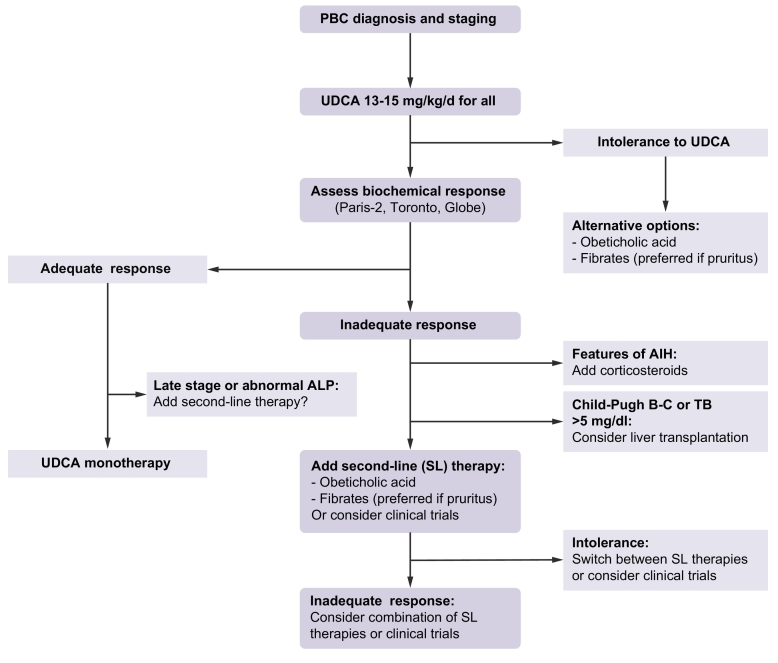
Fig. 1.
Treatment algorithm for PBC.
Initial staging of PBC should preferably be based on non-invasive measures including total bilirubin, ALP, aminotransferases, albumin, platelet count, liver stiffness measurement, and liver ultrasound. All patients must be treated with UDCA as a first-line treatment. Intolerance to UDCA (diarrhoea, stomach burns) may occur rarely (5%). Alternative options (OCA or fibrates) should then be considered. Assessment of biochemical response to UDCA is typically performed at 12 months of UDCA, but earlier evaluation after as few as 6 months of UDCA therapy may be proposed in patients with the most severe or symptomatic (pruritus) disease. The response criteria used must include ALP and bilirubin levels (Paris-2, Toronto, GLOBE, etc.). Abnormal levels of total and conjugated bilirubin or ALP level ≫1.5x ULN are minimal thresholds above which second-line therapies should be considered. Patients with adequate biochemical response to UDCA can be kept on UDCA monotherapy. Advanced-stage responders or those with persisting abnormal ALP might be considered for second-line therapies. In poor biochemical responders, liver biopsy should be considered when AIH-PBC variant or any other hepatic comorbidity is suspected. Addition of corticosteroids (including budesonide) is recommended in patients with AIH-PBC variant. Patients with non-regressive jaundice (bilirubin ≫5 mg/dl) or features of advanced cirrhosis (Child-Pugh B-C) should be referred for liver transplant. All remaining poor responders to UDCA should be considered for second-line therapies (i.e. OCA or fibrates) in addition to continued UDCA. Fibrates should be preferred in patients with pruritus. Second-line therapies could be switched in case of poor tolerance (pruritus for OCA; myalgia for fibrates) or combined in case of insufficient response.
AIH, autoimmune hepatitis; ALP, alkaline phosphatase; OCA, obeticholic acid; PBC, primary biliary cholangitis; UDCA, ursodeoxycholic acid; ULN, upper limit of normal.