate that all four instruments are reliable over time, have a sound discriminatory ability and an internal consistency with acceptable reliability. Cut-off values for each instrument are also suggested. The sample of cats is likely to be representative of the larger population, with the minority of the cats being purebred. The results from comparing the different diagnostic groups of cats revealed significant differences in age, weight and behavioural response to pain. OA cats tended to be older, heavier and more reactive to pain provocations. The latter could indicate a poorer state of mood compared with sound cats. This has been described in previous publications.5 33
The selected criteria for classifying the cats as having OA (medical history, orthopaedic examination and radiography) are the ones recommended by the veterinary community. However, it is likely that the diagnostic criteria will change in the future. Human research clearly indicates that plain radiographs have limited ability to detect osteoarthritic features at an early stage of disease and that their usefulness relates to simply confirming the suspected disease (OA) and excluding other diseases.34 Further, the correlation between clinical signs of OA and radiographic signs OA in cats is weak.1 33 Therefore it is utterly important to find other criteria for diagnosing OA in cats, such as owner-completed questionnaires.
Analysis of the instruments’ readability revealed that the OBW instrument had less than optimal readability. The design of the questionnaire is known to be crucial, and affects understanding of the questions, scoring of individual questions and the overall score.35–38 This is particularly important for owners completing the questionnaire in a busy clinical setting. Measurement of internal consistency with Cronbach’s α showed that all four instruments had acceptable consistency. The FPFF scored the lowest level, and refinement of some questions is advised.
Analysis of repeatability of the four CMIs by measuring test–retest reliability over time revealed a strong linear relationship for three of the four instruments, and the FPFF had a moderately strong relationship. This indicates that the instruments are reliable over time. One must bear in mind that the fairly extended time between the first and the second test occasions when the cat owners filled out the instrument caused a number of dropouts and could potentially bias the results and the cat’s health status may have changed. On the second test occasion the cat owner was sent a paper copy of the CMIs and the cat was not physically examined. However, owners were asked whether the cat’s status of health or disease had changed, and only results where this was unaltered were used.
The discriminatory ability of the four instruments was determined by comparing the total score on the CMI across diagnosis categories. In all cases, the total score of the instrument was significantly different between sound and osteoarthritic cats. Analysis of the AUC indicated that the diagnostic accuracy of the four instruments is acceptable to excellent. It is important to note that there is no gold standard for the diagnosis of OA pain in cats, and so categorisation was based on clinical judgement made up of a combination of history, veterinary clinical examination and radiography. The study’s results support the use of these instruments in making a diagnosis of OA pain in the cat.
The authors have proposed preliminary cut-off values for each CMI with the greatest sensitivity, providing the least false negatives, and the greatest specificity, providing the least false positives. Given the high prevalence of feline OA, combined with the fact that disease has a slow progression and low mortality, decreased sensitivity will lead to prolonged time until diagnosis in most cases, with the cat suffering from chronic pain in the mean time. The authors propose that the CMIs can be used as a screening diagnostic test, and cats testing ‘positive’ can be subjected to further diagnostic tests to confirm or refute the results of the CMI. The cut-off values indicate that individuals scoring 0 are likely not suffering from OA and individuals scoring higher on the test should be investigated further. The suggested cut-off values will make a valuable contribution to using the instruments in clinical practice.
The fairly large group of cats diagnosed as ‘uncertain’ did not differ from the group with OA cats regarding age and weight. The main reason for cats being placed in this group was that they did not have radiographic findings indicating OA. A limitation of the present study is that not all of the osteoarthritic cats and none of the sound cats were radiographed due to practical and ethical concerns. For this reason, most emphasis was placed on the physical examination findings. Notable is the significant difference in the behaviour traits insofar as the osteoarthritic cats had a more reactive response to painful provocations—possibly a poorer state of mood due to the experience of long-standing pain. Lascelles et al 33 showed that cats with higher pain scores due to OA were less friendly than cats with lower pain scores. Kranenburg et al 39 revealed similar results in cats with Spondylosis deformans, where cats with more severe findings had more aggressive behaviour.39 In a recent publication on feline personality, it was also suggested that cats scoring low on agreeableness could be suffering from underlying pain.40 The association between chronic pain and mood or depression has long been known in human medicine.41–43
In conclusion, the authors believe that the four CMIs tested can make a valuable contribution to diagnosing OA in the everyday clinical setting. In addition, these CMIs may serve as any important tool in educating the cat owner on what signs to look for. The FMPI is the instrument that has gone through the most extensive validity and reliability testing. In this study the FMPI performed well and combined with an agreeable layout is the instrument the authors recommend for use in a clinical setting. A valid and reliable method for assessing feline state of mood as an outcome measure of chronic pain needs to be further investigated.
Acknowledgments
The authors would like to thank all the cat owners who contributed to this study. Thanks to Henrik Renlund at Uppsala Clinical Research Center for statistical processing of the collected data, Dr Cecilia Ley for laboratory work and fruitful discussions, and Dr Charles Ley for radiographic expertise.
Footnotes
Funding: Agria Pet Insurance provided funding for part of the study.
Competing interests: None declared.
Ethics approval: The study was approved by the local Ethical Review Board on Animal Experiments (no C23/15). Each cat owner signed an informed client consent form following verbal and written information before inclusion.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon request.
References
- 1. Clarke SP, Bennett D. Feline osteoarthritis: a prospective study of 28 cases. J Small Anim Pract 2006;47:439–45. 10.1111/j.1748-5827.2006.00143.x [DOI] [PubMed] [Google Scholar]
- 2. Clarke SP, Mellor D, Clements DN, et al. Prevalence of radiographic signs of degenerative joint disease in a hospital population of cats. Vet Rec 2005;157:793–9. 10.1136/vr.157.25.793 [DOI] [PubMed] [Google Scholar]
- 3. Godfrey DR. Osteoarthritis in cats: a retrospective radiological study. J Small Anim Pract 2005;46:425–9. 10.1111/j.1748-5827.2005.tb00340.x [DOI] [PubMed] [Google Scholar]
- 4. Hardie EM, Roe SC, Martin FR. Radiographic evidence of degenerative joint disease in geriatric cats: 100 cases (1994-1997). J Am Vet Med Assoc 2002;220:628–32. 10.2460/javma.2002.220.628 [DOI] [PubMed] [Google Scholar]
- 5. Lascelles BDX, Henry JB, Brown J, et al. Cross-Sectional study of the prevalence of radiographic degenerative joint disease in domesticated cats. Vet Surg 2010;39:535–44. 10.1111/j.1532-950X.2010.00708.x [DOI] [PubMed] [Google Scholar]
- 6. Slingerland LI, Hazewinkel HAW, Meij BP, et al. Cross-Sectional study of the prevalence and clinical features of osteoarthritis in 100 cats. Vet J 2011;187:304–9. 10.1016/j.tvjl.2009.12.014 [DOI] [PubMed] [Google Scholar]
- 7. Bennett D, Zainal Ariffin SMbt, Johnston P. Osteoarthritis in the cat: 1. how common is it and how easy to recognise? J Feline Med Surg 2012;14:65–75. 10.1177/1098612X11432828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Quimby JM, Smith ML, Lunn KF. Evaluation of the effects of hospital visit stress on physiologic parameters in the cat. J Feline Med Surg 2011;13:733–7. 10.1016/j.jfms.2011.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Belew AM, Barlett T, Brown SA. Evaluation of the white-coat effect in cats. J Vet Intern Med 1999;13:134–42. 10.1111/j.1939-1676.1999.tb01141.x [DOI] [PubMed] [Google Scholar]
- 10. Bennett D, Morton C. A study of owner observed behavioural and lifestyle changes in cats with musculoskeletal disease before and after analgesic therapy. J Feline Med Surg 2009;11:997–1004. 10.1016/j.jfms.2009.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Klinck MP, Frank D, Guillot M, et al. Owner-perceived signs and veterinary diagnosis in 50 cases of feline osteoarthritis. Can Vet J 2012;53:1181–6. [PMC free article] [PubMed] [Google Scholar]
- 12. Lascelles BDX, Hansen BD, Roe S, et al. Evaluation of client-specific outcome measures and activity monitoring to measure pain relief in cats with osteoarthritis. J Vet Intern Med 2007;21:410–6. 10.1111/j.1939-1676.2007.tb02983.x [DOI] [PubMed] [Google Scholar]
- 13. Zamprogno H, Hansen BD, Bondell HD, et al. Item generation and design testing of a questionnaire to assess degenerative joint disease-associated pain in cats. Am J Vet Res 2010;71:1417–24. 10.2460/ajvr.71.12.1417 [DOI] [PubMed] [Google Scholar]
- 14. Merola I, Mills DS. Behavioural signs of pain in cats: an expert consensus. PLoS One 2016;11:e0150040 10.1371/journal.pone.0150040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Merola I, Mills DS. Systematic review of the behavioural assessment of pain in cats. J Feline Med Surg 2016;18:60–76. 10.1177/1098612X15578725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gruen ME, Dorman DC, Lascelles BDX. Caregiver placebo effect in analgesic clinical trials for cats with naturally occurring degenerative joint disease-associated pain. Vet Rec 2017;180 10.1136/vr.104168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gruen ME, Alfaro-Córdoba M, Thomson AE, et al. The use of functional data analysis to evaluate activity in a spontaneous model of degenerative joint disease associated pain in cats. PLoS One 2017;12:e0169576 10.1371/journal.pone.0169576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sul RM, Chase D, Parkin T, et al. Comparison of meloxicam and a glucosamine-chondroitin supplement in management of feline osteoarthritis. A double-blind randomised, placebo-controlled, prospective trial. Vet Comp Orthop Traumatol 2014;27:20–6. 10.3415/VCOT-12-11-0139 [DOI] [PubMed] [Google Scholar]
- 19. Benito J, Depuy V, Hardie E, et al. Reliability and discriminatory testing of a client-based metrology instrument, feline musculoskeletal pain index (FMPI) for the evaluation of degenerative joint disease-associated pain in cats. Vet J 2013;196:368–73. 10.1016/j.tvjl.2012.12.015 [DOI] [PubMed] [Google Scholar]
- 20. Benito J, Hansen B, Depuy V, et al. Feline musculoskeletal pain index: responsiveness and testing of criterion validity. J Vet Intern Med 2013;27:474–82. 10.1111/jvim.12077 [DOI] [PubMed] [Google Scholar]
- 21. Gruen ME, Griffith E, Thomson A, et al. Detection of clinically relevant pain relief in cats with degenerative joint disease associated pain. J Vet Intern Med 2014;28:346–50. 10.1111/jvim.12312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gruen ME, Griffith EH, Thomson AE, et al. Criterion validation testing of clinical Metrology instruments for measuring degenerative joint disease associated mobility impairment in cats. PLoS One 2015;10:e0131839 10.1371/journal.pone.0131839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stadig S, Bergh A. The feline physical function formula. 2011.
- 24. Freire M, Robertson I, Bondell HD, et al. Radiographic evaluation of feline appendicular degenerative joint disease vs. macroscopic appearance of articular cartilage. Vet Radiol Ultrasound 2011;52:239–47. 10.1111/j.1740-8261.2011.01803.x [DOI] [PubMed] [Google Scholar]
- 25. Leijon A, Ley CJ, Corin A, et al. Cartilage lesions in feline stifle joints - associations with articular mineralizations and implications for osteoarthritis. Res Vet Sci 2017;114:186–93. 10.1016/j.rvsc.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 26. Voss K, Karli P, Montavon PM, et al. Association of mineralisations in the stifle joint of domestic cats with degenerative joint disease and cranial cruciate ligament pathology. J Feline Med Surg 2017;19:27–35. 10.1177/1098612X15606774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. German A, Martin L. Chapter 1: Feline obesity : Encyclopedia of feline clinical nutrition. Aimargues, France: Royal Canin, 2008. [Google Scholar]
- 28. Laflamme D. Development and validation of a body condition score system for cats: a clinical tool. Feline Pract 1997;25:13–18. [Google Scholar]
- 29. Stadig SM, Bergh AK. Gait and jump analysis in healthy cats using a pressure mat system. J Feline Med Surg 2015;17:523–9. 10.1177/1098612X14551588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Likert RA. A technique for the development of attitude scales. Educ and Psych Measurement 1952;12. [Google Scholar]
- 31. R Core Team R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2013. [Google Scholar]
- 32. Lasko TA, Bhagwat JG, Zou KH, et al. The use of receiver operating characteristic curves in biomedical informatics. J Biomed Inform 2005;38:404–15. 10.1016/j.jbi.2005.02.008 [DOI] [PubMed] [Google Scholar]
- 33. Lascelles BDX, Dong Y-H, Marcellin-Little DJ, et al. Relationship of orthopedic examination, goniometric measurements, and radiographic signs of degenerative joint disease in cats. BMC Vet Res 2012;8:10 10.1186/1746-6148-8-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kim C, Nevitt MC, Niu J, et al. Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. BMJ 2015;351 10.1136/bmj.h5983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Choi BCK, Pak AWP. A catalog of biases in questionnaires. Prev Chronic Dis 2005;2:A13. [PMC free article] [PubMed] [Google Scholar]
- 36. Rattray J, Jones MC. Essential elements of questionnaire design and development. J Clin Nurs 2007;16:234–43. 10.1111/j.1365-2702.2006.01573.x [DOI] [PubMed] [Google Scholar]
- 37. von Baeyer CL. Children's self-reports of pain intensity: scale selection, limitations and interpretation. Pain Res Manag 2006;11:157–62. 10.1155/2006/197616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. New York: Oxford University Press, 1989. [Google Scholar]
- 39. Kranenburg HC, Meij BP, van Hofwegen EML, et al. Prevalence of spondylosis deformans in the feline spine and correlation with owner-perceived behavioural changes. Vet Comp Orthop Traumatol 2012;25:217–23. 10.3415/VCOT-11-06-0092 [DOI] [PubMed] [Google Scholar]
- 40. Litchfield CA, Quinton G, Tindle H, et al. The ‘Feline Five’: An exploration of personality in pet cats (Felis catus). PLoS One 2017;12:e0183455 10.1371/journal.pone.0183455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Affleck G, Tennen H, Keefe FJ, et al. Everyday life with osteoarthritis or rheumatoid arthritis: independent effects of disease and gender on daily pain, mood, and coping. Pain 1999;83:601–9. 10.1016/S0304-3959(99)00167-0 [DOI] [PubMed] [Google Scholar]
- 42. Burke ALJ, Mathias JL, Denson LA. Psychological functioning of people living with chronic pain: a meta-analytic review. Br J Clin Psychol 2015;54:345–60. 10.1111/bjc.12078 [DOI] [PubMed] [Google Scholar]
- 43. Shim E-J, Hahm B-J, Go DJ, et al. Modeling quality of life in patients with rheumatic diseases: the role of pain catastrophizing, fear-avoidance beliefs, physical disability, and depression. Disabil Rehabil 2018;40:1509–16. 10.1080/09638288.2017.1300691 [DOI] [PubMed] [Google Scholar]