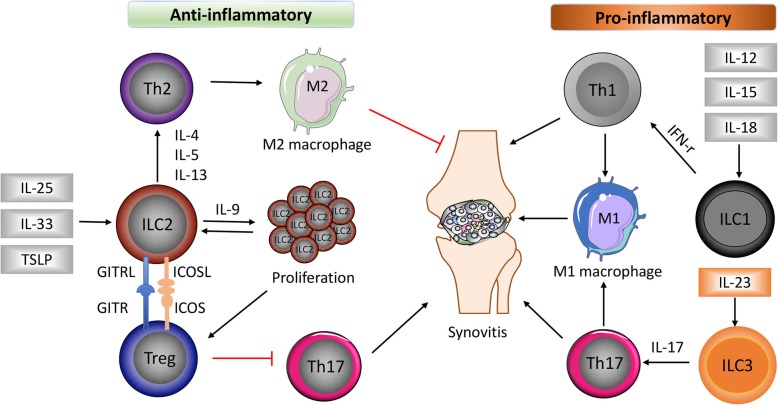
Fig. 1.
The role of different ILC subsets in RA. Damage in the epithelium cells leads to the release of alarmins such as IL-25, IL-33, and thymic stromal lymphopoietin (TSLP), which strongly induces ILC2 differentiation and subsequent Th2 activation by producing IL-4, IL-5, and IL-13. ILC2s proliferate under IL-9 stimulation and activate regulatory T cells (Treg) via binding of glucocorticoid-induced TNFR-related protein (GITR) ligand (GITRL) to GITR and inducible co-stimulator (ICOS) ligand (ICOSL) to ICOS. Th2 activation induces anti-inflammatory M2 macrophages, together with decreased Th17 responses promote resolution of synovitis. In contrast, ILC1s and ILC3s were differentiated under stimulation of IL-12, IL-15, IL-18, and IL-23, respectively, which further cause Th1 and Th17 activation, proinflammatory M1 macrophage induction, and aggravate inflammation in the joint