Abstract
Teledermatology is one of the most important and commonly employed subsets of telemedicine, a special alternative to face-to-face (FTF) doctor--patient consultation that refers to the use of electronic telecommunication tools to facilitate the provision of healthcare between the “seeker” and “provider.” It is used for consultation, education, second opinion, and monitoring medical conditions. This article will review basic concepts, the integration of noninvasive imaging technique images, artificial intelligence, and the current ethical and legal issues.
Keywords: Artificial intelligence, internet, machine learning, real-Time video consultation, skin cancer, social media, store and forward, teledermatology, teledermoscopy, telemedicine
Introduction
Teledermatology (TD) is a subspecialty of dermatology that uses the information and communications technologies to diagnose, monitor, treat, prevent, research, and educate over a distance.[1] It was probably first meant for rural communities or soldiers in faraway lands that had none or little access to physicians; the first innuendo of telemedicine was via phone calls in “The Radio Doctor–Maybe”![2] and it was first fantasied by Hugh Gernsback and his “teledactyl.”[3] Nowadays, it is revolutionizing our understanding of medicine, facing doctors with new standards, and putting all actors in need of rethinking their new role in medicine.[4]
Types of Teledermatology Models
In TD, its categories are based on the nature of the actors involved[5] [Figure 1]. These are:
Figure 1.
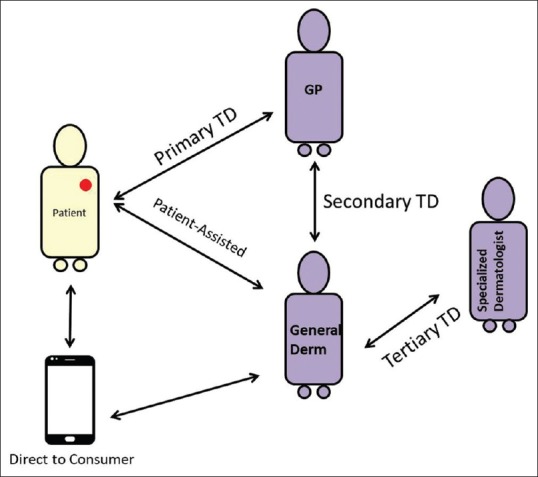
Types of Teledermatology models
Primary TD, which refers to the direct communication between the patient (PT) and the general practitioners (GP)/nurse or dermatologist. It provides a direct service for initial diagnosis and referral
Secondary TD refers to indirect communication between the patient and specialist. PT (seeker) goes to a nurse/GP who then communicates to specialist (provider) to receive advice. Other possible “intermediaries” are health insurance companies and healthcare institutions (nursing homes, emergency departments, or pharmacies)
Tertiary TD refers to “second” opinion among specialists (dermatologist) and a dermatologist with a particular specialization. It is a specialist-to-specialist consult (i.e., dermatologist to pathologist or dermatologist to specialists in confocal microscopy)
Patient Assisted: PT communicates with a healthcare professional, usually for follow-up or monitoring of skin conditions. It can be used, for example, for monitoring a medication scheme or for wound care
Direct to Consumer: PT initiates the care by accessing a healthcare provider through personal devices (smartphone, laptop, or tablet).
Delivery Modalities
TD can be delivered through several modalities.[6]
(1) Real-Time (RT) Video Consultation (Live Interactive): employs live video conferencing. It has the advantage of allowing the provider to ask clarifying questions, which often tip off the seeker. Disadvantages include more time consumption, logistics of differential time zones of the actors, dependence on quality of connectivity (internet speed), and image quality being relatively inferior to static ones
(2) Asynchronous Store-and-Forward (SAF). Clinical, dermoscopic, and other specialized images are sent for consultation. The provider responds at a convenient time. Compared to RT, the advantages of SAF are better image quality and inconsequentiality of time zone. Immediate clarifying questions are not possible but can be undertaken on a second communication. Images and clinical data are sent via computers, laptops, tablets, or smartphones to designated portals (public or private) or apps
(3) Hybrid. Combines the abovementioned modalities.
Reaching the underserved population and urban TD
The dermatologic needs of many communities are underserved.[7] This inaccessibility is influenced by many factors. In the United States (US), the shortage of dermatologic services has resulted in lengthy wait times for in-person evaluations,[8,9] a challenge exacerbated for Medicaid and uninsured patients.[10,11] TD has shown to be cost-effective and decreases wait times and in-person referrals.[12,13,14,15]
TD was described in 1995 as a mechanism for providing care to the underserved populations in rural Oregon, US.[16] Scott et al. reported successful use of telemedicine to provide dermatologic care to three groups of underserved populations.[17] This TD network supported e-mail and transfer of patient-based medical data, access to medical data bases, teleconferencing, quality assurance programs, biomedical repair guidance, continuing health professional education program, and community and patient-oriented health programs.[18] Caroline et al. determined the impact of SAF TD on the delivery of dermatological care with 77% of consults managed with TD alone. This supports its use in unburdening overstretched healthcare resources.[12,14,15] The median time to consult completion was 14 h, which was considerably shorter than wait times for face-to-face (FTF) evaluations.[9] Another study showed that implementing dermoscopy in TD practice for large scale outpatient settings aids in identification and treatment of skin cancers among medically underserved patients.[19] Before implementation of TD the median wait time was of 77 days as opposed to 28 days. TD was proven to be effective at reducing referrals and wait time.
Urban teledermatology
Urban TD (UTD) refers to the TD procedure where both the patient and specialist live in the same city or an urban area.[20] In contrast to TD for underserved populations where distance and lack of specialists are the main factors, in urban settings the difficulty in access is mainly determined by the population density of the city and the time and cost for a patient to reach the doctor's office. The latter is further aggravated for elderly patients. UTD assumes great importance as a feasible mode to break the barriers of disability, which is even more important nowadays due to progressive aging of the population.[21] Its success and rapid growth can be explained by the easy accessibility of various modes of telecommunication using internet which tends to be greater in large cities. In Spain, for example, the number of centers that practice UTD have tripled from 2009 to 2014.[21] A similar increase of UTD was also described in the US where UTD use is greater than TD for rural areas from 2012 onwards in some of their programs.[6,22]
Indian perspective
The dermatologist community in India is clustered in and around urban areas, limiting access to specialists for many patients in rural locations, which is further complicated owing to limited means of communication and transportation.[23] Under the GRAMSTAT (Satellite communication-based technology for rural India) program, the Indian Space Research Organization (ISRO) has initiated several telemedicine pilot projects in 2001 specific to the needs of rural India.[24] A study revealed 81% cost saving in the Chamarajnagar district hospital, Karnataka using this technology.[25] Skin camps are organized by mounting SATCOM on a bus that travels to the remote geographical regions and establish satellite network connectivity with a tertiary center to deliver dermatology care. TD could be used in national health programs to screen or triage melanoma, pigmented skin lesions, leprosy and endemic cases like leishmaniasis.[25] An increased collaboration between dermatologists and primary healthcare providers is required in order to address high patient demand and to provide education and support.[26]
Pre requisite for teledermatology
Landow S.[14] summarizes the requirements for a successful TD as: (1) image quality; (2) preselection of patients (tumoral conditions are the simplest; nevi evaluation should not exceed 1--2 lesions at most; multiple nevi patients should be excluded; hair conditions are difficult to photograph and diagnose);[27] (3) a dermoscopic image is a requirement for pigmented and tumoral lesions; and (4) an effective culture (from seeker and provider) and infrastructure (internet connectivity) [Table 1].[28,29,30]
Table 1.
The pros and cons of teledermatology
| PROS | CONS | |
|---|---|---|
| Accessibility | Makes specialists reachable to patients in remote areas or on long waiting lists[29] | Dependent on availability of internet and its speed, and patient’s or seeker’s ability to operate the device for photography and capture good quality images |
| Equity | Reduces waiting lists and makes specialized medicine equal for all. It democratizes medicine | |
| Quality | It improves quality by reliance on devices for remote diagnoses | Risk of missing or delay in the diagnosis of incidental skin malignancy[30] |
| Cost Efficiency | Increased number of patients can be attended Patients selected for lesion removal/biopsy can be referred directly to surgical day (Sparing one visit)[31] Around 60-70% of FTF visits are avoided |
FTF – Face-to-face
As with any system, there are pros and cons. One possible con is the lost opportunity to show empathy to the patient, to understand his/her needs, and counsel. In fact, only FTF or synchronous TD give the opportunity to ask questions and retrieve medical and non-medical information from the patient. FTF consultation gives the opportunity to establish an emphatic relation but also the space for prejudices.
TD and noninvasive imaging technologies
Medical photography
A good image is the most basic requirement to make a diagnosis in TD. Blurred/out of focus, color imbalance, insufficient view (close-up, medium, large view), non- inclusion of representative lesions, and incorrect positioning constitute some of the most important limitations that prevent a specialist from making the correct diagnosis. Both the clinical and dermoscopic image need to be of good quality.[31] Often there are field-of-view requirementsthat depend on the type of lesion (single, localized, and generalized) [Table 2].
Table 2.
A simple guide to “field of view” requirements of a good image for correct diagnosis by the provider (specialist)
| Type of lesion | |||
|---|---|---|---|
| Photographic requirement | Single lesion | Localized lesions | Generalized lesions |
| Example | Malignant skin tumor | Herpes Zoster infection | Drug Eruption |
| View | |||
| Close-up | √ | √ | √ |
| Medium View | √ | √ | √ (Not essential) |
| Distant View | Not required | √ (Can aid in determining symmetry/asymmetry) | √ |
Dermoscopy
Teledermoscopy (TDD) involves the use of dermoscopic images.[32] Dermoscopy is probably the most commonly used noninvasive imaging technique for cutaneous diagnosis. It is noninvasive, effective, in vivo, acceptable to the patient, and cost-effective. TDD additionally offers a high educational advantage as GP's gain a new skill.[33] TDD is used mostly in skin cancer triage and monitoring of pigmented lesions triage although its use and impact on diagnosis has been increasing in the context of inflammatory and infectious dermatosis as well as disorders of hair, scalp, and nails.[34] It is ideal to include two dermoscopic images: A far view which includes the scale, a close-up view to see more structure details. Depending on the lesion, the image should be taken using polarized or non-polarized light.[35]
Confocal microscopy and ultrasound
Reflectance confocal microscopy (RCM) enables diagnosing of skin conditions with improved diagnostic accuracy and in a noninvasive manner. The learning curve is slow and obtaining confocal images for diagnosing at a distance by an expert can be of benefit to patients.
As more RCM equipment are becoming available and learning to read images correctly requires experience, tele-confocal becomes an alternative.[36] With the development of mobile RCM units, this possibility will become more feasible.
Mobile ultrasound units are already available in the market. Although there are still not enough studies available, the possibility to send high frequency ultrasound images exists.[37] In a near future, there will be units that can be attached to smartphones.
The clinical, dermoscopic, ultrasound, and/or confocal images give information in regard to diagnosis as well as volume and shape[38] and simplify allocating patients to surgery.
TD and skin cancer triage
TD has become a routine procedure for skin cancer triage in many healthcare settings.[39,40] It has yielded favorable results in terms of shortening waiting lists to first dermatologist consultation, preventing unnecessary referrals to F-to-F skin cancer clinics, in diagnostic performance, and cost-effectiveness of skin cancer screening.[41]
Regarding accessibility to skin cancer units mean waiting intervals to the first dermatological consultations have ranged between 2 and 50 days for TD systems versus the 88 to 137 days demonstrated by the conventional letter referral in different studies. Clinic-based evaluations avoided have also being about 50% of patients managed with no need to be referred for in-person visits.[42]
As for diagnostic accuracy, studies available have also calculated concordances ranging from 51% to 85% agreement between F-to-F dermatologists and store-and-forward dermatologists.[42]
Moreover, after more than one decade of TD-based skin cancer screening programs, TD has even shown benefits in terms of proxy healthcare outcomes. The Breslow thickness in patients who had malignant melanoma managed through TD was significantly thinner than in patients whose referrals were conventionally managed.[43]
TDD involves the use of dermoscopic images for remote consultation and decision-making. At conventional in-person consultations, dermoscopy has notably improved the sensitivity and specificity of diagnosing cutaneous lesions.[44] Whether the addition of dermoscopic images to clinical teleconsultations is of utility for remote internet-based skin cancer screening has been a research question recently addressed in experimental studies. A recent randomized clinical trial assessed the diagnostic performance and cost-effectiveness of clinical teleconsultations versus clinical with dermoscopic teleconsultations.[45] In this trial, dermoscopic images improved the diagnostic performance, efficacy, and cost-effectiveness of a store-and-forward TD-based screening system for skin cancer based exclusively on clinical images. The respective diagnostic sensitivity and specificity of purely clinical teleconsultations (86.57% and 72.33%) were improved to 92.86% and 96.24% respectively with addition of TDD. Correct decisions were made in 94.30% of patients through clinical and dermoscopic teleconsultations and in 79.20% of non-dermoscopic teleconsultations. The cost-effectiveness analysis showed TDD as the dominant strategy, with a lower cost-effectiveness ratio (65.13 vs. 80.84).[46]
In relation to this trial, a sensitivity and specificity over 90% are outstanding results for a skin cancer screening system. This high sensitivity, along with an equally good specificity, meaningfully improved making referral decisions and consequently the proportion of correct decisions.
The results of this trial confirm that TDD offers advantages over TD using clinical images alone for routine large-scale screening of patients with skin cancer.[46] Furthermore, the strong evidence provided by this trial, along with the health outcomes achieved by TD in skin cancer patients, may help to prompt policymakers to decide in favor of the implementation and spread of telemedicine programs for skin cancer screening based on clinical and dermoscopic images.
Teledermatology and education
In addition to the obvious role in patient management, TD plays an integral function in education.
Possibilities are multifold including resident training, exchange of knowledge and opinion between different dermatologists, learning of dermatological diseases from different parts of the world, training of other medical specialties for basic dermatological conditions, organization of cost-effective TD-based conferences for learning at a global scale.
Doctors can increase their pool of knowledge without missing out on patient management thanks to the various platforms for mass education like podcasts and webinars.[46]
Dermatology training will be greatly impacted with the advancement and integration of TD in resident training curriculum. Nowadays with ease in transportation, the divide between dermatoses of developing and developing worlds is getting blurred and dermatologists all over the world must be fully equipped to deal with a wider variety of disorders. Various reports exist necessitating the need for global educations and dermatologists over different parts of the world have felt the need to undergo additional training to deal with illnesses typically not encountered in their native population of patients.[47,48,49]
Knowledge of unusual dermatoses in a particular geographical area is only possible via TD case-based learning. Studies have shown that dermatology residents feel more confident at handling various disorders with additional TD learning.[50,51]
Not only is TD a valuable asset for distant learning, studies have reported that respondents undergoing TD e-learning have also reported improvement in their interpersonal and communication skills, such as understanding cultural and ethical issues in skin health, learning more about social issues in international settings, and gaining more confidence in dealing with communities from different cultural backgrounds.[7,8,9,10,52,53,54,55]
There is a growing need for integration of TD training in resident curriculum and many international centers have already incorporated this mode of learning.[56,57] TD can also be used as a tool to evaluate residents.[58]
TD also connects dermatologists with each other for better exchange of knowledge.[59,60] Various surveys and studies have revealed that TD may also be used as an option to seek opinion and gain knowledge from other dermatologists particularly for challenging cases.[61,62] WhatsApp groups make it possible for dermatologists and other specialties to discuss various dermatological diseases and their appropriate management. It is one of the easiest media to exchange knowledge and experience on a one–on-one basis. It is considered to be one of the safest instant messaging media because of encryption technology.[63]
Enabling GPs and o practitioners of different specialties to deal with dermatological disorders will have a great impact on the overall management and need for referrals for patients with additional cutaneous abnormality.[64,65] TD-based educative learning of rural primary care providers and imaging technicians in a 2-year project showed improvement in their knowledge of cutaneous diagnosis and treatment care plans including basic surgical procedures like biopsies, excisions, and cautery.[66]
Although TD has proven to be a beneficious tool for educational purpose, it may have its set of drawbacks. TD-based learning could reduce the residents’ empathetic nature toward patients and loss of integral approach rather than focusing on single lesions.[67,68]
TD and Artificial Intelligence
There is only one dermatologist for 400,000 people in India; with majority of them are concentrated in urban areas. In many Asian and African countries, the accessibility to dermatologists is similar. For example, Madagascar has 10 dermatologists for 25 million population and Senegal has 80 dermatologists for 1.5 million populations (personal communication with Dr. Rogerdominiquw Randrianarimalala, Madagascar).
The potential answer to such a scenario is artificial intelligence-driven image diagnosis, enabling GPs to make a correct diagnosis by feeding a clinical picture to a mobile application to diagnose common dermatological conditions. In this, a mobile application linked to a central machine at a distant location enriched with image-based diagnostic database (employing internet cloud computing) does the analysis and delivers the probabilities of diagnosis or differential diagnoses to assist the non-dermatologist physician. Unlike human experts dependent TD, which requires days to weeks for background support, the response time in machine analysis ranges from a few seconds to hardly more than a minute, depending on the internet speed and the number of concurrent users. Further, in an improvised TD model, this immediate machine analysis can be supported by human dermatology experts who eventually check and verify the machine diagnosis based on the image and patient data provided by the peripheral non-dermatologist physician.
The current accuracy of a mobile application for common 10 dermatology conditions (developed by Niruthm Lab and All India Institute of Medical Sciences, New Delhi, India) is reasonably good. The mean sensitivity and specificity are around 80% and 50%, respectively.[69] This was developed using custom machine learning algorithms, and pre- and post-processing schemes to get these results. About 12,000 images were collected and annotated for data-set development. A mobile phone application for Android and IOS phones was launched which general physicians can use in clinical settings to augment their disease diagnosis for common 20 dermatological diseases
Several studies have evaluated dermatologist-level performance of AI-driven image diagnosis technology for skin cancers.[70,71] Among other studies, one focusing on dermoscopic images for melanoma image classification demonstrated superiority of machine performance over 147 of 157 dermatologists.[72]
However, the current technology (deep learning) has a bottleneck due to its low specificity for non-skin cancer dermatological diseases (specificity ≅ 50%) and it appears to be not accurate enough to rely on AI-driven image analysis alone for non-skin cancer disease conditions. The physician using such an AI-based diagnostic model should be aware of the limitation of the conditions diagnosable by the model; e.g., if pityriasis rosea is not included in the AI model's database, then a patient with this condition may be misdiagnosed with a totally different albeit morphologically similar-appearing condition (as per the reference images stored in the database) such as psoriasis. To further enhance the diagnostic accuracy of AI-based diagnostic systems, integration of other parameters such as patient datalike site(s) involved, duration, rapidity of onset, relationship to known risk factors such as exposure to sunlight, and extent of the disease is essential.[73] Future roadmap of AI-based cutaneous diagnosis heavily relies on evolution of technology capable of providing a unified diagnosis based on integration of image analysis data with patient-related other data.
Teledermatology and business models
TD as a business model has a good potential because it generates revenue for the work done by the physician or nurse while solving the patient's health issue. Payment for TD can be broadly categorized into: (a) Direct TD (Patient seeks out the dermatologist directly) and (b) Third party TD, involving regulated online platforms. Advantages and disadvantages have been summarized in Table 3.
Table 3.
Advantages and disadvantages of direct versus third party business models for teledermatology
| Advantages | Disadvantages | |
|---|---|---|
| Direct TD |
For the patient: Feeling of immediacy, prompt answer For the HCP: Faster way to answer; closer to patient’s need; easier monitoring |
For the patient: The immediacy can sometimes result in reduced information on the condition and misinterpretation. This is especially relevant for instructions of medication. For the HCP: Patient may find it too convenient to directly contact the doctor and may trouble the doctor too frequently and often for trivial concerns. Revenue is not always guaranteed |
| Third party TD | For the patient: clear instructions on uploading images and giving required medical information. | For the patient: requires connecting to an app. The app needs to be friendly user |
| The fees are fixed and posted in advance. The patient’s data is secured on a reliable server |
For the HCP: Some third party platforms retain a high percentage of the revenue, leaving to the HCP a very low fee. | |
| For the HCP: | ||
| Revenue is guaranteed. Better control on cases answered. The HCP fixes the time to answer (S&F TD) always within a reasonable time period (24 h) Payment is guaranteed before the answer is sent |
HCP – Health care practitioner; TD – Teledermatology
Keeping the above aspects in mind, it is prudent for a dermatologist to provide TD through a reliable healthcare portal backed by reputed professionals/organization.
Some portals are privately managed by the physician who becomes the service provider himself and therefore become solely responsible. Others are run by third parties and might offer a list of various dermatologists on their panel. The patient needs to know at all times that there is a person or group available and responsible for the medical advice.
There are different business models worldwide that involve a variety of payment structures. For instance, the public national health system in Spain, rated the most efficient in Europe and the third top model in the world-[74] pays per TD directly to the hospital that responds to the need for a TD consultation; in the Netherlands, the specialist is payed per consultation. Off late, results of studies on provider's expectations have expectedly started getting published.[75]
Medicolegal aspects in India
Despite the concept of telemedicine (TM) being recognized and defined by the World Health Organization (WHO) and its global fanning, there is no definite legislation that singularly deals with the practice of TM in India; for that matter, nor in majority of countries.
Presumptively, since TM represents amalgamation of the practice of medicine with information technology, all the existing laws relating to both “medicine” and “information technology” in India should apply to TM.
The instructions issued by the end-point health care practitioner (HCP) through TD should satisfy the requirements of being in writing and counter-signed by a registered medical practitioner (RMP), in accordance with the Drugs and Cosmetic Rules 1945, without which, the prescription will be invalid in the eyes of the law.
Logically, TM would also be governed by the Information Technology Act, 2000 despite the absence of direct relation of this Act with the provision of healthcare services by using information technology. This includes issues related to security, privacy and confidentiality of patient data and potential misuse and even abuse of electronic records in the form of unauthorized interception and/or disclosure warrant deliberation.[76]
Recommended guidelines and standards for practice of telemedicine in India
Although binding laws remain elusive, the Department of Information Technology, Ministry of Communications and Information Technology had issued Guidelines and Standards for Practice of Telemedicine in India in May, 2003. While the clauses are not binding, it is advisable to follow them to preempt a future medicolegal complication arising in an odd case.[70]
The Guidelines recommend that each healthcare provider should have a unique provider identifier which will flow to all its programs and telemedicine consultation centers (“TCC”). Each of the TM specialty centers (“TSC”) and TCCs are also recommended to have a separate unique and universal identifier code. It is further recommended that each patient also be identified by a unique and universal patient identifier so that one central patient information record can be assimilated, comprehensive medical databases can be built, or if the patient wants, he/she can move across multiple providers without losing data.[70]
The Guidelines also spell out the hardware and software (including detailed configuration and specifications) which is recommended for the setting up of the TCC and TSCs. In the absence of a legislation governing TM, it is suggested that the machinery and equipment of the vendor complies with the specifications given in the Guidelines so as to dilute potential liability issues at a later stage.
Strategies to protect the privacy and maintain patients’ discreetness are essential. Issues such as who can access the individual's health information, technology used for authentication, coding and encryption for storage of patient data and for transmitting medical information must be in-built in any TM or TD-based consultation system.[77] Although, no TM malpractice cases have been filed to date, clarifying how responsibility for decision-making is shared between referring doctors and specialists is essential.
There are various suggested approaches for practitioners of TM and TD to safeguard their position, which may be found in more details elsewhere.[71] Most importantly, the HCP should never hesitate in suggesting essential investigations (irrespective of patient's monetary or logistic power to get them done) and one should always use a disclaimer, such as “This is a Teledermatology-based follow-up advice being given to an off-shore patient, sought actively by him/her. The advice has been given based on the relatively limited understanding of the patient's condition by the doctor from the teledermatology conversation with the patient, and with the doctor's best intent to help the patient within probable and feasible means. No kind of consultation can ever match that of a direct physical patient-to-doctor consultation. The investigations and treatments suggested suffer from standard limitations of Teledermatology, and any adverse outcome [lack of improvement/reaction to a suggested medicine/other problems] arising out of the above suggestions shall not be the responsibility of the suggesting doctor. The whole teledermatology-based advice is not a treatment in itself, rather a sincere attempt on part of the doctor, to facilitate the treatment of a patient seeking for it, owing to reasons best understood and known to the patient.”
Conclusion
TD is the future of the practice of dermatology. Although it cannot substitute traditional medicine, it represents the sole way of managing populations that are getting more numerous and older. With a stagnant number of dermatologists worldwide and their skewed urban clustering, a FTF consultation with each patient will not be possible. TD offers the opportunity to democratize health delivery. The evidence to date supports the accuracy and cost-effectiveness of TD as well as its ability to facilitate and expedite medical attention.[78] With the implementation of AIthe landscape of conventional modes of TD is expected to change susbstantially in coming years. Triage will be done by software and physicians will engage in FTF consultation for only those patients who really need personalized care. The future is here. As Dr Anne Burdick aptly stated, “The teledermatology train is coming: Get on board, get out of the way, or get run over.”[79]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Coates SJ, Kvedar J, Granstein RD. Teledermatology: From historical perspective to emerging techniques of the modern era: Part I: History, rationale, and current practice. J Am Acad Dermatol. 2015;72:563–74. doi: 10.1016/j.jaad.2014.07.061. [DOI] [PubMed] [Google Scholar]
- 2.Lafolla T. History of Telemedicine Infographic [Internet] [Last cited on 2019 May 10]. Available from: https://blog.evisit.com/history-telemedicine-infographic .
- 3.Fenston J. Telemedicine: Adventures in time and space [Internet] [Last cited on 2019 May 10]. Available from: https://www.kbia.org/post/telemedicine-adventures-time-and-space#stream/0 .
- 4.Bashshur RL, Gates M, Shannon GW, Kvedar JC, Tejasvi T. The Empirical foundations of teledermatology: A review of the research evidence. Telemed J E Health. 2015;21:953–79. doi: 10.1089/tmj.2015.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tensen E, van der Heijden JP, Jaspers MWM, Witkamp L. Two decades of teledermatology: Current status and integration in national healthcare systems. Curr Dermatol Rep. 2016;5:96–104. doi: 10.1007/s13671-016-0136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armstrong AW, Wu J, Kovarik CL, Goldyne ME, Oh DH, McKoy KC, et al. State of teledermatology programs in the United States. J Am Acad Dermatol. 2012;67:939–44. doi: 10.1016/j.jaad.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Dermatology. Fresh look at the management of skin diseases in the tropics. Int J Dermatol. 1990;29:413–5. doi: 10.1111/j.1365-4362.1990.tb03823.x. [DOI] [PubMed] [Google Scholar]
- 8.Tsang MW, Resneck JS., Jr Even patients with changing moles face long dermatology appointment wait-times: A study of simulated patient calls to dermatologists. J Am Acad Dermatol. 2006;55:54–8. doi: 10.1016/j.jaad.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Kimball AB, Resneck JS., Jr The US dermatology work force: A speciality remains in shortage. J Am Acad Dermatol. 2008;59:741–5. doi: 10.1016/j.jaad.2008.06.037. [DOI] [PubMed] [Google Scholar]
- 10.Resneck JS, Jr, Pletcher MJ, Lozano N. Medicare, medicaid and access to dermatologists: The effect of patient insurance on appointment access and wait times. J Am Acad Dermatol. 2004;50:85–92. doi: 10.1016/s0190-9622(03)02463-0. [DOI] [PubMed] [Google Scholar]
- 11.Resneck JS, Jr, Isenstein A, Kimball AB. Few medicais and uninsured patients are accessing dermatologists. J Am Acad Dermatol. 2006;55:1084–8. doi: 10.1016/j.jaad.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 12.van der Heijden JP, de Keizer NF, Bos JD, Spuls PI, Witkamp L. Teledermatology applied following patient selection by general practitioners in daily practice improves efficiency and quality of care at lower cost. Br J Dermatol. 2011;165:1058–65. doi: 10.1111/j.1365-2133.2011.10509.x. [DOI] [PubMed] [Google Scholar]
- 13.Kahn E, Sossong S, Goh A, Carpenter D, Goldstein S. Evaluation of skin cancer in Northern California Kaiser Permanente's store and forward teledermatology referral programme. Telemed J E Health. 2013;19:780–5. doi: 10.1089/tmj.2012.0260. [DOI] [PubMed] [Google Scholar]
- 14.Landow SM, Mateus A, Korgavkar K, Nightingale D, Weinstock MA. Teledermatology: Key factors associated with reducing face-to face dermatology visits. J Am Acad Dermatol. 2014;71:570–6. doi: 10.1016/j.jaad.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 15.McGoey ST, Oakley A, Rademaker M. Waikato teledermatology: A pilot project for improving access in New Zealand. J Telemed Telecare. 2015;21:414–9. doi: 10.1177/1357633X15583216. [DOI] [PubMed] [Google Scholar]
- 16.Perednia DA. Teledermatology: One application of telemedicine. Bull Med Libr Assoc. 1995;83:42–7. [PMC free article] [PubMed] [Google Scholar]
- 17.Norton SA, Burdick AE, Philips CM, Berman B. Teledermatology and underserved populations. Arch Dermatol. 1997;133:197–200. [PubMed] [Google Scholar]
- 18.Norton SA, Bice SB. Island telegraph: Telemedicine in the Pacific. Presented at the second Mayo telemedicine symposium and second international conference on the medical aspects of telemedicine, Rochester, Minn. 1995 Apr 6; [Google Scholar]
- 19.Naka F, Lu J, Porto A, Villagra J, Wu ZH, Anderson D. Impact of dermatology eConsults on access to care and skin cancer screening in underserved populations: A model for teledermatology services in community health centers. J Am Acad Dermatol. 2018;78:293–302. doi: 10.1016/j.jaad.2017.09.017. [DOI] [PubMed] [Google Scholar]
- 20.Romero-Aguilera G, Ferrandiz L, Moreno-Ramirez D. Urban teledermatology: Concept, advantages and disadvantages. Actas Dermosifiliogr. 2018;109:471–75. doi: 10.1016/j.ad.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 21.Moreno-Ramirez D, Ferrandiz L. A 10 year history of teledermatolgy for skin cancer management. JAMA Dermatol. 151:1289–90. doi: 10.1001/jamadermatol.2015.3208. [DOI] [PubMed] [Google Scholar]
- 22.Landow SM, Oh DH, Weinstock MA. Teledermatology within the veterans health administration, 2002-2014. Telemed J E Health. 2015;21:769–73. doi: 10.1089/tmj.2014.0225. [DOI] [PubMed] [Google Scholar]
- 23.Jayakar T, Parimalam K. The scope of teledermatology in India. Ind Dematol Online J. 2013;4:82–9. doi: 10.4103/2229-5178.110579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sathyamurthy LS, Bhaskaranarayana A. Telemedicine: Indian space agency's (ISRO) initiative for specialty health care delivery to remote and rural population. In: Sathyamurthy LS, Murthy RL, editors. Telemedicine Manual-Guide Book for Practice of Telemedicine. 1st ed. Bangalore: Indian Space Research Organization, Department of space. Government of India; 2005. pp. 9–13. [Google Scholar]
- 25.Kanthraj GR. Newer insights into teledermatology practice. Ind J Dermatol Venereol leprol. 2011;77:276–87. doi: 10.4103/0378-6323.79696. [DOI] [PubMed] [Google Scholar]
- 26.Janjua SA, McColl I, Thomas J. Teledermatology: A step forward. J Pak Assoc Derma. 2005;15:317–9. [Google Scholar]
- 27.McMahon PJ, Winston FK, Perman MJ, Jew OS, O’Connor DM, Castelo-Soccio LA. Diagnostic accuracy of pediatric teledermatology using parent-submitted photographs. JAMA Dermatol. 2017;153:1243–8. doi: 10.1001/jamadermatol.2017.4280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Uscher-Pines L, Malsberger R, Burgette L, Mulcahy A, Mehrotra A. Effect of teledermatology on access to dermatology care among medicaid enrollees. JAMA Dermatol. 2016;152:905–11. doi: 10.1001/jamadermatol.2016.0938. [DOI] [PubMed] [Google Scholar]
- 29.Keleshian V, Ortega-Loayza AG, Tarkington P. Incidental skin malignancies in teledermatology and in-person cohorts in the veterans affairs health system. J Am Acad Dermatol. 2017;77:965–6. doi: 10.1016/j.jaad.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 30.Galdeano R, Moreno-Álvarez P, Moreno-Ramírez D, Ruiz-de-Casas A, Nieto-García A, Ferrándiz L, et al. Teledermatología prequirúrgica en pacientes con cáncer cutáneo no melanoma. Evaluación económica. Actas Dermosifiliogr. 2009;99:795–802. [PubMed] [Google Scholar]
- 31.Pasquali P. Photography in dermatology. In: Baldi A, Pasquali P, Spugnini E, editors. Skin Cancer: A Practical Approach. 1st ed. New York: Springer; 2014. pp. 291–300. [Google Scholar]
- 32.Bleicher B, Levine A, Markowitz O. Going digital with dermoscopy. Cutis. 2018;102:102–5. [PubMed] [Google Scholar]
- 33.Jones OT, Jurascheck LC, Utukuri M, Pannebakker MM, Emery J, Walter FM. Dermoscopy use in UK primary care: A survey of GPs with a special interest in dermatology. J Eur Acad Dermatol Venereol. 2019;33:1706–12. doi: 10.1111/jdv.15614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sonthalia S, Kaliyadan F. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2019. Jan-May. [Last accessed on 2019 May 13]. Dermoscopy Overview and Extradiagnostic Applications. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537131/ [PubMed] [Google Scholar]
- 35.Benvenuto-Andrade C, Dusza SW, Agero AL, Scope A, Rajadhyaksha M, Halpern AC, et al. Differences between polarized light dermoscopy and immersion contact dermoscopy for the evaluation of skin lesions. Arch Dermatol. 2007;143:329–38. doi: 10.1001/archderm.143.3.329. [DOI] [PubMed] [Google Scholar]
- 36.Witkowski A, Łudzik J, Soyer HP. Telediagnosis with confocal microscopy. Dermatol Clin. 2016;34:505–12. doi: 10.1016/j.det.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 37.Alfageme F, Salgüero I, Martinez C, Roustan G. Teleultrasonography for the early diagnosis of HS in the primary care setting. Exp Dermatol. 2019;28:31. [Google Scholar]
- 38.Pasquali P, Camacho E, Fortuño A. Use of 22 MHz high frequency ultrasound in the management of skin cancer. In: Baldi A, Pasquali P, Spugnini E, editors. Skin Cancer A Practical Approach. 1st ed. New York: Springer; 2014. pp. 245–56. [Google Scholar]
- 39.Moreno-Ramírez D, Ferrándiz L. A 10-year history of teledermatology for skin cancer management. JAMA Dermatol. 2015;151:1289–90. doi: 10.1001/jamadermatol.2015.3208. [DOI] [PubMed] [Google Scholar]
- 40.Massone C, Maak D, Hofmann-Wellenhof R, Soyer HP, Freuhauf J. Teledermatology for skin cancer prevention: An experience on 690 Austrian patients. J Eur Acad Dermatol Venereol. 2014;28:1103–8. doi: 10.1111/jdv.12351. [DOI] [PubMed] [Google Scholar]
- 41.Moreno-Ramírez D, Ferrándiz L, Nieto-Garcia A, Carrasco R, Moreno-Alvarez P, Galdeano R, et al. Store-and-forward teledermatology in skin cancer triage: Experience and evaluation of 2009 teleconsultations. Arch Dermatol. 2007;143:479–84. doi: 10.1001/archderm.143.4.479. [DOI] [PubMed] [Google Scholar]
- 42.Finnane A, Dallest K, Janda M, Soyer HP. Teledermatology for the diagnosis and management of skin cancer: A systematic review. JAMA Dermatol. 2017;153:319–27. doi: 10.1001/jamadermatol.2016.4361. [DOI] [PubMed] [Google Scholar]
- 43.Ferrándiz L, Ruiz-de-Casas A, Martin-Gutierrez FJ, Peral-Rubio F, Mendez-Abad C, Rios-Martin JJ, et al. Effect of teledermatology on the prognosis of patients with cutaneous melanoma. Arch Dermatol. 2012;148:1025–8. doi: 10.1001/archdermatol.2012.778. [DOI] [PubMed] [Google Scholar]
- 44.Annessi G, Bono R, Sampogna F, Faraggiana T, Abeni D. Sensitivity, specificity, and diagnostic accuracy of three dermoscopic algorithmic methods in the diagnosis of doubtful melanocytic lesions: The importance of light brown structureless areas in differentiating atypical melanocytic nevi from thin melanomas. J Am Acad Dermatol. 2007;56:759–67. doi: 10.1016/j.jaad.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 45.Ferrándiz L, Ojeda-Vila T, Corrales A, Martín-Gutiérrez FJ, Ruíz-de-Casas A, Galdeano R, et al. Internet-based skin cancer screening using clinical images alone or in conjunction with dermoscopic images: A randomized teledermoscopy trial. J Am Acad Dermatol. 2017;76:676–82. doi: 10.1016/j.jaad.2016.10.041. [DOI] [PubMed] [Google Scholar]
- 46.Benedetto AV. Travel as a teaching and learning tool. Clin Dermatol. 2019;37:29–37. doi: 10.1016/j.clindermatol.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 47.Elsner P. Dermatology in the tropics and in medical missions: Consequences for the training of dermatologists and for continuing medical education. Hautarzt. 2015;66:355–9. doi: 10.1007/s00105-015-3637-6. [DOI] [PubMed] [Google Scholar]
- 48.Izadnegahdar R, Correia S, Ohata B, Kittler A, ter Kuile S, Vaillancourt S, et al. Global health in Canadian medical education: Current practices and opportunities. Acad Med. 2008;83:192–8. doi: 10.1097/ACM.0b013e31816095cd. [DOI] [PubMed] [Google Scholar]
- 49.Pitt MB, Gladding SP, Suchdev PS, Howard CR. Pediatric global health education: Past, present, and future. JAMA Pediatr. 2016;170:78–84. doi: 10.1001/jamapediatrics.2015.2368. [DOI] [PubMed] [Google Scholar]
- 50.Boyers LN, Schultz A, Baceviciene R, Blaney S, Marvi N, Dellavalle RP, et al. Teledermatology as an educational tool for teaching dermatology to residents and medical students. Telemed J E Health. 2015;21:312–4. doi: 10.1089/tmj.2014.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Scheinfeld N. The use of teledermatology to supervise dermatology residents. J Am Acad Dermatol. 2005;52:378–80. doi: 10.1016/j.jaad.2004.07.050. [DOI] [PubMed] [Google Scholar]
- 52.Yeung H, Sargen MR, Luk KM, Berry EG, Gurnee EA, Heuring E, et al. Teledermatology and teledermatopathology as educational tools for international dermatology: A virtual grand rounds pilot curriculum. Int J Dermatol. 2018;57:1358–62. doi: 10.1111/ijd.14014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yao CA, Swanson J, McCullough M, Taro TB, Gutierrez R, Bradshaw A, et al. The medical mission and modern core competency training: A 10-year follow-up of resident experiences in global plastic surgery. Plast Reconstr Surg. 2016;138:531e–8e. doi: 10.1097/PRS.0000000000002484. [DOI] [PubMed] [Google Scholar]
- 54.Battat R, Seidman G, Chadi N, Chanda MY, Nehme J, Hulme J, et al. Global health competencies and approaches in medical education: A literature review. BMC Med Educ. 2010;10:94. doi: 10.1186/1472-6920-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Juarez JA, Marvel K, Brezinski KL, Glazner C, Towbin MM, Lawton S. Bridging the gap: A curriculum to teach residents cultural humility. Fam Med. 2006;38:97–102. [PubMed] [Google Scholar]
- 56.Patel J, Parr K, Buehler-Bota T, Hood AF. Integrating outpatient teledermatology education into the dermatology resident curriculum. J Grad Med Educ. 2016;8:468–9. doi: 10.4300/JGME-D-15-00792.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nelson CA, Wanat KA, Roth RR, James WD, Kovarik CL, Takeshita J. Teledermatology as pedagogy: Diagnostic and management concordance between resident and attending dermatologists. J Am Acad Dermatol. 2015;72:555–7. doi: 10.1016/j.jaad.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wanat KA, Newman S, Finney KM, Kovarik CL, Lee I. Teledermatology education: Current use of teledermatology in US residency programs. J Grad Med Educ. 2016;8:286–7. doi: 10.4300/JGME-D-16-00041.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van der Heijden JP, Spuls PI, Voorbraak FP, de Keizer NF, Witkamp L, Bos JD. Tertiary teledermatology: A systematic review. Telemed J E Health. 2010;16:56–62. doi: 10.1089/tmj.2009.0020. [DOI] [PubMed] [Google Scholar]
- 60.Burg G, Hasse U, Cipolat C, Kropf R, Djamei V, Soyer HP, et al. Teledermatology: Just cool or a real tool? Dermatology. 2005;210:169–73. doi: 10.1159/000082573. [DOI] [PubMed] [Google Scholar]
- 61.Lozzi GP, Soyer HP, Massone C, Micantonio T, Kraenke B, Fargnoli MC, et al. The additive value of second opinion teleconsulting in the management of patients with challenging inflammatory, neoplastic skin diseases: A best practice model in dermatology? J Eur Acad Dermatol Venereol. 2007;21:30–4. doi: 10.1111/j.1468-3083.2006.01846.x. [DOI] [PubMed] [Google Scholar]
- 62.Abbott LM, Magnusson RS, Gibbs E, Smith SD. Smartphone use in dermatology for clinical photography and consultation: Current practice and the law. Australas J Dermatol. 2018;59:101–7. doi: 10.1111/ajd.12583. [DOI] [PubMed] [Google Scholar]
- 63.Hogan SC, van Hees C, Asiedu KB, Fuller LC. WhatsApp platforms in tropical public health resource-poor settings. Int J Dermatol. 2019;58:228–30. doi: 10.1111/ijd.14237. [DOI] [PubMed] [Google Scholar]
- 64.Williams CM, Kedar I, Smith L, Brandling-Bennett HA, Lugn N, Kvedar JC. Teledermatology education for internal medicine residents. J Am Acad Dermatol. 2005;52:1098–9. doi: 10.1016/j.jaad.2005.01.111. [DOI] [PubMed] [Google Scholar]
- 65.Thind CK, Brooker I, Ormerod AD. Teledermatology: A tool for remote supervision of a general practitioner with special interest in dermatology. Clin Exp Dermatol. 2011;36:489–94. doi: 10.1111/j.1365-2230.2011.04073.x. [DOI] [PubMed] [Google Scholar]
- 66.McFarland LV, Raugi GJ, Taylor LL, Reiber GE. Implementation of an education and skills programme in a teledermatology project for rural veterans. J Telemed Telecare. 2012;18:66–71. doi: 10.1258/jtt.2011.110518. [DOI] [PubMed] [Google Scholar]
- 67.Lami M, Malabanan K, McAuliffe O. Teledermatology in medical education-A ‘rash’ decision? Med Educ Online. 2015;20:30576. doi: 10.3402/meo.v20.30576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen K, Lim A, Shumack S. Teledermatology: Influence of zoning and education on a clinician's ability to observe peripheral lesions. Aust J Dermatol. 2002;43:171–4. doi: 10.1046/j.1440-0960.2002.00589.x. [DOI] [PubMed] [Google Scholar]
- 69.Gupta S, Chauhan V, Kumar S, Dixit A, Mathur J. Development of artificial intelligence based mobile application for ten common dermatological diseases. To be presented as oral presentation in 24th World congress of Dermatology, Milan, Italy. 2019 Jun 10-15; [Google Scholar]
- 70.Fujisawa Y, Otomo Y, Ogata Y, Nakamura Y, Fujita R, Ishitsuka Y, et al. Deep-learning-based, computer-aided classifier developed with a small dataset of clinical images surpasses board-certified dermatologists in skin tumour diagnosis. Br J Dermatol. 2019;180:373–81. doi: 10.1111/bjd.16924. [DOI] [PubMed] [Google Scholar]
- 71.Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115–8. doi: 10.1038/nature21056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Brinker TJ, Hekler A, Enk AH, Klode J, Hauschild A, Berking C, et al. Deep learning outperformed 136 of 157 dermatologists in a head-to-head dermoscopic melanoma image classification task. Eur J Cancer. 2019;113:47–54. doi: 10.1016/j.ejca.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 73.Chou WY, Tien PT, Lin FY, Chiu PC. Application of visually based, computerised diagnostic decision support system in dermatological medical education: A pilot study. Postgrad Med J. 2017;93:256–9. doi: 10.1136/postgradmedj-2016-134328. [DOI] [PubMed] [Google Scholar]
- 74.Redacción Médica. España tiene la sanidad más eficiente de Europa y la 3ª mejor del mundo. [Internet] [Last cited on 2019 May 10]. Available from: https://www.redaccionmedica.com/secciones/sanidad-hoy/espanatiene-la-sanidad-mas-eficiente-de-europa-y-la-3-mejor-delmundo-4821 .
- 75.Snoswell CL, Whitty JA, Caffery LJ, Finnane A, Soyer HP. What do Australian dermatologists expect to be paid for store-and-forward teledermoscopy? A preliminary investigation. J Telemed Telecare. 2019;25:438–44. doi: 10.1177/1357633X18776766. [DOI] [PubMed] [Google Scholar]
- 76.International Lawyers Network. LexCounsel Law Offices. Legal Position concerning Telemedicine in India. [Internet] [Last cited on 2019 May 10]. Available from: https://www.ilntoday.com/2014/02/legal-position-concerning-telemedicine-in-india/
- 77.Thomas J, Kumar P. The scope of teledermatology in India. Indian Dermatol Online J. 2013;4:82–9. doi: 10.4103/2229-5178.110579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lee JJ, English JC., 3rd Teledermatology: A review and update. Am J Clin Dermatol. 2018;19:253–60. doi: 10.1007/s40257-017-0317-6. [DOI] [PubMed] [Google Scholar]
- 79.Burdick AE, Simmons SC. The teledermatology train is coming: Get on board, get out of the way, or get run over. Cutis. 2011;88:213–4. [PubMed] [Google Scholar]


