Abstract
Dual antiplatelet therapy (DAPT) with aspirin and P2Y12 inhibitor is administered following percutaneous coronary intervention (PCI) with coronary stent implantation. Several studies have reported the effects of switching between P2Y12 inhibitors on platelet reactivity (P2Y12 reaction units: PRU), from acute to late phase after PCI. However, the effect of switching at very late phase is unknown. This study examined the effect on PRU in Japanese coronary heart disease patients with long-term DAPT (aspirin + clopidogrel) when switching from clopidogrel to prasugrel. Ninety-six patients were enrolled in this study. The median DAPT duration at enrollment was 1824.0 days. Twenty-three patients with PRU ≥ 208 at enrollment were randomly assigned into either continuing to receive clopidogrel (Continued Group; n = 11) or switching to prasugrel (Switched Group; n = 12). The primary endpoint was the rate of patients who achieved PRU < 208 at the end of 12 weeks of treatment, which was significantly higher in Switched Group relative to Continued Group (90.0% vs. 36.4%; P = 0.024). The secondary endpoint was the PRU at week 12 in groups subdivided according to cytochrome P450 (CYP) 2C19 genotypes. At week 12, extensive metabolizers (EM Group) had 202.3 ± 60.0 and 174.5 ± 22.3 in Continued Group and Switched Group (P = 0.591), respectively; intermediate and poor metabolizers (non-EM Group) had 229.4 ± 36.9 and 148.4 ± 48.4 in Continued Group and Switched Group (P = 0.002), respectively. The PRU for non-EM Group was significantly reduced in Switched Group. Thus, for patients with long-term DAPT (aspirin + clopidogrel) after PCI with coronary stent implantation, switching from clopidogrel to prasugrel resulted in a stable reduction in PRU, regardless of CYP2C19 polymorphism.
Keywords: Percutaneous coronary intervention, Clopidogrel, Genetic polymorphism, Drug change
Introduction
The guidelines recommend dual antiplatelet therapy (DAPT) with aspirin and P2Y12 inhibitor to prevent major adverse cardiovascular events, such as stent thrombosis and reinfarction, in patients after percutaneous coronary intervention (PCI) with coronary stent implantation [1–3]. Clopidogrel has been commonly used as a P2Y12 inhibitor for DAPT.
However, it is also reported that the genetic polymorphisms of its metabolizing enzyme, cytochrome P450 (CYP) 2C19, are involved in the antiplatelet effect of clopidogrel [4, 5]. The CYP2C19 genotypes are classified based on rate of drug-metabolizing activity into three groups: extensive metabolizers (EM), intermediate metabolizers (IM), and poor metabolizers (PM), causing inter-individual variability in response to clopidogrel [6, 7]. In addition, prevalence of IM and PM in the Japanese population is higher than in Western populations [6, 8].
The P2Y12 reaction units (PRU), an index of antiplatelet effects of P2Y12 inhibitors, are also reported to be a relevant factor associated with cardiovascular events [9, 10]. In the latest guidelines, the routine testing of platelet function when using antiplatelet agents is not recommended (Class III) with Level of Evidence A [2]. However, the ADAPT-DES study reported that the incidence of stent thrombosis or myocardial infarction was significantly higher in patients with PRU > 208 after successful PCI, compared to patients with PRU ≤ 208 [11, 12]; and, considering such, the platelet function testing may not as insignificant as claimed.
In the studies that examined association of PRU with CYP2C19 polymorphism in patients treated with clopidogrel, PRU in IM and PM patients was reported significantly higher than in EM patients [7, 13, 14]. Additionally, frequency of cardiovascular events was reported higher in patients treated with clopidogrel who carry CYP2C19 loss-of-function alleles, compared to patients without the alleles [15, 16]. These reports suggest that, even in patients receiving DAPT (aspirin + clopidogrel) after coronary stent implantation, possible future cardiovascular events could be predicted by PRU measurement or CYP2C19 genotype test to identify patients with inadequate antiplatelet response.
Prasugrel is known to be less affected by CYP2C19 polymorphism [17]. The PRASFIT-ACS [18, 19] and PRASFIT-Elective [20] conducted in Japan have reported that prasugrel steadily lowered PRU and reduced the incidence of cardiovascular events in patients irrespective of the CYP2C19 polymorphism. Recent studies have reported that switching between P2Y12 inhibitors affects PRU [21–23]. However, never reported was the change in PRU in patients with different CYP2C19 polymorphism when switching P2Y12 inhibitors from clopidogrel to prasugrel in patients receiving long-term DAPT (aspirin + clopidogrel).
Several reports have suggested that cardiovascular events occurred in spite of long-term DAPT (aspirin + clopidogrel) [12, 24]. The patients receiving long-term DAPT (aspirin + clopidogrel) with CYP2C19 polymorphism may experience the result of poor inhibition of platelet aggregation, even in the chronic phase, thereby increasing the risk of cardiovascular events. Thus, we aimed to examine the effects of switching from clopidogrel to prasugrel on PRU in patients having received long-term DAPT (aspirin + clopidogrel) after PCI with coronary stent implantation, along with CYP2C19 genotype test results.
Methods
Study design
This multicenter, randomized, open-label, parallel-group comparison study was conducted at eight sites in the Kyushu region, Japan, from April 2017 to August 2018. An ethical review committee at each site approved the conduct of this study. The study was conducted in accordance with the Declaration of Helsinki, ethical guidelines for clinical research, ethical guidelines for human genome/gene analysis research, and the Act on Protection of Personal Information, and followed the ICH-GCP guidelines. Monitoring and auditing were also conducted by a third-party organization to ensure the reliability of the data. The present study was registered at the University Hospital Medical Information Network Clinical Trials Registry (UMIN000027089) in Japan.
Patient selection
Patients who met all the following inclusion criteria were enrolled: (1) underwent coronary stent implantation and were consistently with DAPT (aspirin + clopidogrel) for 52 weeks or more; (2) 20 years of age or older; (3) have provided written consent to participate; (4) provided consent on collection and analysis of samples for genetic analysis; and (5) can understand the nature of the study and follow its procedures, in the opinion of the principal investigator.
Patients were excluded if any of following criteria were met (1) bleeding tendencies or diathesis; (2) severe hepatic impairment; (3) severe renal impairment; (4) poor blood pressure control during antihypertensive therapy; (5) history of cerebral infarction or transient ischemic attack; (6) history of hypersensitivity to thienopyridine drugs; (7) pregnant, suspected to be pregnant, wish to be pregnant, or lactating; (8) those the investigator has determined are unable to provide sufficient understanding and cooperation due to mental incapacity (including moderate and severe dementia); (9) scheduled, or must be hospitalized during the observation period, at the discretion of the investigator, or were hospitalized during the period from providing consent to determining eligibility (except when hospitalized for tests); (10) must receive treatment with prohibited concomitant drugs during observation period; and (11) others judged ineligible by investigator.
Treatment
After confirming eligibility of coronary heart disease patients who underwent coronary stent implantation and were consistently with DAPT (aspirin + clopidogrel) for 52 weeks or more, written informed consent was obtained from all enrolled in the study.
At enrollment, characteristics of these patients were aggregated as baseline data, PRU was measured using VerifyNow® assay (Instrumentation Laboratory, Bedford, MA, USA), and CYP2C19 genotype test was performed. The CYP2C19 genotype test results were disclosed to all doctors and patients after completion of this study. Patients with baseline PRU ≥ 208 were randomly assigned (1:1) via an interactive web response system (IWRS), and by a minimization method using PRU as an allocation adjustment factor, into either continuing to receive clopidogrel (hereinafter “Continued Group”) or switching to prasugrel (hereinafter “Switched Group”). The PRU cutoff value was set at 208, in line with ADAPT-DES study [11, 12]. Continued Group remained on the same dosing regimen. Duration of treatment was 12 weeks, during which aspirin (81–100 mg/day) was co-administered in both groups. PRU was measured at the end of 12 weeks of treatment. The following drugs were contraindicated for co-administration during treatment period: (1) aspirin (excluding its use as basal therapy) and other antiplatelet agents, (2) oral anticoagulants, and (3) drugs prohibited from concomitant use specified in the package inserts.
Endpoints
The primary endpoint was rate (%) of patients who achieved PRU < 208 at the end of 12 weeks. The secondary endpoints were as follows: proportion of DAPT score; examine change in PRU in Continued and Switched Groups from baseline to week 12, as well as according to CYP2C19 polymorphism (EM and non-EM (IM and PM) Groups); incidence of bleeding and cardiovascular events; and PRU at baseline according to CYP2C19 polymorphism.
Statistical analysis
A two-sided test with significance level of 5% was used to calculate a 95% confidence interval.
Sample size
Based on the previous study [25], the rate of patients who achieved PRU < 208 in the groups continued on prasugrel and switched to clopidogrel was 94.3% and 69.0%, respectively. Assuming a similar rate in this study and using detection power of 80% and significance level of 5%, the required number of patients was 41 per group. In consideration of dropouts, the target sample size of this study was determined as 90 patients (45 patients per group).
Primary analysis
The primary analysis was evaluated using a Fisher’s exact test to compare rates of patients, between Continued and Switched Groups in the full analysis set (FAS), who achieved PRU < 208 at the end of 12 weeks.
Secondary analysis
Baseline characteristics (including age, gender, medical history, and complications) for all enrolled patients were provided according to PRU (PRU ≥ 208 or PRU < 208), a t test or Fisher’s exact test was performed to compare the groups. Patients assigned to Continued and Switched Groups in the FAS were compared in the same manner. In the FAS, a t test was performed for comparison of change (± SD) in PRU from baseline to week 12, between these two treatment groups, as well as among CYP2C19 polymorphism (EM and non-EM Groups). Additionally, incidence of cardiovascular events was calculated according to these groups in the FAS. Incidence of bleeding events was also calculated in the safety analysis set (SAF), which is further aggregated according to the Bleeding Academic Research Consortium (BARC) criteria. PRU in all patients were compared according to CYP2C19 polymorphism (EM, IM, and PM).
Results
Study population
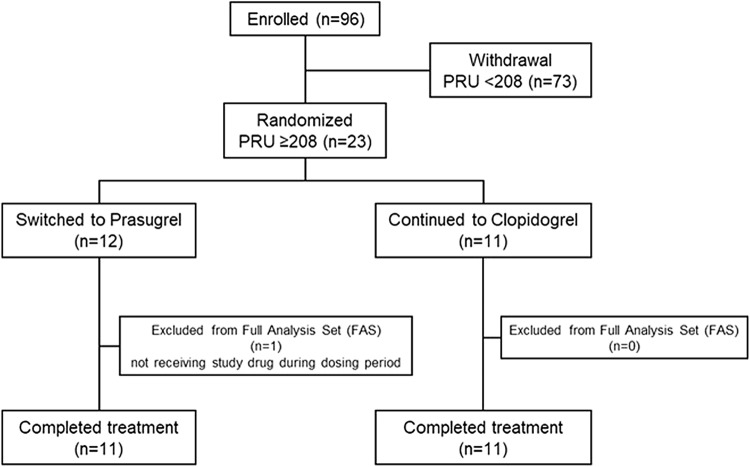
The flowchart of patients through the study is shown in Fig. 1. A total of 96 patients were enrolled, of which 73 (approximately 76%) had PRU < 208, and 23 (approximately 24%) had PRU ≥ 208. The patients who had PRU ≥ 208 were randomly assigned into either Continued Group (n = 11) or Switched Group (n = 12), and 11 in each group completed the 12 weeks of treatment. All in Continued Group received clopidogrel 75 mg daily. In Switched Group, 10 patients received prasugrel 3.75 mg daily, and 1 patient received 2.5 mg daily. Baseline patient characteristics are shown in Tables 1 and 2. As shown in Table 1, overall median DAPT duration was 1824.0 days (range 375–3603) after PCI with coronary stent implantation, and 55 patients (57.3%) had a DAPT score of ≥ 2. The median duration of treatment with clopidogrel was 1866.0 days (range 161–3473). The CYP2C19 genotype test identified 34 patients (35.4%) as EM, 50 (52.1%) as IM, and 12 (12.5%) as PM. The baseline PRU according to CYP2C19 polymorphism was 143.5 ± 59.7 in EM, 173.3 ± 56.3 in IM and 206.4 ± 49.8 in PM, indicating that the PRU were significantly higher in IM and PM, compared to EM. Though the PRU in PM was higher than that in IM, there was no statistically significant difference (Fig. 2). When patients with PRU ≥ 208 were compared to those with PRU < 208, the non-EM group demonstrated higher proportion, 78.3% and 60.3%, respectively, and included more patients of advanced age, females, lower height and lower body weight. In addition, fewer patients with a history of unstable angina were in the group with PRU ≥ 208, compared to those with PRU < 208. With respect to Table 2, no difference was observed other than a high percentage in Continued Group with previous myocardial infarction.
Fig. 1.
Study flowchart
Table 1.
Baseline characteristics
| Overall n = 96 |
PRU < 208 n = 73 |
PRU ≥ 208 n = 23 |
p value | |
|---|---|---|---|---|
| Gender, n (%) | ||||
| Male | 75 (78.1) | 62 (84.9) | 13 (56.5) | 0.008 |
| Female | 21 (21.9) | 11 (15.1) | 10 (43.5) | |
| Age, years | ||||
| Mean ± SD | 69.9 ± 9.6 | 68.6 ± 9.9 | 74.0 ± 7.3 | 0.020 |
| Median [range] | 71.0 [42–89] | 69.0 [42–89] | 74.0 [60–89] | |
| Height, cm | ||||
| Mean ± SD | 161.73 ± 7.22 | 162.58 ± 7.17 | 159.00 ± 6.84 | 0.038 |
| Median [range] | 162.95 [144.6–173.0] | 164.50 [144.6–173.0] | 158.50 [147.8–172.5] | |
| BMI, kg/m2 | ||||
| Mean ± SD | 25.06 ± 3.27 | 25.40 ± 3.49 | 23.96 ± 2.16 | 0.064 |
| Median [range] | 24.90 [15.1–36.4] | 25.42 [15.1–36.4] | 24.06 [20.3–27.5] | |
| Weight, kg | ||||
| Mean ± SD | 65.76 ± 10.74 | 67.36 ± 11.11 | 60.70 ± 7.69 | 0.009 |
| Median [range] | 65.10 [33.5–91.0] | 68.70 [33.5–91.0] | 61.60 [44.7–77.2] | |
| Smoking history, n (%) | ||||
| Never | 47 (49.0) | 32 (43.8) | 15 (65.2) | 0.095 |
| Yes | 49 (51.0) | 41 (56.2) | 8 (34.8) | |
| Medical history, n (%) | ||||
| Myocardial infarction | 54 (56.3) | 42 (57.5) | 12 (52.2) | 0.810 |
| Unstable angina | 25 (26.0) | 23(31.5) | 2 (8.7) | 0.032 |
| Ischemic stroke | 0 (0.0) | 0 (0.0) | 0 (0.0) | – |
| Hemorrhage intracranial | 0 (0.0) | 0 (0.0) | 0 (0.0) | – |
| Arteriosclerosis | 23 (24.0) | 17 (23.3) | 6 (26.1) | 0.784 |
| Stable angina pectoris | 30 (31.3) | 20 (27.4) | 10 (43.5) | 0.197 |
| Complication, n (%) | ||||
| Hypertension | 91 (94.8) | 69 (94.5) | 22 (95.7) | 1.000 |
| Dyslipidemia | 90 (93.8) | 67 (91.8) | 23 (100.0) | 0.330 |
| Diabetes mellitus | 58 (60.4) | 44 (60.3) | 14 (60.9) | 1.000 |
| Hepatic function disorder | 3 (3.1) | 2 (2.7) | 1(4.3) | 0.565 |
| Renal function disorder | 11 (11.5) | 6 (8.2) | 5 (21.7) | 0.126 |
| Atrial fibrillation | 1 (1.0) | 0 (0.0) | 1 (4.3) | 0.240 |
| Clopidogrel dose, mg | ||||
| Mean ± SD | 74.7 ± 2.6 | 74.7 ± 2.9 | 75.0 ± 0.0 | 0.577 |
| Median [range] | 75.0 [50–75] | 75.0 [50–75] | 75.0 [75–75] | |
| Duration of DAPT, days | ||||
| Mean ± SD | 1784.7 ± 834.0 | 1793.9 ± 847.3 | 1757.6 ± 811.3 | 0.858 |
| Median [range] | 1824.0 [375–3603] | 1696.0 [375–3603] | 1866.0 [404–3473] | |
| Duration of Clopidogrel administration, days | ||||
| Mean ± SD | 1785.4 ± 838.8 | 1797.0 ± 846.6 | 1751.2 ± 833.2 | 0.823 |
| Median [range] | 1866.0 [161–3473] | 1866.0 [346–3436] | 1866.0 [161–3473] | |
| PRU at baseline | ||||
| Mean ± SD | 166.9 ± 59.8 | 144.1 ± 47.0 | 239.3 ± 31.7 | < 0.001 |
| Median [range] | 165.0 [5–341] | 155.0 [5–207] | 228.0 [208–341] | |
| CYP2C19 polymorphism, n (%) | ||||
| EM | 34 (35.4) | 29 (39.7) | 5 (21.7) | 0.228 |
| IM | 50 (52.1) | 36 (49.3) | 14 (60.9) | |
| PM | 12 (12.5) | 8 (11.0) | 4 (17.4) | |
| IM + PM | 62 (64.6) | 44 (60.3) | 18 (78.3) | 0.139a |
| DAPT score, n (%) | ||||
| < 2 | 32 (33.3) | 22 (30.1) | 10 (43.5) | 0.301 |
| ≥ 2 | 55 (57.3) | 44 (60.3) | 11 (47.8) | |
An independent t test was used for measurement data, and a Fisher’s exact test was performed for count data
EM extensive metabolizer, IM intermediate metabolizer, PM poor metabolizer
aCompared with EM
Table 2.
Baseline characteristics by treatment group (PRU ≥ 208)
| Switched to prasugrel n = 11 |
Continued clopidogrel n = 11 |
p value | |
|---|---|---|---|
| Gender, n (%) | |||
| Male | 6 (54.5) | 6 (54.5) | 1.000 |
| Female | 5 (45.5) | 5 (45.5) | |
| Age, years | |||
| Mean ± SD | 76.0 ± 8.0 | 71.7 ± 6.6 | 0.187 |
| Median [range] | 74.0 [64–89] | 72.0 [60–80] | |
| Height, cm | |||
| Mean ± SD | 159.84 ± 7.50 | 158.38 ± 6.70 | 0.637 |
| Median [range] | 158.50[151.3–172.5] | 160.60[147.8–166.3] | |
| BMI, kg/m2 | |||
| Mean ± SD | 23.74 ± 2.49 | 24.33 ± 1.88 | 0.533 |
| Median [range] | 23.30[20.3–27.5] | 24.66[20.3–26.6] | |
| Weight, kg | |||
| Mean ± SD | 60.69 ± 8.04 | 61.25 ± 7.83 | 0.869 |
| Median [range] | 60.40 [50.0–77.2] | 62.00 [44.7–71.6] | |
| Smoking history, n (%) | |||
| Never | 7 (63.6) | 7 (63.6) | 1.000 |
| Yes | 4 (36.4) | 4 (36.4) | |
| Medical history, n (%) | |||
| Myocardial infarction | 3 (27.3) | 9 (81.8) | 0.030 |
| Unstable angina | 2 (18.2) | 0 (0.0) | 0.476 |
| Ischemic stroke | 0 (0.0) | 0 (0.0) | – |
| Hemorrhage intracranial | 0 (0.0) | 0 (0.0) | – |
| Arteriosclerosis | 4 (36.4) | 1 (9.1) | 0.311 |
| Stable angina pectoris | 7 (63.6) | 3 (27.3) | 0.198 |
| Complication, n (%) | |||
| Hypertension | 10 (90.9) | 11 (100.0) | 1.000 |
| Dyslipidemia | 11 (100.0) | 11 (100.0) | – |
| Diabetes mellitus | 7 (63.6) | 7 (63.6) | 1.000 |
| Hepatic function disorder | 1 (9.1) | 0 (0.0) | 1.000 |
| Renal function disorder | 2 (18.2) | 3 (27.3) | 1.000 |
| Atrial fibrillation | 0 (0.0) | 0 (0.0) | – |
| Clopidogrel dose, mg | |||
| Mean ± SD | 75.0 ± 0.0 | 75.0 ± 0.0 | – |
| Median [range] | 75.0 [75–75] | 75.0 [75–75] | |
| Duration of DAPT, days | |||
| Mean ± SD | 1942.6 ± 882.7 | 1558.5 ± 764.9 | 0.288 |
| Median [range] | 1937.0 [591–3473] | 1505.0 [404–3051] | |
| Duration of Clopidogrel administration, days | |||
| Mean ± SD | 1941.5 ± 884.5 | 1546.4 ± 810.3 | 0.288 |
| Median [range] | 1937.0 [591–3473] | 1505.0 [161–3051] | |
| PRU at baseline | |||
| Mean ± SD | 238.2 ± 37.9 | 238.2 ± 26.7 | 1.000 |
| Median [range] | 227.0 [208–341] | 228.0 [208–293] | |
| CYP2C19 polymorphism, n (%) | |||
| EM | 2 (18.2) | 3 (27.3) | 1.000 |
| IM | 7 (63.6) | 6 (54.5) | |
| PM | 2 (18.2) | 2 (18.2) | |
| IM + PM | 9 (81.8) | 8 (72.7) | 1.000a |
| DAPT score | |||
| < 2 | 7 (63.6) | 2 (18.2) | 0.070 |
| ≥ 2 | 3 (27.3) | 8 (72.7) | |
| Dose after randomization, mg | |||
| Mean ± SD | 3.636 ± 0.377 | 75.0 ± 0.0 | – |
| Median [range] | 3.750 [2.50–3.75] | 75.0 [75–75] | |
An independent t test was used for measurement data, and a Fisher’s exact test was performed for count data
EM extensive metabolizer, IM intermediate metabolizer, PM poor metabolizer
aCompared with EM
Fig. 2.
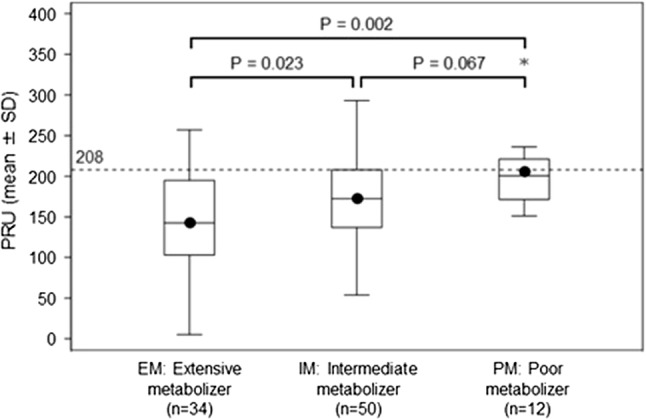
PRU at baseline by CYP2C19 polymorphism. Black dots (•) represent the mean of PRU on each metabolizers. In a box plot, central line/upper edge line represents median/the third quartile/the first quartile. Upper end of the whisker: the maximum value not exceeding the third quartile + 1.5 × interquartile range (IQR). Asterisk (*) indicates an outlier (value that is larger than the upper end of the whisker or smaller than the end of the whisker)
Primary endpoint
As shown in Fig. 3, the rate of patients who achieved PRU < 208 at the end of week 12 after randomization was significantly higher in Switched Group (9/10 patients, 90.0%), relative to Continued Group (4/11 patients, 36.4%) (P = 0.024). Among 11 patients assigned to Switched Group, one was excluded from the denominator because PRU at the end of week 12 was not measured.
Fig. 3.
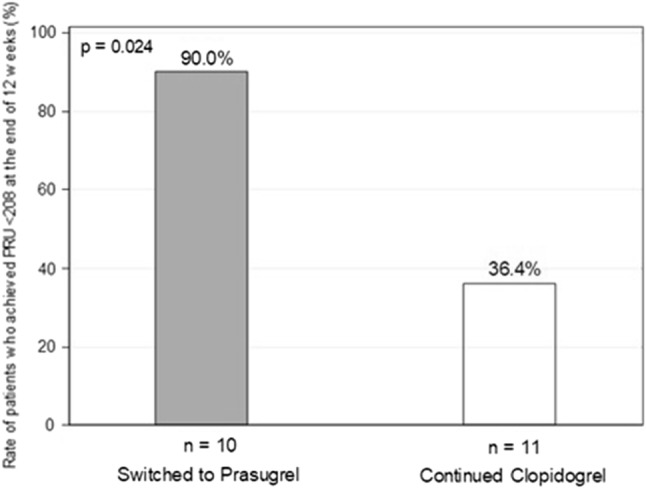
Rate of patients who achieved PRU < 208 at the end of 12 weeks. In “Switched to Prasugrel” group, one patient was excluded from the denominator because PRU at the end of 12 weeks was not measured. PRU was measured by VerifyNow described in “Methods”
Secondary endpoint
PRU at baseline had been 238.2 ± 26.7 in Continued Group and 238.2 ± 37.9 in Switched Group (P = 1.000), though at week 12 changed to 220 ± 42.8 and 153.6 ± 44.8, respectively (P = 0.002), demonstrating significant reduction in PRU in Switched Group (Fig. 4a). When examined according to CYP2C19 polymorphism, PRU at baseline in EM Group had been 234.7 ± 19.9 in Continued Group and 216.5 ± 12.0 in Switched Group (P = 0.341), at week 12 changed to 202.3 ± 60.0 and 174.5 ± 22.3, respectively (P = 0.591), with no difference between these groups (Fig. 4b). In non-EM Group, as well, no difference was observed in PRU at baseline between Continued and Switched Groups (239.5 ± 30.0 and 243.0 ± 40.4, P = 0.844), however, at week 12 changed to 229.4 ± 36.9 and 148.4 ± 48.4, respectively (P = 0.002), demonstrating significant reduction in PRU in Switched Group (Fig. 4c).
Fig. 4.
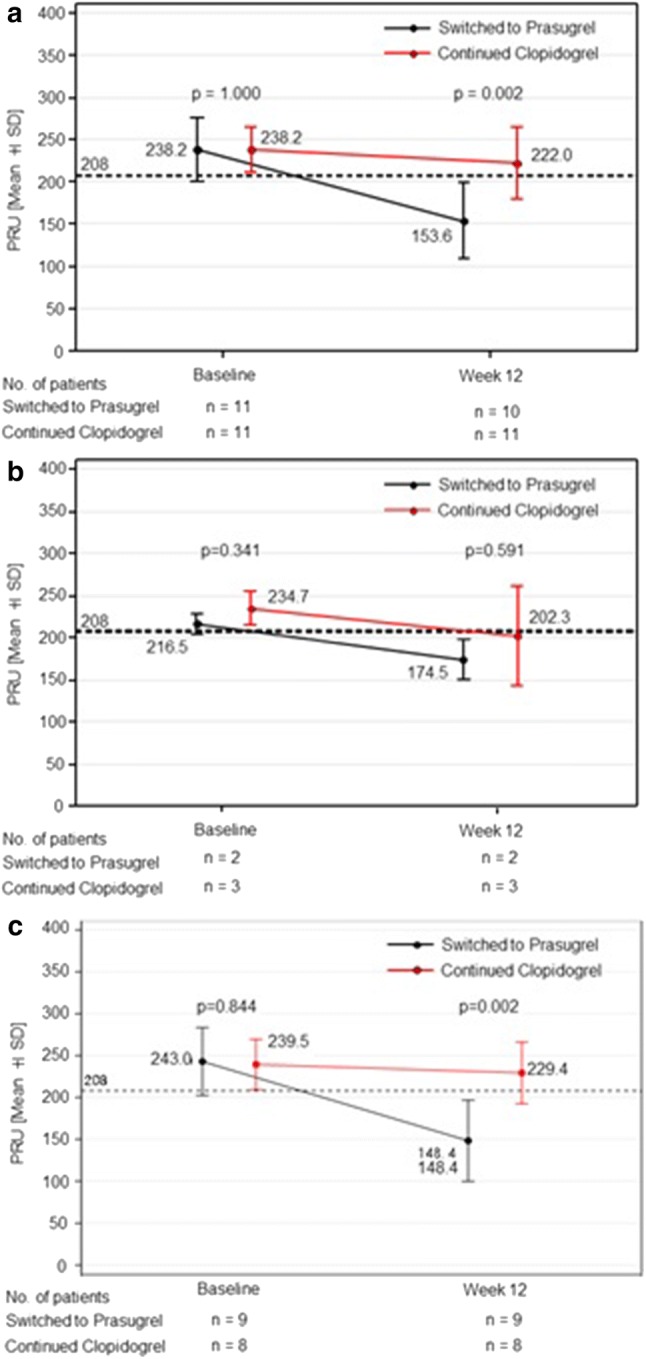
Change from baseline to week 12 in PRU per treatment group. a PRU were measured at baseline and week 12. The mean of PRU on all patients of “Switched to Prasugrel” and “Continued Clopidogrel” were compared. b The mean of PRU on extensive metabolizer (EM) patients of “Switched to Prasugrel” and “Continued Clopidogrel” were compared. c The mean of PRU on intermediate metabolizer (IM) + poor metabolizer (PM) patients of “Switched to Prasugrel” and “Continued Clopidogrel” were compared
No cardiovascular events were observed in either group during the study period. Bleeding events (BARC Type 1) were observed in both treatment groups (2 cases, including nosebleed and subcutaneous bleeding in Continued Group, 1 case of subcutaneous bleeding in Switched Group). Other adverse events were experienced in 5 out of 11 patients in Continued Group (including one serious adverse event: vertebral compression fracture), and in 4 out of 11 in Switched Group (including one serious adverse event: influenza).
Discussion
This study enrolled patients who had been chronically with DAPT (aspirin + clopidogrel) after PCI with coronary stent implantation. PRU were assessed for all patients, and those with PRU ≥ 208 were randomly assigned to Continued Group or Switched Group to evaluate PRU at the end of week 12 of treatment. The rate of patients who achieved PRU < 208 at week 12 was significantly higher in Switched Group relative to Continued Group (90.0% vs. 36.4%). Based on the results of the CYP2C19 genotype test for all patients in this study, the proportions with EM, IM, and PM were 35.4% (34 patients), 52.1% (50 patients), and 12.5% (12 patients), respectively. Compared among the enrolled patients, non-EM Group showed a higher proportion in PRU ≥ 208. Furthermore, there were no cardiovascular or bleeding events with statistically significant differences in either group during the study period.
Examined PRU in patients with long-term DAPT
All patients in this study had been chronically with DAPT (aspirin + clopidogrel) for approximately 5 years (median DAPT duration). About 60% had a DAPT score of ≥ 2, indicating that long-term DAPT treatment was generally appropriate. Few studies have evaluated the antiplatelet effects based on PRU in patients with long-term DAPT duration over 5 years. This study investigated these patients using the PRU cutoff value of 208, at which the risk of cardiovascular events showed significantly higher in the ADAPT-DES study [11, 12], and found a high proportion (a quarter patients) were high-risk with PRU ≥ 208. Since this study was conducted in a small number of patients, these results should be confirmed in a study of larger size.
Switching between P2Y12 inhibitors in patients with long-term DAPT
In our previous study, the CONTINUE VERSUS SWITCH-Kyushu study [25], patients after PCI with coronary stent implantation were treated with prasugrel for 2 weeks, and randomly assigned into either continuing prasugrel or switched to clopidogrel, for the assessment of PRU at week 4 from randomization. The rate of patients who achieved PRU < 208 at week 4 in groups continued prasugrel and switched to clopidogrel was 94.7% and 66.1%, respectively. This study found that the rate of patients who achieved PRU < 208 at week 12 in Switched Group was significantly higher relative to Continued Group (90.0% vs. 36.4%). It is also found that even those with long-term DAPT could reduce their PRU by switching from clopidogrel to prasugrel. The reason why the patients in Switched Group did not achieve PRU < 208 is a future consideration.
Due to the difference in timing of PRU measurement between the ADAPT-DES study and this study, the risk of cardiovascular events in patients with PRU ≥ 208 assessed after long-term DAPT has not been established. It is not rare in healthcare settings that long-term DAPT is required for patients who had placed a first-generation drug-eluting stent, patients with complex PCI, and judged to have a high risk of cardiovascular events, based on such indicators as DAPT score. Although PRU measurement is not generally practiced at all medical facilities, switching from clopidogrel to prasugrel under appropriate risk management based on PRU could be an option for treatment in patients with a potentially high risk of cardiovascular events.
Examined CYP2C19 polymorphism and PRU in patients with long-term DAPT
This study has established that PRU at baseline in IM and PM patients was significantly higher compared to that in EM patients, even after long-term DAPT (aspirin + clopidogrel). In addition, non-EM Group with PRU ≥ 208 in Switched Group steadily decreased PRU compared to Continued Group, with less affected by CYP2C19 polymorphism. Recent meta-analyses studies have reported the frequency of cardiovascular events higher in patients treated with clopidogrel who carry CYP2C19 loss-of-function alleles, compared to patients without the alleles [15, 16]. Additionally, a personalized approach of selecting appropriate antiplatelet agents for patients with CYP2C19 loss-of-function alleles is reported to have reduced the incidence of cardiovascular events [26, 27]. Similar to PRU measurement, it is difficult to perform CYP2C19 genotype testing at all medical facilities. However, prevalence of PM in the Japanese population is approximately 20%, it may be preferable to select an appropriate P2Y12 inhibitor after CYP2C19 genotype test, to reduce the cardiovascular events after DAPT.
Switching between P2Y12 inhibitors and bleeding events
Risk of bleeding events is a recent topic, often mentioned with respect to antiplatelet agents in the field of PCI. The PRASFIT-ACS and PRASFIT-Elective studies conducted in Japan reported that risk of bleeding events was female sex, age ≥ 75 years, and weight ≤ 50 kg [28]. The present study also found that patients with PRU ≥ 208 after long-term DAPT (aspirin + clopidogrel) included more females, more with advanced age and lower body weight, compared to those with PRU < 208. After switching treatment from clopidogrel to prasugrel in these patients, no major bleeding events were observed, and the incidence of minor bleeding events was similar to that in Continued Group. While further consideration is required, the Japanese large-scale studies in patients with cardiac or brain diseases demonstrated the equivalent safety with respect to the incidence of major bleeding events between clopidogrel 75 mg daily prasugrel 3.75 mg daily [17, 19, 29].
The overseas guidelines recommend an early switch from DAPT to single antiplatelet therapy (SAPT) for patients with risk of bleeding events, and some clinical research is ongoing in Japan to investigate the appropriateness of shortening DAPT duration. When changing treatment to SAPT, there are more than a few cases to consider the option of SAPT with a thienopyridine drug, since there are multiple reports on aspirin associated with risk of gastrointestinal and intracranial bleeding [30–32]. In such cases, to reduce future incidence of cardiovascular events, it may be necessary to select an antiplatelet agent in which PRU exhibits an appropriate therapeutic window.
Limitation
In this study, the target number of patients suggested by the rationale could not be collected in this study period. The reasons for this include the small number of patients who had been with long-term DAPT (aspirin + clopidogrel) in each site, different distribution of CYP2C19 polymorphism compared to previous reports, and lower than assumed PRU in patients with CYP2C19 polymorphism. However, the study’s primary endpoint was achieved. In this study, the PRU cutoff value was defined as 208 according to previous studies for patients within 2 years after PCI [11, 12]. Moreover, Asian patients enrolled in the previous studies were very few. Further investigation is required to determine the optimal cutoff value in Japanese patients more than 2 years after PCI.
Conclusion
For patients with long-term DAPT (aspirin + clopidogrel) after PCI with coronary stent implantation, switching from clopidogrel to prasugrel resulted in stable reduction in PRU, regardless of CYP2C19 polymorphism. Further examination is required to investigate whether or not the results of this study lead to a reduction in cardiovascular events.
Acknowledgements
The CONVERT 2 study was supported by Daiichi Sankyo Co., Ltd. The authors are also grateful to the clinical research associates at all sites for their cooperation in this study. We also thank the following collaborators for their support: Nobuhiro Tahara, Shinji Yokoyama, Masanori Ohtsuka, Takaharu Nakayoshi, Masahiro Sasaki, Motoki Sasaki, Satoko Ohno, Yoshiko Rikitake, Shoko Maeda, Toshiyuki Yanai, Tatsuhiro Shibata and Koutatsu Shimozono of Division of Cardiovascular Medicine, Department of Internal Medicine, Kurume University School of Medicine; Kyoko Umeji, Ryota Fukuoka, Toshiya Soejima and Hisashi Koga of Department of Cardiology, Cardiovascular Center, ShinKoga Hospital; Yoritaka Otsuka and Takumi Yoshiga of Division of Cardiology, Sugi Hospital; Katsuhiko Takenaka and Yukimitu Kuwabara of Department of Cardiology, National Hospital Organization Kyushu Medical Center; Hideki Ohshima, Haruya Ohmura and Norihito Okina of Division of Cardiovascular Internal Medicine, Asakura Medical Assosiation Hospital; Yuuichi Hattori, Shisei Sonezaki and Ichiro Onitsuka of Division of Cardiovascular Internal Medicine, Tanushimaru Chuo Hospital; Yuji Murakami and Yutaka Fukuizumi of Division of Cardiovascular Internal Medicine, Fukuoka Sanno Hospital; Shuichiro Sagara, Susumu Takase, Takeo Yufu and Kenji Sadamatu of Division of Cardiovascular Internal Medicine, St. Mary’s Hospital.
Compliance with ethical standards
Conflict of interest
The authors declare the following interests: Hiroyoshi Yokoi has received a speaker honorarium from Daiichi Sankyo Co., Ltd., Sanofi K.K. and Bayer Yakuhin, Ltd. Yoshihiro Fukumoto has received a speaker honorarium from Daiichi Sankyo Co., Ltd. Takafumi Ueno has received a speaker honorarium from Daiichi Sankyo Co., Ltd. The other authors have nothing to disclose regarding the current study.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L, Mehran R, Mukherjee D, Newby LK, O'Gara PT, Sabatine MS, Smith PK, Smith SC., Jr 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2016;68(10):1082–1115. doi: 10.1016/j.jacc.2016.03.513. [DOI] [PubMed] [Google Scholar]
- 2.Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, Jüni P, Kastrati A, Kolh P, Mauri L, Montalescot G, Neumann FJ, Petricevic M, Roffi M, Steg PG, Windecker S, Zamorano JL, Levine GN, ESC Scientific Document Group. ESC Committee for Practice Guidelines (CPG) ESC National Cardiac Societies 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS) Eur Heart J. 2018;39(3):213–260. doi: 10.1093/eurheartj/ehx419. [DOI] [PubMed] [Google Scholar]
- 3.The Japanese Circulation Society et al (2009) Guidelines for management of anticoagulant and antiplatelet therapy in cardiovascular disease. JCS. https://www.j-circ.or.jp/guideline/pdf/JCS2009_hori_h.pdf. Accessed 5 Feb 2019 [PubMed]
- 4.Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias W, Braunwald E, Sabatine MS. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360:354–362. doi: 10.1056/NEJMoa0809171. [DOI] [PubMed] [Google Scholar]
- 5.Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E, Méneveau N, Steg PG, Ferrières J, Danchin N, Becquemont L, French Registry of Acute ST-Elevation and Non-ST-Elevation Myocardial Infarction (FAST-MI) Investigators Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med. 2009;360:363–375. doi: 10.1056/NEJMoa0808227. [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto K, Hokimoto S, Chitose T, Morita K, Ono T, Kaikita K, Tsujita K, Abe T, Deguchi M, Miyagawa H, Saruwatari J, Sumida H, Sugiyama S, Nakagawa K, Ogawa H. Impact of CYP2C19 gene polymorphism on residual platelet reactivity in patients with coronary heart disease during antiplatelet therapy. J Cardiol. 2011;57(2):194–201. doi: 10.1016/j.jjcc.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 7.Li S, Choi JL, Guo LZ, Goh RY, Kim BR, Woo KS, Kim MH, Han JY. Correlation between the CYP2C19 phenotype status and the results of three different platelet function tests in cardiovascular disease patients receiving antiplatelet therapy: an emphasis on newly introduced platelet function analyzer-200 P2Y test. Ann Lab Med. 2016;36(1):42–48. doi: 10.3343/alm.2016.36.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myrand SP, Sekiguchi K, Man MZ, Lin X, Tzeng RY, Teng CH, Hee B, Garrett M, Kikkawa H, Lin CY, Eddy SM, Dostalik J, Mount J, Azuma J, Fujio Y, Jang IJ, Shin SG, Bleavins MR, Williams JA, Paulauskis JD, Wilner KD. Pharmacokinetics/genotype associations for major cytochrome P450 enzymes in native and first- and third-generation Japanese populations: comparison with Korean, Chinese, and Caucasian populations. Clin Pharmacol Ther. 2008;84(3):347–361. doi: 10.1038/sj.clpt.6100482. [DOI] [PubMed] [Google Scholar]
- 9.Tantry US, Bonello L, Aradi D, Price MJ, Jeong YH, Angiolillo DJ, Stone GW, Curzen N, Geisler T, Ten Berg J, Kirtane A, Siller-Matula J, Mahla E, Becker RC, Bhatt DL, Waksman R, Rao SV, Alexopoulos D, Marcucci R, Reny JL, Trenk D, Sibbing D, Gurbel PA, Working Group on On-Treatment Platelet Reactivity Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013;62(24):2261–2273. doi: 10.1016/j.jacc.2013.07.101. [DOI] [PubMed] [Google Scholar]
- 10.Aradi D, Kirtane A, Bonello L, Gurbel PA, Tantry US, Huber K, Freynhofer MK, ten Berg J, Janssen P, Angiolillo DJ, Siller-Matula JM, Marcucci R, Patti G, Mangiacapra F, Valgimigli M, Morel O, Palmerini T, Price MJ, Cuisset T, Kastrati A, Stone GW, Sibbing D. Bleeding and stent thrombosis on P2Y12-inhibitors: collaborative analysis on the role of platelet reactivity for risk stratification after percutaneous coronary intervention. Eur Heart J. 2015;36(27):1762–1771. doi: 10.1093/eurheartj/ehv104. [DOI] [PubMed] [Google Scholar]
- 11.Stone GW, Witzenbichler B, Weisz G, Rinaldi MJ, Neumann FJ, Metzger DC, Henry TD, Cox DA, Duffy PL, Mazzaferri E, Gurbel PA, Xu K, Parise H, Kirtane AJ, Brodie BR, Mehran R, Stuckey TD, Investigators ADAPT-DES. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet. 2013;382:614–623. doi: 10.1016/S0140-6736(13)61170-8. [DOI] [PubMed] [Google Scholar]
- 12.Stuckey TD, Kirtane AJ, Brodie BR, Witzenbichler B, Litherland C, Weisz G, Rinaldi MJ, Neumann FJ, Metzger DC, Henry TD, Cox DA, Duffy PL, Mazzaferri EL, Jr, Gurbel PA, Mehran R, Généreux P, Ben-Yehuda O, Simonton CA, Stone GW, Investigators ADAPT-DES. Impact of aspirin and clopidogrel hyporesponsiveness in patients treated with drug-eluting stents: 2-year results of a prospective, multicenter registry study. JACC Cardiovasc Interv. 2017;10(16):1607–1617. doi: 10.1016/j.jcin.2017.05.059. [DOI] [PubMed] [Google Scholar]
- 13.Campo G, Parrinello G, Ferraresi P, Lunghi B, Tebaldi M, Miccoli M, Marchesini J, Bernardi F, Ferrari R, Valgimigli M. Prospective evaluation of on-clopidogrel platelet reactivity over time in patients treated with percutaneous coronary intervention relationship with gene polymorphisms and clinical outcome. J Am Coll Cardiol. 2011;57(25):2474–2483. doi: 10.1016/j.jacc.2010.12.047. [DOI] [PubMed] [Google Scholar]
- 14.Hwang SJ, Jeong YH, Kim IS, Koh JS, Kang MK, Park Y, Kwak CH, Hwang JY. The cytochrome 2C19*2 and *3 alleles attenuate response to clopidogrel similarly in East Asian patients undergoing elective percutaneous coronary intervention. Thromb Res. 2011;127(1):23–28. doi: 10.1016/j.thromres.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Xi Z, Fang F, Wang J, AlHelal J, Zhou Y, Liu W. CYP2C19 genotype and adverse cardiovascular outcomes after stent implantation in clopidogrel-treated Asian populations: a systematic review and meta-analysis. Platelets. 2017;30(2):229–240. doi: 10.1080/09537104.2017.1413178. [DOI] [PubMed] [Google Scholar]
- 16.Pan Y, Chen W, Xu Y, Yi X, Han Y, Yang Q, Li X, Huang L, Johnston SC, Zhao X, Liu L, Zhang Q, Wang G, Wang Y, Wang Y. Genetic polymorphisms and clopidogrel efficacy for acute ischemic stroke or transient ischemic attack: a systematic review and meta-analysis. Circulation. 2017;135(1):21–33. doi: 10.1161/CIRCULATIONAHA.116.024913. [DOI] [PubMed] [Google Scholar]
- 17.Toba T, Shinke T, Otake H, Sugizaki Y, Takeshige R, Onishi H, Nagasawa A, Tsukiyama Y, Yanaka K, Nagano Y, Yamamoto H, Kawamori H, Matsuura A, Ishihara T, Matsumoto D, Igarashi N, Hayashi T, Yasaka Y, Kadotani M, Fujii T, Shite J, Okada M, Sakakibara T, Hirata KI. Impact of dual antiplatelet therapy with adjusted-dose prasugrel on mid-term vascular response in patients undergoing elective percutaneous coronary intervention with everolimus-eluting stents. Heart Vessels. 2019;34(6):936–947. doi: 10.1007/s00380-018-1322-2. [DOI] [PubMed] [Google Scholar]
- 18.Saito S, Isshiki T, Kimura T, Ogawa H, Yokoi H, Nanto S, Takayama M, Kitagawa K, Nishikawa M, Miyazaki S, Nakamura M. Efficacy and safety of adjusted-dose prasugrel compared with clopidogrel in Japanese patients with acute coronary syndrome: the PRASFIT-ACS study. Circ J. 2014;78(7):1684–1692. doi: 10.1253/circj.CJ-13-1482. [DOI] [PubMed] [Google Scholar]
- 19.Ogawa H, Isshiki T, Kimura T, Yokoi H, Nanto S, Takayama M, Kitagawa K, Nishikawa M, Miyazaki S, Ikeda Y, Nakamura M, Tanaka Y, Saito S. Effects of CYP2C19 allelic variants on inhibition of platelet aggregation and major adverse cardiovascular events in Japanese patients with acute coronary syndrome: The PRASFIT-ACS study. J Cardiol. 2016;68(1):29–36. doi: 10.1016/j.jjcc.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 20.Isshiki T, Kimura T, Ogawa H, Yokoi H, Nanto S, Takayama M, Kitagawa K, Nishikawa M, Miyazaki S, Ikeda Y, Nakamura M, Saito S, PRASFIT-Elective Investigators Prasugrel, a third-generation P2Y12 receptor antagonist, in patients with coronary artery disease undergoing elective percutaneous coronary intervention. Circ J. 2014;78(12):2926–2934. doi: 10.1253/circj.CJ-14-0266. [DOI] [PubMed] [Google Scholar]
- 21.Angiolillo DJ, Saucedo JF, Deraad R, Frelinger AL, Gurbel PA, Costigan TM, Jakubowski JA, Ojeh CK, Effron MB, Investigators SWAP. Increased platelet inhibition after switching from maintenance clopidogrel to prasugrel in patients with acute coronary syndromes: results of the SWAP (SWitching Anti Platelet) study. J Am Coll Cardiol. 2010;56(13):1017–1023. doi: 10.1016/j.jacc.2010.02.072. [DOI] [PubMed] [Google Scholar]
- 22.Trenk D, Stone GW, Gawaz M, Kastrati A, Angiolillo DJ, Müller U, Richardt G, Jakubowski JA, Neumann FJ. A randomized trial of prasugrel versus clopidogrel in patients with high platelet reactivity on clopidogrel after elective percutaneous coronary intervention with implantation of drug-eluting stents: results of the TRIGGER-PCI (Testing Platelet Reactivity In Patients Undergoing Elective Stent Placement on Clopidogrel to Guide Alternative Therapy With Prasugrel) study. J Am Coll Cardiol. 2012;59(24):2159–2164. doi: 10.1016/j.jacc.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 23.Bagai A, Peterson ED, McCoy LA, Effron MB, Zettler ME, Stone GW, Henry TD, Cohen DJ, Schulte PJ, Anstrom KJ, Wang TY. Association of measured platelet reactivity with changes in P2Y12 receptor inhibitor therapy and outcomes after myocardial infarction: Insights into routine clinical practice from the TReatment with ADP receptor iNhibitorS: Longitudinal Assessment of Treatment Patterns and Events after Acute Coronary Syndrome (TRANSLATE-ACS) study. Am Heart J. 2017;187:19–28. doi: 10.1016/j.ahj.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 24.Mauri L, Kereiakes DJ, Yeh RW, Driscoll-Shempp P, Cutlip DE, Steg PG, Normand SL, Braunwald E, Wiviott SD, Cohen DJ, Holmes DR, Jr, Krucoff MW, Hermiller J, Dauerman HL, Simon DI, Kandzari DE, Garratt KN, Lee DP, Pow TK, Ver Lee P, Rinaldi MJ, Massaro JM, DAPT Study Investigators Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med. 2014;371(23):2155–2166. doi: 10.1056/NEJMoa1409312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ueno T, Koiwaya H, Sasaki KI, Katsuki Y, Katsuda Y, Murasato Y, Shimamatsu J, Umeji K, Otsuka Y, Kawasaki T, Shibata Y, Fukumoto Y. Changes in P2Y12 reaction units after switching treatments from prasugrel to clopidogrel in Japanese patients with acute coronary syndrome followed by elective coronary stenting. Cardiovasc Interv Ther. 2017;32(4):341–350. doi: 10.1007/s12928-016-0417-x. [DOI] [PubMed] [Google Scholar]
- 26.Notarangelo FM, Maglietta G, Bevilacqua P, Cereda M, Merlini PA, Villani GQ, Moruzzi P, Patrizi G, Malagoli Tagliazucchi G, Crocamo A, Guidorossi A, Pigazzani F, Nicosia E, Paoli G, Bianchessi M, Comelli MA, Caminiti C, Ardissino D. Pharmacogenomic approach to selecting antiplatelet therapy in patients with acute coronary syndromes: the PHARMCLO trial. J Am Coll Cardiol. 2018;71(17):1869–1877. doi: 10.1016/j.jacc.2018.02.029. [DOI] [PubMed] [Google Scholar]
- 27.Cavallari LH, Lee CR, Beitelshees AL, Cooper-DeHoff RM, Duarte JD, Voora D, Kimmel SE, McDonough CW, Gong Y, Dave CV, Pratt VM, Alestock TD, Anderson RD, Alsip J, Ardati AK, Brott BC, Brown L, Chumnumwat S, Clare-Salzler MJ, Coons JC, Denny JC, Dillon C, Elsey AR, Hamadeh IS, Harada S, Hillegass WB, Hines L, Horenstein RB, Howell LA, Jeng LJB, Kelemen MD, Lee YM, Magvanjav O, Montasser M, Nelson DR, Nutescu EA, Nwaba DC, Pakyz RE, Palmer K, Peterson JF, Pollin TI, Quinn AH, Robinson SW, Schub J, Skaar TC, Smith DM, Sriramoju VB, Starostik P, Stys TP, Stevenson JM, Varunok N, Vesely MR, Wake DT, Weck KE, Weitzel KW, Wilke RA, Willig J, Zhao RY, Kreutz RP, Stouffer GA, Empey PE, Limdi NA, Shuldiner AR, Winterstein AG, Johnson JA, Network IGNITE. Multisite investigation of outcomes with implementation of CYP2C19 genotype-guided antiplatelet therapy after percutaneous coronary intervention. JACC Cardiovasc Interv. 2018;11(2):181–191. doi: 10.1016/j.jcin.2017.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nishikawa M, Isshiki T, Kimura T, Ogawa H, Yokoi H, Miyazaki S, Ikeda Y, Nakamura M, Tanaka Y, Saito S. Risk of bleeding and repeated bleeding events in prasugrel-treated patients: a review of data from the Japanese PRASFIT studies. Cardiovasc Interv Ther. 2017;32(2):93–105. doi: 10.1007/s12928-016-0452-7. [DOI] [PubMed] [Google Scholar]
- 29.Ogawa A, Toyoda K, Kitagawa K, Kitazono T, Nagao T, Yamagami H, Uchiyama S, Tanahashi N, Matsumoto M, Minematsu K, Nagata I, Nishikawa M, Nanto S, Abe K, Ikeda Y, PRASTRO-I Study Group Comparison of prasugrel and clopidogrel in patients with non-cardioembolic ischaemic stroke: a phase 3, randomised, non-inferiority trial (PRASTRO-I) Lancet Neurol. 2019;18(3):238–247. doi: 10.1016/S1474-4422(18)30449-6. [DOI] [PubMed] [Google Scholar]
- 30.Nema H, Kato M, Katsurada T, Nozaki Y, Yotsukura A, Yoshida I, Sato K, Kawai Y, Takagi Y, Okusa T, Takiguchi S, Sakurai M, Asaka M. Endoscopic survey of low-dose-aspirin-induced gastroduodenal mucosal injuries in patients with ischemic heart disease. J Gastroenterol Hepatol. 2008;23(Suppl 2):S234–236. doi: 10.1111/j.1440-1746.2008.05411.x. [DOI] [PubMed] [Google Scholar]
- 31.van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9(2):167–176. doi: 10.1016/S1474-4422(09)70340-0. [DOI] [PubMed] [Google Scholar]
- 32.Whitlock EP, Burda BU, Williams SB, Guirguis-Blake JM, Evans CV. Bleeding risks with aspirin use for primary prevention in adults: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164(12):826–835. doi: 10.7326/M15-2112. [DOI] [PubMed] [Google Scholar]