Abstract
STUDY QUESTION
What is the prevalence of cannabis use and the perceptions of its impact on fertility among infertility patients?
SUMMARY ANSWER
A total of 13% of infertility patients used cannabis within the last year, and current usage is associated with patient perceptions of negative effects of cannabis on fertility and pregnancy.
WHAT IS KNOWN ALREADY
Cannabis use is increasing among the general population and pregnant women, particularly in places where cannabis use is legal despite having known and potential negative effects on fertility and pregnancy.
STUDY DESIGN, SIZE, DURATION
A cross-sectional patient survey study was performed between July 2017 and September 2017. Patients attending a university-affiliated hospital-based fertility clinic (n = 290) were invited to complete a written survey. Inclusion criteria were limited to the ability to read English. There were no exclusion criteria.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Of the 290 patients approached, 270 (93%) agreed to participate. The questions covered demographics, cannabis usage, perceptions of the effect of cannabis on fertility and pregnancy, cessation of use due to infertility and personal history of disclosing cannabis use to healthcare providers (HCP).
MAIN RESULTS AND THE ROLE OF CHANCE
The results showed that 13% of respondents disclosed use of cannabis in the past year (past year users) and 38% had not used cannabis in the past year but had previously used cannabis (>1 year users) while 49% had never used cannabis (never users). Baseline demographics were similar for the three groups, but across four measures of fertility and pregnancy health, past-year users perceived less of a negative effect compared to >1 year users, and never users (P values of 0.02, 0.03, 0.01, <0.001 for questions on pregnancy, offspring health, male fertility and female fertility, respectively). Of past year users, 72% said they had or would disclose use to their HCP, but only 9.4% reported that their HCP had actually instructed them to discontinue use.
LIMITATIONS, REASONS FOR CAUTION
Self-reported patient surveys are subject to reporting bias and may not reflect actual use and perceptions.
WIDER IMPLICATIONS OF THE FINDINGS
This study suggests that cannabis use is common among infertility patients. Given the known negative impacts of cannabis on pregnancy, the authors would have expected informed infertility patients to cease cannabis use as part of their efforts to conceive. As the prevalence of cannabis use in the last year among infertility patients is similar to that in the general Canadian population, it is unclear whether the prevalence of cannabis use in the sample population merely reflects the average usage in society or, after taking into account those who reduced their usage to improve their fertility, is a factor contributing to infertility and thus prompting fertility referral. Given concern about the potential negative impact of cannabis use on fertility, and that only 9% of past year users had been instructed by an HCP to cease cannabis use, HCPs should consider the benefits of counselling about cannabis cessation for patients who are attempting to conceive. Future research should focus on analysing the effects of cannabis use on female fertility and determining whether a reduction in use among patients with infertility can improve conception rates.
STUDY FUNDING/COMPETING INTEREST(S)
Michelle Shin, Clinical Research Associate, is supported by the University of Toronto GREI Fellowship Fund, which is sponsored by unrestricted research grants from EMD Serono, Merck Canada and Ferring Pharmaceuticals. The authors have no potential conflicts of interest to disclose.
Keywords: scannabis, fertility, infertility, perception, pregnancy, prevalence
WHAT DOES THIS MEAN FOR PATIENTS?
Marijuana (cannabis) use was legalized in Canada in October 2018, and as a result, more people have reported that they have been using marijuana over time, even before marijuana legalization took place. Research suggests that marijuana can have a negative effect on fertility for both men and women and can create problems when a woman uses marijuana while pregnant. This study was a written survey of patients with infertility to find out how many people were using marijuana while trying to become pregnant and to find out whether infertility patients thought that marijuana has any ill effects on pregnancy and fertility.
The researchers found that 13% of patients with infertility had been using marijuana within the last year. Only 9.4% of marijuana users had been advised to stop using it by their doctor. They also found that people who used marijuana more recently were less likely to think marijuana can have a negative effect on fertility and pregnancy compared with people who have never used marijuana. The study suggests that there is an opportunity for doctors to reduce marijuana use among people with infertility by talking to patients about the potential negative effects on fertility and the known negative effects on pregnancy The researchers caution that the findings of this study may not be reliable as patients may have not been honest about marijuana use when filling out the survey.
Introduction
Prior to its legalization in October 2018, cannabis (marijuana) was the most widely used illicit drug in Canada. With this legal shift, the prevalence and views of cannabis use among Canadians may transform. Although the effect of such policy changes cannot be definitively predicted, previous experiences with marijuana legislation can provide some insight; an increase in use is likely but not certain (MacCoun, 2011, Cerda et al. 2012, Hall and Weier, 2015, Wall et al. 2016). Supporting the increasing usage hypothesis, recent data from Statistics Canada shows that Canadian cannabis use in the past 3 months reached 17.5% in the first quarter (Q1) of 2019, rising from 14% in Q1 of 2018 (Statistics Canada 2019).
Cannabis is commonly used by women of reproductive age in Canada: 11% of 15–44-year-olds reported past-year use in 2012 (Porath-Waller 2015). The American National Survey on Drug Use and Health estimated past month cannabis use had increased by 62% in pregnant women between 2002 and 2014 (Brown et al. 2017). In a large Northern Californian study of 280 000 females, use in pregnancy was significantly increased from 4 to 7% (2009–2016) based on antenatal toxicology (Young-Wolff et al. 2017). This study within Kaiser Permanente Health Care institutions may be considered valid for extrapolation to Canadian society as they share a similar culture and timing of medical marijuana (MM) legislation; California in 1996 was followed by Canada in 2001.
Owing to the risks of preterm birth and neonatal morbidity, both the Society of Obstetricians and Gynaecologists and the American College of Obstetricians and Gynecologists have released statements encouraging cessation of cannabis use during pregnancy and while breastfeeding. Despite evidence supporting a causative and negative relationship between cannabis and semen concentration/motility, the dialogue rarely considers the fertility implications of cannabis use (Ordean et al., 2017, Braillon and Bewley 2018). Cannabis affects semen parameters as well as other functional properties of sperm via the endocannabinoid system (ECS) (Pacey et al. 2014, du Plessis et al. 2015, Gunderson et al. 2015). The ECS is an ancient, highly conserved and important cellular messaging system that is involved in a variety of physiologic and homeostatic functions in both men and women, including gonadotrophin regulation, endometrial differentiation, folliculogenesis and tubal transport (Wang et al. 2004, Horne et al. 2008, Oláh et al. 2008, El-Talatini et al. 2009, Fonesca et al. 2013) and cannabis’ impact on these important processes, while not yet clear, could be material.
With ample biological plausibility present, focus has increased on cannabis and its potential negative impact on female fertility. A recent review using secondary analysis of a randomized controlled trial evaluating the effects of aspirin on pregnancy and reproduction (EAGeR trial) showed that cannabis, but neither alcohol nor tobacco, made it harder to conceive as it led to an increased time-to-pregnancy (Plowden et al. 2017).
Cannabis use in pregnant and non-pregnant women has been extensively studied, but to our knowledge, there is no data on the prevalence of use in the infertility patient population. These patients are not only planning for a family but also many require access to healthcare to do so. There is a strong demand for health optimization as hopeful patients seek reproductive success and healthy offspring.
This study was designed to determine the self-reported prevalence of cannabis use among infertility patients at a downtown academic hospital-based fertility clinic in Canada, just prior to cannabis legalization. Secondary outcomes included perceptions of the effects of cannabis on pregnancy and fertility, cessation of use due to infertility and personal history of disclosing cannabis use to healthcare providers (HCP). We hypothesized that 10% of infertility patients are cannabis users and that a majority of users would not believe that such use has a negative effect on fertility.
Materials and Methods
This study is a cross-sectional population-based written survey designed to determine the prevalence of cannabis usage and associated perceptions in a metropolitan Canadian population of patients with infertility. The questions for the survey were designed based on expert opinion since there were no pre-existing validated surveys of cannabis usage and perceptions available in the literature. After a validation period that included feedback from clinic staff and a 10-patient pilot survey, a 33-question survey was created (Supplementary Data). The recruitment period occurred between July 2017 and September 2017 when a member of the research team approached all patients attending the Mount Sinai Fertility Clinic in Toronto and invited them to complete a voluntary and anonymous survey regarding cannabis. Inclusion criteria were limited to the ability to read English. There were no exclusion criteria.
A total of 290 patients were approached to participate in the study, of which 270 (93%) patients consented to do so and completed the survey. All unanswered survey questions were treated as missing data. Demographic information was collected along with questions pertaining to cannabis, alcohol and tobacco usage, fertility history, perceived effects of cannabis on fertility and disclosure of use to HCP (Supplementary Data).
Statistical analyses
Respondents were divided into three groups: past year users, >1 year users and never users. We compared the responses between the three groups using chi-square or Fisher exact tests where applicable. Data analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA). Two-tailed P values <0.05 were considered statistically significant.
Ethical approval
The study protocol was approved by the Mount Sinai Hospital Research Ethics Board (REB# 17-0108-E).
Results
Cannabis use
The prevalence of past year cannabis use was 13% in this sample population and just over half (137) of the 270 respondents had used cannabis at least once in their lifetime. With respect to timing of last usage, 71% (25/35) of past year users had used cannabis within the past 2 months (Fig. 1).
Figure 1.
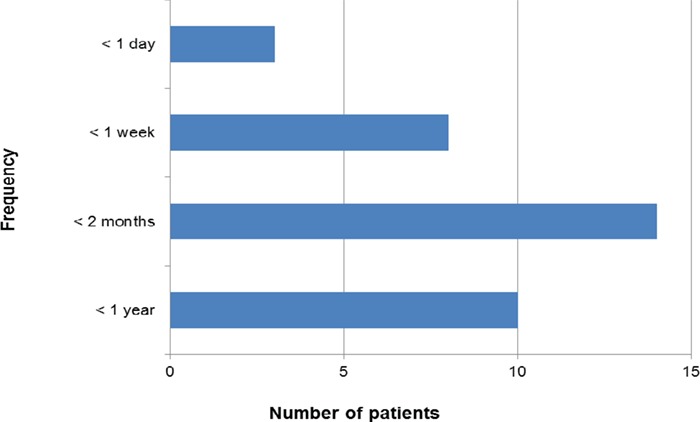
Time of last cannabis use in respondents (patients attending for infertility treatment) who disclosed use of cannabis in the past year (n = 35).
Baseline demographic information is shown in Table I. A total of 76% (206/270) of respondents identified as female. Place of birth, ethnicity and alcohol consumption (>1/day) were significantly correlated with past and current cannabis use; however, smoking status was not. Recreational use far outweighed medicinal use (97 versus 3%). Twenty-five percent of past year users stated that they had quit cannabis use due to infertility compared with only 15% of >1 year users, although this was not statistically significantly different. As those who had not used cannabis in the past year were currently dealing with infertility, we note that in advance of learning of their infertility at least 43 patients were using cannabis (past-year users plus >1 year users that gave up use due to infertility). Twelve patients gave up usage over 1 year ago upon learning of their infertility, while another eight gave up within the past year due to infertility, leaving 23 infertility patients that continued to use cannabis. Excluding users that gave up cannabis use when facing infertility for non-fertility related reasons, in total, 47% of patients using cannabis gave up cannabis use in the face of infertility.
Table I.
Baseline characteristics of respondents in a patient survey on cannabis use performed between July 2017 and September 2017.
| Characteristic | Past-year users (n = 35) | Users > 1 year (n = 102) | Non-users (n = 133) | P value |
|---|---|---|---|---|
| Age—years (mean ± SD) | 35.4 ± 3.9 | 35.5 ± 5.1 | 35.8 ± 5.3 | 0.216 |
| Female sex—n (%) | 24 (68.6) | 74 (72.6) | 108 (81.2) | 0.159 |
| Born in Canada—n (%) | 31 (88.6) | 74 (72.6) | 47 (35.3) | <0.001 |
| Ethnicity—n (%) | <0.001 | |||
| Caucasian | 21 (61.8) | 64 (66.7) | 43 (35.2) | |
| Asian | 5 (14.7) | 16 (16.7) | 45 (36.9) | |
| Other | 8 (23.5) | 16 (16.7) | 34 (27.9) | |
| Level of education—n (%) | 0.117 | |||
| High school | 2 (5.7) | 3 (2.9) | 6 (4.5) | |
| College | 11 (31.4) | 20 (19.6) | 19 (14.3) | |
| Undergraduate degree | 10 (28.6) | 40 (39.2) | 36 (27.1) | |
| Graduate degree | 9 (25.7) | 26 (25.5) | 43 (32.3) | |
| Professional degree | 3 (8.6) | 13 (12.8) | 28 (21.0) | |
| Nulliparous—n (%) | 14 (58.3) | 32 (43.2) | 40 (37.0) | 0.257 |
| Currently pregnant—n (%) | 0 (0) | 0 (0) | 0 (0) | |
| Have children—n (%) | 3 (12.5) | 18 (24.3) | 32 (29.6) | 0.202 |
| Menstrual cycle 24–35 days—n (%) | 22 (91.7) | 64 (86.5) | 95 (88.0) | 0.982 |
| Time trying to conceive—n (%) | 0.356 | |||
| <1 year | 9 (37.5) | 18 (24.3) | 23 (21.3) | |
| >1 year | 5 (20.8) | 26 (35.1) | 35 (32.4) | |
| >2 years | 9 (37.5) | 26 (35.1) | 49 (45.3) | |
| Undergoing fertility treatment—n (%) | 32 (91.4) | 98 (96.1) | 118 (88.7) | 0.112 |
| Smokers—n (%) | 3 (8.6) | 4 (3.9) | 3 (2.3) | 0.188 |
| Drink alcohol—n (%) | 33 (94.3) | 78 (76.5) | 52 (39.1) | <0.001 |
Perceptions
Some general trends were apparent in the perception of cannabis’ effect on four fertility-related health outcomes (pregnancy, offspring health, male fertility and female fertility) (Fig. 2). Across all three groups, for all four questions, few respondents believed that cannabis had no effect on fertility-related health outcomes. Past-year users were more likely to disagree or be unsure while the other two groups were more likely to respond ‘yes’ with respect to all four questions. This likely contributes to the past-year users’ continued use of cannabis while dealing with infertility. These differences of perception between the three groups were significant for all questions with P values of 0.02, 0.03, 0.01, <0.001 for questions on pregnancy, offspring health, male fertility and female fertility, respectively.
Figure 2.
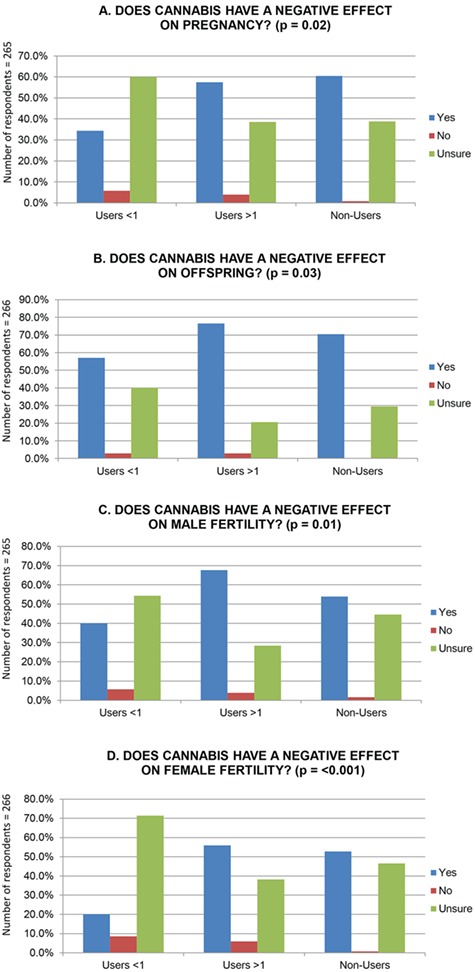
Perceptions of whether cannabis use has a negative effect on fertility. (A) Pregnancy (P = 0.02), (B) offspring (P = 0.03), (C) male fertility (P = 0.01) and (D) female fertility (P < 0.001) by group: past-year users, users >1 year and non-users (using Fisher’s exact test).
As to whether cannabis has a negative effect on fertility, 40% of past-year users believed ‘yes’ for male fertility and only 20% answered ‘yes’ for female fertility. For >1 year users, patients were more likely to perceive a negative impact of cannabis on fertility in general and similarly demonstrated a greater perceived impact on male fertility than on female fertility with 68% of respondents choosing ‘yes’ for male fertility and 56% choosing ‘yes’ for female fertility. Never users remained consistent in their responses that slightly favoured ‘yes’ versus ‘unsure’, regardless of sex. Fewer than 10% participants chose ‘no’ for the effect of cannabis on all the formerly mentioned parameters, with never users being less likely to choose ‘no’ than the other groups (Fig. 2).
Disclosure
Disclosure of use was also examined in the survey (Table II). We found that although 12% of anytime users (past year and >1 year users) had previously failed to disclose cannabis use, a much larger 78% felt that they could be honest with their HCP. In total, 72% of past year users said they would be willing to disclose use compared with 51% of >1 year users (P = 0.041). The difference could be explained by >1 year users who had not used cannabis in many years, not deeming the historical use relevant to their current health. Furthermore, out of the past-year users, only 9.4% had been instructed to discontinue use by their healthcare provider; however, 26% of that group stated they had quit cannabis within the last year due to infertility.
Table II.
Disclosure of cannabis use and cessation.
| Question |
Past Year Users
(n = 35) n (%) |
Users > 1 Year
(n = 102) n (%) |
P-value * |
|---|---|---|---|
| Able to be honest about cannabis use in a healthcare setting? | 0.192 | ||
| Yes | 23 (67.6) | 82 (81.2) | |
| No | 4 (11.8) | 5 (5) | |
| Unsure | 7 (20.6) | 14 (13.9) | |
| Told or will tell fertility physician about using cannabis? | 0.041 | ||
| Yes | 23 (71.9) | 36 (50.7) | |
| No | 3 (9.4) | 23 (32.4) | |
| Unsure | 6 (18.8) | 12 (16.9) | |
| Have been instructed to decrease or stop cannabis use by a healthcare provider while trying to conceive? | 0.726 | ||
| Yes | 3 (9.4) | 9 (19.2) | |
| No | 27 (84.4) | 76 (86.4) | |
| Unsure | 2 (6.3) | 3 (3.4) | |
| Have you stopped using cannabis because of infertility? | 0.228 | ||
| Yes | 8 (25.8) | 12 (15.8) | |
| No | 23 (74.2) | 64 (84.2) |
*Pearson’s chi-squared test and Fisher’s exact test
Discussion
Based on recent epidemiological data and current public perceptions of safety of cannabis use in general, we had hypothesized a 10% current usage among patients with infertility. In our study, which included a population of patients with infertility attending a metropolitan academic hospital-based fertility clinic, we found that the self-reported prevalence of cannabis use in the last year is 13%. Given that patients are not typically referred to a fertility clinic until they have been trying to conceive for at least 1 year, one would expect patients open to reducing cannabis use would have already reduced any modifiable behaviours that are perceived to have a negative impact on fertility prior to being referred for fertility treatment. This suggests that people who continue to use cannabis recreationally do not perceive any negative impact on fertility. Our findings confirmed the assumption that current marijuana users are less likely to perceive a negative impact on fertility than past years or non-users, and thus one can conclude it is this perception that leads to such a high incidence of use among people who are actively trying to conceive, despite medically relevant concerns that cannabis use can negatively impact fertility.
It is also important to note that the 13% prevalence of past-year cannabis use likely represents an underestimation of the true prevalence of use among infertility patients, a fact highlighted by the data from Kaiser Permanente Health Care Institutions, USA (Young-Wolff et al. 2017). The higher prevalence found via toxicology versus that determined by self-reporting suggested that use has commonly been underestimated in survey studies. Likewise, in a study comparing umbilical cord sampling to a survey of self-reported cannabis usage in pregnancy in a US state with marijuana legalization, 22.4% of umbilical cord assays had detectable cannabis metabolites compared with only 6% of participants reporting use within the past 30 days (Metz et al. 2019). Of note, in the Metz et al. (2019) study the self-reported prevalence of cannabis use within the last year was 14.7% among these pregnant patients, which is similar to the 13% reported in our study. Given that marijuana was not yet legal for recreational use at the time of our survey, it is possible that participants were being even less forthcoming about cannabis use than in other reported studies, in which case the true prevalence in our patient population may be much higher. Patients may also not have been forthcoming about cannabis use if they believed that recreational drug use might exclude them from fertility care, which may be the case at other fertility clinics around the world, but is not at our fertility centre. Furthermore, the data from Statistics Canada demonstrates a growing rate of use in Canada from early 2018 until early 2019 suggesting that usage among infertility patients has likely continued to grow since legalization (Statistics Canada 2019).
While the process of recreational cannabis legalization plays out within Canadian borders, it is difficult to predict exactly how and if usage trends will be affected. In American states where MM is legal, higher rates of marijuana use are reported compared with non-legal states, which is hypothesized to be related to four societal mechanisms: existing state-level community attitudes and behavioural norms may lead to MM legalization; enacting MM laws may lead to reduced disapproval and perceived riskiness of use, medical endorsement for its use as a treatment and increased commercial availability, promotion and access (Cerda et al. 2012). While these proposed mechanisms were created in the context of MM legislation, they can be used to discuss recreational legalization and provide us with a framework to understand the current climate in Canadian society. Based on these mechanisms, it is reasonable to infer that many of them are already in place in much of our society and that the prevalence could remain relatively stable.
In our study, previous cannabis use at any time was predicted by having been born in Canada, by Caucasian ethnicity and by alcohol consumption. This differs to the previously mentioned study in the USA, which only demonstrated correlations between cannabis use and young age (22–25 years old) and Medicaid instead of private medical insurance (Metz et al. 2019). These differences between studies likely represent the difference between the general pregnancy population in the USA where private medical insurance plays a pivotal role in medical care compared with the population of patients included in this fertility clinic study who are generally older, are almost all covered under public health insurance and are of a more varied ethnic background.
Regardless of whether use increases, decreases or stays the same, the fact that 13% of patients seeking fertility consultation or treatment used cannabis within the past year should be alarming. Patients are typically only referred to a fertility clinic after at least 1 year of infertility; therefore, this should be a motivated group of patients looking to optimize their chances of successfully achieving a pregnancy, and one would expect a low level of cannabis use compared to the general population if cannabis is known to have a negative impact on fertility. The prevalence of use in our study is indicative of the mixed information on cannabis that is readily available to patients.
Our study highlights that those infertility patients who are current users of cannabis are less likely to perceive that there is a harmful effect of cannabis on fertility compared with those who have never used cannabis, suggesting that perceptions of harm are clear motivators of use while actively trying to conceive. In a study assessing online Tweet messages about cannabis use in pregnancy, of the 550 Tweets captured from 2006 to April 2017, 77.6% had a neutral tone, making it seem that the health effects of cannabis use in pregnancy and the post-partum period are unclear despite the known adverse outcomes in pregnancy (Dakkak et al., 2018). When performing a Google search of ‘marijuana and fertility’, reassuring headlines, such as the following, are common and likely contributing to public perception of little to no risk of use while trying to conceive: ‘Marijuana use does not lower chances of getting pregnant’ (Abdalla, 2018). These types of headline commonly cite two large survey studies in the USA both of which demonstrated no statistically significant difference in time-to-pregnancy and fecundability in non-users compared with daily users (Kasman et al., 2018, Wise et al., 2018). However, these studies were surveying the general population and thus cannot be assumed to be generalizable to people struggling with infertility. Recently, the Canadian Medical Association Journal published a short article about marijuana and fertility, highlighting some of the potential negative effects of marijuana use while actively trying to conceive. The article has the potential to influence the sentiment of articles reported online (Ilnitsky and Uum, 2019).
A critical issue that this study leads us to consider is whether the prevalence reported in our study merely indicates that infertility patients use cannabis at similar rates to those in Canadian society not dealing with fertility challenges or whether cannabis use is a contributing cause to the patient’s infertility and resulting need for fertility healthcare. We note that 16% (43/270) of the sample population was either using cannabis or gave up using cannabis due to infertility; however, 16% is not materially greater than the average usage rate in the broader Canadian population, so this indicates that marijuana may not be a key driver of infertility. A public perception of the safety and potential health benefits of cannabis is predominant in Canadian society but there are potentially harmful effects on both fertility and, most importantly, pregnancy. The effect of cannabis on male fertility, in particular on semen analysis parameters, has been studied and that information has been used to counsel patients on cessation (Pacey et al. 2014, du Plessis et al. 2015, Gunderson et al. 2015). Our study reflected that there is some public awareness of this effect since 40% of <1 year users perceived there to be a negative effect on male fertility compared with only 20% for female fertility. This discrepancy highlights that the contemporary understanding of cannabis’ effect on female fertility is less robust, but it does continue to garner attention. Despite our findings on marijuana use in our population compared to that in broader society, future research should focus on delineating the effects of cannabis use on female fertility and whether simple interventions to reduce use among patients with infertility can improve conception rates.
Furthermore, there is growing evidence of the potential detrimental effect of cannabis use in pregnancy, including an increased risk of preterm birth, neonatal morbidity and stillbirth (Varner et al., 2014, Metz et al. 2017, Corsi et al., 2019). Patients who are attending a fertility clinic are actively trying to conceive and therefore should be aware of these potentially detrimental effects in pregnancy as it is likely the most motivating factor for reducing use. In a cross-sectional survey study at a tertiary antenatal care clinic in Baltimore, MD, USA, researchers found that for women who successfully quit cannabis use in pregnancy, the most common motivator was to prevent harm to their pregnancy (Mark et al. 2017). We found in our study that 25% of past-year cannabis users quit as a result of infertility issues within that same year. However, only 9.4% of respondents reported that they were instructed to curb use by their doctor. This could be because doctors were not asking about cannabis use or were aware of the use and not recommending cessation. In either case, the fertility clinic may represent a practical, effective and under-utilized arena for intervention and cessation.
While there may be fertility centres around the world that require patients not to be using cannabis prior to fertility treatment, this is not typical in Canada where there are few eligibility criteria for fertility treatment, even for government-funded IVF cycles. Fertility clinics and government-funded fertility services that typically have eligibility criteria that encourage improvement in health status prior to treatment, such as a healthy weight and being a non-smoker, should consider whether being a non-user of cannabis should be added to the list of requirements to potentially improve pregnancy outcomes. As more jurisdictions globally consider legalization of marijuana, and with growing numbers of articles on the benefits and safety of marijuana posted on social media, it is anticipated that fertility clinics around the world will be seeing more patients using cannabis. Our study highlights the need to start addressing this issue with patients early on in their fertility treatment.
Studies to better characterize the complex relationship between cannabis, female fertility and patient care are warranted given the limited status of our scientific understanding and the perceived uncertainty of its effect among fertility patients. HCPs should be equipped with the evidence needed to accurately counsel patients who are using cannabis and receiving reproductive care. We hope this study of cannabis prevalence and perceptions among infertility patients helps to better prepare HCPs for addressing this issue with patients who are planning conception.
Conclusion
In this survey of 270 infertility patients, the prevalence of self-reported past-year cannabis use was 13%. A majority of patients were willing to disclose cannabis use to a HCP, but only 9.4% had been counselled to discontinue use. Perceptions of the negative effects of cannabis on fertility and pregnancy are correlated with recent use. Given concern about the potential negative impact of cannabis use on fertility, HCPs should consider the benefits of counselling on cannabis cessation for patients that are attempting to conceive.
Supplementary Material
Acknowledgements
The authors would like to thank Dr Zhong-Cheng Luo, Department of Obstetrics and Gynaecology, Lunenfeld-Tanenbaum Research Institute, Mount Sinai Hospital, Sinai Health System, for providing statistical support for the study; to Michelle Shin, Clinical Research Association, for her assistance with study recruitment; and to Jonathan Royce for assistance in editing the manuscript for publication.
Authors’ roles
T.J. and C.A.J. initially conceived of the research project and study design including survey construction and testing. B.N. and T.J. performed data collection and data analysis. All authors contributed to the initial writing, critical discussion and editing of the manuscript and provided approval for the final version of the manuscript.
Funding
No specific funding was obtained for this research. Michelle Shin, Clinical Research Associate, is supported by the University of Toronto GREI Fellowship Fund, which is sponsored by unrestricted research grants from EMD Serono, Merck Canada and Ferring Pharmaceuticals.
Conflict of interest
The authors have no potential conflicts of interest to disclose.
References
- Abdalla S. SPH study: marijuana use does not lower chances of getting pregnant. The Brink March 2018. Available at:https://www.bu.edu/articles/2018/marijuana-use-and-chances-of-pregnancy/. (15 December 2019, date last accessed). [Google Scholar]
- Braillon A, Bewley S. Committee opinion no. 722: marijuana use during pregnancy and lactation. Obstet Gynecol 2018;131:164. [DOI] [PubMed] [Google Scholar]
- Brown QL, Sarvet AL, Shmulewitz D, Martin SS, Wall MM, Hasin DS. Trends in marijuana use among pregnant and non-pregnant reproductive-aged women, 2002-2014. JAMA 2017;317:207–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend 2012;120:22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsi DJ, Walsh L, Weiss D, El-Chaar D, Hawken S, Fell DB et al. . Association between self-reported prenatal cannabis use and maternal, perinatal, and neonatal outcomes. JAMA 2019;322:145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- du Plessis SS, Agarwal A, Syriac A. Marijuana, phytocannabinoids, the endocannabinoid system, and male fertility. J Assist Reprod Genet 2015;32:1575–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakkak H, Brown R, Twynstra J, Charbonneau K, Seabrook JA. The perception of pre- and post-natal marijuana exposure on health outcomes: a content analysis of twitter messages. J Neonatal Perinatal Med 2018;11:409–415. [DOI] [PubMed] [Google Scholar]
- El-Talatini MR, Taylor AH, Elson JC, Brown L, Davidson AC, Konje JC. Localisation and function of the endocannabinoid system in the human ovary. PLoS One 2009;4:e4579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonesca BM, Correia-da-Silva G, Almada M, Costa MA, Teixeira NA. The endocannabinoid system in the postimplantation period: a role during decidualization and placentation. Int J Endocrinol 2013; 510540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson TA, Jorgensen N, Andersson AM, Bang AK, Nordkap L, Skakkebaek NE et al. . Association between use of marijuana and male reproductive hormones and semen quality: a study among 1,215 healthy young men. Am J Epidemiol 2015;182:473–481. [DOI] [PubMed] [Google Scholar]
- Hall W, Weier M. Assessing the public health impacts of legalizing recreational cannabis use in the USA. Clin Pharmacol Ther 2015;97:607–615. [DOI] [PubMed] [Google Scholar]
- Horne AW, Phillips JA, Kane N, Lourenco PC, McDonald SE, Williams AR et al. . CB1 expression is attenuated in fallopian tube and decidua of women with ectopic pregnancy. PLoS One 2008;3:e3969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilnitsky S, Van Uum S. Marijuna and fertility. CMAJ 2019;1919:E638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasman AM, Thoma ME, McLain AC, Eisenberg ML. Association between use of marijuana and time to pregnancy in men and women: findings from the National Survey of Family Growth. Fertil Steril 2018;109:866–871. [DOI] [PubMed] [Google Scholar]
- MacCoun RJ. What can we learn from the Dutch cannabis coffee shop system? Addiction 2011;106:1899–1910. [DOI] [PubMed] [Google Scholar]
- Mark K, Gryczynski J, Axenfeld E, Schwartz RP, Terplan M. Pregnant women’s current and intended cannabis use in relation to their views toward legalization and knowledge of potential harm. J Addict Med 2017;11:211–216. [DOI] [PubMed] [Google Scholar]
- Metz TD, Allshouse AA, Hogue CJ, Goldenberg RL, Dudley DJ, Varner MW et al. . Maternal marijuana use, adverse pregnancy outcomes and neonatal morbidity. Am J Obstet Gynecol 2017;217:478.e1–478.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metz TD, Silver RM, McMillin GA, Allshouse AA, Jensen TL, Mansfield C et al. . Prenatal marijuana use by self-report and umbilical cord sampling in a state with marijuana legalization. Obstet Gynecol 2019;133:98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oláh M, Milloh H, Wenger T. The role of endocannabinoids in the regulation of luteinizing hormone and prolactin release. Differences between the effects of AEA and 2AG. Mol Cell Endocrinol 2008;286:S36–S40. [DOI] [PubMed] [Google Scholar]
- Pacey AA, Povey AC, Clyma JA, McNamee R, Moore HD, Baillie H et al. . Modifiable and non-modifiable risk factors for poor sperm morphology. Hum Reprod 2014;29:1629–1636. [DOI] [PubMed] [Google Scholar]
- Plowden TC, Zolton JR, Radin R, Sjaarda L, Kim K, Connell MT et al. . Exposure of alcohol, tobacco, and marijuana exposure and time to pregnancy. Fertil Steril 2017;108:e30–e31. [Google Scholar]
- Porath-Waller AJ. Clearing the smoke on cannabis: maternal cannabis use during pregnancy-an update. Canadian Centre on Substance Abuse 2015. [Google Scholar]
- Ordean A, Wong S, Graves LSOGC. No. 349 - substance use in pregnancy. J Obstet Gynecol 2017;39:922–937.e2. [DOI] [PubMed] [Google Scholar]
- Statistics Canada Cannabis Stats Hub. Updated August 14, 2019. Available at: https://www150.statcan.gc.ca/n1/pub/13-610-x/cannabis-eng.htm (14 August 2019, date last accessed).
- Varner MW, Silver RM, Rowland Hogue CJ, Willinger M, Parker CB, Thorsten VR et al. . Association between stillbirth and illicit drug use and smoking during pregnancy. Obstet Gynecol 2014;123:113–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall MM, Mauro C, Hasin DS, Keyes KM, Carda M, Martins SS et al. . Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: commentary on Stolzenberg et al. (2015) and reanalysis of US National Survey on Drug Use in Households data 2002-2011. Int J Drug Policy 2016;29:9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Guo Y, Wang D, Kingsley PJ, Marnett LJ, Das SK et al. . Aberrant cannabinoid signaling impairs oviductal transport of embryos. Nat Med 2004;10:1074–1080. [DOI] [PubMed] [Google Scholar]
- Wise LA, Wesselink AK, Hatch EE, Rothman KJ, Mikkelsen EM, Sorensen HT, Mahalingaiah S. Merijuana use and fecundability in a North American preconception cohort study. J Epidemiol Community Health 2018;72:208–215. [DOI] [PubMed] [Google Scholar]
- Young-Wolff KC, Tucker LY, Alexeeff S, Armstrong MA, Conway A, Weisner C et al. . Trends in self-reported and biochemically tested marijuana use among pregnant females in California from 2009-2016. JAMA 2017;318:2490–2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


