Abstract
We aimed to use hand dexterity and grip strength test as objective measures to compare the difference in surgeon fatigue associated with robotic and laparoscopic colorectal surgery. We used the Purdue Pegboard Test to assess hand dexterity and the Camry Electronic Handgrip Dynamometer to assess hand grip strength. Eighteen patients were operated on, including 10 robotic and 8 laparoscopic cases. Statistical analysis revealed no difference in dexterity or muscle fatigue after operating with the robot. In contrast, there was a significant difference in the hand grip strength of both hands after laparoscopic surgery. Our results show that the resultant fatigue after laparoscopy affects both hands of the surgeon. In contrast, there was no difference in dexterity or muscle fatigue after operating with the robot. Given the demands of complex colorectal surgeries, robotics may be a means of optimizing surgeon performance by reducing fatigue.
Keywords: ergonomics, fatigue, minimally invasive surgery, laparoscopy, robot
INTRODUCTION
While minimally invasive techniques have been introduced for various types of colorectal procedures, the widespread adoption of minimally invasive surgery (MIS) has been hampered by the technical challenges associated with their implementation. Studies have shown that performing laparoscopic surgery imposes more physical stress on the surgeon than open surgery [1], and authors have also described how the resultant surgical fatigue can result in mental exhaustion, increased irritability, impaired surgical judgement and reduced dexterity [2,3]. Indeed, the benefits of laparoscopy to patients appear to come at the expense of their surgeons’ well-being.
While numerous publications have failed to demonstrate an improvement in clinical outcomes after robotic surgery, one of the true advantages of robotics—ergonomics—remains unrefuted but difficult to objectively quantify. Earlier studies evaluating surgical ergonomics have mainly utilized subjective assessments and self-reported measures like questionnaires [4,5]. In addition, there is also a sparsity of studies looking into the effect of fatigue affecting surgical performance [6]. We aimed to use hand dexterity and grip strength test as objective measures to compare the difference in surgeon fatigue associated with robotic and laparoscopic colorectal surgery.
MATERIALS AND METHODS
A pilot study was conducted between February 2019 and May 2019. We used the Purdue Pegboard Test (PBT) to assess hand dexterity and the Camry Electronic Handgrip Dynamometer to assess hand grip strength (Figure A & B). Before each operative procedure, the surgeon was tasked by a qualified occupational therapist (YHT) to perform the PBT in a standardized sequence. This was followed by the hand grip strength test for the right hand (five times) and then the left hand (five times). Two hours into each surgery, the surgeon would take a technique break and repeat both tests in the same sequence.
Figure 1.
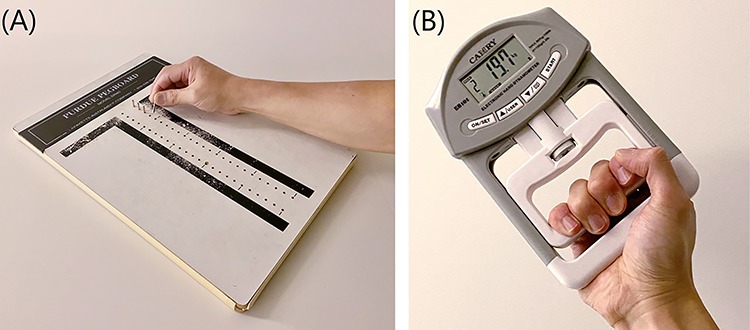
(A) Purdue Pegboard Test; (B) Camry Electronic Handgrip Dynamometer.
RESULTS
Eighteen patients were operated on, including 10 robotics cases and 8 laparoscopic ones. Table 1 summarizes the patient demographic and operative details. In the robotic group, the mean number of pegs placed in 30 seconds for the right hand prior to surgery was 13.5; 11.4 for the left hand and 9.9 for both hands (Table 2). The mean number for assembling in 60 seconds was 7.8. The mean grip strength for the right and left hands was 36.9 and 31.1 kg, respectively. The corresponding results after operative for 2 hours were 13.0, 10.9, 8.9 and 7.6. The mean grip strength for the right hand was 36.1 and 30.6 kg for the left hand. Statistical analysis revealed no difference in dexterity or muscle fatigue after operating with the robot. In the laparoscopic group, the mean number of pegs placed in 30 seconds for the right hand prior to surgery was 13.5; 11.5 for the left hand and 9.6 for both hands. The mean number for assembling in 60 seconds was 8.2. The mean grip strength for the right and left hands was 37.7 and 32.3 kg, respectively. The corresponding results after operating for 2 hours were 14.0, 10.8, 9.8 and 8.0. The mean grip strength for the right hand was 35.0 and 29.0 kg for the left hand. In contrast, there was a significant difference in the hand grip strength of right and left hands after laparoscopic surgery (P = 0.04 and 0.02, respectively).
Table 1.
Patients’ demographic and operative procedure
| Operative procedure | Laparoscopy (n = 8) | Robot (n = 10) |
|---|---|---|
| Gender (F:M) | 4: 4 | 4: 6 |
| Age (year) | 70.3 | 56.3 |
| BMI (kg/m2) | 22.2 | 28.1 |
| Operative procedure | ||
| Right hemicolectomy | 4 | - |
| Left hemicolectomy | 1 | - |
| Subtotal colectomy | 2 | - |
| Low anterior resection | 1 | 5 |
| Anterior resection | - | 1 |
| Radical proctectomy | - | 1 |
| Transanal surgery | - | 3 |
Table 2.
Hand dexterity and grip strength test before surgery (Test 1) and after 2 hours of operating (Test 2)
| Test 1 | Test 2 | P value | |
|---|---|---|---|
| Hand dexterity test | |||
| Right hand | |||
| Robot | 13.5 | 13.0 | 0.18 |
| Laparoscopy | 13.5 | 14.0 | 0.17 |
| Left hand | |||
| Robot | 11.4 | 10.9 | 0.32 |
| Laparoscopy | 11.5 | 10.8 | 0.38 |
| Both hands | |||
| Robot | 9.9 | 8.9 | 0.06 |
| Laparoscopy | 9.6 | 9.8 | 0.76 |
| Assemble | |||
| Robot | 7.8 | 7.6 | 0.52 |
| Laparoscopy | 8.2 | 8.0 | 0.71 |
| Hand grip strength test (kg) | |||
| Right hand | |||
| Robot | 36.9 | 36.1 | 0.42 |
| Laparoscopy | 37.7 | 35.0 | 0.04* |
| Left hand | |||
| Robot | 31.1 | 30.6 | 0.61 |
| Laparoscopy | 32.3 | 29.0 | 0.02* |
Comparing individual test results between the robotic and laparoscopic groups showed no significant difference in dexterity and fatigue.
DISCUSSIONS
The challenges of laparoscopy have been attributed to the shortcomings in the design of conventional instruments and the awkward posturing adopted by operators for protracted periods of surgery. Most laparoscopic instruments incorporate a ringed pistol-type handle that results in excessive flexion and deviation of the surgeon’s wrist during tissue manipulation. The hand-to-tip force transmission is also less efficient compared to the instruments used in open surgery [7]. The visual display of the operative field is also paramount to the conduct of laparoscopic surgery. While three-dimensional scope systems have been introduced in an attempt to address the lack of stereopsis, many of these still suffer from limitations, such as the loss of light intensity as a result of using polarized glasses [8]. Robotic surgical system not only reduces the reliance on a trained assistant, it also provides greater surgeon comfort, autonomy and improved fluidity of surgical motion [9]. Newer generation scopes also provide superior image quality and depth perception.
Our results show that the amount of physical fatigue after laparoscopy is significantly more, affecting both hands of the surgeon. However, the dexterity and presumable overall performance of the surgeon was not impaired. This could be because the PBT did not require significant motor power to complete, and perhaps the hand-eye coordination of an experienced MIS surgeon was able to compensate for the loss of strength. Alternatively, the complexity of the cases performed laparoscopically might not have been enough to stress the surgeon, or this might not have been apparent after only 2 hours of operating, taking into account that the timing also included less-demanding tasks like port placement. Conversely, it could be argued that the use of robotics mitigated the amount of fatigue experienced by the surgeon even in complex colorectal operations, given that the majority of the robotic cases were either low anterior resection or transanal procedures. Given the demands of complex colorectal surgeries and high-volume workload, robotics may be a means of optimizing surgeon performance by reducing fatigue [10]. This would expectedly help to reduce iatrogenic injuries and mistakes caused by human error and possibly justify the added expense of robotic technology.
As this was a pilot study evaluating the feasibility of such a method of assessment, our analysis inevitably suffers from the limitations of a small sample size. In addition, operator posture and arm positions during surgery were not recorded, although these were assumed to have been ergonomically ideal given the experience of the surgeon studied. While the study of a single surgeon’s ergonomics allowed comparability across the two MIS platforms, it also limited the generalizability of our findings. The results may also differ from surgeons who utilize different laparoscopic and robotic equipment from our institution.
Conflict of interest statement
None declared.
ACKNOWLEDGEMENT
L.-J.K.: original idea creator and manuscript writing; J.C.-Y.N.: data interpretation and participate manuscript writing; C.-C.C.: participate in operative procedure and Y.-K.L.: data interpretation and statistics analysis.
References
- 1. Berguer R, Smith WD, Chung YH. Performing laparoscopic surgery is significantly more stressful for the surgeon than open surgery. Surg Endosc 2001;15:1204–7. [DOI] [PubMed] [Google Scholar]
- 2. Cuschieri A. Whither minimal access surgery: Tribulations and expectations. Am J Surg 1995;169:9–19. [DOI] [PubMed] [Google Scholar]
- 3. Grissinger M. An exhausted workforce increases the risk of errors. PT 2009;34:120–3. [PMC free article] [PubMed] [Google Scholar]
- 4. Moore LJ, Wilson MR, McGrath JS, Waine E, Masters RS, Vine SJ. Surgeons' display reduced mental effort and workload while performing robotically assisted surgical tasks, when compared to conventional laparoscopy. Surg Endosc 2015;29:2553–60. [DOI] [PubMed] [Google Scholar]
- 5. Dias RD, Ngo-Howard MC, Boskovski MT, Zenati MA, Yule SJ. Systematic review of measurement tools to assess surgeons' intraoperative cognitive workload. Br J Surg 2018;105:491–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCormick F, Kadzielski J, Landrigan CP, Evans B, Herndon JH, Rubash HE. Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg 2012;147:430–5. [DOI] [PubMed] [Google Scholar]
- 7. Berguer R, Forkey DL, Smith WD. Ergonomic problems associated with laparoscopic surgery. Surg Endosc 1999;13:466–8. [DOI] [PubMed] [Google Scholar]
- 8. Schwab K, Smith R, Brown V, Whyte M, Jourdan I. Evolution of stereoscopic imaging in surgery and recent advances. World J Gastrointest Endosc 2017;9:368–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Köckerling F. Robotic vs. standard laparoscopic technique - what is better? Front Surg 2014;1:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hurley AM, Kennedy PJ, O’Connor L, Dinan TG, Cryan JF, Boylan G, et al. SOS save our surgeons: stress levels reduced by robotic surgery. Gynecol Surg 2015;12:197–206. [Google Scholar]


