Abstract
Background.
Aims of this study are to explore the associations of readmission to psychiatric hospital over time, to develop a statistical model for early readmission to psychiatric hospital and to assess the feasibility of predicting early readmission.
Method.
The sample comprised 7891 general psychiatric discharges in South London, taken from a large anonymised repository of electronic patient records. We initially explored time to readmission using Cox regression – this included investigation of time-dependent effects. Subsequently, we used logistic regression to create a predictive model for 90-day readmission. We investigated the effect on readmission of a set of variables that included demographic variables, diagnosis and legal status during the index admission, previous service use, housing variables and individual item scores on the Health of the Nation Outcome Scales (HoNOS) at admission and at discharge.
Results.
Fifteen per cent of those discharged were readmitted within 90 days. Cox regression demonstrated that the estimated baseline hazard of readmission declined steeply after discharge and that the effects of several predictors, especially diagnosis, changed over time – most notably, personality disorder was associated with increased readmission relative to schizophrenia at the time of discharge, but did not significantly differ by 1-year postdischarge. In the logistic regression, increased readmission was associated with personality disorder diagnosis; shorter length of the index admission (excepting zero length admissions); number of discharges in the preceding 2 years; and having a high score at discharge on the HoNOS overactive and aggressive behaviour item, cognitive problems item or hallucinations and delusions items. Detention under Section 3 or a forensic section of the Mental Health Act during the index admission was associated with reduced readmission. The coefficient of discrimination for the logistic regression, which is equivalent to r2, was 0.04 and the estimated area under the receiver operating curve was 0.65.
Conclusions.
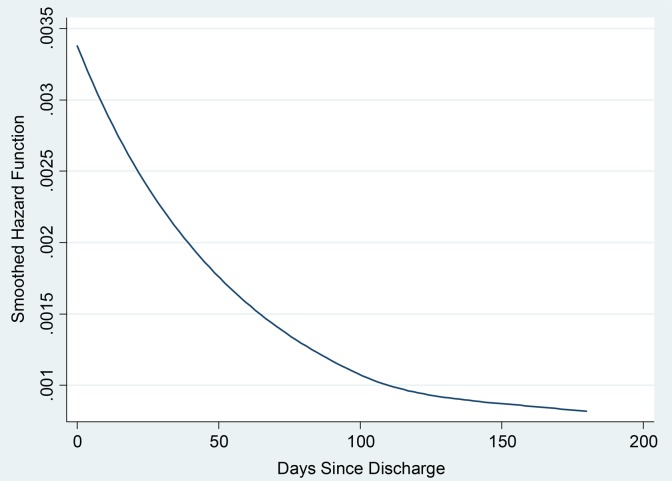
The association found between early readmission and personality disorder diagnosis merits further investigation, as does the possible trade-off between reduction in length of stay and increased readmission. Other novel findings such as the associations found with HoNOS item scores also merit replication. As with previous studies, we found that the rate of readmission declines steeply after hospital discharge, so that the period immediately subsequent to discharge is a period of comparatively high risk. However, prediction of early readmission within this high-risk group remains challenging – it seems most likely that many unmeasured influences operate subsequent to the time of discharge.
Key words: Hospital, patient readmission, psychiatric, Psychiatric Department
Introduction
In health systems oriented towards community treatment for mental health problems, the achievement of a low rate of hospital readmission is a widely applied performance indicator (OECD, 2011) and has the potential to significantly impact on the cost of services by reducing the use of hospital beds (Mangalore & Knapp, 2007). It has been the target of a number of specific interventions (Vigod et al. 2013) as well as broader-based community treatment approaches. Understanding the predictors of psychiatric readmission – especially those which occur soon after discharge, a phenomenon sometimes called ‘bouncing back’ (Kind et al. 2007a, b, 2008, 2010; Sherman, 2009) – would help to guide service redesign and stimulate further research and development work. Furthermore, if individual predictions discriminate sufficiently well between those who will and those who will not be readmitted, they could in principle guide individual treatment in hospital and during the transition back to the community. The literature however suggests that relatively few variables are consistently associated with readmission (Klinkenberg & Calsyn, 1996; Durbin et al. 2007), of which perhaps the best established are time since discharge (Durbin et al. 2007) – with the period immediately after discharge being associated with highest risk – and number of previous discharges (Russo et al. 1997; Sytema & Burgess, 1999; Moran et al. 2000; Hendryx et al. 2003; Thompson et al. 2003; Clements et al. 2006; Carr et al. 2008; Mellesdal et al. 2010; Wheeler et al. 2011; Zilber et al. 2011). There is rather less evidence for diagnosis, which appears to have consistent effects only in larger studies indicating that effect sizes are likely to be smaller (Mojtabai et al. 1997; Korkeila et al. 1998; Heggestad, 2001; Hodgson et al. 2001; Thompson et al. 2003; Valevski et al. 2007; Carr et al. 2008; Heggestad et al. 2011) and also for younger age (Mojtabai et al. 1997; Korkeila et al. 1998; Sytema & Burgess, 1999; Heggestad, 2001; Hendryx et al. 2001, 2003; Valevski et al. 2007; Zilber et al. 2011). There is some evidence for an effect of gender (Schoenbaum et al. 1995; Korkeila et al. 1998; Heggestad, 2001; Hodgson et al. 2001; Valevski et al. 2007; Carr et al. 2008; Mellesdal et al. 2010), albeit with little consistency in the size and significance of the effect or its direction. Predictive models for readmission have begun to be developed in the UK (Nuffield Trust, 2011), including the Scottish SPARRA-MD model for psychiatric readmissions (NHS National Services Scotland, 2009), which makes use of data on previous hospital utilisation, diagnosis and age. Recently, routine outcome measurement and electronic patient records have broadened the range of potential predictive factors that might be investigated. We investigated readmission among an inclusive sample of individuals discharged from general psychiatric wards in a large, single metropolitan NHS Foundation Trust in Southeast London. First we constructed an exploratory Cox regression model intended to provide an overall picture of the factors associated with readmission and how the effects of these vary over time. Subsequently, in order to create a model better suited to making predictions of readmission risk, we performed a logistic regression of the odds of readmission. Based on graphical analyses of the survivor function, findings of time-dependence in the effects of some key covariates, and to maximise statistical power, we chose to analyse readmissions in the first 90 days after discharge.
Method
Data came from the National Institute of Health Research (NIHR) Biomedical Research Centre (BRC) Case Register, which is an anonymised copy of the South London and Maudsley NHS Foundation Trust's paperless electronic patient record database, optimised for data extraction (Stewart et al. 2009). The Case Register includes data covering all secondary mental health care for the London Boroughs of Croydon, Lambeth, Lewisham and Southwark since 2006.
The main study analyses were performed on a dataset previously used for a study of the effects of facilitated discharge by home treatment teams, and full details of dataset construction have been published elsewhere (Tulloch et al. 2014). That study included an adjusted estimate of the effect of facilitated discharge on readmission, but did not address the broader question of the associations of readmission. In brief, the dataset comprised all hospital stays ending with a discharge from one of the adult general psychiatric wards operated by the Trust to an address within the four London Boroughs above and occurring on any day between 1st June 2008 and 31st May 2013. When the same individual had more than one discharge over this period, the first was selected. Dates of readmission were transformed into survival durations and also into a dichotomous variable representing readmission within 90 days of discharge. The latter was defined as missing for those not followed up for 90 days, with these individuals being excluded from analysis (N = 91, comprising 65 who moved outside the study area and 26 who died). Survival durations were censored if death occurred or when a subject moved outside the catchment area of the Trust, the latter ensuring that we did not include analysis time during which an individual would normally be admitted to a hospital outside the Trust. All observations not ending in failure, death or movement outside the study area by the time of data extraction (8th November 2013) were administratively censored – in other words, the last date of follow up was 8th November 2013. The following 33 covariates were also extracted: (1) age at admission; (2) sex; (3) ethnicity – coded as White British, Black or Other; (4) marital status; (5) having dependent children or access to children; (5) the ICD-10 primary diagnosis recorded closest to discharge; (6) the most restrictive legal status during the admission, categorised as per Tulloch et al. (2014); (7) the number of discharges from inpatient mental health services in the 2 years preceding admission (0,1,2, ≥3); (8) the log-transformed length in days of the longest of these admissions; (9) the number of periods of home treatment starting in the 2 years preceding admission (0,1, ≥2); (10) having a different address at discharge from admission; (11) being discharged to a care home; (12–32) scores on individual items from the Health of the Nation Outcome Scales (HoNOS (Wing et al. 1998)) at admission and at discharge, excluding the other mental and behavioural problems items and the problems with occupation items, all recoded as ‘low’ (0–1) or ‘high’ (2–4); (33) whether or not there was a ‘facilitated discharge’ by a home treatment team. These variables were included in the present analysis either because their effects on readmission have previously been investigated, or because they are closely related to such variables, or because their effects seemed worthy of further investigation and they were recorded for a significant proportion of admissions (the latter applied particularly to the HoNOS item scores).
Initial descriptive and unadjusted analyses were performed. As described in Tulloch et al. (2014), we used multiple imputation by chained equations to ‘fill in’ missing data (van Buuren et al. 1999; Royston, 2004). To provide an overall understanding of the effects of covariates on readmission, how these effects vary over time, and how the underlying hazard of readmission varies over time, we first fitted a full Cox regression model on each of the imputed datasets, combining parameter estimates from separate analyses of each imputed dataset as per Rubin's rules (Rubin, 1987), and including all of the 33 covariates listed above. Prior to the fitting of this full model, functional forms for continuous covariates had been defined using the method of fractional polynomials (Royston & Sauerbrei, 2008) in a dataset with complete values on key covariates (demographic variables, diagnosis and service use variables). The full model was tested for non-proportional hazards by estimating the slope of the scaled Schoenfeld residuals in five randomly chosen imputed datasets, and a final model was then fitted in which any non-proportional hazards were allowed for by adding in parameters to represent interactions between covariates and time.
Next, we fitted a multivariable logistic regression, modelling the odds of readmission in the 90 days after hospital discharge. As noted above, we chose to analyse 90-day readmissions based on the survivor function, our findings in relation to time-dependent effects and our wish to maximise statistical power. We excluded individuals lost to follow up within 90 days of discharge. Here, unlike the Cox regression, we aimed to fit a parsimonious model, so after definition of the functional form for continuous covariates using the methods above, we adopted the following procedure, largely following Hosmer et al. (2008):
-
(1)
All 33 covariates were included in an initial model. Probability values for each coefficient were calculated using the Wald test: individual p values for continuous and dichotomous variables and an overall p value for multi-level categorical variables.
-
(2)
All variables with p ≥ 0.20 were subtracted.
-
(3)
All variables with p ≥ 0.05, but p < 0.20 were subtracted in turn, starting with the least significant, examining other coefficients for a change in value of greater than 20%, which would indicate the possibility of confounding by the subtracted variable.
-
(4)
Each of the subtracted variables was then retested for inclusion, aiming to include variables with adjusted p value <0.05 or evidence of a substantial confounding effect as defined above.
Goodness of fit was estimated using the Hosmer and Lemeshow test (Hosmer & Lemeshow, 1980), with the number of groups adjusted accorded to sample size (Paul et al. 2013). We performed the test on the whole dataset and also on the subset of observations for which covariate data were complete, but still using the estimates taken from the final analysis of imputed data. The coefficient of discrimination (mean predicted probability of readmission among those who were readmitted minus mean predicted probability of readmission among those who were not readmitted), which provides a measure analogous to r2 and which does not require an estimated likelihood (Tjur, 2009), was estimated again on the whole dataset and on the subset of observations with complete covariate data. Area under the receiver operating characteristics curve (AUROC) was also calculated.
As the logistic regression was based on a complete sample comprising all those readmitted as well as those not readmitted, the exponential of the intercept term represents the baseline odds of readmission. Using this estimate, multiplying by the relevant odds ratios, and then converting using the formula that odds=probability/(1−probability) it is possible to produce predictions of the probability of readmission. A single worked example is given in the Results section.
Results
Sample characteristics
The sample for the main analysis comprised 7891 hospital discharges. Overall characteristics of the sample based on complete data are shown in Table 1 – for the sake of brevity, only those variables included in the final models and key demographic variables are shown. Demographic and clinical variables were either complete or near-complete, with the exception of the measure of having dependent children or other access to children, which was 27% missing. Service use data were complete. Individual HoNOS item scores at the time of admission were generally missing in around 22% of cases, and at the time of discharge in around 45% of cases.
Table 1.
Characteristics of all inpatient discharges in the sample
| Variable | N with complete data (%) | Mean (s.d.) or N (Proportion) |
|---|---|---|
| Age | 7891 (100%) | 39.1 years (12.4) |
| Gender | 7891 (100%) | |
| Male | 4382 (56%) | |
| Female | 3509 (44%) | |
| Ethnicity | 7724 (98%) | |
| White British | 3929 (51%) | |
| Any Black ethnic group | 2842 (37%) | |
| Other | 953 (12%) | |
| Marital status | 7763 (98%) | |
| Single | 5572 (72%) | |
| Divorced, separated or widowed | 1058 (14%) | |
| Married or cohabiting | 1133 (15%) | |
| Primary diagnosis | 7667 (97%) | |
| Schizophrenia (F20) | 1911 (26%) | |
| Other psychotic disorders (F21–F29) | 1256 (16%) | |
| Hypomania/mania/bipolar disorder (F30–F31) | 918 (12%) | |
| Depression (F32–F39) | 1204 (16%) | |
| Neurotic and anxiety disorders (F40–F49) | 662 (9%) | |
| Personality disorders (F60–F69) | 440 (6%) | |
| Drug & alcohol disorders (F10-F19) | 873 (11%) | |
| Other primary diagnosis | 403 (5%) | |
| Legal status* | 7891 (100%) | |
| Informal | 4657 (59%) | |
| Section 2 | 1672 (21%) | |
| Section 3/Forensic | 1562 (20%) | |
| Length of the index hospital admission† | 7891 (100%) | |
| Zero days | 253 (3%) | |
| 1–5 days | 1736 (22%) | |
| 6–18 days | 2052 (26%) | |
| 19–47 days | 1940 (25%) | |
| 48 days or more | 1910 (24%) | |
| Discharges ending in preceding 2 years‡ | 7891 (100%) | |
| None | 6495 (82%) | |
| One | 877 (11%) | |
| Two | 305 (4%) | |
| Three or more | 214 (3%) | |
| Community Mental Health Team at discharge | 7891 (100%) | |
| Assertive outreach | 233 (3%) | |
| Other, not assertive outreach | 4903 (62%) | |
| None | 2755 (35%) | |
| Admission HoNOS item scores | ||
| Overactive, aggressive, disruptive or agitated behaviour | 6229 (79%) | |
| Score 0 or 1 | 3803 (61%) | |
| Score 2, 3 or 4 | 2426 (39%) | |
| Non-accidental self-injury | 6217 (79%) | |
| Score 0 or 1 | 4496 (72%) | |
| Score 2, 3 or 4 | 1721 (28%) | |
| Cognitive problems | 6189 (78%) | |
| Score 0 or 1 | 4915 (79%) | |
| Score 2, 3 or 4 | 1274 (21%) | |
| Discharge HoNOS item scores | ||
| Overactive, aggressive, disruptive or agitated behaviour | 4308 (55%) | |
| Score 0 or 1 | 3807 (88%) | |
| Score 2, 3 or 4 | 501 (12%) | |
| Non-accidental self-injury | 4308 (53%) | |
| Score 0 or 1 | 3893 (90%) | |
| Score 2, 3 or 4 | 415 (10%) | |
| Hallucinations and delusions | 4301 (55%) | |
| Score 0 or 1 | 3292 (77%) | |
| Score 2, 3 or 4 | 1009 (23%) |
Note. *Legal status was defined as the most restrictive section of the Mental Health Act in force during the first week of the admission. If detention was only under Section 136, Section 5(2) or Section 5(4), this was treated as informal legal status.
†Arithmetic mean LOS was 40.4 days (s.d. 79 days); median LOS was 18 days.
‡Among those with at least one discharge from hospital in the preceding 2 years, the median length of the longest admission was 41 days (interquartile range 17–100).
In the unadjusted analysis of readmission, median follow-up time (to failure or censoring) was 1201 days (median absolute deviation 485 days; range 161–1985 days).
The overall Kaplan–Meier estimate of the risk of readmission was 8% at 30 days, 21% at 180 days and 30% at 1 year. Within 90 days of discharge, 1156 individuals had been readmitted (15% of those discharged, whether excluding censored cases or not).
Survival analysis
Examination of imputed and original data indicated no anomalies resulting from the imputation process. Testing of first degree fractional polynomials in the subsample with a partial selection of complete or near-complete covariates indicated that an inverse transformation was most appropriate to model the effect of index length of stay (LOS): there was no evidence of non-linearity for the effects of age or length of the longest previous admission. Bootstrapping indicated that this transformation or very similar transformations such as inverse square root or inverse square were selected in over 80% of samples. Testing of scaled Schoenfeld residuals within five randomly selected imputed datasets consistently indicated non-proportional hazards in the case of ethnicity, diagnosis, length of the index admission, whether or not the individual was under the care of a CMHT at the time of discharge, most restrictive legal status during the admission and the discharge HoNOS self-harm item and hallucinations and delusions item. The model was therefore first refitted including interactions with time for each of the above variables. The interaction between time and the inverse of the index LOS was non-significant in this model, and therefore the final model contains interactions with time only for the other six variables listed above.
When all parameters used to model each variable were tested simultaneously using the Wald test, the probability of all parameters being equal to zero was less than 0.05 for ethnicity (p = 0.0009); marital status (p < 0.0001); diagnosis (p < 0.0001); length of the index hospital admission (p = 0.0003); number of hospital discharges in the 2 years preceding the index admission date (p < 0.0001); most restrictive legal status during admission (p = 0.0002); whether the individual was under the care of a community mental health team at the time of discharge (p = 0.0084); the score on the admission HoNOS overactive, aggressive, disruptive or agitated behaviour item (p = 0.0307); the admission HoNOS non-accidental self-injury item (p = 0.0279); the discharge HoNOS overactive, aggressive, disruptive or agitated behaviour item (p < 0.0001); the discharge HoNOS non-accidental self-injury item (p = 0.0046) and the discharge HoNOS hallucinations and delusions item (p = 0.0004). For ease of interpretation the results are tabulated, including category-based estimates for continuous covariates (see Table 2). Estimates for variables modelled using an interaction with time are presented for day 0 and for day 365, to provide some sense of the magnitude and direction of the time-dependent effects. As noted in the Method section, this Cox model was a full model, including all 33 covariates: for the sake of concision, variables whose parameter estimates fell outside a conventional level of statistical significance are listed, with a p value, in the footnote but their parameter estimates are not included in the body of Table 2.
Table 2.
Cox regression analysis of time to readmission
| Variable | Hazard ratio (95% CI) | p Value |
|---|---|---|
| Ethnicity | ||
| White British | 1 | 0.0009 |
| Any Black ethnic group | ||
| Day 1 | 1.01 (0.91–1.13) | |
| Day 365 | 1.12 (1.03–1.21) | |
| Other ethnicity | ||
| Day 1 | 0.83 (0.71–0.98) | |
| Day 365 | 0.94 (0.83–1.06) | |
| Marital status | ||
| Single | 1 | <0.0001 |
| Divorced/separated/widowed | 1.02 (0.91–1.14) | |
| Married | 0.76 (0.68–0.86) | |
| Diagnosis | <0.0001 | |
| Schizophrenia (F20) | 1 | |
| Other psychotic disorders (F21–F29) | ||
| Day 1 | 1.00 (0.87–1.15) | |
| Day 365 | 0.98 (0.88–1.09) | |
| Hypomania/mania/bipolar disorder (F30–F31) | ||
| Day 1 | 1.10 (0.94–1.29) | |
| Day 365 | 1.07 (0.95–1.21) | |
| Depression (F32–F39) | ||
| Day 1 | 0.79 (0.65–0.96) | |
| Day 365 | 0.67 (0.57–0.78) | |
| Neurotic and anxiety disorders (F40–F49) | ||
| Day 1 | 0.87 (0.69–1.09) | |
| Day 365 | 0.68 (0.56–0.82) | |
| Personality disorders (F60–F69) | ||
| Day 1 | 1.50 (1.20–1.86) | |
| Day 365 | 1.11 (0.92,1.34) | |
| Drug & alcohol disorders (F10–F19) | ||
| Day 1 | 0.98 (0.80–1.19) | |
| Day 365 | 0.89 (0.76–1.04) | |
| Other primary diagnosis | ||
| Day 1 | 0.88 (0.69–1.13) | |
| Day 365 | 0.72 (0.59–0.88) | |
| Length of the index hospital admission | 0.0003 | |
| Zero days | 1 | |
| 1–5 days | 1.38 (1.16–1.65) | |
| 6–18 days | 1.49 (1.20–1.84) | |
| 19–47 days | 1.52 (1.21–1.91) | |
| 48 days or more | 1.54 (1.22–1.93) | |
| Number of psychiatric hospital discharges in 2 years before admission | <0.0001 | |
| None | 1 | |
| One | 1.49 (1.35–1.66) | |
| Two | 1.69 (1.45–1.96) | |
| Three or more | 2.63 (2.22–3.10) | |
| Community Mental Health Team at time of discharge | 0.0084 | |
| None | 1 | |
| Assertive Outreach | ||
| Day 1 | 0.96 (0.75–1.23) | |
| Day 365 | 1.10 (0.91–1.33) | |
| Other Community Mental Health Team | ||
| Day 1 | 0.99 (0.89–1.10) | |
| Day 365 | 1.13 (1.04–1.23) | |
| Legal status during admission | 0.0002 | |
| Informal | 1 | |
| Section 2 | ||
| Day 1 | 0.90 (0.80–1.03) | |
| Day 365 | 0.97 (0.88–1.07) | |
| Section 3 or Forensic | ||
| Day 1 | 0.84 (0.73–0.95) | |
| Day 365 | 1.02 (0.92–1.13) | |
| Admission HoNOS overactive, aggressive, disruptive or agitated behaviour = 2, 3 or 4 | 1.10 (1.02–1.20) | 0.0307 |
| Admission HoNOS non-accidental self-injury = 2, 3 or 4 | 0.88 (0.79–0.99) | 0.0279 |
| Discharge HoNOS overactive, aggressive, disruptive or agitated behaviour = 2, 3 or 4 | 1.43 (1.25–1.65) | <0.0001 |
| Discharge HoNOS non-accidental self-injury = 2, 3 or 4 | 0.0046 | |
| Day 1 | 1.41 (1.12–1.76) | |
| Day 366 | 0.99 (0.80–1.23) | |
| Discharge HoNOS hallucinations and delusions = 2, 3 or 4 | 0.0004 | |
| Day 1 | 1.33 (1.16–1.53) | |
| Day 366 | 1.17 (1.04–1.32) | |
Note. Time-varying coefficients were collectively significant as follows: ethnicity p = 0.0203; diagnosis p = 0.0106; Community Mental Health Team treatment p = 0.0122; legal status p < 0.0001; discharge HoNOS deliberate self-harm item p = 0.0043; discharge delusions and hallucinations p = 0.0107. The analysis also included the following non-significant parameters: age (p = 0.45); sex (p = 0.42); having dependent children or access to children (p = 0.96); length of the longest admission ending in the 2 years preceding admission (p = 0.22); being under the care of a Home Treatment Team during or at the end of the index admission (p = 0.32); discharge to a carehome at the end of the admission (p = 0.26); the admission HoNOS items for drug and alcohol problems (p = 0.08); cognitive problems (p = 0.06); physical illness and disability (p = 0.051); delusions and hallucinations (p = 0.44); depressed mood (0.38); relationship problems (p = 0.36); problems with activities of daily living (p = 0.37); housing problems (0.50); and the discharge HoNOS items for drug and alcohol problems (p = 0.51); cognitive problems (0.40); physical illness and disability (0.71); depressed mood (0.57); relationship difficulties (0.22); activities of daily living (p = 0.30) and housing difficulties (p = 0.78).
Taking each significant variable in turn, only ‘other’ ethnicity was associated with hazard of readmission at the time of discharge (HR 0.83; 95% confidence interval (CI) 0.71–0.98); this small effect tended towards zero over time and was non-significant at 1 year after discharge. The effect of any black ethnicity – non-significant at discharge – increased over time and was significant at 1 year after discharge, albeit similarly of very modest size (HR 1.12; 95% CI 1.03–1.21). Being married was associated with reduced readmission (HR 0.76; 95% CI 0.68–0.86).
The effect of diagnosis was highly significant (p < 0.0001 overall). To express the effects of each diagnostic category in detail requires consideration of both the main effect of that diagnosis and its interaction with time. Immediately after discharge, only the hazard ratio for personality disorder differed significantly from the baseline category, which was schizophrenia (HR 1.50; 95% CI 1.20–1.86). Broadly, interactions with time were not significant for the psychotic diagnostic categories but were highly significant for the non-psychotic diagnostic categories, meaning that the hazard of readmission declined relative to the psychotic categories over time. Combining main effects and interactions, the difference in the hazard of readmission between personality disorder and the psychotic disorders that was apparent immediately after discharge was therefore abolished over time; while the hazard of readmission for depression and anxiety disorders become significantly lower over time relative to schizophrenia (for depression at 365 days, HR was 0.67, with 95% CI 0.57–0.78; for anxiety disorders at 365 days, HR was 0.68, with 95% CI 0.56–0.82).
The effect of the length of the index admission was non-linear. The only truly marked difference was between those who were discharged on the same day as admission, and those who stayed for at least one day. For example, the hazard ratio for those who stayed between 1 and 5 days was 1.38 (95% CI 1.16–1.65). Although increased LOS was associated with increased readmission, the difference between those with very short LOS and very long LOS was less than the above difference, and the effect tended towards an asymptotic value with increasing LOS. Notably, the functional form of the relationship selected through the use of the fractional polynomial procedure differed in the logistic regression model (see below) suggesting that the functional form for the effect of index LOS may itself vary over time.
The number of discharges from hospital in the 2 years preceding the index admission date was positively associated with the hazard of readmission, and the size of this effect was substantial. For example, the hazard ratio for readmission for those with three or more discharges was 2.63 (95% CI 2.22–3.10). Being under Section 3 or a forensic section was associated with reduced readmission, but this effect attenuated over time. Being under a community mental health team was associated with no difference in readmission at baseline, but a relatively higher hazard of readmission over time.
Of the admission HoNOS items, only two reached a conventional level of statistical significance, and their probability values were not far below that level. Of the discharge HoNOS items, high scores on three items were strongly associated with increased risk of readmission: the overactive, aggressive, disruptive or agitated behaviour item, the non-accidental self-injury item and the hallucinations and delusions item. The latter two effects declined over time.
Overall, the hazard of readmission declined quickly after discharge (see Fig. 1).
Fig. 1.
Estimated Hazard function for readmission. Note. This estimated hazard function is based on a Cox regression adjusting only for complete or near-complete demographic, clinical and service use variables and does not account for time-varying covariate effects.
Logistic regression analysis
After the model-building process, the variables included in the logistic regression model, together with the probability of all parameters used to model that variable being equal to zero, were as follows: diagnosis (p = 0.0056); length of the index admission, which was entered as two fractional polynomial terms, reflecting a non-linear and non-monotonic functional form (p = 0.0085); number of discharges from psychiatric hospital in the 2 years preceding the index admission date (p < 0.0001); legal status during the admission (p = 0.0428); the admission HoNOS cognitive problems item (p = 0.0069), the discharge HoNOS overactive, aggressive, disruptive or agitated behaviour item (<0.0001) and the discharge HoNOS hallucinations and delusions item (p < 0.0001). Odds ratios for each level of these variables, together with 95% confidence interval, and with category-based estimates for continuous variables are tabulated in Table 3.
Table 3.
Logistic regression analysis of odds of 90-day readmission
| Variable | Odds ratio (95% CI) | p Value |
|---|---|---|
| Diagnosis | 0.0056 | |
| Schizophrenia (F20) | 1 | |
| Other psychotic disorders (F21–F29) | 1.00 (0.81–1.23) | |
| Hypomania/mania/bipolar disorder (F30–F31) | 1.16 (0.92–1.46) | |
| Depression (F32–F39) | 0.86 (0.67–1.09) | |
| Neurotic and anxiety disorders (F40–F49) | 0.94 (0.70–1.25) | |
| Personality disorders (F60–F69) | 1.57 (1.17–2.09) | |
| Drug & alcohol disorders (F10–F19) | 1.12 (0.87–1.43) | |
| Other primary diagnosis | 0.92 (0.66–1.27) | |
| Length of the index hospital admission | 0.0085 | |
| Zero days | 1 | |
| 1–5 days | 1.50 (1.08–2.08) | |
| 6–18 days | 1.43 (0.99–2.05) | |
| 19–47 days | 1.27 (0.89–1.81) | |
| 48 days or more | 1.11 (0.78–1.57) | |
| Number of psychiatric hospital discharges in 2 years before admission | <0.0001 | |
| None | 1 | |
| One | 1.53 (1.26–1.86) | |
| Two | 1.68 (1.24–2.27) | |
| Three or more | 3.14 (2.29–4.30) | |
| Legal status during admission | 0.0428 | |
| Informal | 1 | |
| Section 2 | 0.96 (0.81–1.14) | |
| Section 3 or Forensic | 0.75 (0.59–0.94) | |
| Admission HoNOS cognitive problems = 2, 3 or 4 | 1.27 (1.07–1.51) | 0.0069 |
| Discharge HoNOS overactive, aggressive, disruptive or agitated behaviour = 2, 3 or 4 | 1.90 (1.56–2.33) | <0.0001 |
| Discharge HoNOS hallucinations and delusions = 2, 3 or 4 | 1.53 (1.27–1.85) | <0.0001 |
Note. The baseline odds were 0.068 (95% CI 0.044–0.105), equivalent to a probability of readmission within 90 days of 6.3%.
The footnote to Table 3 includes the baseline odds of readmission –0.068 (95% CI 0.044–0.105). As noted in the methods, this figure may be used to estimate the probability of readmission. For example, a person with a diagnosis of depression who had an admission lasting 2 weeks and had one discharge in the 2 years preceding the index admission, who had been an informal patient, and who scored at the lower level on the HoNOS items for cognitive problems at admission and on the HoNOS items for agitated behaviour and delusions and hallucinations at discharge would have an approximate predicted odds of 30 day readmission of 0.068 × 0.86 × 1.43 × 1.53 × 1 × 1 × 1 × 1 = 0.13. Transforming using the equality p = odds/(1 + odds) gives an estimated probability of readmission of 12%.
In the subset of observations with complete data on the variables included in the model (N = 3561), the probability of lack of fit based on the Hosmer and Lemeshow test applied to 103 groups was 0.25, indicating acceptable model fit. The coefficient of discrimination – equal to the difference between the mean predicted probability of readmission among those readmitted (0.18) and the mean predicted probability of readmission among those who were not readmitted (0.14) – was 0.04, and the AUROC was 0.63, both results indicating limited predictive ability. Analysing all observations, and based on 500 groups, the probability of lack of fit was 0.16, the coefficient of discrimination was again 0.04, and the AUROC was 0.65.
Discussion
Strengths and limitations
Strengths of the study are its large sample size and the fact that we were able to study not just standard clinical, demographic and service use variables, but also symptoms, behaviours and social problems measured by the HoNOS. We also based our main logistic regression analysis on a thorough characterisation of readmission over time using the Cox regression, allowing us to identify variables for which it is possible that time-dependent effects might lead to differing conclusions depending on the analysis period adopted and techniques used.
The clearest limitation of our study is that data derive only from a single NHS Trust. However, both the neighbourhoods served by the Trust – either predominantly inner city (Lambeth, Lewisham and Southwark) or a mixture of inner city and suburban (Croydon) – and also the structure of the services it provides are similar to those in other parts of London and in other major urban centres in the UK, increasing the chance that our findings would generalise elsewhere. In those, presumably rare, cases where an individual still resident within the Trust's geographical catchment area was readmitted to a hospital outside the Trust, and was not then transferred back into a Trust hospital, we would not have recorded a readmission. Another limitation was the fairly high level of missing data affecting discharge HoNOS scores. Although we used multiple imputation to accommodate these missing values, effect estimates should be viewed cautiously.
Comparison of results from the Cox regression and the logistic regression
Broadly, the results from the logistic regression were consistent with those that would have been predicted from the Cox model, bearing in mind the time-dependent effects observed in the latter. Differences in the HoNOS items selected are likely to be explained by the exclusion of later readmissions and by intercorrelations between HoNOS items and the diagnostic items: despite this, the two most significant effects (the discharge HoNOS overactive, aggressive, disruptive or agitated behaviour item and the discharge HoNOS hallucinations and delusions item) featured in both models. There is a more important difference in the functional form of the effect of the length of the index admission: in both models, those who were discharged on the same day as admission were least likely to be readmitted, but in the 90-day readmission model there was a peak of readmission risk among those with the shortest non-zero admissions, with risk of readmission then declining with increasing LOS.
Interpretation of study results
In our discussion of how the results of our analyses are to be interpreted we focus on the results of the logistic regression, and especially on those covariate effects that we observed both in the Cox and the logistic regression – that is, the effects of diagnosis, LOS for the index admission, legal status, number of previous discharges and the discharge HoNOS items representing aggressive and disturbed behaviour and delusions and hallucinations.
Diagnosis
In line with previous research, we found that diagnosis had modest-sized effects on readmission. However, we believe that our demonstration of time-dependence is novel, and may help to explain inconsistencies between previous studies that adopt different definitions of readmission. Shortly after discharge, only a diagnosis of personality disorder was found to be associated with an increased rate of readmission and there was no difference between other diagnoses. However, over time, the rate of readmission declined more steeply for non-psychotic diagnoses, so that a clear distinction was observable at 1 year between depression and anxiety disorders and psychotic disorders. These effects are presumably related to some interaction between the natural history of illness and clinical practice. Contrary to some previous research, we found no effect of age (Mojtabai et al. 1997; Korkeila et al. 1998; Sytema & Burgess, 1999; Heggestad, 2001; Hendryx et al. 2001, 2003; Valevski et al. 2007; Zilber et al. 2011) or gender (Schoenbaum et al. 1995; Korkeila et al. 1998; Heggestad, 2001; Hodgson et al. 2001; Valevski et al. 2007; Carr et al. 2008; Mellesdal et al. 2010) after adjustment for other variables.
Length of stay, number of previous discharges and legal status
It is notable that the 3% of admissions culminating in a discharge on the same day were those least likely to be readmitted. It seems most likely that those who are discharged almost immediately after admission are a different and atypical group – perhaps people who are admitted to a psychiatric hospital on the strength of dubious evidence of mental disorder and who are rapidly discovered not to need admission. In the survival analysis, it appeared that other differences in LOS made little difference to the rate of readmission. However, when only readmissions within the first 90 days were considered, those with LOS of a few days were those most likely to be readmitted, and the risk of readmission then fell with increasing LOS.
If this effect of LOS for non-zero day length admissions accurately estimates the causal effect of interventions that reduce LOS, the latter might be supposed to produce a countervailing increase in the risk of early readmission. However, the size of the marginal effect may be sufficiently small that an overall effect would be detectable only for interventions producing dramatic reductions in LOS and having no compensatory effect on readmission. This would explain our related finding that home treatment at the time of discharge has no apparent effect on readmission despite its being associated with a 4-day reduction in LOS (Tulloch et al. 2014). More generally, this finding raises the possibility of a trade-off between LOS and readmission with greater LOS promoting stability and a reduced risk of early readmission. Certainly, there is some evidence from the USA that reduction of already shorter psychiatric admissions may be associated with increased readmission (Figueroa et al. 2004), although most studies have found no such relationship (Durbin et al. 2007).
We suspect that the apparently protective effect of being detained under Section 3 or a forensic section of the Mental Health Act may reflect a related effect – someone released from hospital at a particular LOS and who has been detained is likely to be more fully recovered than someone released at the same LOS but who has not been so detained. Alternatively, it may perhaps reflect some effect of the use of Section 17 extended leave from hospital in this group – this provision allows for the recall of a released patient if, for example, they do not continue to take medication, and may help to promote adherence in the early period after release.
The effect of number of previous discharges was in line with previous research, suggesting that this factor reflects some underlying propensity to readmission not measured by other variables.
HoNOS symptoms and behaviour
Finally, in line with the original ambitions of the study, we found evidence of an effect of some specific symptoms and behaviours as measured by HoNOS scale scores collected as part of the Trust's routine outcome measurement programme. Aggressive and disturbed behaviour in particular appeared to be associated with a heightened risk of early readmission, and a similar effect was observed for delusions and hallucinations at the time of discharge. These effects were observed in both the Cox and the logistic regression. We suggest that they represent direct influences of symptoms and behaviour on clinical practice, with those who continue to be actively psychotic and/or disturbed after discharge being more likely to be readmitted.
Although these results may seem intuitively correct, they contrast with the results of two previous, smaller Australian studies. The first – which studied readmission in 1177 patients admitted to a single hospital – found no relationship with either the total score at admission or with each of several individual item scores that were tested (Byrne et al. 2010). The second, which compared 222 readmitted patients with 253 non-readmitted patients found no association between total HoNOS score and readmission, but did not examine associations with individual HoNOS item scores (Callaly et al. 2011). A third Australian study found the same relationships with the aggressive and disturbed behaviour item and the cognitive problems item as we did, and also found a relationship with the total HoNOS score, but this was based on a very small sample (N = 53) (Parker et al. 2002) and it is possible that the agreement with our results could have arisen by chance.
Implications
Despite the statistical significance of the effects included, the logistic regression model had only modest ability to discriminate between those who were readmitted and those who were not, presumably reflecting the influence on readmission of a large number of unmeasured and probably immeasurable factors, many of them varying over time. How beneficial such a model could be depends on the practical use to which it is put. Conceivably, being able to define a higher risk stratum for readmission could help in developing and testing new interventions intended to reduce readmission. If such an intervention is developed, a predictive tool could help in targeting that intervention at those who are most likely to benefit. Of note, it does not appear from the present study or the earlier related study (Tulloch et al. 2014) that such interventions would include facilitated discharge by Home Treatment Teams.
Our findings also suggest some specific situations where particular clinical attention may yield the benefit of reduced readmission. Clinicians responsible for inpatients, it appears, would be well advised to address unresolved psychotic symptoms or continuing disturbed or agitated behaviour.
Certainly, there is scope for further research. Firstly, as new data accrue in our repository we plan to validate the predictive model based on these – this will be facilitated by the increasing completeness of HoNOS item scores necessitated by the development of payment mechanisms in English psychiatric services. A second potential role for further research will be to further examine the role of personality in early readmission – this appeared to be important, but we know very little about the methods and practices by which a diagnosis of personality disorder come to be recorded in the notes, and we also do not know whether it is specific personality traits or a personality disorder diagnosis which are more strongly associated with readmission, or whether the use of structured measurement methods for either would increase the strength of any association. Perhaps most importantly, the question of how LOS impacts on readmission deserves detailed investigation, perhaps using randomisation to slightly longer or shorter LOS to ensure that its causal effect is estimated without bias, and using mediation analysis to test the extent to which any effect is due to improvement in psychotic and disturbed behaviours prior to discharge.
Acknowledgements
The authors are pleased to acknowledge the support of colleagues at the NIHR Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and Institute of Kings College London.
Financial Support
All authors are financially supported by the NIHR Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and Institute of Psychiatry, Kings College London. The study used NIHR Biomedical Research Centre infrastructure funded by NIHR and the Guy's and St. Thomas’ Hospital Trustees. ADT is also supported by an NIHR Health Services Delivery Research project grant (11/1015/20). GT is also funded by a NIHR Applied Research Programme (RP-PG-0606–1053). However, the study did not form part of any specifically funded programme of work. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflict of Interest
None.
Ethical Standards
No ethical approval was required as the analyses were based on fully anonymised data.
References
- van Buuren S, Boshuizen HC, Knook DL (1999). Multiple imputation of missing blood pressure covariates in survival analysis. Statistics in Medicine 18, 681–694. [DOI] [PubMed] [Google Scholar]
- Byrne SL, Hooke GR, Page AC (2010). Readmission: a useful indicator of the quality of inpatient psychiatric care. Journal of Affective Disorders 126, 206–213. [DOI] [PubMed] [Google Scholar]
- Callaly T, Trauer T, Hyland M, Coombs T, Berk M (2011). An examination of risk factors for readmission to acute adult mental health services within 28 days of discharge in the Australian setting. Australasian Psychiatry 19, 221–225. [DOI] [PubMed] [Google Scholar]
- Carr VJ, Lewin TJ, Sly KA, Conrad AM, Tirupati S, Cohen M, Ward PB, Coombs T (2008). Adverse incidents in acute psychiatric inpatient units: rates, correlates and pressures. The Australian and New Zealand Journal of Psychiatry 42, 267–282. [DOI] [PubMed] [Google Scholar]
- Clements KM, Murphy JM, Eisen SV, Normand S-LT (2006). Comparison of self-report and clinician-rated measures of psychiatric symptoms and functioning in predicting 1-year hospital readmission. Administration and Policy in Mental Health and Mental Health Services Research 33, 568–577. [DOI] [PubMed] [Google Scholar]
- Durbin J, Lin E, Layne C, Teed M (2007). Is readmission a valid indicator of the quality of inpatient psychiatric care? The Journal of Behavioral Health Services & Research 34, 137–150. [DOI] [PubMed] [Google Scholar]
- Figueroa R, Harman J, Engberg J (2004). Use of claims data to examine the impact of length of inpatient psychiatric stay on readmission rate. Psychiatric Services 55, 560–565. [DOI] [PubMed] [Google Scholar]
- Heggestad T (2001). Operating conditions of psychiatric hospitals and early readmission — effects of high patient turnover. Acta Psychiatrica Scandinavica 103, 196–202. [DOI] [PubMed] [Google Scholar]
- Heggestad T, Lilleeng SE, Ruud T (2011). Patterns of mental health care utilisation: distribution of services and its predictability from routine data. Social Psychiatry and Psychiatric Epidemiology 46, 1275–1282. [DOI] [PubMed] [Google Scholar]
- Hendryx MS, Moore R, Leeper T, Reynolds M, Davis S (2001). An examination of methods for risk-adjustment of rehospitalization rates. Mental Health Services Research 3, 15–24. [DOI] [PubMed] [Google Scholar]
- Hendryx MS, Russo JE, Stegner B, Dyck DG, Ries RK, Roy-Byrne P (2003). Predicting rehospitalization and outpatient services from administration and clinical databases. The Journal of Behavioral Health Services & Research 30, 342–351. [DOI] [PubMed] [Google Scholar]
- Hodgson RE, Lewis M, Boardman AP (2001). Prediction of readmission to acute psychiatric units. Social Psychiatry and Psychiatric Epidemiology 36, 304–309. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S (1980). Goodness of fit tests for the multiple logistic regression model. Communications in Statistics – Theory and Methods 9, 1043–1069. [Google Scholar]
- Hosmer DW, Lemeshow S, May S (2008). Applied Survival Analysis: Regression Modeling of Time-to-Event Data. John Wiley & Sons: Hoboken, New Jersey. [Google Scholar]
- Kind AJH, Smith MA, Frytak JR, Finch MD (2007a). Bouncing back: patterns and predictors of complicated transitions 30 days after hospitalization for acute ischemic stroke. Journal of the American Geriatrics Society 55, 365–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind AJH, Smith MA, Pandhi N, Frytak JR, Finch MD (2007b). Bouncing-back: rehospitalization in patients with complicated transitions in the first thirty days after hospital discharge for acute stroke. Home Health Care Services Quarterly 26, 37–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind AJH, Smith MA, Liou J-I, Pandhi N, Frytak JR, Finch MD (2008). The price of bouncing back: one-year mortality and payments for acute stroke patients with 30-day bounce-backs. Journal of the American Geriatrics Society 56, 999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind AJH, Smith MA, Liou J-I, Pandhi N, Frytak JR, Finch MD (2010). Discharge destination's effect on bounce-back risk in Black, White, and Hispanic acute ischemic stroke patients. Archives of Physical Medicine and Rehabilitation 91, 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinkenberg WD, Calsyn RJ (1996). Predictors of receipt of aftercare and recidivism among persons with severe mental illness: a review. Psychiatric Services 47, 487–496. [DOI] [PubMed] [Google Scholar]
- Korkeila JA, Lehtinen V, Tuori T, Helenius H (1998). Frequently hospitalised psychiatric patients: a study of predictive factors. Social Psychiatry and Psychiatric Epidemiology 33, 528–534. [DOI] [PubMed] [Google Scholar]
- Mangalore R, Knapp M (2007). Cost of schizophrenia in England. The Journal of Mental Health Policy and Economics 10, 23–41. [PubMed] [Google Scholar]
- Mellesdal L, Mehlum L, Wentzel-Larsen T, Kroken R, Arild Jorgensen H (2010). Suicide risk and acute psychiatric readmissions: a Prospective Cohort Study. Psychiatric Services 61, 25–31. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Nicholson RA, Neesmith DH (1997). Factors affecting relapse in patients discharged from a public hospital: results from survival analysis. The Psychiatric Quarterly 68, 117–129. [DOI] [PubMed] [Google Scholar]
- Moran PW, Doerfler LA, Scherz J, Lish JD (2000). Rehospitalization of psychiatric patients in a managed care environment. Mental Health Services Research 2, 191–198. [Google Scholar]
- NHS National Services Scotland (2009). SPARRA Mental Disorder: Scottish Patients at Risk of Readmission and Admission (to psychiatric hospitals or units). A report on the development of SPARRA MD and recommendations for its use. January. Information Services Division.
- Nuffield Trust (2011). Predictive Risk and Health Care: An Overview. Nuffield Trust: London. [Google Scholar]
- OECD (2011). Health at a Glance 2011: OECD Indicators. OECD Publishing: Paris. [Google Scholar]
- Parker G, O'Donnell M, Hadzi-Pavlovic D, Proberts M (2002). Assessing outcome in community mental health patients: a comparative analysis of measures. International Journal of Social Psychiatry 48, 11–19. [DOI] [PubMed] [Google Scholar]
- Paul P, Pennell ML, Lemeshow S (2013). Standardizing the power of the Hosmer–Lemeshow goodness of fit test in large data sets. Statistics in Medicine 32, 67–80. [DOI] [PubMed] [Google Scholar]
- Royston P (2004). Multiple imputation of missing values. Stata Journal 4, 227–241. [Google Scholar]
- Royston P, Sauerbrei W (2008). Multivariable Model-Building: A Pragmatic Approach to Regression Analysis Based on Fractional Polynomials for Modelling Continuous Variables. John Wiley & Sons: Chichester. [Google Scholar]
- Rubin DB (1987). Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons: New York. [Google Scholar]
- Russo J, Roy-Byrne P, Jaffe C, Ries R, Dagadakis C, Avery D (1997). Psychiatric status, quality of life, and level of care as predictors of outcomes of acute inpatient treatment. Psychiatric Services 48, 1427–1434. [DOI] [PubMed] [Google Scholar]
- Schoenbaum SC, Cookson D, Stelovich S (1995). Postdischarge follow-up of psychiatric inpatients and readmission in an HMO setting. Psychiatric Services 46, 943–945. [DOI] [PubMed] [Google Scholar]
- Sherman FT (2009). Rehospitalizations: packaging discharge and transition services to prevent ‘bounce backs’. Geriatrics 64, 8–9. [PubMed] [Google Scholar]
- Stewart R, Soremekun M, Perera G, Broadbent M, Callard F, Denis M, Hotopf M, Thornicroft G, Lovestone S (2009). The South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLAM BRC) case register: development and descriptive data. BMC Psychiatry 9, 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sytema S, Burgess P (1999). Continuity of care and readmission in two service systems: a comparative Victorian and Groningen case-register study. Acta Psychiatrica Scandinavica 100, 212–219. [DOI] [PubMed] [Google Scholar]
- Thompson EE, Neighbors HW, Munday C, Trierweiler S (2003). Length of stay, referral to aftercare, and rehospitalization among psychiatric inpatients. Psychiatric Services 54, 1271–1276. [DOI] [PubMed] [Google Scholar]
- Tjur T (2009). Coefficients of determination in logistic regression models—a new proposal: the coefficient of discrimination. The American Statistician 63, 366–372. [Google Scholar]
- Tulloch AD, Khondoker MR, Thornicroft G, David AS (2014). Home treatment teams and facilitated discharge from psychiatric hospital. Epidemiology and Psychiatric Sciences 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valevski A, Olfson M, Weizman A, Shiloh R (2007). Risk of readmission in compulsorily and voluntarily admitted patients. Social Psychiatry and Psychiatric Epidemiology 42, 916–922. [DOI] [PubMed] [Google Scholar]
- Vigod S, Kurdyak P, Dennis C-L, Leszcz T, Taylor V, Blumberger D, Seitz D (2013). Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. British Journal of Psychiatry 202, 187–194. [DOI] [PubMed] [Google Scholar]
- Wheeler A, Moyle S, Jansen C, Robinson E, Vanderpyl J (2011). Five-year follow-up of an acute psychiatric admission cohort in Auckland, New Zealand. New Zealand Medical Journal 124, 30–8. [PubMed] [Google Scholar]
- Wing JK, Beevor A, Curtis R, Park S, Hadden S, Burns A (1998). Health of the Nation Outcome Scales (HoNOS). Research and development. British Journal of Psychiatry 172, 11–18. [DOI] [PubMed] [Google Scholar]
- Zilber N, Hornik-Lurie T, Lerner Y (2011). Predictors of early psychiatric rehospitalization: a national case register study. Israel Journal of Psychiatry and Related Sciences 48, 49–53. [PubMed] [Google Scholar]