Abstract
Background
Surgery residents complete their research training early in residency. Non-surgical trainees typically have research incorporated toward the last two years of their fellowship, conferring an advantage to apply for grants with recent research experience and preliminary data.
Methods
The NIH RePORTER database was queried for K08 awardees trained in medicine, pediatrics, and surgery from 2013–2017. 406 K08 recipients were identified and time from completion of clinical training to achieving a K08 award was measured. Data were compared using ANOVA and expressed as mean. P<0.05 was considered significant.
Results
Surgeons took longer to obtain a K08 than those trained in internal medicine (surgery=3.7 years, internal medicine=2.58 years p<0.0001)). All K08 recipients without a PhD took longer to obtain a K08 than recipients with a PhD (MD=3.50 years and MD/PhD=2.42 years(p=<0.0001).
Conclusions
Surgeons take longer to achieve a K08 award than clinicians trained in internal medicine, possibly due to an inherent disadvantage in training structure.
Keywords: Basic Science, Research, K08, Career Development, R01
Introduction
The competition for grant funding has become increasingly more competitive. Although surgeons have historically been productive in research and contributed significantly to basic and clinical science, there is growing concern that fewer surgeons are performing research.1 Prolific surgical discoveries dominated the New England Journal of Medicine in the 1920s – 1950s, but now, since the 1970s, less than 10 percent of the journal’s articles are devoted to surgery.2 There have been several hypotheses concerning why surgeons have become less involved in research—an overall decrease in available funding coupled with an increase in pressure to be clinically productive has certainly contributed.3
The National Institutes of Health (NIH) provide several award mechanisms that are considered the benchmark of research success in academic medicine. The Mentored Clinical Science Research Career Development Award (K08) is specifically sought after by junior faculty interested in developing their career as a clinician-scientist. The benefit of the K08 award is the protected research time to extend the period of mentorship during the transition to an independent primary investigator.4 Given the trend of surgeons becoming less involved in research, it is not surprising to note that fewer surgeons applied for a K08 award than their non-surgical counterparts over a recent 10-year period. Surgeons were 2.5 times less likely to apply, and of those who applied, only 43.3% obtained K08 awards, while 52.2% of non-surgeons were successfully funded.5
In an increasingly competitive environment, it is important to delineate why surgeons are falling behind. In addition to increased clinical responsibilities, we hypothesized that the decline of the surgeon scientist may be due to inherent differences in training structure between surgeons and their medicine-pediatric counterparts. For surgeons, research training starts earlier in the junior years of residency, typically after the second or third clinical year. Surgery residents complete 2–3 years of either basic science or clinical research, then return for an additional 3–5 years of clinical training involving completion of residency and fellowship, with no protected time for research during these years. This leaves the junior academic surgeon applying for funding with a remote research experience, as well as a lack of formal research mentorship, which may be a significant disadvantage in securing grants.5 Non-surgical trainees, however, typically have research incorporated toward the last two years of their fellowship, allowing for a swift transition and scientific momentum to apply for grants with preliminary data and established mentorship. Given these differences in training structure, we hypothesized that surgeons would take longer to secure a K08 award than physicians trained in medicine or pediatrics. Furthermore, we hypothesized that obtaining a PhD degree would allow clinician scientists to obtain a K08 more quickly.
Materials and Methods
Population
The study population consisted of K08 recipients from 2013–2017. Data was obtained from the NIH Research Portfolio Online Reporting Tools (RePORTER),6 an online database that provides access to all NIH supported research and awards. The database was queried with the activity code: K08. Departments included were the following: internal medicine, pediatrics, surgery, neurosurgery, urology, otolaryngology, orthopedic surgery, plastic surgery, and vascular surgery. This query generated data including recipient name, research subject matter, and total first year funding. While the Research Project Grant Program (R01) award has been examined by other investigators as the most important milestone in securing funding, it typically marks the transition from a mentored junior faculty scientist to independent investigator.7,8 Investigating the differences in K08 recipients, however, better demonstrates the transition from trainee to junior faculty and thus, is a better representation of preparedness for research immediately after clinical training.
Data Collection
After the database generated by the NIH RePORTER, several additional data were gathered from department websites. These included sex, residency completion date, fellowship completion date, current employer, and presence of additional graduate degrees. When department websites were insufficient, medical social networking websites such as LinkedIn and Doximity were used. Individuals were contacted directly if necessary. Descriptive statistics were analyzed using GraphPad Prism Software. Data were tested for normality and compared using a Students t-test, Mann-Whitney test, and ANOVA with p < 0.05 considered significant.
Results
Demographics
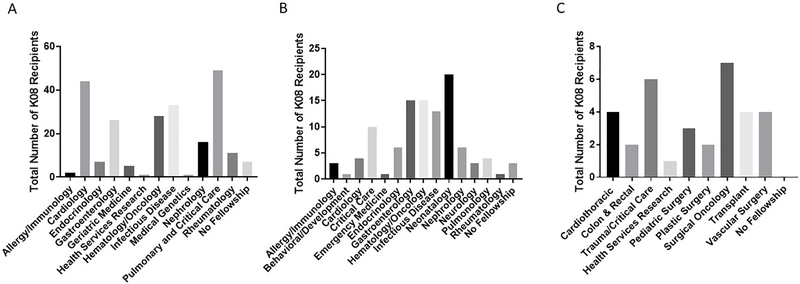
We identified a total of 406 K08 recipients from 2013–2017 in our query. As shown in Table 1, there were 230 K08 recipients who completed residency in internal medicine, 105 in pediatrics, and 71 in surgery. Of the 406 recipients, 260 were male and 146 were female. Among K08 recipients, surgeons had the highest percentage of males (74.7%), followed by internal medicine (68.3%) then pediatrics (47.6%). Within medicine, those who were further trained in pulmonary and critical care medicine had the largest number of K08 grants. Within pediatrics, neonatologists had the highest number of K08’s, and within surgery, those who were trained in surgical oncology had the most K08 awards (Figure 1).
Table 1.
K08 Recipient Demographics
| Characteristics | Internal Medicine (n=230) | Pediatrics (n=105) | Surgery (n=71) | Total |
|---|---|---|---|---|
| Male | 157 | 50 | 53 | 260 |
| Female | 73 | 55 | 18 | 146 |
| Degrees | ||||
| MD | 147 | 74 | 53 | 274 |
| MD/PhD | 83 | 31 | 18 | 132 |
| Academic Rank | ||||
| Professor | 0 | 0 | 1 | 1 |
| Associate Professor | 8 | 15 | 31 | 54 |
| Assistant Professor | 204 | 79 | 37 | 320 |
| Instructor/Lecturer | 15 | 10 | 0 | 25 |
| Private Practice | 3 | 1 | 2 | 6 |
Figure 1.
Specialty distribution of K08 recipients: (A) Internal Medicine. (B) Pediatrics. (C) General Surgery
Time to K08 award from completion of training
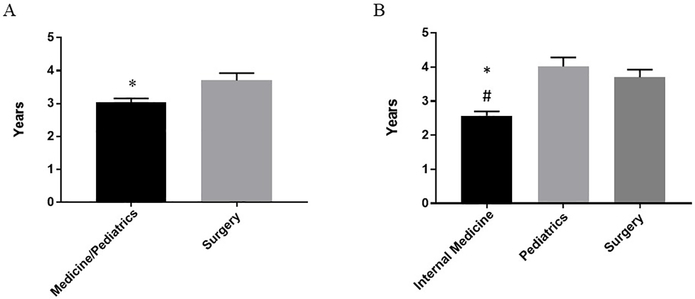
Our primary outcome was to measure the time (in years) from completion of clinical training to securing a K08 award. As seen in Figure 2A, K08 recipients who completed a surgical residency took longer to obtain a K08 award than those trained in medicine and pediatrics (surgery mean = 3.70 years and internal medicine/pediatrics mean = 3.03 years (p = 0.0045)). An additional sub-analysis of internal medicine and pediatrics is shown in Figure 2B. Clinicians who trained in internal medicine achieved a K08 faster than those who trained in pediatrics (internal medicine mean = 2.58 years; pediatrics mean = 4.02 years (p-value <0.0001)). Surgeons also took longer than clinicians trained in internal medicine to obtain a K08 award (surgery mean = 3.70 years (p-value <0.0001)). The difference between surgery and pediatrics, however, was not statistically significant (p = 0.6911).
Figure 2.
Time from end of clinical training to K08 award in years as a function of residency completed: (A) Combined internal medicine and pediatrics vs. surgery, *p<0.05. (B) Sub-analysis of internal medicine vs. pediatrics vs. surgery, *p<0.05 vs. pediatrics, #p<0.05 vs. surgery.
An additional sub-analysis of K08 recipients who completed a surgical sub-specialty residency is shown in Table 2. Recipients who completed residency in neurosurgery were the fastest to obtain a K08 award (mean = 2.44 years), while those who were trained in otolaryngology took the longest (4.38 years). However, multivariate analysis did not show any statistically significant difference in time to K08 among surgical sub-specialists. Inferential statistics among the different residencies completed in surgery was limited due the small size of the individual groups.
Table 2.
Surgery Sub-Analysis
| Characteristics | General Surgery (n=33) | Neurosurgery (n=9) | Otolaryngology (n=8) | Orthopedic Surgery (n=6) | Urology (n=9) | Plastic Surgery (n=5) | Vascular Surgery (n=1) |
|---|---|---|---|---|---|---|---|
| Sex | |||||||
| Male | 26 | 4 | 6 | 6 | 7 | 3 | 1 |
| Female | 7 | 5 | 2 | 0 | 2 | 2 | 0 |
| Degrees | |||||||
| MD | 25 | 7 | 4 | 5 | 8 | 4 | 0 |
| MD/PhD | 8 | 2 | 4 | 1 | 1 | 1 | 1 |
| Academic Rank | |||||||
| Professor | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Associate Professor | 18 | 2 | 3 | 1 | 5 | 2 | 0 |
| Assistant Professor | 14 | 6 | 5 | 5 | 3 | 3 | 1 |
| Time to K08 (years) | 3.94 | 2.44 | 4.38 | 3.0 | 3.88 | 4.20 | 3.0 |
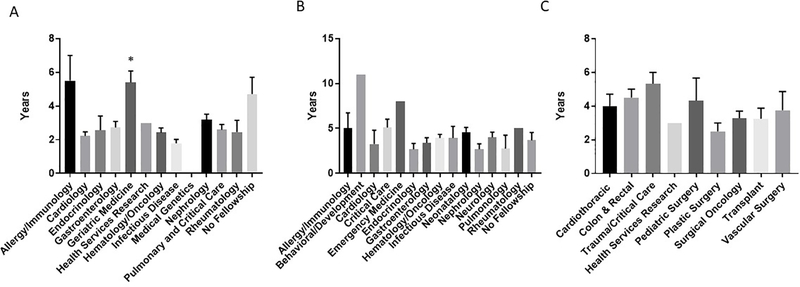
Figure 3 demonstrates the effect of fellowship training on time to K08 award after completion of internal medicine, pediatric, and general surgery residencies. Multivariate analysis showed a statistically significant difference in time to K08 for internal medicine physicians who trained in infectious disease (mean = 1.79 years) compared to those who trained in geriatrics (mean = 5.40 years (p = 0.0187)). There were no significant differences in time to K08 for any fellowship in either pediatrics or general surgery.
Figure 3.
Analysis of effect of fellowship on time from end of clinical training to K08 award. (A) Sub-analysis of internal medicine fellowships, *p<0.05 vs. infectious disease. (B) Sub-analysis of pediatric fellowships. (C) Sub-analysis of general surgery fellowships
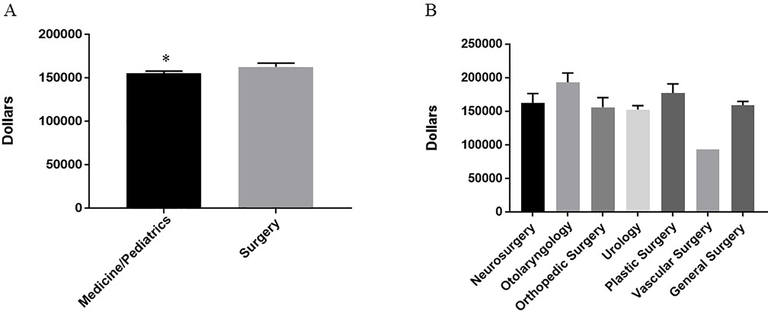
Funding
Surgeons received a significantly larger award for first year funding than both internal medicine and pediatrics (surgery mean = $162,727, internal medicine/pediatrics = $155,471 (p-value = 0.0025), Figure 4A). Further sub-analysis examined possible differences among surgeons in first year funding amounts (Figure 4B). There was no statistically significant difference in funding among surgeons. Additionally, there was no difference between internal medicine and pediatrics for first year funding (internal medicine mean = $155,237; pediatrics mean = $155,983; p-value = 0.1605).
Figure 4:
First-year funding in U.S. Dollars. (A) Funding dollars of K08s from internal medicine and pediatrics vs. surgery, *p<0.05. (B) Sub-analysis of funding dollars of surgical specialties.
Academic Rank
Differences in academic rank are seen among individuals in both Table 1 and Table 2. There were four different levels of academic rank: full professor, associate professor, assistant professor, and instructor/lecturer. A small number of K08 recipients in surgery, medicine, and pediatrics currently work in private practice. These individuals were excluded in analysis of variations in academic rank. Surgeons were more likely to have a higher academic rank then K08 recipients who trained in internal medicine and pediatrics. Among those currently working in academics, 45.6% of surgeons hold the rank of associate professor compared to 14.6% of those trained in pediatrics (p-value <0.0001), and just 3.5% of those trained in internal medicine (p-value <0.0001).
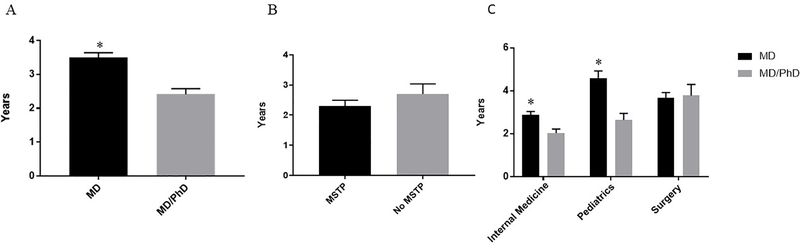
Impact of PhD on time to K08 award
Of all K08 recipients, 32.5% had both an MD and a PhD, whereas 67.5% had only an MD. The majority of K08 recipients with a PhD received their PhD during medical school as part of the Medical Scientist Training Program (MSTP) (MSTP = 72%, Non-MSTP = 28%). The proportion of recipients with a PhD was roughly equivalent across all groups (internal medicine = 36.1%; pediatrics = 29.5%; surgery = 25.4% (p-value=0.181)). Together, all K08 recipients without a PhD took longer to obtain a K08 than recipients with a PhD (MD mean = 3.50 years and MD/PhD mean = 2.42 years (p=<0.0001) Figure 5A), regardless of specialty. There was no significant difference in time to K08 between those who participated in MSTP vs. those who did not (MSTP mean = 2.31 years, Non-MSTP mean = 2.70 years (p=0.2652) Figure 5B).
Figure 5.
Impact of PhD. (A) Impact of PhD on time to K08 across all specialties, *p<0.05. (B) Impact of PhD obtained through MSTP and no MSTP on time to K08 across all specialties. (C) Impact of PhD on time to K08 as a function of specialty, *p<0.05.
Further sub-analysis revealed that a PhD does not confer an advantage to surgeons in the timing to obtain a K08 award. K08 recipients with a PhD who completed a surgical residency took a mean of 3.68 years to obtain a K08 award, whereas those without a PhD took 3.78 years (p=0.9599). For those who completed a medicine or pediatric residency, however, a PhD degree did provide a significant advantage. K08 recipients with a PhD who completed an internal medicine residency took less time (mean = 2.04 years) than those without a PhD (mean = 2.88 years (p=<0.0007)). Additionally, K08 recipients with a PhD who completed a pediatrics residency took significantly less time (mean = 2.65 years) than those without a PhD (mean = 4.60 years (p=0.0001)) to obtain K08 funding (Figure 5C).
Discussion
It is becoming more widely accepted that the number of physician scientists are declining.9–12 Most vulnerable to this decline have been surgeons, and multiple explanations have been identified as to why surgeons have been disproportionately affected by this trend, including a lack of a formal research training curriculum and increasing clinical demands for junior faculty.13.14 Recommendations in the literature in curtailing this decline of surgeon scientists have been largely focused on interventions after residency, with proposed guidelines being geared towards strategies of success for junior faculty.15 This study is focused instead on identifying barriers intrinsic to differences in training structure that are present prior to finishing clinical training.
To our knowledge, there has not been a study comparing the amount of time from end of training to receiving a K08 award across different specialties. We found that surgeons took longer to obtain a K08 award after finishing clinical training than those trained in internal medicine. The difference between internal medicine and surgery was about 14 months. This is not a large amount of time, however, in a competitive academic environment, where grant funding success is often measured by the novelty of ideas, 14 months may be significant for professional advancement. Surgeons also held a higher academic rank than their medicine and pediatric counterparts, most likely due to the increased length of time spent as a junior faculty member until they received their K08 award. This finding is likely due to two factors: the lack of preliminary data and established research mentorship that surgeons often have due to their remote research experience, as well as the greater clinical workload facing junior surgeon faculty.
Contrary to our hypothesis, the sub-analysis revealed that there was no statistical difference between how long it took to achieve a K08 award between pediatricians compared to surgeons. This is likely multifactorial and may be due to pediatrics residency training placing a lesser emphasis on resident research involvement than internal medicine and surgery. Indeed, there have been efforts in U.S. pediatric training programs to incorporate a more formal research curriculum to later boost pediatric research productivity,16 although this has not been uniformly adopted. Our data demonstrate that obtaining a PhD allowed K08 recipients to obtain funding faster after clinical training. This effect was most dramatic in recipients trained in pediatrics, with a mean difference of almost 2 years (MD alone = 4.60 years; MD/PhD = 2.65 years). This suggests that pediatric clinicians benefit from a formal degree in research training more so than internal medicine physicians and surgeons, and it may be that the PhD degree provides the emphasis on research that the pediatric training paradigm may be lacking.
Even though obtaining a PhD was beneficial for both internal medicine and pediatric physicians, surgeons with a PhD did not obtain a K08 any faster than those without a PhD. Again, this is likely due to a significant amount of time passing between research training and applying for funding. Since surgical training is longer than both internal medicine and pediatrics, there is inevitably a larger period of time between obtaining a PhD degree (either in medical school or during dedicated research years) and completing clinical training. For surgeons this produces certain disadvantages, such as the need to relearn basic science techniques, adjust to new cutting-edge research technology, and regenerate preliminary data, potentially mitigating the benefit of a PhD degree. Additionally, because junior surgeon faculty often have more clinical responsibilities than non-surgeon faculty, the benefit of the PhD may be blunted by the need to be productive clinically early in surgery.
Our data demonstrates that surgeons receive a larger first year funding K08 award than both internal medicine and pediatric physicians. This is likely due to differences in salary. A review of physician compensation reports17 show that surgeons make more annually than non-surgeons, and the NIH typically covers a designated percentage of a K08 recipient’s salary, allowing them to receive a larger first year award. This can be misleading as it only pertains to an individual’s funding award, rather than a whole department. The majority of data suggest that surgical departments still receive less NIH funding than internal medicine, and are disproportionately affected by the decrease in NIH funding over the last 10 years.1
There are limitations to this study. First, training structure is not homogenous across all the surgical specialties included in this study. Although general surgery and neurosurgery typically offer dedicated research time early in clinical training, other surgery residency programs, such as otolaryngology, urology, and orthopedic surgery do not always offer time for research in residency training. Second, given that fewer surgeons receive K08 awards than both internal medicine and pediatric clinician scientists, the small sample size limited the sub-analysis for surgical specialties, and care must be taken to draw inferential statistics in these groups. Third, we limited our study to K08 awards and did not examine other grants including R01, Department of Defense, or VA merit awards. Fourth, this study examined the speed at which different specialties received NIH funding. Academic productivity, rather than time to K08 may be a better metric of success of the clinician scientist, and may be a limiting factor in obtaining the K08 in the first place. Lastly, we did not analyze the differences in clinical practice between surgeons and non-surgeons as junior faculty. New surgeons face increased clinical demand and are typically “on service” 12 months a year, whereas junior faculty in internal medicine are typically allotted several contiguous weeks, or even months, at a time that are dedicated to research. This lack of contiguous extended protected time may be an additional contributing factor to delay funding acquisition for surgeons.
Conclusions
Surgeons take longer to achieve a K08 award than clinicians trained in internal medicine, but not pediatrics. This may be due to an inherent disadvantage in training structure, causing new surgeon graduates to enter a competitive environment without any recent research experience, preliminary data, or established mentorship. Given the large volume of residency programs involved in this study and the heterogeneity of training structures, this data alone does not provide sufficient evidence to support moving research time during surgical residency to the end of clinical training.
Physician-scientists trained in internal medicine were fasted to obtain a K08 award. Internal medicine fellowships often have dedicated research time structured into the end of their training curriculum, and it is important to consider whether offering this same opportunity to surgeons in fellowships would offer the same advantage. Given that changing the research training paradigm in surgical residency is unlikely in the near future, offering additional research time in fellowship may be a more feasible programmatic change rather than eliminating early research training in residency altogether. Alternatively, this data may provide an opportunity to conduct a prospective study comparing traditional surgical resident research training to an experimental “surgeon-scientist track,” where programs with a strong commitment to research offer an alternative curriculum and move dedicated research time from the beginning to the end of clinical training. Regardless, there needs to be a concerted effort to help surgeons obtain grants early, enter the academic environment competitively, and thereby maintain the surgeon scientist.
Highlights.
Fewer surgeons are performing research and obtaining funding.
Surgeons take longer to obtain a K08 award than internal medicine physicians.
Surgeons receive larger first-year funding than both internal medicine and pediatrics.
K08 recipients in surgery held a higher academic rank than non-surgeons.
Obtaining a PhD reduces the amount of time it takes to obtain a K08 award.
Acknowledgments
Funding sources:
TAM is supported by K08DK113226 from the National Institutes of Health, the Koret Foundation, and the Department of Surgery at the Indiana University School of Medicine
MG is supported by K08DK101608, R03DK111473 and R01DK118568 from the National Institutes of Health, March of Dimes Foundation Grant No. 5-FY17-79, the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital, and the Department of Pediatrics at Washington University School of Medicine, St. Louis.
KS is supported by NIH 4T32HD043010-14, Association for Academic Surgery/ Association for Academic Surgery Foundation Trainee Research Fellowship Award, and The Children’s Discovery Institute of Washington University and Saint Louis Children’s Hospital.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Narahari A, Mehaffey J, Hawkins R, et al. Surgeon Scientists Are Disproportionately Affected by Declining NIH Funding Rates. J Am Coll Surg, 2018. 226(4): p. 474–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gawande A Two hundred years of surgery. N Engl J Med, 2012. 366(18): p. 1716–23. [DOI] [PubMed] [Google Scholar]
- 3.Kodadek L, Kapadia M, Changoor N, et al. Educating the surgeon-scientist: A qualitative study evaluating challenges and barriers toward becoming an academically successful surgeon. Surgery, 2016. 160(6): p. 1456–1465. [DOI] [PubMed] [Google Scholar]
- 4.Scott J, Carlson E. K08 and K99 cardiovascular training: comparisons and trends among current awardees. Circ Res, 2012. 110(7): p. 910–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rangel SJ, Moss RL Recent trends in the funding and utilization of NIH career development awards by surgical faculty. Surgery, 2004. 136(2): p. 232–9. [DOI] [PubMed] [Google Scholar]
- 6.National Institute of Health. NIH Research Portfolio Online Reporting Tools (RePORT). Bethesda, Maryland, USA. Available at https://projectreporter.nih.gov/reporter.cfm. [Accessed June 20, 2018].
- 7.Good M, McElroy S, Berger J, Wynn J. Name and Characteristics of National Institutes of Health R01-Funded Pediatric Physician-Scientists: Hope and Challenges for the Vanishing Pediatric Physician-Scientists. JAMA Pediatr, 2018. 172(3): p. 297–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King A, Sharma-Crawford I, Shaaban A, et al. The pediatric surgeon’s road to research independence: utility of mentor-based National Institutes of Health grants. J Surg Res, 2013. 184(1): p. 66–70. [DOI] [PubMed] [Google Scholar]
- 9.Yin H, Gabrilove J, Jackson R, et al. Sustaining the Clinical and Translational Research Workforce: Training and Empowering the Next Generation of Investigators. Acad Med, 2015. 90(7): p. 861–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen SR The clinical investigator as an endangered species. N Engl J Med, 1980. 302(16): p. 927. [PubMed] [Google Scholar]
- 11.Milewicz D, Lorenz R, Dermody T, et al. Rescuing the physician-scientist workforce: the time for action is now. J Clin Invest, 2015. 125(10): p. 3742–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collins F Scientists need a shorter path to research freedom. Nature, 2010. 467(7316): p. 635. [DOI] [PubMed] [Google Scholar]
- 13.Suliburk J, Kao L, Kozar R, Mercer D. Training future surgical scientists: realities and recommendations. Ann Surg, 2008. 247(5): p. 741–9. [DOI] [PubMed] [Google Scholar]
- 14.Keswani S, Moles C, Morowitz M, Zeh H. The Future of Basic Science in Academic Surgery: Identifying Barriers to Success for Surgeon-scientists. Ann Surg, 2017. 265(6): p. 1053–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldstein A, Blair A, Keswani S, et al. A Roadmap for Aspiring Surgeon-Scientists in Today’s Healthcare Environment. Ann Surg, 2019. 269(1): p. 66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roth D, Chan N, Vohra S. Initial successes and challenges in the development of a pediatric resident research curriculum. J Pediatr, 2006. 149(2): p. 149–50. [DOI] [PubMed] [Google Scholar]
- 17.Medscape. 2016. Medscape Physician Compensation Report. New York, New York, USA. Available at https://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=2 [Accessed March 8 2019]