Abstract
Purpose
Medical schools look for ways to provide clinical experiences and skill development in connection with knowledge. One method used is to provide emergency medical technician (EMT) training to medical students; however, limited data are available concerning EMT training in medical education. Therefore, the aim of this study was to review student feedback about the EMT curriculum through multiple iterations of the curriculum.
Methods
Students completed a voluntary school administered survey upon completion of their first year of medical school. Student responses to statements related to the EMT course and program were analyzed for classes matriculating in academic years 2012–2017. A one-way ANOVA with post hoc Tukey Honestly Significant Difference (HSD) was performed across all years for each survey statement.
Results
Mean response scores to statements related to the EMT course were higher when the EMT course was a standalone course and lower when integrated with biomedical science coursework. Students “strongly agreed” or “agreed” with most statements related to experiences and clinical skill development provided by the EMT program. Response rates ranged between 46–52 (88–100%) for 2012, 40–46 (74–85%) for 2013, 72–79 (88–96%) for 2014, 73–86 (71–83%) for 2015, 47–65 (46–63%) for 2016, 62–82 (59–78%) for 2017.
Conclusion
Our data show that first year medical students liked the course design best when the EMT course was a standalone course at the start of the M.D. program while students liked experiences and clinical skill development provided by the EMT program regardless of course design.
Keywords: emergency medical technician, medical curriculum, student perspectives, curriculum design
Introduction
Medical schools continually examine methods, pedagogy, and curriculum to better connect knowledge to clinical experiences and skill performance. Recent recommendations to achieve this were described by Cooke et al.1 One idea used by United States medical schools during the 1970s and 1980s was offering emergency medical technician (EMT) training as this was a relatively new specialty recognized by the Department of Labor.2–4 Since these initial reports, continuation or expansion of medical school EMT training has been limited. Recently, however, two new expansion schools adopted this into the preclinical years of their curriculum.5,6
The University of South Carolina (UofSC) School of Medicine Greenville matriculated its Charter Class in 2012 with the vision of teaching clinical medicine along with biomedical sciences content throughout the preclinical years. To augment the traditional methods of teaching history-taking and physical skill performance, an EMT course was included at the beginning of the first year prior to the start of the biomedical sciences. This curriculum map was similar to that used at Hofstra North Shore, Long Island Jewish School of Medicine, also one of the new expansion schools.6 Different from Hofstra, UofSC School of Medicine Greenville students are required to pass the National Registry for EMTs (NREMT) examination, maintain a State EMT certification, and must complete one twelve-hour shift on an ambulance 4 times in the second semester of the first year and 6 times during the second year. This additional experience was a method to increase the exposure to clinical medicine and particular aspects of population health. The hours, content, and assessment required for EMT training are regulated by the State, so minimum guidelines had to be followed; however, additional hours, content, and assessment could be added as program outcomes dictated.
Tangible benefits of EMT training not only supports an early exposure to clinical knowledge and community-based experiences, but also provides a less stressful indoctrination to medical school, promotes teamwork and effective communication strategies with diverse ages and cultures, and introduces students to social determinants of health and the communities where their future patients may emanate.6,7 Kwiatkowski et al found that EMT training increases students’ confidence levels in areas such as delivering patient care, employing team-building skills, and applying deductive reasoning into their patient interaction6 which is important to increase confidence levels when employing learned skills.8 Another study reported that students who were required to complete reflections about any aspect of medical school encountered frequently wrote about their EMT experiences which included the competencies of patient care, professionalism, systems-based practice, and communication and interpersonal skills.7 While these reports provide valuable insight from two student cohorts regarding perceptions of EMT training, longitudinal feedback may be more valuable for medical schools considering such a program. This study is a report of 6 years of student perceptions of an EMT course and program and the differences noted when curricular modifications were instituted.
Materials and Methods
First year medical students at UofSC School of Medicine Greenville complete an EMT course during their first semester of medical school. Upon completion of the course, students must successfully pass the NREMT exam to become State certified and complete one 12 hr EMT shift 4 times in the second semester of the first year and 6 times during the second year. The EMT curriculum for the Charter Class of 2016 (matriculation July 2012) and the Class of 2017 (matriculation July 2013) has previously been reported.5,7 The course for students matriculating in 2012 had an isolated EMT course administered prior to the start of biomedical science coursework. Following this, the Curriculum Committee voted to integrate the EMT course into the Structure and Function of the Human Body 1 (SF1) module, a course that was predominately gross anatomy and embryology, for the classes matriculating in 2013 and 2014. The integration of EMT and SF1 increased the number of weeks for EMT course delivery. Following the third iteration, the Curriculum Committee voted to revert back to the original design of separating the courses. Table 1 describes the EMT course content and duration for the first 6 years.
Table 1.
Emergency Medical Technician (EMT) Course Content, Dates and Description
| EMT Course Content Area | Required State Hours | Year Students Matriculated into Medical School | |||||
|---|---|---|---|---|---|---|---|
| †2012 | †2013 | 2014 | 2015 | 2016 | 2017 | ||
| Preparatory Module | 32 | 35 | 37 | 33 | 33 | 33 | 33 |
| Airway Module | 20 | 20 | 32 | 22 | 21 | 21 | 21 |
| Patient Assessment Module | 20 | 20 | 32 | 20 | 21 | 21 | 21 |
| Medical Module | 48 | 48 | 59 | 58 | 55 | 55 | 55 |
| Trauma Module | 40 | 41 | 43 | 43 | 40 | 40 | 40 |
| Pediatrics Module | 12 | 17 | 12 | 16 | 12 | 12 | 12 |
| Operations Module | 12 | 20 | 19 | 18 | 22 | 18 | 18 |
| Skill Prep/Review | 16 | 17 | 16 | 18 | 18 | 21 | 21 |
| Total Course Hours | 200 | 218 | 250 | 228 | 222 | 221 | 221 |
| Ambulance Field Hours | 24 | 24 | 24 | 24 | 24 | 24 | 24 |
| Required Patient Encounters | 5 | 5 | 10 | 10 | 10 | 10 | 10 |
| Examinations | N/A | 9 | 6 | 4 | 4 | 4 | 4 |
| Biomedical Sciences Integration | N/A | No | Yes | Yes | No | No | No |
| Dates of Course | N/A | August 1-September 9 | August 1-November 1 | July 31-October 24 | July 29-September 18 | July 27-September 9 | July 19-September 1 |
| Total number of weeks | N/A | 5.5 | 13 | 11.5 | 7.5 | 6.5 | 6.5 |
Notes: Biomedical Sciences Integration = Integration of Emergency Medicine Technician (EMT) course with biomedical science content (i.e. gross anatomy).† Represents data previously published and reprinted with permission from: copyright © The National Association of EMS Physicians, http://www.naemsp.org/Pages/default.aspx, reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the National Association of EMS Physicians.5
Abbreviation: N/A, not applicable.
At the completion of their first year, students complete the voluntary program-to-date (PTD) survey which includes statements about the EMT course and program. For student perceptions of the statements related to the EMT course, students rate statements using the following Likert Scale descriptors with associated point values: Very Dissatisfied = 1, Dissatisfied = 2, Neutral – Neither Satisfied or Dissatisfied = 3, Satisfied = 4, Very Satisfied = 5. For student perceptions of experiences and clinical skill development provided by the EMT program (ie, EMT course and required 12 hr EMT shifts), students rate statements using the Likert scale with the following descriptors and associated point values: Strongly Disagree = 1, Disagree = 2, Neutral-Neither Agree nor Disagree = 3, Agree = 4, Strongly Agree = 5. Being a new medical school, the number of students matriculating were approximately half the projected full class for the first two classes and increased by 25% for the third and fourth classes. The number of surveys sent to each class were: first class 52, second class 54, third class 82, fourth and fifth classes 103 and sixth class 105. We analyzed student responses to statements about the EMT program in conjunction with the layout of the course.
Statistics
We analyzed data using GraphPad Instat® version 3.10 (GraphPad Software, San Diego, California). We performed a one-way ANOVA with post hoc Tukey Honestly Significant Difference (HSD) for comparison across all years for responses to each survey statement pertaining to EMT course design or EMT experiences and clinical skill development.
Ethical Approval
This study was reviewed and exempted by the University of South Carolina Institutional Review Board (IRB) with a cooperative review by the Greenville Health System IRB based on researcher affiliations.
Copyright permission was granted with the full acknowledgment to the original sources of publication as follows: copyright © The National Association of EMS Physicians, reprinted by permission of Taylor & Francis Ltd on behalf of The National Association of EMS Physicians.
Results
Overall student response rates ranged between 46–52 (88–100%) for 2012, 40–46 (74–85%) for 2013, 72–79 (88–96%) for 2014, 73–86 (71–83%) for 2015, 47–65 (46–63%) for 2016, and 62–82 (59–78%) for 2017. Student response rates for each statement are provided in Tables 2 and 3.
Table 2.
Student Perceptions of the Statements Related to Emergency Medical Technician (EMT) Course
| Statement | Year Students Matriculated into Medical School | ||||||
|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | ||
| A) Academic Workload/Demands on Student Time | Mean (SEM) | 4.31 (0.08) | 3.60 (0.08)*, *** | 3.89 (0.05)††† | 4.08 (0.05)### | 4.28 (0.07) | 4.46 (0.06) |
| N (%) | 52 (100%) | 45 (83%) | 79 (96%) | 86 (83%) | 65 (63%) | 82 (78%) | |
| B) Incorporation of Clinically Relevant Material | Mean (SEM) | 4.47 (0.09) | 3.95 (0.09)**, *** | 4.35 (0.06) | 4.42 (0.05) | 4.31 (0.07)* | 4.57 (0.06) |
| N (%) | 52 (100%) | 44 (81%) | 78 (95%) | 86 (83%) | 65 (63%) | 82 (78%) | |
| C) Fairness of Summative Assessments in Course | Mean (SEM) | 4.42 (0.08) | 3.89 (0.08)*, *** | 4.04 (0.05)††,††† | 4.17 (0.05) | 4.33 (0.07) | 4.37 (0.05) |
| N (%) | 52 (100%) | 45 (83%) | 79 (96%) | 86 (83%) | 64 (62%) | 81 (77%) | |
| D) Helpfulness in Preparing You for USMLE® exams | Mean (SEM) | 3.55 (0.07) *** | 2.58 (0.08)††,††† | 3.14 (0.04) | 3.03 (0.04) | 2.94 (0.07) | 3.71 (0.06)### |
| N (%) | 46 (88%) | 40 (74%) | 72 (88%) | 73 (71%) | 47 (46%) | 62 (59%) | |
| E) Appropriateness of Teaching Methods | Mean (SEM) | 4.23 (0.08) | 3.41 (0.07)*** | 4.06 (0.05)††,††† | 4.33 (0.05) | 4.11 (0.06)## | 4.41 (0.05) |
| N (%) | 52 (100%) | 46 (85%) | 79 (96%) | 86 (83%) | 64 (62%) | 82 (78%) | |
| F) General Module Organization | Mean (SEM) | 4.23 (0.08) | 3.13 (0.07) *** | 3.66 (0.04)††† | 4.14 (0.05)# | 4.03 (0.06)### | 4.38 (0.05) |
| N (%) | 52 (100%) | 45 (83%) | 79 (96%) | 86 (83%) | 65 (63%) | 82 (78%) | |
| G) Overall Module Quality | Mean (SEM) | 4.37 (0.08) | 3.57 (0.07)*** | 3.97 (0.05)††† | 4.13 (0.05) | 4.11 (0.06) | 4.46 (0.06)### |
| N (%) | 52 (100%) | 46 (85%) | 78 (95%) | 86 (83%) | 65 (63%) | 82 (78%) | |
Notes: Results are reported as the mean of the Likert scale responses (Mean) and standard error of the mean (SEM). Likert Scale descriptors with associated point values: Very Dissatisfied = 1, Dissatisfied = 2, Neutral – Neither Satisfied or Dissatisfied = 3, Satisfied = 4, Very Satisfied = 5. N= number of students responding to statement. % = percent of students responding to statement. A) ***p<0.001 2013 vs 2012, 2015, 2016, and 2017. *p<0.05 2013 vs 2014. †††p<0.001 2014 vs 2012, 2016 and 2017. ###p<0.001 2015 vs 2017. B) ***p<0.001 2013 vs 2012, 2015, and 2017. **p<0.01 2013 vs 2014 and 2016. *p<0.05 2016 vs 2017. C) *p<0.05 2013 vs 2015. ***p<0.001 2013 vs 2012, 2016, and 2017. ††p<0.01 2014 vs 2016. †††p<0.001 2014 vs 2017. D) ***p<0.001 2012 vs 2013, 2014, 2015, and 2016. †††p<0.001 2013 vs 2014, 2015, and 2017. ††p<0.01 2013 vs 2016. ###p<0.001 2017 vs 2014, 2015 and 2016. E) ***p<0.001 2013 vs all other years. ††p<0.01 2014 vs 2015. †††p<0.001 2014 vs 2017. ##p<0.01 2016 vs 2017. F) ***p<0.001 2013 vs all other years. †††p<0.001 2014 vs all other years. #p<0.05 2015 vs 2017. ###p<0.001 2016 vs 2017. G) ***p<0.001 2013 vs all other years. †††p<0.001 2014 vs 2012 and 2017. ###p<0.001 2017 vs 2015 and 2016.
Table 3.
Student Perceptions of Experiences and Clinical Skill Development Provided by the Emergency Medical Technician (EMT) Program
| Statement | Year of EMT Course | ||||||
|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | ||
| A) The EMT curriculum provided me with the opportunities I expected | Mean (SEM) | 4.25 (0.08) | 3.80 (0.08)**, *** | 4.21 (0.05) | 4.16 (0.05) | 4.02 (0.06)†† | 4.35 (0.05) |
| N (%) | 52 (100%) | 46 (85%) | 78 (95%) | 85 (83%) | 64 (62%) | 81 (77%) | |
| B) Participating as an EMT made me more confident in my clinical skills | Mean (SEM) | 4.35(0.08)*** | 3.98 (0.08)*, ** | 4.30 (0.05)††† | 3.96 (0.05)## | 3.80 (0.07)### | 4.24 (0.05) |
| N (%) | 52 (100%) | 46 (85%) | 79 (96%) | 85 (83%) | 65 (63%) | 82 (78%) | |
| C) The EMT curriculum allowed me the opportunity to gain better understanding of our patient population | Mean (SEM) | 4.69 (0.10) | 4.60 (0.11) | 4.62 (0.06) | 4.56 (0.05) | 4.40 (0.07) | 4.57 (0.06) |
| N (%) | 51 (98%) | 45 (83%) | 78 (95%) | 86 (83%) | 65 (63%) | 82 (78%) | |
| D) The EMT curriculum gave me a better understanding of the different levels of medical care and how they work together for the care of patients | Mean (SEM) | 4.67 (0.10) | 4.24 (0.09)*, ** | 4.62 (0.06) | 4.42 (0.05) | 4.38 (0.07) | 4.57 (0.06) |
| N (%) | 51 (98%) | 46 (85%) | 79 (96%) | 86 (83%) | 64 (62%) | 82 (78%) | |
| E) The EMT curriculum allowed me the opportunity to practice patient based care while interacting with other members of the health care team | Mean (SEM) | 4.58 (0.09)**, *** | 3.98 (0.08)†, ††, ††† | 4.42 (0.06)## | 4.26 (0.05) | 4.12 (0.06) | 4.32 (0.05) |
| N (%) | 52 (100%) | 46 (85%) | 78 (95%) | 86 (83%) | 65 (63%) | 82 (78%) | |
| F) The EMT curriculum has been a clinically relevant portion of my medical education | Mean (SEM) | 4.46 (0.09)*, *** | 3.98 (0.08)†, ††† | 4.38 (0.06)### | 4.19 (0.05) | 3.97 (0.06)## | 4.27 (0.05) |
| N (%) | 52 (100%) | 46 (85%) | 79 (96%) | 85 (83%) | 64 (62%) | 82 (78%) | |
| G) The EMT curriculum had a positive influence on my medical education | Mean (SEM) | 4.46 (0.09)*, ** | 4.07 (0.09)†† | 4.23 (0.05) | 4.17 (0.05) | 4.12 (0.06)† | 4.39 (0.05) |
| N (%) | 52 (100%) | 46 (85%) | 79 (96%) | 86 (83%) | 65 (63%) | 82 (78%) | |
Notes: Results are reported as the mean of the Likert scale responses (Mean) and standard error of the mean (SEM). Likert Scale descriptors with associated point values: Strongly Disagree = 1, Disagree = 2, Neutral – Neither Agree nor Disagree = 3, Agree = 4, Strongly Agree = 5. N= number of students responding to statement. % = percent of students responding to statement. A) ***p<0.001 2013 vs 2012, 2014 and 2017. **p<0.01 2013 vs 2015. ††p<0.01 2016 vs 2017. B) ***p<0.001 2012 vs 2015 and 2016. **p<0.01 2013 vs 2012 and 2014. *p<0.05 2013 vs 2017. †††p<0.001 2014 vs 2015 and 2016. ##p<0.01 2015 vs 2017. ###p<0.001 2016 vs 2017. C) No difference among groups. D) **p<0.01 2013 vs 2012 and 2014. *p<0.05 2013 vs 2017. E) ***p<0.001 2012 vs 2013 and 2016. **p<0.01 2012 vs 2015. †††p<0.001 2013 vs 2014. †p<0.05 2013 vs 2015. ††p<0.01 2013 vs 2017. ##p<0.01 2014 vs 2016. F) ***p<0.001 2012 vs 2013 and 2016. *p<0.05 2012 vs 2015. †††p<0.001 2013 vs 2014. †p<0.05 2013 vs 2017. ###p<0.001 2014 vs 2016. ##p<0.01 2016 vs 2017. G) *p<0.05 2012 vs 2015. **p<0.01 2012 vs 2013 and 2016. ††p<0.01 2013 vs 2017. †p<0.05 2016 vs 2017.
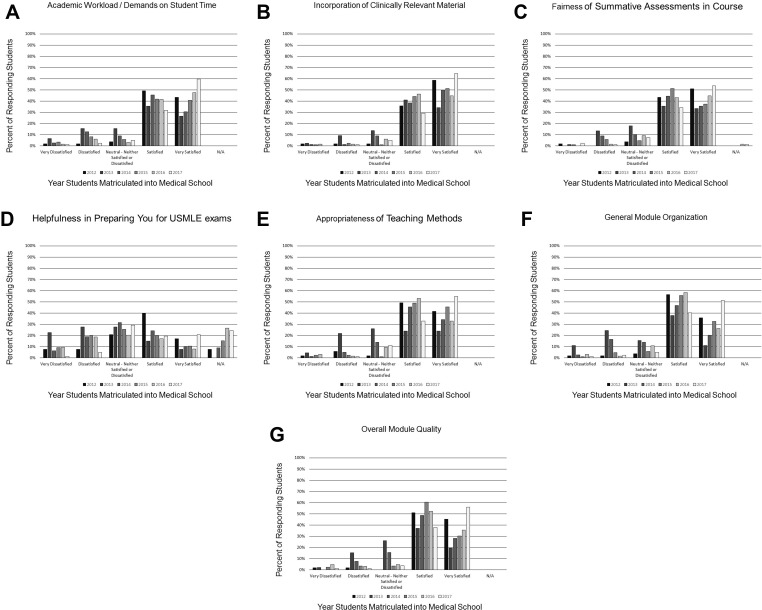
Figure 1 and Table 2 illustrate student responses to statements relating to EMT course design and Likert scale response means, respectively. For all statements related to course design, there was a statistically significant decrease in response means between the initial 2012 standalone course and the second 2013 integrated course. Response means for most statements increased from the second through the sixth course with no significant difference between the first and sixth courses.
Figure 1.
Student perceptions from 6 classes (2012–2017) for the 6 statements (1a-1g) related to the Emergency Medical Technician course. On the X-axis, bar graph shades depict each class and responses based on Likert Scale descriptors as follows: Very Dissatisfied = 1, Dissatisfied = 2, Neutral – Neither Satisfied or Dissatisfied = 3, Satisfied = 4, Very Satisfied = 5. (A) Statement: Academic workload/demands on student time. (B) Statement: Incorporation of clinically relevant material. (C) Statement: Fairness of summative assessments in course. (D) Statement: Helpfulness in Preparing You for USMLE® exams. (E) Statement: Appropriateness of teaching methods. (F) Statement: General module organization. (G) Statement: Overall module quality.
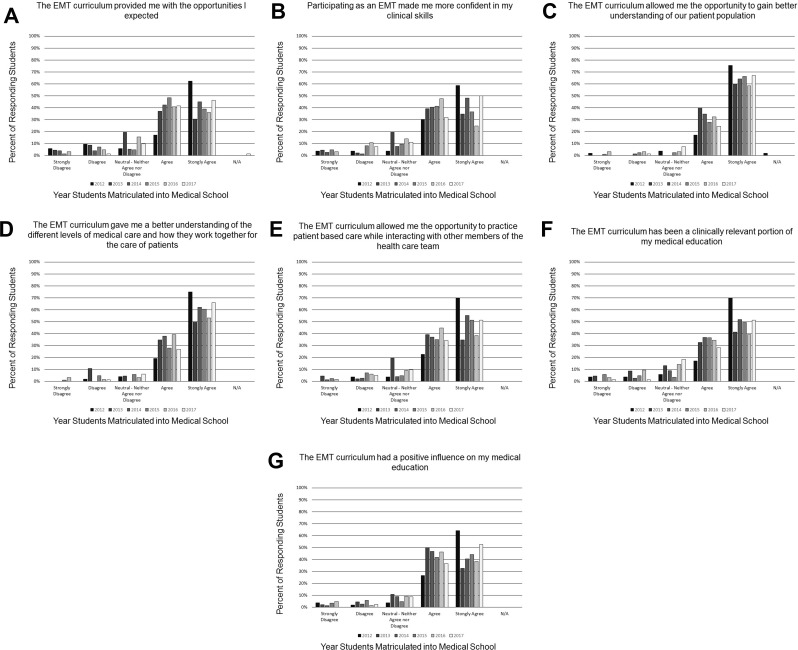
Figure 2 and Table 3 illustrate student responses to statements relating to experiences and clinical skill development and Likert scale means, respectively. Similar to the course design results, there was a statistically significant decrease in response means between the initial 2012 standalone and the second 2013 integrated course. For all statements related to experiences and clinical skill development, students in the 2012 course selected “Strongly Agree” more often than students in all subsequent courses. The only statement with a mean score ≥4.40 and no statistically significant change across all years was “The EMT curriculum allowed me the opportunity to gain better understanding of our patient population.”
Figure 2.
Student perceptions from 6 classes (2012–2017) for the 6 statements (2a-2g) related to experiences and clinical skill development provided by the Emergency Medical Technician program. On the X-axis, bar graph shades depict each class and responses based on Likert Scale descriptors as follows: Strongly Disagree = 1, Disagree = 2, Neutral – Neither Agree nor Disagree = 3, Agree = 4, Strongly Agree = 5. (A) Statement: The EMT curriculum provided me with the opportunities I expected. (B) Statement: Participating as an EMT made me more confident in my clinical skills. (C) Statement: The EMT curriculum allowed me the opportunity to gain better understanding of our patient population. (D) Statement: The EMT curriculum gave me a better understanding of the different levels of medical care and how they work together for the care of patients. (E) Statement: The EMT curriculum allowed me the opportunity to practice patient-based care while interacting with other members of the health care team. (F) Statement: The EMT curriculum has been a clinically relevant portion of my medical education. (G) Statement: The EMT curriculum had a positive influence on my medical education.
“Helpfulness in preparing for USMLE® exams” was the only statement with a response mean <4.00 for all six courses, and >50% of responses from the first course were “Satisfied” or “Very Satisfied.” Similar responses were noted in all six courses for “Incorporation of Clinically Relevant Material, Appropriateness of Teaching Methods, General Module Organization, and Overall Module Quality” with a mean response score between 4.0 and 4.5.
Discussion
To our knowledge, this is the first attempt to describe medical student perceptions of course design, experience, and clinical skill development in an EMT course and shift work over a six-year period. In addition, our results provide student feedback when the format was a standalone course at the beginning of medical school compared to when it was integrated into basic science coursework. In general, student responses were more positive to course design when the course was standalone rather than integrated. Student perceptions of their experience and clinical skill development showed similar response patterns except when students responded positively to gaining a better understanding of their patient population across all years independent of course format. This result may be a reflection of the monthly ambulance experience required throughout the first 2 years.
Most student responses for statements related to Academic Workload/Demands on Student Time and Fairness of Summative Assessments were “Satisfied” or “Very Satisfied” when the course was standalone with a shift toward “Neutral,” “Dissatisfied,” and “Very dissatisfied” when integrated. A possible explanation for this finding may be the stress or academic rigors students perceived when doubling their coursework with EMT and SF1.
The first and sixth classes had the highest percent of “Very Satisfied” or “Satisfied” responses to all other course design components while the second and third classes had the lowest. Although the reasons for these trends were not specifically evaluated, plausible explanations are that the EMT course is pass-fail and not used in determining class rank contrary to biomedical science courses which result in letter grades and are used to determine rank; therefore, students may have spent more time and placed more emphasis on the SF1 material when the courses were integrated during the second and third classes. In addition, students in the first, fourth, fifth, and sixth classes often commented that they appreciated the comradery of the standalone EMT course prior to beginning the traditional biomedical science courses.
Except for the first class, most students did not perceive that the EMT course helped prepare them for USMLE exams with <41% in most years responding “Very Satisfied” or “Satisfied” and an increasing number of students responding N/A (which did not have an associated point value) through year five to this statement. This was an expected finding in that EMT material is certainly less comprehensive than what would be expected on a USMLE examination.
Similar responses over the 6 years were noted with Incorporation of Clinically Relevant Material, Appropriateness of Teaching Methods, General Module Organization, and Overall Module Quality with a mean response score between 4.0 and 4.5 with >90% of students responding “Very Satisfied” or “Satisfied” to all four statements by the first class. There was a decrease in mean response score and percent of students responding “Very Satisfied” or “Satisfied” in the second class when integration occurred, with both the mean response score and percent of students responding “Very Satisfied” or “Satisfied” increasing over the next 2 classes, slightly decreasing in the fifth class, and an increase in the sixth class.
The positive responses in all categories by the first class may be due to the fact that students were proud to be in the Charter Class and had more positive feelings about all aspects of the school. Further, there were no students above them that could have biased their thoughts or opinions because of perceived comments expressed by upper-level students which may have been the case with the other classes.
Responses to the experience and clinical skill development questions from all classes followed trends similar to the curricular questions. The first class again responded more positively in most categories than the remaining years, except for the opportunity to gain a better understanding of the patient population, in which all years had a mean response score ≥4.40 and ≥90% of responses being “Strongly Agree” or “Agree.” The majority of responses in all categories and from all classes had a mean response score >4.0 with ≥85% responding “Strongly Agree” or “Agree” which suggests that students seemed to favor the experiential and clinical aspects of EMT training. This was true even for the 2 years where EMT was integrated with SF1. Responses in most categories were slightly lower in the second class which may be a result of the first attempt of integrating EMT with SF1. One explanation for these positive results may again be related to the requirement for ongoing ambulance shifts during the first 2 years.
Student responses to the opportunities expected varied across classes with the number of students that “Strongly Disagreed” or “Disagreed” decreasing for subsequent years. This was somewhat unexpected because all students applying to this medical school understand that EMT training is a component of the first-year curriculum. It may be that there were mixed or false expectations about what constitutes this type of training and the ongoing ambulance requirements for the first 2 years. Another explanation might be that individual student experiences could have varied throughout each ambulance shift with some students encountering more critically ill or injured patients while others were exposed to less urgent transports. One anecdotal story from a second-year student related to their final EMS shift in their second year. When dispatched to the scene of multiple gunshot victims, the student was assigned to assist with the care of a middle-aged male who sustained a single gunshot wound to the chest. Vital signs were lost en route to the hospital, so the student was asked to performed cardiopulmonary resuscitation. On emergency department arrival, the student directly witnessed an open thoracotomy and was allowed to briefly perform open heart massage under the direct instruction and close supervision of the Trauma and Emergency Medicine attending until the patient was transported emergently to the operating room. This experience would be rare for most preclinical medical students, and it is likely that this student will always recall and reflect on this unique experience.
The highest mean response scores from all classes (4.40–4.69) and where ≥91% of responses were “Strongly Agree” and “Agree” were noted in students having the opportunity to understand patient populations. In addition, this category did not have statistically significant differences amongst classes. This was expected because the clinical shifts on the ambulance during the course and each subsequent month exposes the student to disenfranchised communities where their future patients may reside. This is perhaps the most important aspect and positive attribute of the EMT program. It is likely that the majority of medical students have never encountered a broad spectrum of socioeconomic conditions nor observed poverty-stricken, violent neighborhoods. It is anticipated that this experience will strengthen each students cultural competencies and instill more compassion and empathy towards these individuals when encountered in their future practice.
High mean response scores where ≥85% of responses were also “Strongly Agree” and “Agree” were noted in the category of students understanding the different levels of medical care and how each works together. During EMT shifts, students have the opportunity to observe how care is initiated in the field and continued in the hospital environment. This is particularly true for cerebrovascular accidents, ST-elevation myocardial infarctions, sepsis, and trauma where expedient prehospital care directly impacts care in the emergency department and outcome.9–13 A similar trend in mean scores, although slightly lower, were noted in the practicing of patient-based care and interacting with other team members. This was expected because students are exposed to interprofessional providers in the field (firefighters and law enforcement officers) and in the hospital setting when transfer of care is performed (allied health, nurses, physicians).
Overall, students in each year valued the influence EMT training had on their medical education with ≥83% of students responding “Strongly Agree” or “Agree” in all years. This is an important finding given the responses to the curricular design statement regarding USMLE preparation, especially now because students seem to place extraordinary emphasis on how all medical school courses prepare them to be successful on this exam because of the importance it plays for specialty and residency program selection.14
One limitation of this report is the lower response rates from students completing the survey in 2016 compared to other years. It is unclear as to why this occurred. Further, the survey was administered upon completion of the academic year which was 8 months following the completion of the EMT course and 10 months prior to taking the USMLE® Step 1 exam. An additional limitation is that student expectations for the first class of students might have been different than subsequent years because this class did not have the ability to discuss the course or the shifts with previous students.
Conclusion
In conclusion, students preferred a standalone EMT course format over an integrated EMT course. Most students strongly agreed that the EMT program allowed them to better understand patient populations and had a positive influence on their medical education; however, they did not feel the course helped prepare them for USMLE exams.
Ethical Approval
This study received exemption from Human Research Subjects on 6/6/2017 by the University of South Carolina institutional review board. The reference number is Pro00066701.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Cooke M, Irby DM, O’Brien BC. Carnegie Foundation for the Advancement of T. Educating Physicians: A Call for Reform of Medical School and Residency. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]
- 2.Harrison RR, Maull KI, Boyan CP. Emergency medical technician (EMT-A) instruction of medical students. J Am Coll Emer Phys. 1979;8(12):513–514. doi: 10.1016/S0361-1124(79)80297-X [DOI] [PubMed] [Google Scholar]
- 3.Bradley K, Anwar RA, Davidson SJ, Mariano J. A time efficient EMT-A course for first year medical students. Ann Emerg Med. 1982;11(9):478–481. doi: 10.1016/S0196-0644(82)80066-8 [DOI] [PubMed] [Google Scholar]
- 4.Burdick WP, Davidson SJ. Expansion of emergency medicine’s responsibilities for preclinical education of medical students. Ann Emerg Med. 1985;14(2):131–133. doi: 10.1016/S0196-0644(85)81074-X [DOI] [PubMed] [Google Scholar]
- 5.Blackwell TH, Halsey RM, Reinovsky JH. Emergency medical technician training for medical students: a two-year experience. Prehosp Emergency Care. 2016;20(4):518–523. doi: 10.3109/10903127.2015.1115930 [DOI] [PubMed] [Google Scholar]
- 6.Kwiatkowski T, Rennie W, Fornari A, Akbar S. Medical students as EMTs: skill building, confidence and professional formation. Med Educ Online. 2014;19:24829. doi: 10.3402/meo.v19.24829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Russ-Sellers R, Blackwell TH. Emergency medical technician training during medical school: benefits for the hidden curriculum. Acad Med. 2017;92(7):958–960. doi: 10.1097/ACM.0000000000001579 [DOI] [PubMed] [Google Scholar]
- 8.Shapiro LN, Defoe D, Jung MK, Li TS, Yao SC. Effects of clinical exposure to osteopathic manipulative medicine on confidence levels of medical students. J Am Osteopath Assoc. 2017;117(8):e1–e5. doi: 10.7556/jaoa.2017.105 [DOI] [PubMed] [Google Scholar]
- 9.Studnek JR, Artho MR, Garner CL Jr, Jones AE. The impact of emergency medical services on the ED care of severe sepsis. AM J Emerg Med 2012;30(1)51–56. doi: 10.1016/j.ajem.2010.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim S, Shin SD, Ro YS, et al. Effect of Emergency Medical Services Use on Hospital Outcomes of Acute Hemorrhagic Stroke. Prehosp Emerg Care. 2016;20(3):324––32.. doi: 10.3109/10903127.2015.1102996 [DOI] [PubMed] [Google Scholar]
- 11.Brown JP, Mahmud E, Dunford JV, Ben-Yehuda O. Effect of prehospital 12-lead electrocardiogram on activation of the cardiac catheterization laboratory and door-to-balloon time in ST-segment elevation acute myocardial infarction. Am J Cardiol. 2008;101(2):158-61. doi: 10.1016/j.amjcard.2007.07.082 [DOI] [PubMed] [Google Scholar]
- 12.Feero S, Hedges JR, Simmons E, Irwin L. Does out-of-hospital EMS time affect trauma survival? Am J Emerg Med. 1995;13(2):133––5.. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez RP, Cummings GR, Phelan HA, Mulekar MS, Rodning CB. Does increased emergency medical services prehospital time affect patient mortality in rural motor vehicle crashes? A statewide analysis. Am J Surg. 2009;197(1):30–34. doi: 10.1016/j.amjsurg.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 14.National Resident Matching Program, Data Release and Research Committee: Results of the 2018 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; 2018. [Google Scholar]