Abstract
Objectives
Paranoia is a key symptom in psychosis and associated with a range of poor outcomes. Earlier life experiences increase vulnerability to paranoid thinking, and attachment theory has been proposed as a key model in explaining this causal pathway. Previous reviews highlight evidence of associations between insecure attachment styles and overall severity of psychotic symptoms. Studies report on associations between insecure attachment and paranoia, but to date, this literature has not been adequately synthesized. The aim of the current review was to report the strength and consistency of associations between paranoia and insecure attachment across published studies, and provide systematic appraisal of study quality.
Method
We carried out a systematic review of electronic databases using search terms to capture concepts of adult attachment, paranoia, and psychosis. We pre‐registered the review protocol and followed PRISMA guidelines.
Results
Significant associations were reported in 11 out of 12 studies between an insecure attachment and paranoia, with associations remaining significant in studies that controlled for comorbid symptoms. The strongest, most commonly reported relationship was between an anxious attachment style and paranoia.
Conclusions
The findings support the proposed role of attachment insecurity in the development and maintenance of paranoia in psychosis and highlight the need to address insecure attachment representations in the treatment of paranoia.
Practitioner points
There is consistent evidence of associations between insecure attachment style and paranoia.
Insecure anxious attachment is more consistently associated with paranoia than an insecure avoidant attachment.
Associations between attachment and paranoia remain significant when key confounders are controlled for in the analyses.
Interventions that address insecure attachment representations and promote a more secure attachment are likely to help reduce paranoia.
Keywords: adult attachment, paranoia, psychosis, review
Background
Paranoia is an unfounded or exaggerated belief, characterized by themes of persecution, conspiracy, and interpersonal threat and ranging from suspiciousness to highly distressing delusions (Freeman et al., 2005). Up to 90% of individuals with a psychotic disorder report persecutory delusions (Moutoussis, Williams, Dayan, & Bentall, 2007). Higher levels of paranoia are associated with poorer treatment response, increased rates of hospitalization, social isolation, emotional distress and poorer quality of life (Freeman, 2016). Empirical studies have therefore attempted to identify the aetiological factors underpinning paranoia. The study of paranoia as a symptom in its own right is consistent with the single‐symptom approach, which ultimately aims to inform the development of more targeted and effective treatments for specific symptoms (Bentall et al., 2014). The increased utility of a focus on paranoia can elucidate key mechanisms that may underlie specific psychiatric phenomena (Persons, 1986). This can enable wider transdiagnostic application in terms of the treatment of paranoia (whereby there is a recognized need for more effective treatment; Freeman, 2016) and may help to overcome issues of heterogeneity within psychiatric diagnoses (Bo, Abu‐Akel, Kongerslev, Haahr, & Simonsen, 2011).
One mechanism that has been increasingly implicated in the development and maintenance of paranoia is insecure attachment. According to Bowlby (1969), if disruption occurs within the primary caregiver–infant relationship, such as through neglect and/or abuse, an insecure attachment can develop.
Early experiences with primary caregivers are suggested to lead to the development of ‘internal working models’, which include representations of the responses of attachment figures (models of others) and representations of self‐efficacy and self‐value (models of self) (Bowlby, 1969). These representations provide a basis for future interpersonal relating and variations in attachment bonds during infancy are argued to be major determinates of later mental health (Mikulincer & Shaver, 2012).
In adulthood, a ‘secure’ attachment style is associated with a positive view of the self, distress tolerance, and a value of close relationships (Mikulincer & Shaver, 2012). Adult insecure attachment styles are suggested to encompass three main categories: anxious, avoidant, and fearful and/or disorganized (Bartholomew & Horowitz, 1991; Main & Solomon, 1990). An anxious attachment style, also known as ‘pre‐occupied’ or ‘anxious‐ ambivalent’, is characterized by a negative view of the self, worry in relation to others, and increased negative affect. In contrast, avoidant attachment, also known as ‘dismissing’, is characterized by a negative view of others, a more positive view of self, and is associated with social withdrawal and the suppression of negative affect. A fearful attachment reflects a combination of negative beliefs about the self and others. This is largely associated with a desire for close relationships and a simultaneous fear, and subsequent avoidance, of others (Bartholomew & Horowitz, 1991). Fearful attachment as assessed on adult attachment measures has been argued to have conceptual overlap with the disorganized concept of attachment in infancy, with some suggesting that fearful attachment in adulthood is the equivalent of the disorganized child (Bartholomew & Horowitz, 1991). A more disorganized attachment is linked to parental maltreatment and interpersonal trauma (Lyons‐Ruth & Jacobvitz, 1999) and is conceptualized as occurring when an attachment figure may be experienced as frightening and/or unpredictable. This attachment type has been implicated with dissociative experiences in response to later trauma (Liotti, 2004). However, disorganized attachment is rarely assessed in psychosis research and is not well captured using self‐report measures (Berry, Varese, & Bucci, 2017).
There is a theoretical argument based on empirical research findings for the specific role of attachment insecurity in pathways from adverse childhood experiences to paranoia (Bentall & Fernyhough, 2008; Bentall et al., 2014; MacBeth, Gumley, Schwannauer, & Fisher, 2011). Previous research indicates support for this notion by demonstrating how attachment insecurity is specifically associated with paranoia across clinical (Wickham, Sitko, & Bentall, 2015) and wider non‐clinical (Mickelson, Kessler, & Shaver, 1997; Pickering, Simpson, & Bentall, 2008) studies (indicating effects generalizable to the wider population).
There is further parallel literature that evidences how specific adverse childhood experiences, such as being raised in institutional care and/or neglect, are specifically associated with increased risk of paranoia. Conversely, childhood sexual abuse is associated with increased risk of hallucinations and not paranoia (Shevlin, McAnee, Bentall, & Murphy, 2015). Attachment disrupting experiences (e.g., being raised in institutional care) are proposed to be specifically relevant to paranoia due to fostering negative beliefs about the self and others develop (characteristics of insecure attachment), which detrimentally impact ability to trust others (Bentall et al., 2014; Korver‐Nieberg, Berry, Meijer, de Haan, & Ponizovsky, 2015).
Insecure attachment is also recognized as likely to influence paranoia in the context of psychosis by promoting negative beliefs (of self and others) and by increasing negative affect, interpersonal sensitivity, and/or social withdrawal (Berry, Barrowclough, & Wearden, 2007; Ponizovsky, Vitenberg, Baumgarten‐Katz, & Grinshpoon, 2013). These factors have all been identified as key mechanisms implicated within models of paranoia and persecutory delusion formation (Freeman & Garety, 2014; Freeman, Garety, Kuipers, Fowler, & Bebbington, 2002).
Several reviews have explored the role of attachment in the context of psychosis, focusing on the construct validity of attachment (Gumley, Taylor, Schwannauer, & MacBeth, 2014), the role of attachment in recovery specifically (Berry et al., 2007; Korver‐Nieberg, Berry, Meijer, & Haan, 2014), and associations between attachment and overall positive and negative symptoms (Carr, Hardy, & Fornells‐Ambrojo, 2017). Despite the importance of the single‐symptom approach within the field of psychosis, no previous review has systematically examined the evidence for the specific relationship between insecure attachment and paranoia. Therefore, the aim of the current review was to provide an up‐to‐date examination of the association between insecure attachment and paranoia in the context of psychosis and provide a systematic appraisal of study quality.
Method
Search strategy
The review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines (Moher, Liberati, Tetzlaff, Altman, & Prisma Group, 2009). A search was conducted on PsycINFO, Ovid MEDLINE, EMBASE, Web of Science, and PubMed from inception to December 2017. The following keywords were used (‘attachment’ OR ‘adult attachment’ OR ‘attachment theory’) AND (‘Paranoi*’ OR ‘Persecut*’ OR ‘Delusion*’ OR ‘suspici*’) OR (‘Psychosis’ OR ‘Psychotic’ OR ‘Schizo*’ OR ‘Severe Mental’ OR ‘Serious Mental’ OR ‘Serious Psychiatric’ OR ‘Severe Psychiatric’). Medical Subject Headings (MESH) terms were also used for the attachment search string. Database searches were limited to papers published in the English language. Reference lists of retrieved articles were also searched by hand for additional studies.
Eligibility criteria
Inclusion criteria for the studies were (1) samples of people with a diagnosis of a schizophrenia spectrum disorder or other psychotic disorder; (2) validated assessment of adult attachment; (3) validated assessment of paranoia; (4) peer‐reviewed; and (5) English language. Exclusion criteria were (1) studies reporting parental bonding or other related concepts not distinctly measuring attachment; (2) if <50% of the study sample comprised a diagnosis of a schizophrenia spectrum disorder; (3) studies comprising only non‐clinical participants or not reporting clinical and non‐clinical data separately; and (4) conference extracts, book chapters, theoretical or review articles.
Study selection (Figure 1)
Figure 1.
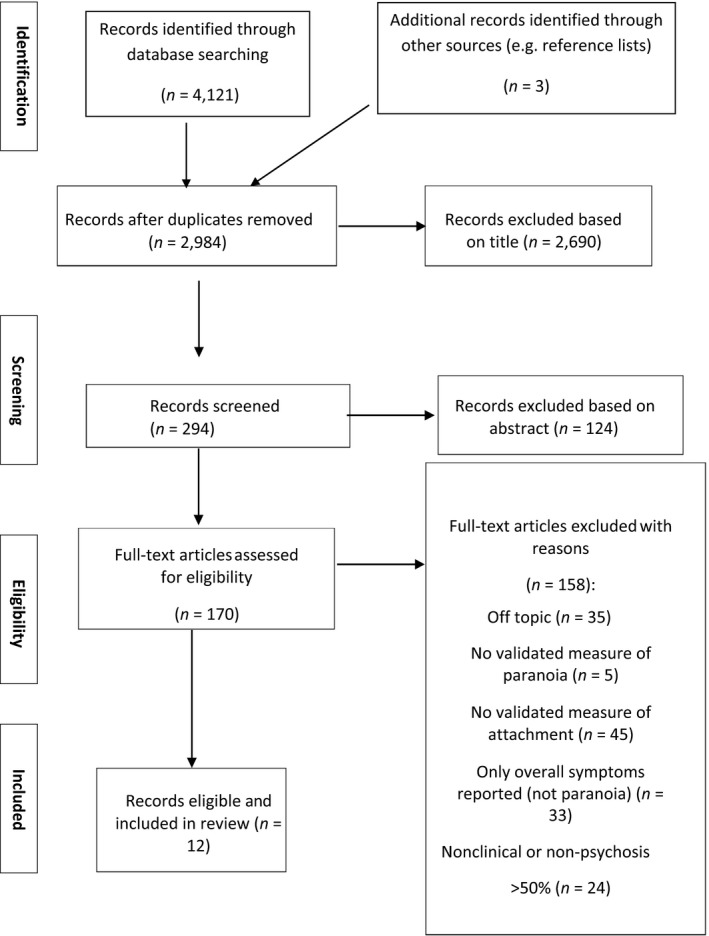
PRISMA flow diagram of systematic search.
The database searched retrieved 4,121 records. Titles, abstracts, and full‐text papers were also screened by an independent researcher, and high levels of agreement were achieved (k = 0.85). All full‐text articles were reviewed by all authors and were only included if all authors were in agreement. A total of 12 studies met inclusion criteria.
Data extraction
Data were extracted from eligible studies using a data extraction sheet that recorded: (1) design; (2) sample; (3) measures; and (4) summary of findings (including effect size if reported).
Quality assessment
The Effective Public Health Practice Project tool (EPHPP; Thomas, Ciliska, Dobbins, & Micucci, 2004) was used to assess the methodological quality of studies. The EPHPP recommended for use in reviewing non‐randomized intervention studies and has been reported to have good inter‐rater reliability (Armijo‐Olivo, Stiles, Hagen, Biondo, & Cummings, 2010) and construct and content validity (Thomas et al., 2004). Ratings (strong, moderate, or weak) were made across the domains of (1) selection bias; (2) study design; (3) confounders; (4) blinding; (5) data collection method; (6) withdrawals/dropouts; and (7) analysis. Overall global rating scores were calculated for each study: strong (no weak ratings), moderate (one weak rating), or weak (two or more weak ratings).
Given that most studies used cohort or cross‐sectional designs, the section of ‘blinding’ was removed, and the domain of ‘design’ was adapted. Cohort designs are recognized as more methodologically robust than cross‐sectional designs (Mann, 2003) in the conclusions they yield; therefore, cohort (longitudinal) designs were assigned a moderate rating, and cross‐sectional a weak rating. The adapted EPHPP measure ratings achieved high levels of agreement (κ = .92).
Results
Overview of studies (Table 1)
Table 1.
Summary of included studies
| Source | Design | Sample characteristics | Measures | Attachment subtypes | Key findings | |
|---|---|---|---|---|---|---|
| Attachment | Paranoia | |||||
| Dozier and Lee (1995) USA | Cross‐sectional | Paranoid schizophrenia (24), undifferentiated schizophrenia (23), bipolar affective disorder (27), panic disorder (1), conversion disorder (1) (n = 76). 45 male | AAI | BSI | Secure versus insecure prototype | Individuals who relied on more hyperactivating (anxious) reported higher symptoms than those with deactivating (avoidant) (specific statistic not reported). Avoidant attachment (deactivating) reported as negatively correlated with paranoid ideation on BSI (r = −.23, p < .05) |
| Mean age not reported | Used the Q‐Set | Interviewer rating of symptoms (including suspiciousness) | Deactivating (avoidant) versus hyperactivating (anxious) | Interviewers conversely rated individuals with deactivating symptoms as more suspicious (r = .55) and more symptomatic overall | ||
| Community sample | No confounders controlled for | |||||
| Berry et al. (2008) UK | Longitudinal – cohort prospective | Schizophrenia (77), schizoaffective disorder (15), psychosis not otherwise specified (NOS) (4). (n = 96). 66 male | PAM | PANSS | Avoidance | Attachment avoidance was positively correlated with paranoia subscale score (r = .39, p < .001). No relationship found between attachment anxiety and paranoia (r = .19, p = .69) |
| 54 participated in study follow‐up. Mean age = 44 | PAM – informant version | Anxiety | Regression analysis found that attachment avoidance was a significant predictor of paranoia (β = .20, p = .44) independent of illness severity (controlled for by PANSS total score) | |||
| Inpatient and community sample | Attachment ratings were found to be moderately stable over time, and informant versions of the PAM showed replication of findings with similar levels of significance. The only significant association between change in symptoms over 6 months was in relation to attachment anxiety and hallucinations | |||||
| MacBeth et al. (2011) UK Scotland | Cross‐sectional | First‐episode psychosis sample; schizophrenia (11), schizoaffective disorder (3), persistent delusional disorder (2), bipolar affective disorder (11), mania with psychotic symptoms (1), recurrent depressive disorder with psychotic symptoms (2). (n = 34). 20 male | AAI | PANSS | Secure | Approximately a third of the sample coded as securely attached |
| Mean age not reported | Dismissing | No significant relationships found between attachment classifications and PANSS paranoia items (nor other PANSS items) | ||||
| Community sample | Preoccupied | No confounders controlled for | ||||
| Korver‐Nieberg et al. (2013) UK | Cross‐ sectional (case–control) | Early psychosis (according to ICD‐10; distinct diagnoses not described). (n = 32). 19 male | PAM | PANSS | Avoidance | Attachment anxiety was positively associated with ideas of social reference on GPTS (r = .42, p < .05) even after controlling for the frequency of positive and negative symptoms on the CAPE. Attachment anxiety reported as initially positively correlated with persecution on GPTS; however, this was no longer significant when controlling for frequency of symptoms |
| Mean age 17.1. | GPTS | Anxiety | Attachment avoidance was initially positively correlated with ideas of social reference but this was no longer significant after controlling for frequency of symptoms on the CAPE. Attachment avoidance was reported as significantly correlated with persecution on GPTS and this remained significant when controlling for symptoms frequency (r = .45, p < .05) | |||
| Community sample | CAPE | |||||
| Ponizovsky et al. (2013) Israel | Cross‐sectional | Schizophrenia (n = 100). 70 male | RQ | PANSS | Secure | Sample split into four RQ attachment subgroups: over half of the sample was classed as secure (and only 10 with dismissing) |
| Mean age 40.3 | Dismissing | In regression analyses, emotional distress combined with RQ attachment showed both preoccupied (β = .417, p < .0001) and fearful‐avoidant attachment (β = .353, p < .0001) style to be significant predictors of PANSS suspiciousness/persecution (and also PANSS delusions), whereas dismissing‐avoidant was not | ||||
| Community sample | Preoccupied | No other confounders controlled for | ||||
| Fearful | ||||||
| Wickham et al. (2015) UK | Cross‐sectional (case–control) | Schizophrenia (122), schizoaffective disorder (17), substance‐induced psychosis (6), PNOS (15), acute and transient psychotic disorder (12), delusional disorder (4). (n = 176). 123 male | RQ | Persecution and Deservedness Scale (PaDS) | Avoidance | Used RQ to yield scores on anxiety and avoidance attachment dimensions for main analysis |
| Mean age not reported. Range 17–77 years | PANSS | Anxiety | Correlational analyses showed both insecure attachment styles correlated with paranoia (anxiety: PaDS r = .44, PANSS r = .34, avoidance: PaDS r = .21, PANSS r = .24, all p < .01) | |||
| Community and inpatient samples | Regression analysis showed attachment anxiety significantly predicted paranoia in clinical sample using the PaDS when controlling for hallucinations, and the effect for attachment avoidance was did not reach significance. When using the PANSS and controlling for hallucinations, both attachment dimensions predicted paranoia. Neither attachment style predicted hallucinations when controlling for paranoia (both on PaDS and PANSS) | |||||
| A mediation model using clinical participants was estimated twice using different measures of paranoia (PaDS and PANSS item 6). Partial medication was reported for the relationship between attachment anxiety and paranoia (on both PaDS and PANSS) with negative self‐esteem as a mediator (PaDS = β = .014, p < .001; PANSS = β = .09, p < .01). Full mediation occurred between attachment avoidance and paranoia via self‐esteem (PaDS = β = .11, p < .001; PANSS = β = .07, p < .01) | ||||||
| All analyses controlled for age, sex and comorbidity of hallucinations | ||||||
| Korver‐Nieberg et al. (2015)a | Cross‐sectional | Schizophrenia (426), schizoaffective disorder (38), non‐affective psychosis (26) (n = 500). 402 males | RQ | PANSS | Avoidance | Pooled sample of 500 and analysed specifically looking at attachment and paranoia (PANSS suspiciousness item 6) |
| Mean age = 37.5 | Anxiety | PANSS item 6 suspiciousness/persecution was rated higher in individuals with any attachment insecurity (fearful‐avoidant, preoccupied, dismissing‐avoidant) compared to securely attached individuals | ||||
| Community and inpatient samples | RQ attachment dimensions were grouped into attachment anxiety and attachment avoidance. PANSS item 6 suspiciousness/persecution was associated with attachment anxiety (r = .183, p < .001) and attachment avoidance (r = .173, p < .001) | |||||
| No confounders controlled within correlational analysis | ||||||
| Strand et al. (2015) Sweden | Cross‐sectional | Schizophrenia (16), schizoaffective disorder (6), other psychoses (20), bipolar disorder (5). (n = 47). 30 male | RQ | Revised Symptom Checklist (SCL‐90R) | Secure | No significant association between secure attachment or dismissing attachment and symptoms |
| Mean age = 43.02 | Dismissing | The only significant positive correlation was between preoccupied attachment and paranoia (p = .001, r = .463) | ||||
| Community sample | Preoccupied | No confounders controlled for | ||||
| Fearful | ||||||
| Sitko et al. (2016) UK | Longitudinal – experience sampling method (ESM) (case–control) | Schizophrenia (6), Schizoaffective disorder (2), paranoid schizophrenia (8), PNOS (4). (n = 19). 16 male | RQ and ESM measure adapted from Adult Attachment Style (AAS) questionnaire. ESM measure validated against the RQ using a binary approach (secure vs. insecure) | PANSS | Secure | Linear regression found that attachment insecurity predicted the occurrence of paranoia. This relationship remained significant even when controlling for concurrent auditory hallucinations (β = .139, p = .001) and self‐esteem (β = .140, p = .001) |
| Mean age = 47.14 | ESM measure derived from PaDS and used in previous ESM studies (Udachina, Varese, Oorschot, Myin‐Germeys, & Bentall, 2012; Varese, Udachina, Myin‐Germeys, Oorschot, & Bentall, 2011 | Insecure – state attachment insecurity defined as a mean score of six statements derived from AAS | Auditory hallucinations also predicted by preceding elevated levels of attachment insecurity; however, this effect was no longer significant after controlling for paranoia | |||
| Community sample | Attachment insecurity still predicted and preceded paranoid thinking when controlling for self‐esteem | |||||
| Fett et al. (2016) UK | Cross‐sectional (case–control) | ICD‐10 psychotic episode (n = 39). 23 male | PAM | GPTS | Avoidance | Regression analysis found that attachment anxiety was positively associated with GPTS social reference (β = .70, p < .001) and persecution paranoia (β = .49, p < .001) |
| Mean age 17.1 | PANSS | Anxiety | Attachment avoidance was positively associated with GPTS social reference (β = .52, p < .001) and persecution paranoia (β = .43, p < .001) | |||
| Community sample | No confounders controlled for | |||||
| Castilho et al. (2017) Portugal | Cross‐sectional | Schizophrenia (33), schizoaffective disorder (3), PNOS (4). (n = 37). 30 male | ECR‐RS | PC | Avoidance | Initial analyses showed attachment anxiety was predominant. Correlational analyses found a significant association between attachment anxiety (in relation to mother) and PC frequency (r = .33, p = .05) |
| Mean age = 37.14 | Anxiety | Further analyses included experiential avoidance as a mediator between the relationship of attachment anxiety (in relation to mother) and frequency of paranoid ideation (PC). Experiential avoidance was reported to mediate this relationship. | ||||
| Inpatient sample | No confounders controlled for | |||||
| Pearce et al. (2017) | Cross‐sectional | Schizophrenia (35), schizoaffective disorder (19), delusional disorder (1), brief psychotic disorder (7), PNOS (13), other (20), no diagnosis (4), bipolar affective disorder (13) | RQ | CAPE | Secure | Of those that completed the RQ measure, the majority reported fearful attachment styles (n = 55) |
| (n = 131). Male 30 | Dismissing | Correlational analyses showed preoccupied and dismissive attachment were not associated with paranoia (nor voices). Fearful attachment was positively associated with paranoia (r = .54, p < .001) (and also associated with voices). Paranoia and voices reported as highly correlated | ||||
| Mean age = 40.26 | Preoccupied | Correlation comparison tests revealed that the correlation between fearful attachment and paranoia was larger than the correlation between fearful attachment and voices | ||||
| Fearful | Fearful attachment was found to mediate the relationship between childhood trauma and paranoia, when controlling for voices (β = .05, p < .05) | |||||
| Childhood trauma alone did not appear to predict paranoia independent of the mediators | ||||||
The Revised Symptom Checklist SCL‐90R – (Derogatis, 1997).
AAI = Adult Attachment Interview (George et al., 1996); AAS = Adult Attachment Style Questionnaire (Collins & Read, 1990); BSI = Brief Symptom Index (Derogatis & Spencer, 1982); CAPE = Community Assessment of Psychic Experiences (Stefanis et al., 2002); ECR‐RS = Experiences in Close Relationships – Relationship Structure (Fraley et al., 2011); GPTS = Green Paranoid Thoughts Scale (Green et al., 2008); PaDS = Persecution and Deservedness Scales (Melo et al., 2009); PAM = Psychosis Attachment Measure (Berry, Wearden, Barrowclough, & Liversidge, 2006); PANSS = Positive and Negative Syndrome Scale (Kay et al., 1987); PC = Paranoia Checklist (Freeman et al., 2005); RQ = Relationship Questionnaire (Bartholomew & Horowitz, 1991).
Studies were conducted in the United Kingdom (n = 7), Portugal (n = 1), Switzerland (n = 1), Sweden (n = 1), the United States (n = 1), and Israel (n = 1), with one study amalgamating data (Korver‐Nieberg et al., 2015) from five previous studies that were conducted in Israel (Ponizovsky, Arbitman, Baumgarten‐Katz, & Grinshpoon, 2014; Ponizovsky, Nechamkin, & Rosca, 2007; Ponizovsky et al., 2013), the United Kingdom (Berry, Barrowclough, & Wearden, 2008), and the Netherlands (Korver, Quee, Boos, Simons, & Haan, 2012). One study combined two datasets from previous studies conducted within the United Kingdom (Wickham et al., 2015). Sample size ranged from 19 to 500. A large proportion of participants were males with a diagnosis of schizophrenia. The reported age ranged from 17.1 to 77 years. Participants were recruited from either community settings (n = 465), inpatient settings (n = 37), or both (n = 772).
Five different measures of attachment were used across the 12 studies. Six studies (Korver‐Nieberg et al., 2015; Pearce et al., 2017; Ponizovsky et al., 2013; Sitko, Varese, Sellwood, Hammond, & Bentall, 2016; Strand, Goulding, & Tidefors, 2015; Wickham et al., 2015) used The Relationship Questionnaire (RQ: Bartholomew & Horowitz, 1991) to measure attachment subtypes (secure, dismissing, pre‐occupied, fearful). Two studies (Korver‐Nieberg et al., 2015; Wickham et al., 2015) created superordinate attachment anxiety and avoidance dimensions by yielding scores from the four RQ subtypes. One study used the RQ to validate an experience‐sampling method (ESM) binary approach of security and insecurity, with attachment insecurity comprising of individuals who identified as pre‐occupied, dismissing, and fearful (Sitko et al., 2016). Three studies (Berry et al., 2008; Fett et al., 2016; Korver‐Nieberg et al., 2013) use the Psychosis Attachment Measure (PAM; Berry et al., 2008) to assess attachment avoidance and attachment anxiety. One study (MacBeth et al., 2011) used the Adult Attachment Interview (AAI; George, Kaplan, & Main, 1996) for categorical classifications of attachment (secure, dismissing, and pre‐occupied). One study (Castilho et al., 2017) used Experiences in Close Relationships – Relationship Structure (ECR‐RS: Fraley, Heffernan, Vicary, & Brumbaugh, 2011) to assess attachment anxiety and avoidance.
Regarding paranoia, item P6 on the Positive and Negative Syndrome Scale (PANSS; Kay, Fiszbein, & Opfer, 1987) was often used. Studies also used the paranoia items from the Community Assessment of Psychic Experiences (CAPE; Stefanis et al., 2002), the Revised Symptom Checklist (SCL‐90R; Derogatis, 1997), the Brief Symptom Inventory (BSI; Derogatis & Spencer, 1982), and the Paranoia Checklist (Freeman et al., 2005). Three studies used multiple indicators of paranoia (Fett et al., 2016; Korver‐Nieberg et al., 2013; Wickham et al., 2015), including the persecution subscales of the Persecution and Deservedness Scale (PaDS; Melo, Corcoran, Shryane, & Bentall, 2009) and the Green Paranoid Thoughts Scale (GPTS; Green et al., 2008). One study used an adapted ESM measure of paranoia measure derived from the PaDS (Sitko et al., 2016). Table 2 details paranoia measures used across studies, including constructs assessed.
Table 2.
Summary of paranoia measures
| Measure of paranoia | Description of measure | Paranoia subscales | Construct validity |
|---|---|---|---|
| Community Assessment of Psychic Experiences (CAPE) (Stefanis et al., 2002) | A 42‐item self‐report questionnaire measuring lifetime prevalence of psychosis‐like experiences | Five items (items 2, 6, 7, 10, 22) assessing paranoia (frequency and distress), including feelings of persecution and feeling that there ‘is a conspiracy against you’ | Convergent validity has been demonstrated with the paranoia subscales with results correlating with other self‐report measures of paranoia (e.g., Paranoia Checklist; Freeman et al., 2005) (Schlier, Jaya, Moritz, & Lincoln, 2015) |
| Brief Symptom Inventory (BSI) (Derogatis & Spencer, 1982) | A 53‐item self‐report questionnaire (derived as a short version of the SCL‐90‐R; Derogatis, 1975) measuring nine symptom dimensions over the past 7 days | Five items (items 4, 10, 24, 48, 51) that assess paranoid ideation (frequency and distress), including hostility, suspiciousness, and ideas of social reference | Demonstrated convergent/construct validity with scores from the paranoid ideation subscales correlating with other measures of paranoia (e.g., Minnesota Multiphasic Personality Inventory) (Derogatis & Melisaratos, 1983) |
| Positive and Negative Syndrome Scale (PANSS) (Kay et al., 1987) | A 30‐item semi‐structured clinical interview measure of psychopathology that rates the presence and severity of symptoms within the past week | One specific item (item P6) assessing suspiciousness/persecution defined as ‘ideas of persecution, as reflected in guardedness, a distrustful attitude, suspicious hypervigilance or frank delusions that others mean harm’ | Demonstrated construct validity (Kay et al., 1987) with scores of item 6 (paranoid ideation) correlating with various measures of paranoia, including the PaDS (Melo et al., 2009; Wickham et al., 2015) |
| Experience‐sampling method (ESM) measure (used within Sitko et al., 2016) | A self‐report experience‐sampling method measure of paranoia to assess paranoid thinking over 6 days, derived from the PaDS (Melo et al., 2009) | Two‐item statements rated on 7‐point Likert scales that assessed self‐reported state paranoia, encompassing suspiciousness and paranoid ideation (‘Right now I worry that others are plotting against me’, ‘I believe that some people want to hurt me deliberately’) | The ESM measure of paranoia demonstrated validity in previous research (Udachina et al., 2012; Varese et al., 2011) |
| Persecution and Deservedness Scales (PaDS) (Melo et al., 2009) | A self‐report 20‐item trait measure of paranoid thinking (severity) and the perception that persecution is deserved | 10‐item measure persecution and 10‐item measure perceived deservedness of persecution | The measure demonstrates good concurrent validity with the persecution subscale correlating with PANSS suspiciousness/persecution item 6 (Wickham et al., 2015) |
| The Revised Symptom Checklist (SCL‐90‐R) (Derogatis, 1997) | A 90‐item self‐report measure of psychological distress (severity) relating to subscales of symptoms experienced over the last 7 days | Six items measuring paranoid ideation, including hostility, suspiciousness, and ideas of social reference | The SCL‐90R has demonstrated high convergent validity with the MMPI in relation to paranoid ideation subscales (Derogatis, Rickels, & Rock, 1976) |
| Green Paranoid Thoughts Scale (GPTS) (Green et al., 2008) | A 32‐item self‐report measure assessing severity of paranoia over the past month | Two scales that assess persecution (16‐items) and ideas of social reference (16‐items) | Demonstrated concurrent and convergent validity with both scales positively correlating with other measures of paranoia (Green et al., 2008; Statham, Emerson, & Rowse, 2019) |
| Paranoia Checklist (PC) (Freeman et al., 2005) | An 18‐item self‐report measure of paranoid ideation (frequency, distress, and conviction) | 18 items that assess paranoid ideation, including suspiciousness, ideas of persecution, and ideas of social reference | Measure has been reported as positively correlating with other measures of paranoia (e.g., MMPI, Paranoia Scale) (Horton, Barrantes‐Vidal, Silvia, & Kwapil, 2014; Statham et al., 2019) |
Study quality (Table 3)
Table 3.
Quality rating (strong, moderate of weak) for the six Effective Public Health Practice Project domains and overall quality rating
| Study | Selection bias | Study design | Confounders | Data collection | Withdrawal | Analysis | Global rating |
|---|---|---|---|---|---|---|---|
| Dozier and Lee (1995) | Weak | Weak | Weak | Strong | n/a | Moderate | Weak |
| Berry et al. (2008) | Weak | Moderate | Moderate | Strong | Weak | Strong | Weak |
| MacBeth et al. (2011) | Weak | Weak | Weak | Strong | n/a | Moderate | Weak |
| Korver‐Nieberg et al. (2013) | Weak | Weak | Strong | Strong | n/a | Strong | Weak |
| Ponizovsky et al. (2013) | Moderate | Weak | Moderate | Strong | n/a | Moderate | Moderate |
| Korver‐Nieberg et al. (2015) | Weak | Weak | Weak | Strong | n/a | Strong | Weak |
| Wickham et al. (2015) | Weak | Weak | Strong | Strong | n/a | Strong | Weak |
| Strand et al. (2015) | Weak | Weak | Weak | Strong | n/a | Strong | Weak |
| Fett et al. (2016) | Weak | Weak | Weak | Strong | n/a | Strong | Weak |
| Sitko et al. (2016) | Weak | Moderate | Strong | Moderate | Strong | Strong | Moderate |
| Castilho et al. (2017) | Weak | Weak | Weak | Strong | n/a | Moderate | Weak |
| Pearce et al. (2017) | Weak | Weak | Moderate | Strong | n/a | Strong | Weak |
Most studies were rated as weak (n = 10). Only two studies achieved a moderate global rating (Ponizovsky et al., 2013; Sitko et al., 2016). Studies often failed to fully report their selection procedures or the number of participants who agreed to participate. Male participants were overrepresented across studies, and studies often relied on convenience sampling with the help of clinicians within services, which limits the generalizability of results. ESM research can often recruit individuals who are highly engaged and willing to repeatedly report data (Scollon, Prieto, & Diener, 2009); therefore, this may have introduced increased sampling bias in Sitko et al. (2016). Only one study used a more systematic means of sampling whereby individuals were recruited following consecutive attendance at a clinic (Ponizovsky et al., 2013).
Studies often employed a cross‐sectional design (n = 10) to assess the association of insecure attachment and paranoia. This design increases the risk of inflated associations due to the overlap between the constructs. The two studies that used longitudinal designs were considered more methodologically robust in the assessment of this association and achieved a moderate rating (Berry et al., 2008; Sitko et al., 2016). Six studies (Castilho et al., 2017; Dozier & Lee, 1995; Fett et al., 2016; Korver‐Nieberg et al., 2015; MacBeth et al., 2011; Strand et al., 2015) did not statistically control for relevant confounders (e.g., illness severity, comorbidity of hallucinations). Two studies were rated as strong (Sitko et al., 2016; Wickham et al., 2015) as these controlled for several relevant confounders. Three studies received a moderate rating (Berry et al., 2008; Pearce et al., 2017; Ponizovsky et al., 2013) as confounders had been controlled for in one or two relevant analyses, but not all. Notably, only two studies used additional clinician measures to corroborate self‐report attachment (Berry et al., 2008) and self‐report paranoia (Dozier & Lee, 1995), enabling some assessment of social desirability bias.
The measures used were considered valid and reliable, as per eligibility criteria, earning a strong rating in most cases. However, paranoia measurement was often restricted to a specific item on a validated measure that assessed suspiciousness/persecution, which is problematic given the dimensional structure of paranoia. The validation of the ESM attachment measure was reported to be moderately associated with attachment subtypes (Sitko et al., 2016). In relation to withdrawals, one longitudinal study reported 80–100% of participants completing the study, earning a strong rating (Sitko et al., 2016), with one study reporting that <60% of participants completed the study (Berry et al., 2008; earning a weak rating). Analyses were rated as stronger in eight studies that clearly examined the relationship between attachment and paranoia, with the other four studies rated as moderate (Castilho et al., 2017; Dozier & Lee, 1995; MacBeth et al., 2011; Ponizovsky et al., 2013).
Relationship between attachment and paranoia
Studies explored multiple attachment representations within one sample; therefore, for clarity, specific associations are described below according to the main attachment categories of anxiety, avoidance, fearful, and other associations.
Anxious attachment
Positive associations between attachment anxiety (or a ‘pre‐occupied’ attachment) and paranoia were reported in seven out of 11 studies that investigated attachment anxiety representations (Castilho et al., 2017; Fett et al., 2016; Korver‐Nieberg et al., 2013, 2015; Ponizovsky et al., 2013; Strand et al., 2015; Wickham et al., 2015). Correlational effect sizes across studies tended to be moderate, ranging from r = .18 to r = .46.
Attachment anxiety was positively associated with paranoia in two first‐episode psychosis community samples (Fett et al., 2016; Korver‐Nieberg et al., 2013). Fett et al. (2016) reported positive associations with attachment anxiety and ideas of social reference and persecution subscales (GPTS; Green et al., 2008; social reference: β = .70; persecution: β = .49). Confounders were not controlled for in the regression analysis conducted within this study. However, results were less likely to have been impacted by a lack of controlling for comorbid symptoms, as overall symptom severity was relatively low within this sample. Conversely, Korver‐Nieberg et al. (2013) controlled for the frequency of overall symptoms. The authors reported that only attachment anxiety remained positively correlated with the ideas of social reference subscale (r = .42), whereas the relationship to the persecution subscale (GPTS; Green et al., 2008) became non‐significant after controlling for symptom frequency. These results indicate how observed associations may differ depending on whether studies control for co‐occurring symptoms.
In a further study, Korver‐Nieberg et al. (2015) analysed a large amalgamated sample and reported that attachment anxiety was positively associated with paranoia (r = .18). No confounders were controlled for within this analysis. This is an important limitation, particularly as individuals within this sample were reported as having moderate overall severity of symptoms and a relatively long illness duration. A further study reported that a pre‐occupied attachment style predicted paranoia (β = .42) in regression analyses when combined with emotional distress (Ponizovsky et al., 2013).
Strand et al. (2015) reported a positive association between pre‐occupied attachment and paranoia (r = .46) within a community sample. The inclusion of participants with affective psychoses in this study could have introduced heterogeneity, and the sample size was small, limiting generalizability of findings. In another study, attachment was positively associated with paranoia (r = .33) in an inpatient sample (Castilho et al., 2017). Mediation analyses reported that experiential avoidance mediated the relationship between attachment anxiety and paranoia. The authors reported how attachment anxiety was predominant within the inpatient sample; consequently, this subtype may have been overrepresented. Importantly, no comorbid symptoms or confounders were statistically controlled for in neither Strand et al. (2015) nor Castilho et al. (2017). This may be a more pertinent limitation to the inpatient sample (Castilho et al., 2017) as these individuals were in a more acute phase of illness and likely experiencing severe or co‐occurring symptoms.
In a study that used multiple indicators of paranoia, attachment anxiety was reported as positively associated with measures of paranoia (r = .44 and r = .34, respectively) in a community and inpatient sample (Wickham et al., 2015). This study controlled for a range of confounders (age, sex, comorbidity of hallucinations) and reported that attachment anxiety predicted paranoia. Mediation analysis indicated that the relationship between attachment anxiety and paranoia was partially mediated by negative self‐esteem (PaDS: β = .014 and PANSS: β = .09).
Avoidant attachment
Positive associations between avoidant attachment and paranoia were reported in five out of 11 studies that investigated this relationship (Berry et al., 2008; Fett et al., 2016; Korver‐Nieberg et al., 2013, 2015; Wickham et al., 2015), with one study reporting a negative association with paranoia (Dozier & Lee, 1995). Effect sizes tended to be small to moderate (ranging from 0.21 to 0.45). Four of these studies reported a positive association with attachment anxiety (as summarized earlier; Fett et al., 2016; Korver‐Nieberg et al., 2013, 2015; Wickham et al., 2015).
One study (Dozier & Lee, 1995) reported a negative association between self‐reported paranoia and the deactivating (avoidant attachment) category of the AAI (r = −.23). Interviewers also rated participants’ symptoms, including suspiciousness. Whilst this was not a validated scale of assessment, results showed that interviewers rated more avoidant individuals as more suspicious. This could indicate an element of bias for avoidant individuals in relation to the self‐reporting of paranoia. Within a sample of individuals with a diagnosis of a first‐episode psychosis, Fett et al. (2016) reported that attachment avoidance was positively associated with paranoia (social reference and persecution; β = .70, and β = .49, respectively). However, comorbid symptoms were not controlled for within analyses in these two community samples (Dozier & Lee, 1995; Fett et al., 2016).
Within their large community and inpatient sample, Korver‐Nieberg et al. (2015) reported that attachment avoidance was positively associated with paranoia (r = .18). When controlling for several confounders within a combined community and inpatient sample, Wickham et al. (2015) reported that avoidant attachment was positively correlated with paranoia (PaDS and PANSS; r = .21, and r = .24, respectively). However, regression analysis showed that attachment avoidance was no longer significantly related to paranoia on the PaDS when controlling for the effect of hallucinations. Mediation analysis showed that full mediation occurred between attachment avoidance and paranoia (PaDS and PANSS) via negative self‐esteem. When Korver‐Nieberg et al. (2013) controlled for the frequency of symptoms within their first‐episode community sample, attachment avoidance was no longer significantly associated with ideas of social reference (GPTS), but remained positively associated with persecution (GPTS) (r = .45).
Furthermore, Berry et al. (2008) found that only attachment avoidance was positively associated with severity of paranoia (r = .39) in a community and inpatient sample. Regression analyses reported that attachment avoidance was a significant predictor of paranoia over time (PANSS P6; β = .20) when controlling total symptoms scores, suggesting that increased attachment avoidance in more paranoid individuals was not accounted for by illness severity. This study was more able to infer causality due to its longitudinal design, and the use of an informant version of the PAM that reported similar findings indicated that self‐reporting of attachment was reliable.
Fearful attachment
Of the three studies that explored specific associations between paranoia and fearful attachment, two reported positive associations (Pearce et al., 2017; Ponizovsky et al., 2013). Ponizovsky et al. (2013) reported, in addition to a positive association with pre‐occupied attachment, that a fearful‐avoidant attachment style predicted paranoia in linear regression analyses (β = .353) when combined with emotional distress in a community sample. This analysis showed that a fearful‐avoidant attachment style also predicted hallucinations; however, the comorbidity of these two experiences (paranoia and hallucinations) within analyses was not controlled for. Pearce et al. (2017) reported a positive association specifically between fearful attachment and paranoia (r = .54) within a community‐based sample with higher representation of females compared to other study samples. When covariation of hallucinations was then adjusted for within mediational analyses, fearful attachment mediated the relationship between childhood trauma and paranoia (β = .05). Fearful attachment was not found to be related to hallucinations. It was noted that a substantial proportion of participants were classified as having a fearful attachment style, indicating that this subtype may have been overrepresented.
Other attachment associations
Within a longitudinal study, it was reported that general attachment insecurity (as measured by an ESM measure) predicted the occurrence of paranoia over time, with the relationship remaining significant when controlling for both auditory hallucinations (β = .14) and self‐esteem (β = .14; Sitko et al., 2016). Despite the sample being small and subject to potential bias, this study was better able to infer the causal role of attachment insecurity in predicting paranoia due to controlling for the effects of both self‐esteem and co‐occurring hallucinations.
One study reported no significant association between any attachment subtypes (derived from the AAI) and paranoia (PANSS item 6) within a first‐episode psychosis community sample (MacBeth et al., 2011). The lack of association found could be due to the sample having low levels of positive psychotic symptoms overall. There was also no adjustment within analyses for co‐occurring symptoms. The sample size was small (n = 34) which may have resulted in insufficient statistical power to detect associations, and there was a small number of individuals in the ‘pre‐occupied’ category. Furthermore, these different results may reflect the use of a narrative attachment assessment, whereas the majority of studies within the current review used a self‐report method.
Both Korver‐Nieberg et al. (2015) and Wickham et al. (2015) used superordinate attachment anxiety and attachment avoidance dimensions from the RQ, which included secure attachment; therefore, some of the variance within associations may be attributed to secure attachment style.
Discussion
This is the first review to examine the association between insecure attachment and paranoia within psychosis, whilst systematically appraising the quality of studies. Overall, the available evidence provides support for the role of attachment insecurity in the presence of paranoid thinking within psychosis. However, due to the majority of studies being cross‐sectional and rated as weak in quality, this evidence needs to be interpreted with caution.
Despite most studies being rated as weak in quality, positive associations between insecure attachment and paranoia were found in 11 of the 12 studies, with anxious attachment showing the strongest and most predominant relationship with paranoia. Fewer studies reported an association with an avoidant attachment style, with four of these five studies reporting positive associations with both anxiety and avoidance attachment subtypes. Two of three studies that investigated fearful attachment reported a positive association with paranoia, with strong correlation coefficients. Positive associations were consistent across a range of different paranoia and attachment measures and across both community and inpatient settings.
Whilst it was not an aim of the current review to examine the magnitude of associations between attachment and paranoia, compared to other co‐occurring symptoms, a number of studies did report such comparisons and/or attempted to control for the effect of co‐occurring symptoms (a step recognized as important when attempting to identify symptom‐specific associations; Bentall et al., 2014). Studies reported that insecure attachment and paranoia associations were independent of illness severity/other symptoms after controlling for their effect (Berry et al., 2008; Korver‐Nieberg et al., 2013), or, associations to other symptoms then became non‐significant when paranoia was controlled for (Sitko et al., 2016; Wickham et al., 2015). An insecure attachment style was largely associated with paranoia even when controlling for the effects of self‐esteem, illness severity, and/or the comorbidity of hallucinations in studies that controlled for relevant confounders. Therefore, the available evidence provides support for attachment insecurity playing a specific role in the presence of paranoid thinking within psychosis.
The finding that anxious attachment was most associated with paranoia contrasts previous reviews in psychosis that have more often reported a positive relationship between avoidant attachment and paranoia (Berry et al., 2007; Korver‐Nieberg et al., 2014). This could be explained by the paucity of studies that had explored associations at the time of these reviews. Furthermore, the measures used within studies to assess paranoia may explain why an anxious attachment was most predominantly associated with paranoia. Most measures used within studies assessed the construct of persecution (e.g., PANSS item 6), a more distressing symptom characterized by severe threat (Freeman & Garety, 2014) which may relate more to an anxious attachment.
An anxious attachment style may be more related to paranoia due to associations with pre‐occupation/worry, increased negative affect, and increased interpersonal sensitivity (Mikulincer & Shaver, 2012). This pre‐occupation with relationships can predispose an individual towards a hypervigilance for threat in the social world (Mikulincer, Shaver, & Pereg, 2003). The threat anticipation model (Freeman et al., 2002) outlines how affective processes, such as anxiety and worry, combined with interpersonal sensitivity, are important casual factors in paranoia. Heightened negative affect and interpersonal sensitivity make a threatening interpretation of others more likely, which can fuel ideas of persecution (Freeman et al., 2014).
Paranoid delusions are related to negative beliefs about the self as vulnerable (MacBeth, Schwannauer, & Gumley, 2008). A negative self‐view is characteristic of attachment anxiety and therefore may lead individuals to perceive themselves as increasingly vulnerable, which can ultimately increase a sense of threat and harm from others (Freeman et al., 2014). These attachment representations, encompassing low self‐esteem and assumptions about others, can drive paranoid thinking (Freeman et al., 2002). Importantly, when studies in the current review did control for the effects of negative self‐esteem, an insecure attachment was at times still associated with paranoia, which provides support for the specific role of insecure attachment in paranoid thinking (Bentall & Fernyhough, 2008).
Several studies within the review reported associations with avoidant attachment. Attachment avoidance is associated with a more negative view of others, minimization of affect, and social withdrawal (Hazan & Shaver, 1987). Individuals with attachment avoidance downregulate their affect through avoidance strategies and can have a positive view of self but negative view of others (Ponizovsky et al., 2013). Both social withdrawal and negative beliefs about others are also implicated in models of paranoia (Freeman et al., 2002). Therefore, this attachment style may play a role in the development and/or maintenance of paranoia within psychosis. Studies that investigated fearful attachment also reported positive associations. The fearful attachment style differs from other attachment styles as fearful individuals can largely avoid close relationships (Bartholomew & Horowitz, 1991), yet can exhibit high anxiety and dependency on others (Korver‐Nieberg et al., 2015). This attachment type is characterized by both a negative view of self and others. Given the role of negative beliefs of the self and other in paranoia, this style could be particularly pertinent. Individuals who score highly on measures of both anxious and avoidant attachment are suggested to fall under a disorganized attachment pattern (argued to be similar to fearful attachment). Disorganized attachment is defined by attachment behaviours that are unpredictable, and a disoriented and confused response when attempting to seek care (Main & Solomon, 1990). Such an attachment pattern is argued to have more extreme emotional and behavioural disturbances, and a disorganized attachment has been implicated as a developmental antecedent of dissociation in response to later trauma (Liotti, 2004).
However, only a limited amount of studies explored a fearful/disorganized attachment subtype. In the broader sense, attachment insecurity can increase negative affect, a negative view (of self and/or others), interpersonal sensitivity, and could lead to social withdrawal, which in turn increases vulnerability to affective and specific psychotic symptoms such as paranoia (Korver‐Nieberg et al., 2014). Therefore, any attachment insecurity is likely to promote and maintain paranoia and may explain why frequent associations across various attachment insecurity subtypes are often found.
There are some important limitations within the current review. Overall, the methodological quality of studies was poor which impacts the generalizability of results. Most notably, sample sizes were often small and likely lacked sufficient statistical power. Studies were mainly cross‐sectional in nature, which was useful for determining associations between attachment and paranoia; however, causation cannot be inferred from this design. Some studies did not control for confounders and/or relied on a single item assessing paranoia on an overall measure. Self‐report measures were most commonly used, which can have several limitations. Firstly, self‐report measures of attachment and paranoia can be impacted by social desirability bias, and only two studies used additional measures of data collection (clinician‐rated measures) in addition to self‐report data. Secondly, avoidant individuals may underreport symptoms due to a tendency to minimize affect (Gumley et al., 2014). Thirdly, avoidant individuals may lack ability to reflect and identify with a dismissing attachment style (Strand et al., 2015), resulting in these individuals not been adequately captured using self‐report measures. Fourth, clinician ratings of symptoms tend to be higher than self‐report of symptoms (Carr et al., 2017). Furthermore, given the conceptualized hierarchical structure of paranoia (Freeman et al., 2005), whereby paranoid thoughts are ordered depending on the severity of perceived threat, only a small number of studies investigated paranoia across the hierarchy and distinguished between ideas of social reference and persecution. In addition, as highlighted in the introduction, paranoia is on a continuum, with significant levels often found within non‐clinical samples. Our decision to focus on paranoia in the context of psychosis therefore excluded a potentially important parallel literature on attachment and paranoia in the general population. Finally, the review could also be criticized for not incorporating a meta‐analysis. However, we would argue that aggregating information from heterogeneous samples with different measures of the factors investigated would be problematic (Borenstein, Cooper, Hedges, & Valentine, 2009) as any summary effect is likely to be unrepresentative of the ‘true’ association between attachment and paranoia. Moreover, due to the relatively small number of studies in the review, we would have no means to examine how associations are moderated by methodological variances in this literature using meta‐regressions and subgroup analyses.
The role of insecure attachment has important clinical implications for the treatment and prevention of paranoia in psychosis. Techniques aimed at promoting a secure attachment and reducing interpersonal threat are likely to be useful in reducing paranoia for individuals with psychosis (Phillips, Francey, Edwards, & McMurray, 2009). Interventions that reduce negative ideas and encourage more positive views of the self and other are likely to lead reduce paranoia (Freeman, Freeman, & Garety, 2016). The attachment system is primarily activated by threat (Bowlby, 1969). Therefore, promoting a more secure attachment may result in a reduced sense of threat. Techniques or strategies to improve affect regulation are important (Hutton, Kelly, Lowens, Taylor, & Tai, 2013), particularly as heightened anxiety can make a threatening interpretation more likely (Freeman et al., 2016).
Attachment representations inform expectations and predictions of social situations with models of relating that form in childhood remaining influential in adult life (Collins & Read, 1994). Importantly, attachment representations can change as a result of interpersonal experiences. Psychological therapy may provide an opportunity to modify negative views of the self and/or others and promote a more secure attachment (Danquah & Berry, 2013).
Future research should consider and address the methodological limitations of currently published findings. It would be useful for future research to use longitudinal designs, control for several relevant confounders, and include more comprehensive assessments of paranoia (e.g., not limited to a single item upon a measure), all of which would also help to minimize construct overlap and better elucidate specific associations between insecure attachment and specific constructs of paranoia. Utilizing attachment measures that explore varying representations (including fearful/disorganized attachment) would be useful across the phase of illness, in addition to utilizing comprehensive measures of paranoia. Studies that improve the reporting of participant selection procedures, that use more systematic means of sampling, that can recruit more representative samples, would increase the generalizability of results. Importantly, attachment style may change as a result of being diagnosed with psychosis (Berry et al., 2008). Therefore, longitudinal studies of individuals across the psychosis continuum are vital to elucidate any causal directions and could clarify how attachment insecurity may lead to the development and persistence of paranoia within psychosis.
References
- Armijo‐Olivo, S. , Stiles, C. R. , Hagen, N. A. , Biondo, P. D. , & Cummings, G. G. (2010). Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological Research. Journal of Education in Clinical Practices, 18, 12–18. [DOI] [PubMed] [Google Scholar]
- Bartholomew, K. , & Horowitz, L. M. (1991). Attachment styles among young adults: A test of a four‐category model. Journal of Personality and Social Psychology, 61, 226–244. 10.1037/0022-3514.61.2.226 [DOI] [PubMed] [Google Scholar]
- Bentall, R. P. , de Sousa, P. , Varese, F. , Wickham, S. , Sitko, K. , Haarmans, M. , & Read, J. (2014). From adversity to psychosis: Pathways and mechanisms from specific adversities to specific symptoms. Social Psychiatry and Psychiatric Epidemiology, 49, 1011–1022. 10.1007/s00127-014-0914-0 [DOI] [PubMed] [Google Scholar]
- Bentall, R. P. , & Fernyhough, C. (2008). Social predictors of psychotic experiences: Specificity and psychological mechanisms. Schizophrenia Bulletin, 34, 1012–1020. 10.1093/schbul/sbn103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry, K. , Barrowclough, C. , & Wearden, A. (2007). A review of the role of adult attachment style in psychosis: Unexplored issues and questions for further research. Clinical Psychology Review, 27, 458–475. 10.1016/j.cpr.2006.09.006 [DOI] [PubMed] [Google Scholar]
- Berry, K. , Barrowclough, C. , & Wearden, A. (2008). Attachment theory: A framework for understanding symptoms and interpersonal relationships in psychosis. Behaviour Research and Therapy, 46, 1275–1282. 10.1016/j.brat.2008.08.009 [DOI] [PubMed] [Google Scholar]
- Berry, K. , Varese, F. , & Bucci, S. (2017). Cognitive attachment model of voices: Evidence base and future implications. Frontiers in Psychiatry, 8, 111 10.3389/fpsyt.2017.00111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry, K. , Wearden, A. , Barrowclough, C. , & Liversidge, T. (2006). Attachment styles, interpersonal relationships and psychotic phenomena in a non‐clinical student sample. Personality and Individual Differences, 41, 707–718. 10.1016/j.paid.2006.03.009 [DOI] [Google Scholar]
- Bo, S. , Abu‐Akel, A. , Kongerslev, M. , Haahr, U. H. , & Simonsen, E. (2011). Risk factors for violence among patients with schizophrenia. Clinical Psychology Review, 31, 711–726. 10.1016/j.cpr.2011.03.002 [DOI] [PubMed] [Google Scholar]
- Borenstein, M. , Cooper, H. , Hedges, L. , & Valentine, J. (2009). Effect sizes for continuous data. The Handbook of Research Synthesis and Meta‐Analysis, 2, 221–235. [Google Scholar]
- Bowlby, J. (1969). Attachment. Attachment and loss: Vol. 1: Loss. New York, NY: Basic Books. [Google Scholar]
- Carr, S. C. , Hardy, A. , & Fornells‐Ambrojo, M. (2017). Relationship between attachment style and symptom severity across the psychosis spectrum: A meta‐analysis. Clinical Psychology Review, 59, 145–158. 10.1016/j.cpr.2017.12.001 [DOI] [PubMed] [Google Scholar]
- Castilho, P. , Martins, M. J. , Pinto, A. M. , Viegas, R. , Carvalho, S. , & Madeira, N. (2017). Understanding the effect of attachment styles in paranoid ideation: The mediator role of experiential avoidance. Journal of Contextual Behaviour Science, 6(1), 42–46. 10.1016/j.jcbs.2016.11.007 [DOI] [Google Scholar]
- Collins, N. L. , & Read, S. J. (1990). Adult attachment, working models, and relationship quality in dating couples. Journal of Personality and Social Psychology, 58(4), 644 10.1037/0022-3514.58.4.644 [DOI] [PubMed] [Google Scholar]
- Collins, N. L. , & Read, S. J. (1994). Cognitive representations of attachment: The structure and function of working models In Bartholomew K. & Perlman D. (Eds.), Advances in personal relationships, Vol. 5. Attachment processes in adulthood (pp. 53–90). London, UK: Jessica Kingsley Publishers. [Google Scholar]
- Danquah A. N., & Berry K. (Eds.) (2013). Attachment theory in adult mental health: A guide to clinical practice. New York, NY: Routledge. [Google Scholar]
- Derogatis, L. R. (1975). The SCL‐90‐R. Baltimore, MD: Johns Hopkins University School of Medicine, Clinical Psychometric Research Unit. [Google Scholar]
- Derogatis, L. R. (1997). SCL‐90: Administration, scoring and procedures manual‐I for the (revised) version and other instruments of the psychopathology rating scale. Clinical Psychometrics Research Unit, Johns Hopkins University School of Medicine. [Google Scholar]
- Derogatis, L. R. , & Melisaratos, N. (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13, 595–605. 10.1017/S0033291700048017 [DOI] [PubMed] [Google Scholar]
- Derogatis, L. R. , Rickels, K. , & Rock, A. F. (1976). The SCL‐90 and the MMPI: A step in the validation of a new self‐report scale. The British Journal of Psychiatry, 128(3), 280–289. 10.1192/bjp.128.3.280 [DOI] [PubMed] [Google Scholar]
- Derogatis, L. R. , & Spencer, P. M. (1982). Administration and procedures: BSI. Baltimore, MD: Johns Hopkins University School of Medicine, Clinical Psychometric Research Unit. [Google Scholar]
- Dozier, M. , & Lee, S. W. (1995). Discrepancies between self‐and other‐report of psychiatric symptomatology: Effects of dismissing attachment strategies. Developmental Psychopathology, 7, 217–226. 10.1017/S095457940000643X [DOI] [Google Scholar]
- Fett, A. K. , Shergill, S. S. , Korver‐Nieberg, N. , Yakub, F. , Gromann, P. M. , & Krabbendam, L. (2016). Learning to trust: Trust and attachment in early psychosis. Psychological Medicine, 46, 1437–1447. 10.1017/S0033291716000015 [DOI] [PubMed] [Google Scholar]
- Fraley, R. C. , Heffernan, M. E. , Vicary, A. M. , & Brumbaugh, C. C. (2011). The experiences in close relationships—Relationship Structures Questionnaire: A method for assessing attachment orientations across relationships. Psychological Assessment, 23, 615 10.1037/a0022898 [DOI] [PubMed] [Google Scholar]
- Freeman, D. (2016). Persecutory delusions: A cognitive perspective on understanding and treatment. The Lancet Psychiatry, 3, 685–692. 10.1016/S2215-0366(16)00066-3 [DOI] [PubMed] [Google Scholar]
- Freeman, D. , Freeman, J. , & Garety, P. (2016). Overcoming paranoid and suspicious thoughts: A selfhelp guide using cognitive behavioural techniques. Hachette, UK. [Google Scholar]
- Freeman, D. , & Garety, P. (2014). Advances in understanding and treating persecutory delusions: A review. Social Psychiatry and Psychiatric Epidemiology., 49, 1179–1189. 10.1007/s00127-014-0928-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman, D. , Garety, P. A. , Bebbington, P. E. , Smith, B. , Rollinson, R. , Fowler, D. , … Dunn, G. (2005). Psychological investigation of the structure of paranoia in a non‐clinical population. British Journal of Psychiatry, 186, 427–435. 10.1192/bjp.186.5.427 [DOI] [PubMed] [Google Scholar]
- Freeman, D. , Garety, P. A. , Kuipers, E. , Fowler, D. , & Bebbington, P. E. (2002). A cognitive model of persecutory delusions. British Journal of Clinical Psychology, 41, 331–347. 10.1348/014466502760387461 [DOI] [PubMed] [Google Scholar]
- Freeman, D. , Pugh, K. , Dunn, G. , Evans, N. , Sheaves, B. , Waite, F. , … Fowler, D. (2014). An early Phase II randomised controlled trial testing the effect on persecutory delusions of using CBT to reduce negative cognitions about the self: the potential benefits of enhancing self confidence. Schizophrenia Research, 160(1–3), 186–192. 10.1016/j.schres.2014.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- George, C. , Kaplan, N. , & Main, M. (1996). Adult Attachment Interview (3rd ed.). Berkley, CA: University of California. [Google Scholar]
- Green, C. E. L. , Freeman, D. , Kuipers, E. , Bebbington, P. , Fowler, D. , Dunn, G. , & Garety, P. A. (2008). Measuring ideas of persecution and social reference: The Green et al. Paranoid Thought Scales (GPTS). Psychological Medicine, 38(1), 101–111. 10.1017/S0033291707001638 [DOI] [PubMed] [Google Scholar]
- Gumley, A. I. , Taylor, H. E. F. , Schwannauer, M. , & MacBeth, A. (2014). A systematic review of attachment and psychosis: Measurement, construct validity and outcomes. Acta Psychiatrica Scandinavica, 129, 257–274. 10.1111/acps.12172 [DOI] [PubMed] [Google Scholar]
- Hazan, C. , & Shaver, P. (1987). Romantic love conceptualized as an attachment process. Journal of Personality and Social Psychology, 52, 511 10.1037/0022-3514.52.3.511 [DOI] [PubMed] [Google Scholar]
- Horton, L. E. , Barrantes‐Vidal, N. , Silvia, P. J. , & Kwapil, T. R. (2014). Worries about being judged versus being harmed: Disentangling the association of social anxiety and paranoia with schizotypy. PLoS One, 9(6), e96269 10.1371/journal.pone.0096269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton, P. , Kelly, J. , Lowens, I. , Taylor, P. J. , & Tai, S. (2013). Self‐attacking and self‐reassurance in persecutory delusions: A comparison of healthy, depressed and paranoid individuals. Psychiatry Research, 205(1–2), 127–136. 10.1016/j.psychres.2012.08.010 [DOI] [PubMed] [Google Scholar]
- Kay, S. R. , Fiszbein, A. , & Opfer, L. A. (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13, 261 10.1093/schbul/13.2.261 [DOI] [PubMed] [Google Scholar]
- Korver, N. , Quee, P. J. , Boos, H. , Simons, C. J. , & Haan, L. (2012). Genetic Risk and Outcome of Psychosis (GROUP), a multi site longitudinal cohort study focused on gene–environment interaction: Objectives, sample characteristics, recruitment and assessment methods. International Journal of Methods in Psychiatric Research, 21, 205–221. 10.1002/mpr.1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korver‐Nieberg, N. , Berry, K. , Meijer, C. , de Haan, L. , & Ponizovsky, A. M. (2015). Associations between attachment and psychopathology dimensions in a large sample of patients with psychosis. Psychiatry Research, 228(1), 83–88. 10.1016/j.psychres.2015.04.018 [DOI] [PubMed] [Google Scholar]
- Korver‐Nieberg, N. , Berry, K. , Meijer, C. J. , & Haan, L. (2014). Adult attachment and psychotic phenomenology in clinical and non‐clinical samples: A systematic review. Psychology and Psychotherapy: Theory, Research and Practice, 87(2), 127–154. 10.1111/papt.12010 [DOI] [PubMed] [Google Scholar]
- Korver‐Nieberg, N. , Fett, A. K. J. , Meijer, C. J. , Koeter, M. W. , Shergill, S. S. , de Haan, L. , & Krabbendam, L. (2013). Theory of mind, insecure attachment and paranoia in adolescents with early psychosis and healthy controls. The Australian and New Zealand Journal of Psychiatry, 47, 737–745. 10.1177/0004867413484370 [DOI] [PubMed] [Google Scholar]
- Liotti, G. (2004). Trauma, dissociation, and disorganized attachment: Three strands of a single braid. Psychotherapy: Theory, Research, Practice, Training, 41(4), 472 10.1037/0033-3204.41.4.472 [DOI] [Google Scholar]
- Lyons‐Ruth, K. , & Jacobvitz, D. (1999). Attachment disorganization: Unresolved loss, relational violence, and lapses in behavioral and attentional strategies In Cassidy J. & Shaver P. R. (Eds.), Handbook of attachment: Theory, research, and clinical applications (pp. 520–554). New York, NY: The Guilford Press. [Google Scholar]
- MacBeth, A. , Gumley, A. , Schwannauer, M. , & Fisher, R. (2011). Attachment states of mind, mentalization, and their correlates in a first‐episode psychosis sample. Psychology and Psychotherapy: Theory, Research, and Practice, 84(1), 42–57. 10.1348/147608310X530246 [DOI] [PubMed] [Google Scholar]
- MacBeth, A. , Schwannauer, M. , & Gumley, A. (2008). The association between attachment style, social mentalities, and paranoid ideation: An analogue study. Psychology and Psychotherapy: Theory, Research, and Practice, 81(1), 79–93. 10.1348/147608307X246156 [DOI] [PubMed] [Google Scholar]
- Main, M. , & Solomon, J. (1990). Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation In Greenberg M. T., Dante C. D. & Cummings E. M. (Eds.), Attachment in the preschool years: Theory, research, and intervention (pp. 121–160). Chicago, IL: University of Chicago Press. [Google Scholar]
- Mann, C. J. (2003). Observational research methods. Research design II: Cohort, cross sectional, and case‐control studies. Emergency Medicine Journal, 20(1), 54–60. 10.1136/emj.20.1.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melo, S. , Corcoran, R. , Shryane, N. , & Bentall, R. P. (2009). The persecution and deservedness scale. Psychology and Psychotherapy: Theory, Research, and Practice, 82, 247–260. 10.1348/147608308X398337 [DOI] [PubMed] [Google Scholar]
- Mickelson, K. D. , Kessler, R. C. , & Shaver, P. R. (1997). Adult attachment in a nationally representative sample. Journal of Personality and Social Psychology, 73, 1092 10.1037/0022-3514.73.5.1092 [DOI] [PubMed] [Google Scholar]
- Mikulincer, M. , & Shaver, P. R. (2012). An attachment perspective on psychopathology. World Psychiatry, 11(1), 11–15. 10.1016/j.wpsyc.2012.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikulincer, M. , Shaver, P. R. , & Pereg, D. (2003). Attachment theory and affect regulation: The dynamics, development, and cognitive consequences of attachment‐related strategies. Emotion, 27(2), 77–102. 10.1023/A:1024515519160 [DOI] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , & Prisma Group (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moutoussis, M. , Williams, J. , Dayan, P. , & Bentall, R. P. (2007). Persecutory delusions and the conditioned avoidance paradigm: Towards an integration of the psychology and biology of paranoia. Cognitive Neuropsychiatry, 12, 495–510. 10.1080/13546800701566686 [DOI] [PubMed] [Google Scholar]
- Pearce, J. , Simpson, J. , Berry, K. , Bucci, S. , Moskowitz, A. , & Varese, F. (2017). Attachment and dissociation as mediators of the link between childhood trauma and psychotic experiences. Clinical Psychology & Psychotherapy, 24, 1304–1312. 10.1002/cpp.2100 [DOI] [PubMed] [Google Scholar]
- Persons, J. B. (1986). The advantages of studying psychological phenomena rather than psychiatric diagnosis. American Psychologist, 41, 1252–1260. 10.1037/0003-066X.41.11.1252 [DOI] [PubMed] [Google Scholar]
- Phillips, L. J. , Francey, S. M. , Edwards, J. , & McMurray, N. (2009). Strategies used by psychotic individuals to cope with life stress and symptoms of illness a systematic review. Anxiety Stress and Coping, 22, 371–410. 10.1080/10615800902811065 [DOI] [PubMed] [Google Scholar]
- Pickering, L. , Simpson, J. , & Bentall, R. P. (2008). Insecure attachment predicts proneness to paranoia but not hallucinations. Personality and Individual Differences, 44, 1212–1224. 10.1016/j.paid.2007.11.016 [DOI] [Google Scholar]
- Ponizovsky, A. M. , Arbitman, M. , Baumgarten‐Katz, I. , & Grinshpoon, A. (2014). Attachment styles, quality of life and service satisfaction outcomes in people with schizophrenia in Israel. Schizophrenia Research, 1(1), 1–9. [Google Scholar]
- Ponizovsky, A. M. , Nechamkin, Y. , & Rosca, P. (2007). Attachment patterns are associated with symptomatology and course of schizophrenia in male inpatients. American Journal of Orthopsychiatry, 77, 324 10.1037/0002-9432.77.2.324 [DOI] [PubMed] [Google Scholar]
- Ponizovsky, A. M. , Vitenberg, E. , Baumgarten‐Katz, I. , & Grinshpoon, A. (2013). Attachment styles and affect regulation among outpatients with schizophrenia: Relationships to symptomatology and emotional distress. Psychology and Psychotherapy: Theory, Research, and Practice, 86, 164–182. 10.1111/j.2044-8341.2011.02054.x [DOI] [PubMed] [Google Scholar]
- Schlier, B. , Jaya, E. S. , Moritz, S. , & Lincoln, T. M. (2015). The Community Assessment of Psychic Experiences measures nine clusters of psychosis‐like experiences: A validation of the German version of the CAPE. Schizophrenia Research, 169(1–3), 274–279. 10.1016/j.schres.2015.10.034 [DOI] [PubMed] [Google Scholar]
- Scollon, C. N. , Prieto, C. K. , & Diener, E. (2009). Experience sampling: Promises and pitfalls, strength and weaknesses In Diener E. (Ed.), Assessing well‐being: Social indicators research series (pp. 157–180). Dordrecht, the Netherlands: Springer; 10.1007/978-90-481-2354-4 [DOI] [Google Scholar]
- Shevlin, M. , McAnee, G. , Bentall, R. P. , & Murphy, J. (2015). Specificity of association between adversities and the occurrence and co‐occurrence paranoia and hallucinations: Evaluating the stability of childhood risk in an adverse adult environment. Psychosis, 7, 206–216. 10.1080/17522439.2014.980308 [DOI] [Google Scholar]
- Sitko, K. , Varese, F. , Sellwood, W. , Hammond, A. , & Bentall, R. (2016). The dynamics of attachment insecurity and paranoid thoughts: An experience sampling study. Psychiatry Research, 246, 32–38. 10.1016/j.psychres.2016.08.057 [DOI] [PubMed] [Google Scholar]
- Statham, V. , Emerson, L. M. , & Rowse, G. (2019). A systematic review of self‐report measures of paranoia. Psychological Assessment, 31(2), 139 10.1037/pas0000645 [DOI] [PubMed] [Google Scholar]
- Stefanis, N. C. , Hanssen, M. , Smirnis, N. K. , Avramopoulos, D. A. , Evdokimidis, I. K. , Stefanis, C. N. , & Van Os, J. (2002). Evidence that three dimensions of psychosis have a distribution in the general population. Psychological Medicine, 32, 347–358. 10.1017/S0033291701005141 [DOI] [PubMed] [Google Scholar]
- Strand, J. , Goulding, A. , & Tidefors, I. (2015). Attachment styles and symptoms in individuals with psychosis. Nordic Journal of Psychiatry, 69(1), 67–72. 10.3109/08039488.2014.929740 [DOI] [PubMed] [Google Scholar]
- Thomas, B. H. , Ciliska, D. , Dobbins, M. , & Micucci, S. (2004). A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews on Evidence Based Nursing, 1, 176–184. 10.1111/j.1524-475X.2004.04006.x [DOI] [PubMed] [Google Scholar]
- Udachina, A. , Varese, F. , Oorschot, M. , Myin‐Germeys, I. , & Bentall, R. P. (2012). Dynamics of self‐esteem in “poor‐me” and “bad‐me” paranoia. The Journal of Nervous and Mental Disease, 200, 777–783. 10.1097/NMD.0b013e318266ba57 [DOI] [PubMed] [Google Scholar]
- Varese, F. , Udachina, A. , Myin‐Germeys, I. , Oorschot, M. , & Bentall, R. P. (2011). The relationship between dissociation and auditory verbal hallucinations in the flow of daily life of patients with psychosis. Psychosis, 3(1), 14–28. 10.1080/17522439.2010.548564 [DOI] [Google Scholar]
- Wickham, S. , Sitko, K. , & Bentall, R. P. (2015). Insecure attachment is associated with paranoia but not hallucinations in psychotic patients: The mediating role of negative self‐esteem. Psychological Medicine, 45, 1495–1507. 10.1017/S0033291714002633 [DOI] [PubMed] [Google Scholar]


