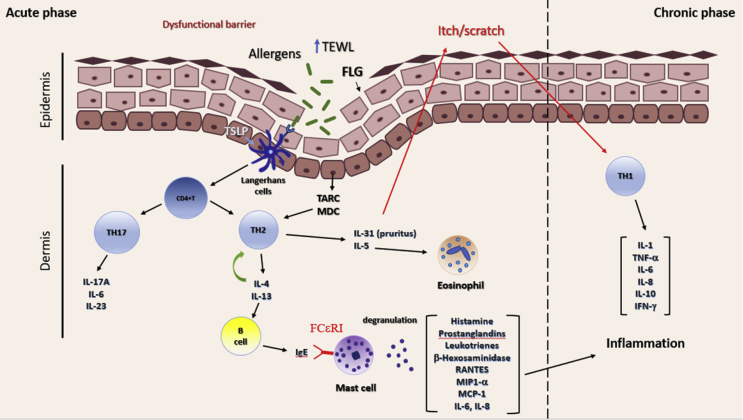
Fig. 1.
AD patients have a dysfunctional epidermis due to a mutation in the filaggrin gene (FLG) that allows transepidermal water loss (TEWL) and easy entrance of allergens in the skin. Allergens induce the production of the thymus and activation-regulated chemokine (TARC), macrophage-derived chemokine (MDC), and thymic stromal lymphopoietin (TSLP) in the keratinocytes. TLSP activates Langerhans cells (dendritic cells), which induce the differentiation of CD4+T cells into T helper type 2 cells (TH2), whose infiltration into tissue is mediated by TARC and MDC. TH2 cells produce IL-4, IL-5, IL-13, and IL-31, among others. IL-31 induces pruritus response in the epidermis, which causes the change into the inflammatory chronic phase. IL-5 is related to eosinophil recruitment to the damaged tissue, whereas IL-4 further induces TH2 polarization and IgE production by B cells. IgE crosslinks with specific receptor FCεRI on mast cells, causing mast cell degranulation and release of allergic mediators (histamine, prostaglandins, leukotrienes, MIP-α, MCP-1, IL-6, and IL-8), which in cooperation with T helper cells type 1 (TH1) released mediators (IL-1, IL-6, IL-8, IL-10, TNF-α, and IFN-γ) enhance the inflammatory phase of AD. Recently, TH17 secreted mediators (IL-17A, IL-6, IL-23) have been shown to play a role in the development of AD.
IL, interleukin; AD, atopic dermatitis; IFN, interferon; MCP-1, monocyte chemoattractant protein-1; TNF-α, tumor necrosis factor-alpha; MIP, macrophage inflammatory protein; IgE, immunoglobulin E.