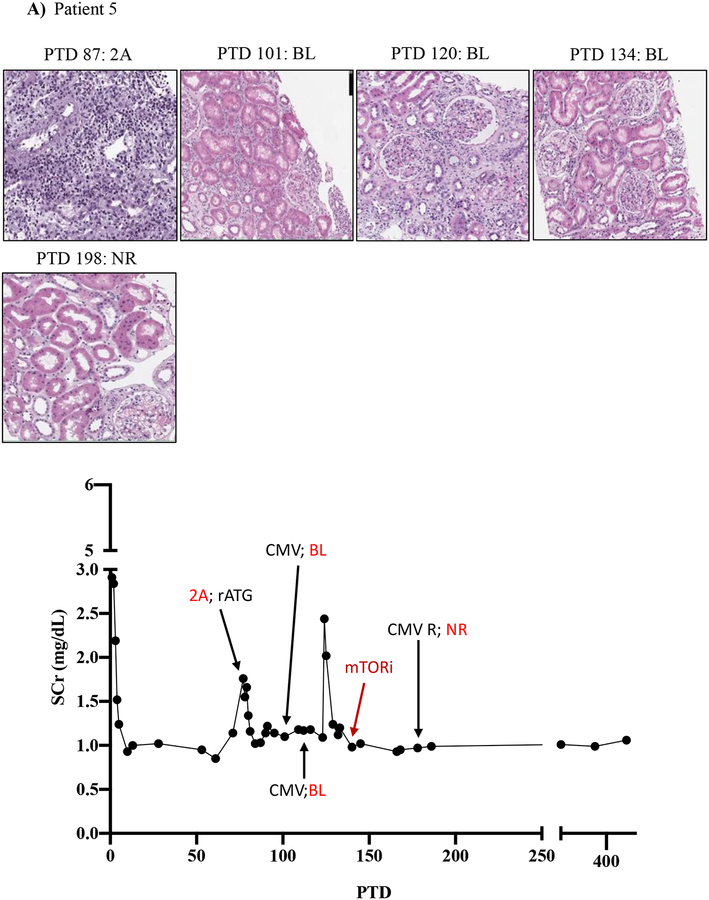
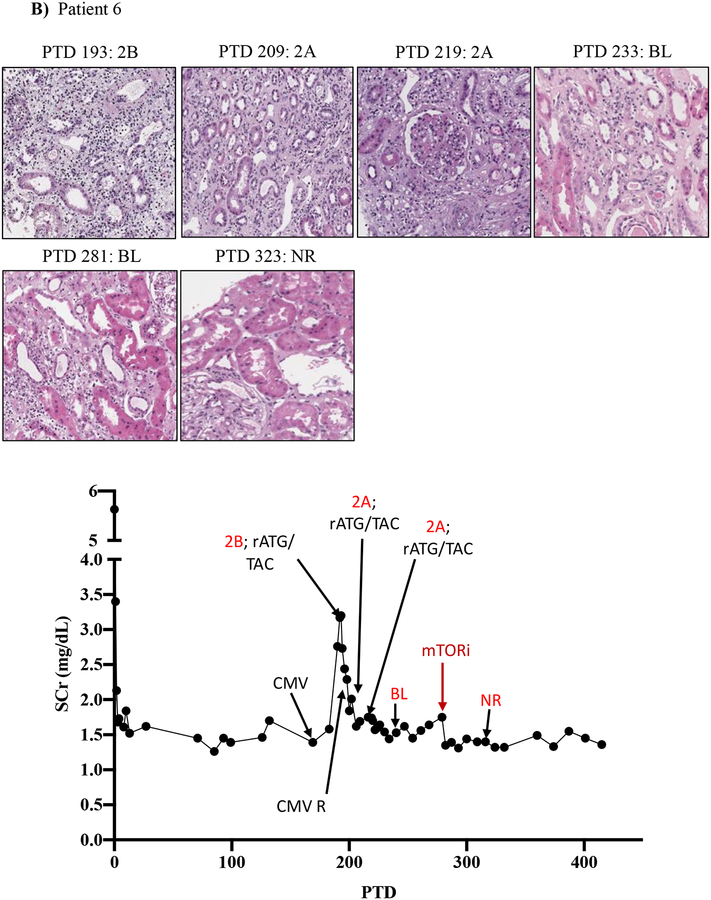
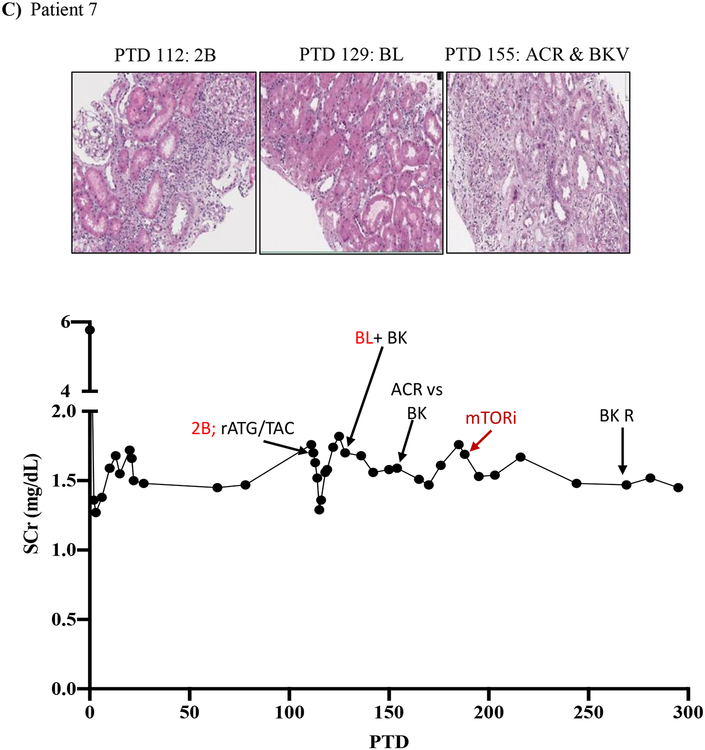
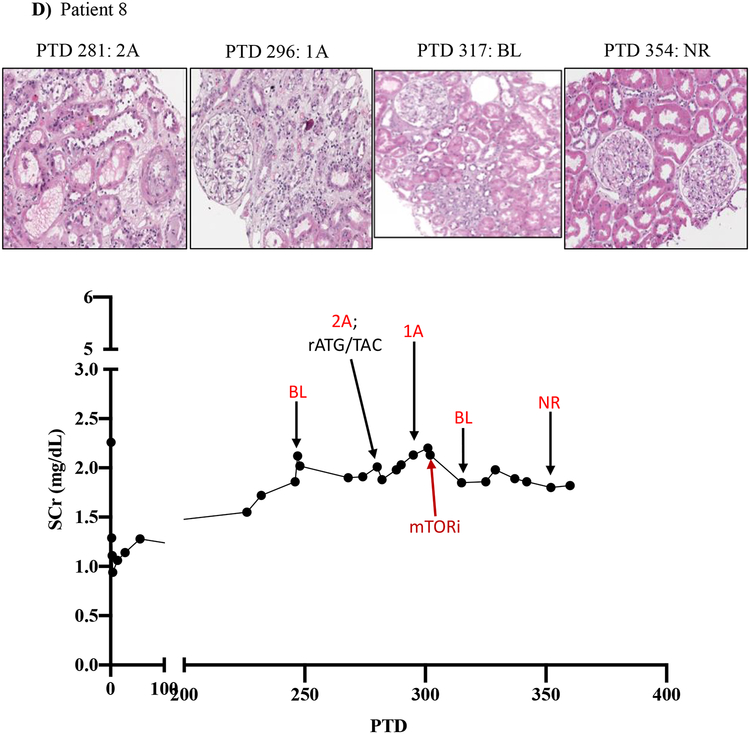
Figure 5. mTOR inhibition can rescue belatacept resistant rejections.
A-D) Diagrams show serum creatinine, histology, Banff lesion score (red), and treatment course of four patients that underwent rejection under belatacept and were treated with mTORi. Renal allograft pathology was determined by H&E stain analysis (micrographs) at specified timepoints. A) Shows a 50-year-old Caucasian female with ESRD secondary to hypertension that received a first kidney transplant from a deceased donor. She had a low cPRA (13%) and no evidence of pre-transplant DSA. The patient received rATG induction, belatacept, MMF, and early steroid withdrawal (5 days). B) Shows a 53-year-old unsensitized (cPRA 0%) Caucasian male with ESRD due to DM that received a first renal transplant from a living donor. Immunosuppression included alemtuzumab, belatacept, MMF, and steroid withdrawal at 5 days. CMV infection occurred on PTD 170 and required cessation of MMF therapy for resolution. C) Shows a 46-year-old unsensitized Caucasian male with focal segmental glomerulosclerosis that underwent a first kidney transplant from a living related one haplotype mismatched donor. Immunosuppression included rATG induction, belatacept, MMF, and early steroid cessation at 5 days. D) Shows a 44-year-old unsensitized Caucasian male with ESRD due to obstructive uropathy that underwent living related donor kidney transplant. Immunosuppression consistent of rATG induction, belatacept and MMF maintenance therapy with early steroid cessation on PTD 5.
ACR, acute cellular rejection; BL, borderline; CCS, corticosteroids; DM, diabetes mellitus; ESRD, end stage renal disease; GN, glomerulonephritis; MMF, mycophenolate mofetil; NR, no rejection; rATG, rabbit Anti-thymocyte globulin; TAC, tacrolimus.