Abstract
Suicide is among the leading causes of death in the United States, with rates having risen substantially over the past two decades. Anger is a common symptom of several disorders associated with suicide, and the little research that has been done in the area suggests that it may be an often overlooked transdiagnostic risk factor for both suicidal ideation and behavior. The current study used the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) dataset to evaluate anger at Wave 1 as a risk factor for suicidal ideation and suicide attempt at Wave 2 (three years later) in a nationally representative sample of 34,653 participants. Chi-square analyses indicated that participants reporting problematic anger at Wave 1 were significantly more likely to endorse suicidal ideation (χ2 = 65.35, p < .001) and suicide attempt (χ2= 24.86, p < .001) at Wave 2. Multivariate regression analyses confirmed that problematic anger significantly predicted suicidal ideation (OR = 1.48, 95% CI [1.21,1.82], p < .001) and attempt (OR = 1.53, 95% CI [1.07,2.19], p = .020) over the three year period, even after adjusting for psychiatric risk factors, and demographic and historical covariates. Findings suggests the potential benefit of integrating anger assessment and treatment into research and clinical programs focused on reducing suicide risk.
Keywords: suicidal ideation, suicide attempt, anger
Between 1999 and 2017, the suicide rate in the United States has increased by 33%, making it the 10th leading cause of death (Hedegaard et al., 2018). Given its prevalence and public health impact, identifying risk factors for suicide is critical.
Multiple disorders associated with heightened suicide risk involve dysregulated anger (e.g., borderline personality disorder, posttraumatic stress disorder, intermittent explosive disorder; Nepon et al., 2010; Nock et al., 2010; 2014), suggesting that anger may be a transdiagnostic risk factor for suicide. For years, research with adolescents has documented a link between anger and suicide attempts (SA; e.g., Gispert et al., 1985; 1987; Hawton et al., 1982; Lehnert et al., 1994; Withers & Kaplan, 1987), and recent research has extended these findings into adulthood (Daniel et al., 2009). For example, in a study of psychiatric inpatients, anger measured during hospitalization prospectively predicted SA in the year following discharge, above and beyond other well-established risk factors such as psychiatric symptoms and recent SA (Sadeh & McNiel, 2013.)
Other research has examined the association between anger and completed suicide using retrospective methods. Morgan and Priest (1984) conducted a qualitative study of hospital case notes of inpatients who died by suicide and found that many expressed elevated anger before their death. In a case-controlled retrospective study of veterans who received primary care in the 6 months prior to death by suicide, researchers also found that medical records were more likely to contain documented expressions of anger (Dobscha et al., 2014).
Several cross-sectional studies have documented associations between anger and suicidal ideation (SI; Hawkins & Cougle, 2013; Hawkins et al., 2014; Horesh et al., 1997; Jang et al., 2014; Kachadourian et al., 2018; Kotler et al., 2001; Wilks et al., 2019) and attempt history (Ammerman et al., 2015; Hawkins & Cougle, 2013; Hawkins et al., 2014). These studies, while informative, have been limited by the timing of assessments and the fact that several of them assessed the presence of lifetime SI (e.g., Kachadourian et al., 2018; Hawkins & Cougle, 2013; Hawkins et al, 2014) or history of attempt (e.g., Ammerman et al., 2015; Hawkins & Cougle, 2013), which makes it difficult to ascertain the direction of the relationship between anger and suicidal thoughts and behaviors.
That anger is linked to suicidality is consistent with two prominent conceptual models of suicide. The fluid vulnerability theory (FVT; Rudd, 2006) proposes that risk for suicide fluctuates as function of both chronic and acute risk factors. According to FVT, some individuals are triggered to acute periods of SI more quickly than others, and there are individual differences in capacity to recover from urges to die by suicide. Individuals prone to anger may encounter frequent situational triggers of anger and distress. Increased anger may serve to push away social supports and increase isolation, relationship distress, and negative thoughts and feelings. Additionally, individuals with anger difficulties may find it more difficult to recover from these acute episodes (Tafrate et al., 2002; Wilkowski & Robinson, 2010).
The link between anger and suicidality is also consistent with the interpersonal-psychological theory of suicide (IPTS; Joiner, 2007). According to the IPTS, individuals are at the greatest risk for SI when they feel a lack of connection with others (thwarted belongingness) and feel they are a burden on others (perceived burdensomeness). Individuals who experience increased anger may be at higher risk of experiencing thwarted belongingness and perceived burdensomeness due to frequent interpersonal conflicts and relationship difficulties. Previous research has found evidence that the relationship between anger and SI is mediated by both of these factors (Hawkins et al., 2014; Rogers et al., 2017).
According to IPTS, the transition from ideation to lethal attempt requires an acquired capability for suicide that develops through repeated painful and provocative experiences, and research has demonstrated that the link between anger and this acquired capability is fully mediated by such experiences (Hawkins et al., 2014). Importantly, the FVT and IPTS models are not mutually exclusive, and recently researchers have suggested integrating these two theoretical approaches (Wolfe-Clark & Bryan, 2017).
To summarize, theory and previous research indicates that there is a relationship between anger and suicidality; however, many of these studies have been limited by reliance upon non-representative samples (e.g., treatment seekers) and either retrospective or cross-sectional designs. Although there is much evidence to indicate that anger is associated with suicide, it less clear whether, and to what extent, anger contributes to suicidal thoughts and attempts prospectively. To our knowledge, no studies have examined the longitudinal relationship between anger and suicidal thoughts and behaviors using a nationally-representative sample. The current study sought to examine whether problematic anger longitudinally predicted SI and SA in a large, nationally-representative sample, controlling for established risk factors. We hypothesized that problematic anger at Time 1 would be associated with SI and SA at Time 2.
Material and Methods
Participants and Procedure
Participants were from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The NESARC consisted of face-to-face interviews conducted by the National Institute on Alcohol Abuse and Alcoholism (NIAAA; for more details, see Grant & Kaplan, 2005; Grant et al., 2003; NIAAA, 2010). Wave 1 interviews were conducted between 2001 and 2002 and included 43,093 respondents. Of these individuals, 39,959 persons were eligible for Wave 2 (2004–2005), and 34,653 (86.7% response rate) completed Wave 2. The average interval between Waves was 3 years and 18 days (1,113 days; range 870 to 1,470 days). The NESARC study received full ethical review and approval from the U.S. Census Bureau and the U.S. Office of Management and Budget (Grant & Dawson, n.d.). All participants provided informed consent prior to completing the interviews.
The target population of the NESARC was the adult, civilian population residing in the 50 United States (US) and the District of Columbia. The housing unit sampling frame of the NESARC is based on the US Bureau of the Census Supplementary Survey, and also included a group quarters’ sampling frame derived from the Census 2000 Group Quarters Inventory. This sampling frame captures subgroups of the population with heavy substance use patterns who are not often included in general population surveys (e.g., military personnel living off base; persons in rooming houses, non-transient hotels and motels, shelters, facilities for housing workers, college quarters, and group homes). Hospitals, jails, and prisons were not sampled.
The final sample included 34,653 participants who had completed both Waves. The sample was 42 % male (n = 14,564), with a mean age of 45.97 years (SD = 17.37). The sample was nationally representative (NIAAA, 2010) with regard to race/ethnicity: Fifty-eight percent (n = 20,174) identified as White, 19% (n = 6,577) Black, 2% (n = 580) American Indian/Alaskan Native, 3% (n = 966) Asian/Native Hawaiian/Pacific Islander, and 18% (n = 6,356) Hispanic or Latino.
Measures
The NESARC interview contained items to assess the presence of psychiatric disorders and alcohol use patterns in addition to demographic and background information. Specific variables derived from the NESARC interview used in the present study are described below.
Demographics and background information.
Demographic and background variables assessed at Wave 1 included age, gender, race, education level, marital status, and annual income. These variables were controlled in multivariate analyses.
Psychiatric diagnoses.
Presence of major depressive disorder, bipolar disorder, psychotic disorder, or substance use disorder in the past 12 months was assessed at Wave 1 using the National Institute on Alcohol Abuse and Alcoholism Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version, a structured diagnostic interview designed for lay interviewers and shown to have good to excellent reliability (Grant et al., 2003). Presence of major depressive disorder, bipolar disorder, or psychotic disorder was coded 1=one or more severe mental disorders, 0=no severe mental disorders. Substance abuse was coded 0=neither alcohol nor drug abuse, 1=either alcohol or drug abuse, and 2=both alcohol and drug abuse.
Problematic anger.
At Wave 1, participants were asked “Do you often get angry or lash out when someone criticizes or insults you in some way?” (0=no, 1=yes).
History of suicidal ideation/attempts was coded ‘yes’ if the respondent affirmed any of three items. First, in the context of questions about low mood or anhedonia in Wave 1, respondents were asked did they “Think about committing suicide?” Second, in the same context, respondents were asked did they “Attempt suicide?” Third, respondents in Wave 2 were asked “In your entire life did you ever attempt suicide?… How old were you the most recent time that happened?” from which it was determined if the most recent SA occurred at an age before the Wave 1 interview.
Suicidal ideation between Waves 1 and 2 was coded ‘yes’ if the respondent affirmed the following item at Wave 2, which was asked in context of questions about low mood or anhedonia: “During that time since your last interview when (your mood was at its lowest/you enjoyed or cared the least about things), did you think about committing suicide?”
Suicidal attempt between Waves 1 and 2 was coded ‘yes’ if the respondent affirmed either of two items at Wave 2. In the context of questions about low mood or anhedonia, respondents were asked, “During that time since your last interview when (your mood was at its lowest/you enjoyed or cared the least about things), did you attempt suicide?” Respondents were also asked, “In your entire life did you ever attempt suicide?… How old were you the most recent time that happened?”, from which it was determined if the most recent SA occurred at an age after the Wave 1 interview.
Data Analytic Strategy
Analyses were conducted using SAS 9.3 supplemented with the SUDAAN software package to adjust for population level variables and method-related sampling bias (e.g., survey design, nonresponse, and sample attrition; Research Triangle Institute [RTI], 2008). The SUDAAN add-on has been used in multiple reports of NESARC data (e.g., NIAAA, 2010) and is explained in greater detail elsewhere (RTI, 2008). All analyses reported below have been adjusted to be representative of the U.S. civilian noninstitutional population. Descriptive analyses were used to present frequencies or means of independent and dependent variables (Table 1). Chi-square analyses were conducted to show relationship between anger and suicide variables. Multivariate logistic regression analyses were conducted in which SI and SA served as dependent variables and anger, psychiatric risk factors, and demographic and historical covariates served as independent variables. Odds ratios and 95% confidence intervals for adjusted models were estimated using SUDAAN, which uses Taylor series linearization to adjust for the design effects of sample surveys like the NESARC. Multivariate logistic regression analyses also covaried for days between subjects’ Wave 1 and Wave 2 interviews.
Table 1.
Descriptive statistics of the sample.
| Variable | M (SD) | n (%) |
|---|---|---|
| Wave 1 | ||
| Age (in years) | 45.97 (17.37) | |
| Annual income ($) | 28,752.87 (3,8338.28) | |
| Male gender | 14,564 (42.03) | |
| Race, white | 20,174 (58.22) | |
| Married | 17,401 (50.21) | |
| High school graduate | 28,909 (83.42) | |
| Anger problems endorsed | 3,264 (9.42) | |
| Past 12 months severe mental disorders | 2,932 (8.46) | |
| Major depressive disorder | 2,614 (7.54) | |
| Bipolar disorder | 616 (1.78) | |
| Psychotic disorder | 135 (0.39) | |
| Past 12 months substance use disorder | ||
| Either alcohol or drug use disorder | 2,645 (7.63) | |
| Both alcohol and drug use disorder | 330 (0.95) | |
| History of suicidal ideation or attempt | 3,498 (10.09) | |
| Wave 2 | ||
| Suicidal ideation between Waves 1 and 2 | 1,284 (3.71) | |
| Suicide attempt between Waves 1 and 2 | 323 (0.93) |
Results
Chi-Square Test of Independence
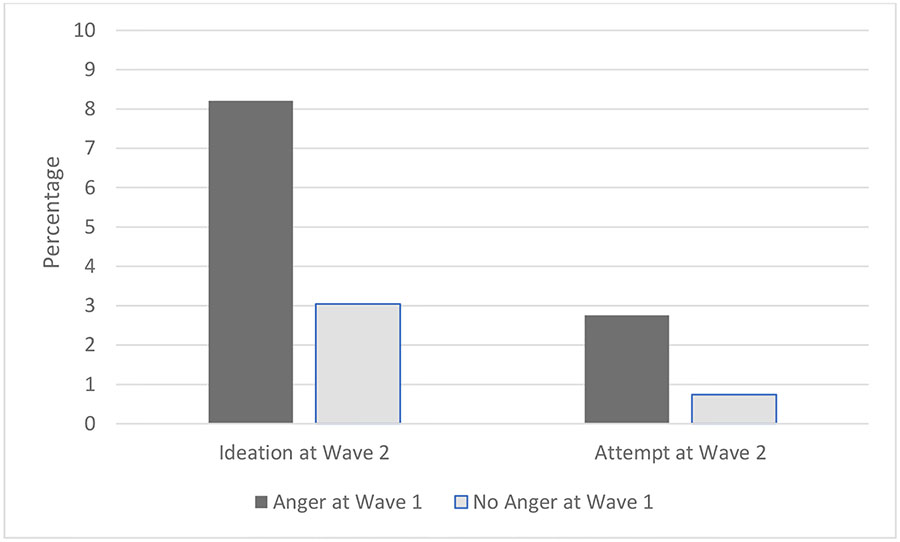
Two-hundred forty-five individuals reported experiencing both SI and attempt between Waves 1; 2, 1,039 reported SI only; and 78 reported an attempt without ideation. Of the 3,264 participants who endorsed problematic anger at Wave 1, 8.21% (n = 286) reported SI at Wave 2; of the 31,289 participants who did not endorse problematic anger at Wave 1, 3.04 % (n = 998) reported SI at Wave 2. Chi-square analyses confirmed that participants reporting problematic anger at Wave 1 were more likely to endorse SI between Waves 1 and 2, χ2 = 65.35, p < .001. Similarly, 90 of the participants who had endorsed problematic anger at Wave 1 reported a SA between Waves 1 and 2, for a 2.76% incidence. Of those who did not endorse problematic anger at Wave 2, 233 attempted suicide (0.74%). Again, these percentages were significantly different, χ2 = 24.86, p < .001, see Figure 1.
Figure 1.
Percentage of individuals endorsing suicidal ideation or suicide attempt at Wave 2 and endorsement of anger at Wave 1.
Multivariate Logistic Regression Analyses
Two multivariate logistic regression models were conducted to predict SI or SA between Waves 1 and 2. As shown in Table 2, all variables except for time between Waves, income, race, and education level were significant unique predictors of SI between Waves 1 and 2. Problematic anger at Wave 1 was a unique predictor of SI between Waves 1 and 2, OR = 1.48, 95% CI [1.21,1.82], p < .001.
Table 2.
Multivariate logistic regressions predicting suicidal ideation and suicide attempts between NESARC Waves 1 and 2.
| Suicidal ideation between Waves 1 & 2 | Suicide attempt between Waves 1 & 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||||
| Variable assessed at Wave 1 | OR | Lower | Upper | p | OR | Lower | Upper | p |
| Time | 1.00 | 1.00 | 1.00 | .736 | 1.00 | 1.00 | 1.00 | .353 |
| Age (in years) | .99 | .98 | .99 | <.001 | .98 | .97 | .99 | <.001 |
| Annual income ($) | 1.00 | 1.00 | 1.00 | .791 | 1.00 | 1.00 | 1.00 | <.001 |
| Male gender | .81 | .67 | .99 | .039 | .74 | .53 | 1.03 | .076 |
| Race, white | 1.10 | .93 | 1.30 | .266 | .77 | .55 | 1.09 | .134 |
| Married | .82 | .70 | .96 | .014 | 1.01 | .74 | 1.38 | .968 |
| High school graduate | .88 | .70 | 1.10 | .262 | .90 | .60 | 1.33 | .580 |
| Anger problems endorsed | 1.48 | 1.21 | 1.82 | <.001 | 1.53 | 1.07 | 2.19 | .020 |
| Past 12 months major depressive, bipolar, or psychotic disorder | 2.48 | 2.04 | 3.02 | <.001 | 2.20 | 1.56 | 3.10 | <.001 |
| Past 12 months alcohol or drug use disorder | 1.24 | 1.05 | 1.47 | .011 | 1.63 | 1.19 | 2.24 | .003 |
| History of suicidal ideation or attempt | 6.79 | 5.70 | 8.08 | <.001 | 6.51 | 4.59 | 9.23 | <.001 |
Note. NESARC = National Epidemiologic Survey on Alcohol and Related Conditions; OR = odds ratio; CI = confidence interval.
In the second model predicting SA between Waves 1 and 2, all variables except for time between Waves, gender, race, marital status, and education level were significant unique predictors. Problematic anger at Wave 1 was a unique predictor of SA between Waves 1 and 2, OR = 1.53, 95% CI [1.07,2.19], p = .020.
In a post-hoc analysis of the association between anger and SA, SI between Waves 1 and 2 was entered as a covariate. In this model problematic anger was no longer significantly associated with SA, OR = 1.19, 95% CI [0.80,1.78], p = .38, though age, race, income, substance use, history of SI/SA, and SI between waves were.
Discussion
To our knowledge, this was the first study to longitudinally examine the relationship between problematic anger and suicidal thoughts and behaviors in a nationally-representative sample. We found that problems with anger were significantly related to subsequent SI and attempts, and these associations remained even when covarying for established risk factors for suicide such as history of suicidal thoughts and behaviors, psychiatric comorbidities, and demographics. In fact, the presence of anger problems at Wave 1 increased the odds of SI and attempt at Wave 2 by 48% and 53%, respectively.
It is important to note, however, that while problematic anger at Wave 1 predicted SA at Wave 2 even when self-report of prior ideation or attempt was included in the model, anger was not associated with SA at Wave 2 if SI at Wave 2 was included in the model. This suggests that problematic anger does increase their risk for SA over time even in the context of a history of SI (i.e. longitudinally), but it does not confer additional risk over and above current SI (i.e. cross-sectionally). Taken together, our findings indicate that problematic anger may be a helpful variable to identify those who later go on to ideate or make a SA. However, if an individual is currently expressing SI, anger provides little additional information about current risk of SA.
Our findings are consistent with the fluid vulnerability theory (FVT; Rudd, 2006) and interpersonal psychological theory of suicide (IPTS; Joiner, 2007). Problematic anger may lead individuals to have increased interpersonal conflict and reduced social support. Individuals with anger difficulties may be more likely to feel disconnected from others and like they are a burden on those around them, leading them to be at higher risk for SI. Furthermore, increased anger may also contribute to an increased risk of SA due to the association between anger and aggression. Individuals who are used to acting on anger by “lashing out” aggressively at others, may be more likely to turn this aggression inward towards themselves.
The current findings highlight the importance of assessing anger when conducting suicide risk assessments in clinical practice. Existing suicide risk assessment tools do not typically assess anger (e.g., Columbia-Suicide Severity Rating Scale; Posner et al., 2011). Furthermore, practice guidelines for the assessment and management of suicide do not consistently include assessment of anger in their recommendations. For example, anger is included in Department of Veterans Affairs and Defense practice guidelines (VA/DoD, 2013), but not those of the American Psychiatric Association (APA; APA, 2016). In addition to assessing anger as part of suicide risk assessments, our findings also suggest that interventions to reduce anger difficulties may be beneficial for reducing risk for suicidal thoughts and behaviors. Additional research is needed to examine the effects of anger management treatment on subsequent suicidality.
This study is not without limitations. Notably, the measurement of problematic anger relied on a single item that was specific to interpersonal situations, “Do you often get angry or lash out when someone criticizes or insults you in some way?” The use of a single item does not adequately capture the multidimensional construct of anger difficulties. Future research should examine which dimensions of anger are associated with SI and attempts over time. SI was only assessed in the context of experiencing low mood or anhedonia, making it possible that participants who experienced SI outside of low mood/anhedonia were missed. The Waves of data collection were three years apart, which limits the ability to examine anger as a proximal risk factor for suicide. Furthermore, we did not include every possible candidate risk factor for suicide as our analyses were limited to variables measured by the NESARC at Wave 1. Finally, the data was collected over 15 years ago, which may reduce its generalizability.
In conclusion, the current study provides further evidence of the importance of anger as a risk factor for SI and attempts, using a longitudinal nationally-representative sample. These findings highlight the importance of assessing and treating anger in patients at risk for suicide.
Acknowledgments
This work was supported by Career Development Awards IK2RX002965 (to K.D.) and 1K2RX001298 (to E.V.) from the United States Department of Veterans Affairs Rehabilitation R&D Service. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government or any of the institutions with which the authors are affiliated.
References
- American Psychiatric Association, 2016. The American Psychiatric Association Practice Guidelines for the Psychiatric Evaluation of Adults (Third Edition). American Psychiatric Association, Arlington, VA: Retrieved from: https://psychiatryonline.org/doi/10.1176/appi.books.9780890426760.pe02#x27954.8322323 [Google Scholar]
- Ammerman BA, Kleiman EM, Uyeji LL, Knorr AC, McCloskey MS, 2015. Suicidal and violent behavior: The role of anger, emotion dysregulation, and impulsivity.Pers. Individ. Differ 79, 57–62. doi: 10.1016/j.paid.2015.01.044 [DOI] [Google Scholar]
- Daniel SS, Goldson DB, Erkanli A, Franklin JC, Mayfield AM, 2009. Suicidal and violent behavior: The role of anger, emotion dysregulation, and impulsivity. J. Clin. Child. Adolesc. Psychol 38, 661–671. doi: 10.1016/j.paid.2015.01.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Veterans Affairs and Department of Defense (VA/DoD), 2013. VA/DoD clinical practice guideline for assessment and management of patients at risk for suicide. Washington, CD: Author. [Google Scholar]
- Dobscha SK, Denneson LM, Kovas AE, Teo A, Forsberg CW, Kaplan MS, Bossarte R, McFarland BH, 2014. Correlates of suicide among veterans treated in primary care: Case-control study of a nationally representative sample. J. Gen. Intern. Med 29, 853–860. doi: 10.1007/s11606-014-3028-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Norman RE, Freedman G, Baxter AJ, Pirkis JE, Harris MG, Page A, Carnahan L, Degenhardt L, Vos T, Whiteford HA, 2014. The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study 2010. PloS One. 9, e91936. doi: 10.1371/journal.pone.0091936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gispert M, Davis MS, Marsh L, Wheeler K, 1987. Predictive factors in repeated suicide attempts by adolescents. Hosp. Community Psychiatry. 38, 390–393. doi: 10.1176/ps.38.4.390 [DOI] [PubMed] [Google Scholar]
- Gispert M, Wheeler K, Marsh L, Davis MS, 1985. Suicidal adolescents: Factors in evaluation. Adolescence. 20, 753–762. [PubMed] [Google Scholar]
- Grant BF, Dawson DA, (n.d.). Introduction to the National Epidemiologic Survey on Alcohol and Related Conditions. Retrieved from https://pubs.niaaa.nih.gov/publications/arh29-2/74-78.htm
- Grant BF, Kaplan KD, 2005. Source and accuracy statement for the 2004–2005 wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism (NIAAA). [Google Scholar]
- Grant BF, Kaplan KD, Shepard J, Moore T, 2003. Source and accuracy statement for wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism (NIAAA). [Google Scholar]
- Hawkins KA, Cougle JR, 2013. A test of the unique and interactive roles of anger experience and expression in suicidality: Findings from a population-based study. J. Nerv. Ment. Dis 201, 959–963. doi: 10.1097/NMD.0000000000000041 [DOI] [PubMed] [Google Scholar]
- Hawkins KA, Hames JL, Ribeiro JD, Silva C, Joiner TE, Cougle JR, 2014. An examination of the relationship between anger and suicide risk through the lens of the interpersonal theory of suicide. J. Psychiatr. Res 50, 59–65. doi: 10.1016/j.jpsychires.2013.12.005 [DOI] [PubMed] [Google Scholar]
- Hawton K, Cole D, O’Grady J, Osborn M, 1982. Motivational aspects of deliberate self-poisoning in adolescents. Br. J. Psychiatry 141, 286–291. doi: 10.1192/bjp.141.3.286 [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Curtin SC, Warner M, 2018. Suicide mortality in the United States, 1999–2017 NCHS Data Brief, no 330. National Center for Health Statistics, Hyattsville, MD. [PubMed] [Google Scholar]
- Horesh N, Rolnick T, Iancu I, Dannon P, Lepkifker E, Apter A, Kotler M, 1997. Anger, impulsivity and suicide risk. Psychother. Psychosom 66, 92–96. doi: 10.1159/000289115 [DOI] [PubMed] [Google Scholar]
- Jang JM, Park JI, Oh KY, Lee KH, Kim MS, Yoon MS, Ko SH, Cho HC, Chung YC, 2014. Predictors of suicidal ideation in a community sample: roles of anger, self-esteem, and depression. Psychiatry Res. 216, 74–81. doi: 10.1016/j.psychres.2013.12.054 [DOI] [PubMed] [Google Scholar]
- Joiner TE Jr., 2005. Why do people die by suicide? Harvard University Press, Cambridge, MA. [Google Scholar]
- Kachadourian LK, Gandelman E, Ralevski E, Petrakis IL, 2018. Suicidal ideation in military veterans with alcohol dependence and PTSD: the role of hostility. Am. J. Addict 27, 124–130. doi: 10.1111/ajad.12688 [DOI] [PubMed] [Google Scholar]
- Kotler M, Iancu I, Efroni R, Amir M, 1993. Anger, impulsivity, social support, and suicide risk in patients with posttraumatic stress disorder. J. Nerv. Ment. Dis 189, 162–167. [DOI] [PubMed] [Google Scholar]
- Lehnert KL, Overholser JC, Spirito A, 1994. Internalized and externalized anger in adolescent suicide attempters. J. Adolesc. Res 9, 105–119. doi: 10.1177/074355489491008 [DOI] [Google Scholar]
- Morgan HG, & Priest P, 1984. Assessment of suicide risk in psychiatric in-patients. Br. J. Psychiatry 145, 467–469. doi: 10.1192/bjp.145.5.467 [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA), 2010. Alcohol use and alcohol use disorders in the United States, a 3-year follow-up: Main findings from the 2004–2005 wave 2 national epidemiological study on alcohol and related conditions NIH Publication No 10–7677. [Google Scholar]
- Nepon J, Belik S, Bolton J, Sareen J, 2010. The relationship between anxiety disorders and suicide attempts: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Depress. Anxiety 27, 791–798. doi: 10.1002/da.20674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC, 2010. Mental disorders, comorbidity and suicidal behaviors: results from the National Comorbidity Survey Replication. Mol. Psychiatry 15, 868–876. doi: 10.1038/mp.2009.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Stein MB, Heeringa SG, Ursano RJ, Colpe LJ, Fullerton CS, Hwang I, Naifeh JA, Sampson NA, Schoenbaum M, Zaslavsky AM, Kessler RC, Army SC, 2014. Prevalence and correlates of suicidal behavior among soldiers: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA Psychiatry. 71, 514–522. doi: 10.1001/jamapsychiatry.2014.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ, 2011. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults.Am. J. Psychiatry 168, 1266–1277. doi: 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Triangle Institute, 2008. Software for Survey Data Analyses (SUDAAN) (Version 10) [Computer software]. Research Triangle Park, NC: Author. [Google Scholar]
- Rogers ML, Kelliher-Rabon J, Hagan CR, Hirsch JK, Joiner TE, 2017. Negative emotions in veterans relate to suicide risk through feelings of perceived burdensomeness and thwarted belongingness. J. Affect. Disord 208, 15–21. doi: 10.1016/j.jad.2016.09.038 [DOI] [PubMed] [Google Scholar]
- Rudd MD, 2006. Fluid vulnerability theory: A cognitive approach to understanding the process of acute and chronic risk, in Ellis TE, (Ed.), Cognition and Suicide: Theory, Research, and Therapy. American Psychological Association, Washington, D.C., pp. 355–368 [Google Scholar]
- Sadeh N, McNiel DE, 2013. Facets of anger, childhood sexual victimization, and gender as predictors of suicide attempts by psychiatric patients after hospital discharge.J. Abnorm. Psychol 122, 879–890. 10.1037/a0032769 [DOI] [PubMed] [Google Scholar]
- Schneider B, 2009. Substance use disorders and risk for completed suicide. Arch. Suicide Res 13, 303–316. doi: 10.1080/13811110903263191 [DOI] [PubMed] [Google Scholar]
- Tafrate RC, Kassinove H, Dundin L, 2002. Anger episodes in high‐and low‐trait‐anger community adults.J. Clin. Psychol 58, 1573–1590. 10.1002/jclp.10076 [DOI] [PubMed] [Google Scholar]
- Wilkowski BM, Robinson MD, 2010. The anatomy of anger: An integrative cognitive model of trait anger and reactive aggression.J. Pers 78, 9–38. 10.1111/j.1467-6494.2009.00607.x [DOI] [PubMed] [Google Scholar]
- Wilks CR, Morland LA, Dillon KH, Mackintosh MA, Blakey SM, Wagner HR, VA Mid-Atlantic MIRECC Workgroup, Elbogen EB, 2019. Anger, social support, and suicide risk in US military veterans. J. Psychiatr. Res 109, 139–144. doi: 10.1016/j.jpsychires.2018.11.026 [DOI] [PubMed] [Google Scholar]
- Withers LE, Kaplan DW, 1987. Adolescents who attempt suicide: A retrospective clinical chart review of hospitalized patients. Prof. Psychol. Res. Pract 18, 391–393. doi: 10.1037/0735-7028.18.4.391 [DOI] [Google Scholar]
- Wolfe-Clark AL, Bryan CJ, 2017. Integrating two theoretical models to understand and prevent military and veteran suicide. Armed Forces Soc. 43, 478–499. doi: 10.1177/0095327X16646645 [DOI] [Google Scholar]