Figure 1.
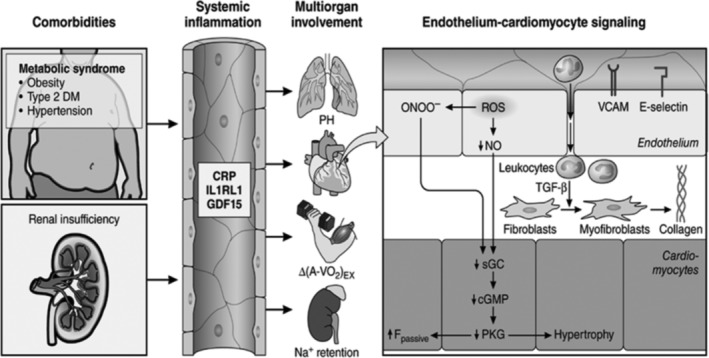
Systemic and myocardial signaling in heart failure (HF) with preserved ejection fraction (HFpEF). Comorbidities induce systemic inflammation, evident from elevated plasma levels of inflammatory biomarkers, such as soluble interleukin 1 receptor‐like 1 (IL1RL1), C‐reactive protein (CRP), and growth differentiation factor 15 (GDF15). Chronic inflammation affects the lungs, myocardium, skeletal muscle, and kidneys leading to diverse HFpEF phenotypes with variable involvement of pulmonary hypertension (PH), myocardial remodeling, deficient skeletal muscle oxygen extraction (ΔA‐Vo2) during exercise (Ex), and renal Na + retention. Myocardial remodeling and dysfunction begin with coronary endothelial microvascular inflammation manifest from endothelial expression of adhesion molecules, such as vascular cell adhesion molecule (VCAM) and E‐Selectin. Expression of adhesion molecules attracts infiltrating leukocytes secreting transforming growth factor β (TGF‐β), which converts fibroblasts to myofibroblasts with enhanced interstitial collagen deposition. Endothelial inflammation also results in the presence of reactive oxygen species (ROS), reduced nitric oxide (NO) bioavailability, and production of peroxynitrite (ONOO–). This reduces soluble guanylate cyclase (sGC) activity, cyclic guanosine monophosphate (cGMP) content, and the favorable effects of protein kinase G (PKG) on cardiomyocyte stiffness and hypertrophy. HFpEF indicates heart failure with preserved ejection fraction. (Reproduced with permission from Reference 16)
