Abstract
Background:
Shoulder pain and dysfunction are common indications for rotator cuff repair surgery, yet the factors that are associated with these symptoms are not fully understood.
Purpose/Hypothesis:
This study aimed to investigate the associations of patient and disease-specific factors with baseline patient-reported outcome measures (PROMs) in patients undergoing rotator cuff repair. We hypothesized that tear size and mental health status, as assessed by the Veterans RAND 12-Item Health Survey mental component score (VR-12 MCS), would be associated with baseline total Penn Shoulder Score (PSS) and its pain, function, and satisfaction subscale scores.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
We prospectively identified 12 patient factors and 12 disease-specific factors as possible statistical predictors for baseline PROMs in patients undergoing surgical repair of superior-posterior rotator cuff tears at a single institution over a 3-year period. Multivariable statistical modeling and Akaike information criterion comparisons were used to investigate the unique associations with, and relative importance of, these factors in accounting for variation in baseline PSS and its subscale scores.
Results:
A total of 1442 patients who had undergone surgery by 23 surgeons met inclusion criteria, with a baseline median total PSS of 38.5 (pain, 12; function, 24.2; satisfaction, 2). Adjusted R2 in multivariable models demonstrated that the 24 general patient and disease-specific factors accounted for 22% to 24% of the variability in total PSS and its pain and function subscale scores. Large/massive tear size was significantly associated with worse PSS total score and function score but not pain or satisfaction scores. Lower VR-12 MCS was significantly associated with worse total PSS and all 3 subscale scores. Among other factors significantly associated with baseline PROMs were sex, race, preoperative opioid use, years of education, employment status, acromion status, and adhesive capsulitis. Lower VR-12 MCS, preoperative opioid use, female sex, and black race were the factors most strongly associated with baseline PROMs.
Conclusion:
Large/massive tear size, lower VR-12 MCS, and several additional patient and disease-specific factors are associated with baseline PROMs in patients undergoing rotator cuff repair. Further studies are needed to investigate whether these factors will also predict poor postoperative PROMs.
Keywords: shoulder, rotator cuff repair, pain, function, satisfaction, PROMs, Penn Shoulder Score, preoperative factors, multivariable model
Rotator cuff (RC) tears are present in approximately 30% of individuals by 70 years of age; these tears may remain asymptomatic in some patients16,19,37 and can cause pain, weakness, and loss of shoulder function in others.24,29 During surgical decision making, baseline symptoms related to shoulder pain and function are often considered together with patient demographics, such as age and comorbidities, and disease-specific factors, such as tear type and size.7 Yet the relationships of baseline pain and function to patient and tear characteristics are not fully understood.
A limited number of studies have investigated the relationships of general patient factors and tear characteristics with baseline pain and function, with varying results.6,9,11,18,36 Age,6,18 sex,6,11,18 race,9,18 body mass index (BMI),36 smoking,18 comorbidities,6,9 education level,9,11 and mental health status3,6,36 have been shown to correlate with baseline pain and/or function in patients with RC tears. However, with the exception of 1 study,36 RC tear characteristics have not been shown to be associated with baseline pain and function.6,9,11,18 These previous studies have generally been of modest size, relatively homogeneous due to narrow selection criteria, and based on retrospective collection of limited numbers of variables for analysis, thereby limiting their power and generalizability. Factors that potentially affect preoperative status were not prospectively collected on a large cohort in these prior studies.
To address the need for high-quality, prospective, standardized data surrounding orthopaedic procedures, the Cleveland Clinic has developed the Orthopaedic Minimal Data Set Episode of Care system (OME).5 Currently, OME prospectively collects sociodemographic factors, joint-specific variables of disease severity and treatment, and joint-specific validated patient-reported outcome measures (PROMs) at baseline and 1 year after treatment for more than 30 elective orthopaedic procedures. Data are electronically stored in a secure Research Electronic Data Capture (REDCap)12 database. As of November 2018, OME had been used by 57 orthopaedists at 14 sites within the Cleveland Clinic Health System to document episode-of-care details and PROMs at baseline on 97% of more than 30,000 elective knee, hip, and shoulder surgeries, including more than 2200 patients with RC repair (RCR). This study’s purpose was to investigate the extent to which general patient factors and disease-specific factors are associated with baseline PROMs in patients undergoing RCR. We hypothesized that both larger tear size and worse mental health status as assessed by the Veterans RAND 12-Item Health Survey mental component score (VR-12 MCS) would be associated with worse baseline total Penn Shoulder Score (PSS) and its pain, function, and satisfaction subscale scores. We tested these hypotheses and examined additional relationships in the prospectively collected, comprehensive, and standardized OME cohort data using multivariable analysis with control for confounding by general patient and disease-specific factors.
METHODS
Rotator Cuff Repair Surgical Cohort
Patients undergoing surgery for RC tendon tear at the Cleveland Clinic Health System between February 2015 and February 2018 were considered for the study and were included if undergoing repair of superior-posterior RC tears, defined as a tear of the supraspinatus, infraspinatus, and/or teres minor tendons. Patients with superior-posterior RC tears that were not repaired (due to the tears being low-grade partial-thickness, or irreparable), isolated subscapularis tendon tears, and/or incomplete baseline data acquisition were excluded.
Variable Selection
A total of 24 preoperative patient and disease-specific factors were prospectively identified as possible predictors for baseline pain, function, and satisfaction. These included 12 general patient factors (age, sex, race, BMI, smoking status [nonsmoker, former, current], preoperative opioid use, years of education, employment status [not employed, employed, retired], workers’ compensation status, mental health status [VR-12 MCS], comorbidities [Charlson comorbidity index, CCI], and chronic pain) and 12 disease-specific factors (prior shoulder surgery, RC tear type, RC tear size [small, medium, large/massive], surgical repair type, subscapularis tendon status, biceps tendon tear type, acromioclavicular [AC] joint status, glenoid cartilage status, humeral head cartilage status, acromion status, adhesive capsulitis, and labral tear) (Table 1).
TABLE 1.
Baseline General Patient and Disease-Specific Characteristics of 1442 Patients Undergoing Superior-Posterior Rotator Cuff Tendon Repair
| Value | |
|---|---|
| General Patient Characteristics | |
| Age, ya | 58 (52–64) |
| Body mass indexa | 29.2 (25.8–33.1) |
| Charlson comorbidity indexa | 1 (0–3) |
| Education, ya | 14 (12–16) |
| VR-12 mental component scorea | 52.9 (43.1–60.5) |
| Sex | |
| Female | 565 (39) |
| Male | 877 (61) |
| Race | |
| White | 1112 (77) |
| Black | 176 (12) |
| Other | 30 (2) |
| Not available | 124 (9) |
| Smoking status | |
| Current | 223 (15) |
| Quit | 488 (34) |
| Never | 731 (51) |
| Preoperative opioid use | |
| Yes | 654 (45) |
| No | 788 (55) |
| Chronic pain | |
| Yes | 515 (36) |
| No | 927 (64) |
| Employment status | |
| Full-time | 667 (46) |
| Part-time | 38 (3) |
| Retired | 249 (17) |
| Self-employed | 75 (6) |
| Not employed | 394 (27) |
| Not applicable | 19 (1) |
| Workers’ compensation | |
| Yes | 110 (8) |
| No | 1332 (92) |
| Disease-Specific Characteristics | |
| Prior surgery | |
| Yes | 169 (12) |
| No | 1273 (88) |
| Rotator cuff tear type | |
| Full | 1100 (76) |
| Partial | 342 (24) |
| Rotator cuff tear size | |
| Large (3–5 cm)/massive (>5 cm) | 560 (39) |
| Medium (1–3 cm) | 623 (43) |
| Small (<1 cm) | 259 (18) |
| Surgery type | |
| Primary | 1336 (93) |
| Revision | 106 (7) |
| Subscapularis tendon | |
| Torn | 301 (21) |
| Normal | 1141 (79) |
| Biceps tendon tear type | |
| Full | 179 (12) |
| Partial | 499 (35) |
| Normal | 764 (53) |
| Acromioclavicular joint | |
| Abnormal | 132 (9) |
| Normal | 1310 (91) |
| Glenoid cartilage | |
| Grade 3/grade 4 | 68 (5) |
| Normal/grade 1/grade 2 | 1374 (95) |
| Humeral head cartilage | |
| Grade 3/grade 4 | 89 (6) |
| Normal/grade 1/grade 2 | 1353 (94) |
| Acromion | |
| Abnormal | 542 (38) |
| Normal | 900 (62) |
| Adhesive capsulitis | |
| Yes | 45 (3) |
| No | 1397 (97) |
| Labral tear | |
| Yes | 272 (19) |
| No | 1170 (81) |
These values are presented as median (interquartile range). All other values in the table are presented as n (%). VR-12, Veterans RAND 12-Item Health Survey.
The PSS (scored 0 to 100) was selected as the PROM for use because of its demonstrated validity and reliability in assessing the shoulder.13,17 Its subscales include pain (3 items, each on a 10-point scale; 0–30 points), function (20 items, each on a 10-point scale; normalized to 0–60 points), and satisfaction (1 item; 0–10), with higher scores representing less pain, better function, and higher satisfaction.17
Data Source
Data on 20 of the 24 preoperative patient and disease-specific factors were obtained from the Cleveland Clinic’s OME database,5 which is approved by Cleveland Clinic’s institutional review board (#06–196) and has been shown to be a valid and efficient tool for collecting comprehensive and standardized data on RCR.26 Data on 4 factors (comorbidities, preoperative opioid use, chronic pain, and workers’ compensation status) were obtained from the Cleveland Clinic’s electronic medical record (EMR) (Epic Systems), Perioperative Health Documentation System database, and Epic Cost of Goods Sold system. The CCI was calculated from the comorbidity data.22 Preoperative opioid use was counted “yes” if an opioid was prescribed in the patient’s EMR and/or ordered from Epic Cost of Goods Sold between 3 months and 24 hours before surgery. Chronic pain was counted “yes” if the patient’s EMR contained an International Classification of Diseases, Ninth Revision, diagnosis code of 338.2 (chronic pain) and/or 304.0x (opioid dependence).
Statistical Modeling
Multivariable statistical modeling was performed on the eligible cohort to investigate the associations of the 24 general patient factors and disease-specific factors with baseline PSS (total score and the pain, function, and satisfaction subscale scores). All 24 prospectively chosen patient and surgical factors were included as model covariates. Age, BMI, years of education, VR-12 MCS, and CCI were treated as continuous variables. Because the number of degrees of freedom allowed in statistically rigorous multivariable analysis is limited by the size of the cohort, the sample counts for categorical variables were assessed a priori for appropriate opportunities to group clinically similar categories or ones likely too small to allow identification of distinguishable effects (Table 1). For example, glenoid and humeral head cartilage statuses were each reduced to little or no arthritis (normal/grade 1/grade 2) versus significant arthritis (grade 3/grade 4) based on the Outerbridge classification,20 and part-time employment, self-employment, and full-employment categories were combined into a single “employed” group. Similarly, acromion status was reduced to abnormal (eg, presence of os acromiale or acromial spur) or normal. AC joint status was also reduced to abnormal (eg, presence of AC joint arthritis or distal clavicle osteolysis) or normal.
PSS total scores and the pain and function subscale scores were modeled through use of linear regression, and PSS satisfaction subscale scores were modeled through use of proportional odds logistic regression due to assumption violations of linear regression. Trichotomous predictors (race, smoking status, employment status, RC tear size, biceps tendon tear type) were modeled categorically, and tests were conducted both overall and, to clarify the nature of differences, for dichotomous comparisons against respective reference categories of white, non-smokers, employed, small tear size, and normal, respectively. The estimated effects for each predictor on the PSS total, pain, and function scores and the odds ratio for each variable on the PSS satisfaction score were initially determined in the full models. These effects estimate the unique associations of each covariate with each outcome after adjustment for possible confounding by all other covariates. No data-driven variable selection was performed. The 95% confidence intervals, P values, and R2 values for each predictor in the full models are reported. The relative importance of each variable in explaining variation in baseline PROMs was assessed by calculating and ranking the increases in the Akaike information criterion14 upon removal of that variable from the full model.
We used 3 sensitivity analyses to examine the robustness of our results. First, sensitivity to false-positive findings due to testing relationships of each variable with the PSS total score and the 3 subscale scores was examined by Bonferroni-Holm multiple comparison adjustment of each P value for these 4 simultaneous tests. Second, possible interactions of our focal variables, VR-12 MCS and tear size, with other predictors were examined by augmenting the models for each outcome simultaneously by first-order interactions of VR-12 MCS and tear size with every variable statistically significantly related to any of the 4 outcomes after this Bonferroni-Holm adjustment. Because correlated predictors may conceal each other’s effects, we not only examined models containing all these interactions simultaneously, but also used forward selection, backward elimination, and stepwise model fitting to check that prominent interactions were not hidden by mutual adjustments.
Third, we removed plausible causal intermediaries (mediators) from our models. Cross-sectional data collection obscures time sequence and thus the directions of influences inducing statistical correlations. Whereas the 12 disease-specific factors and 6 of the general patient factors are considered relatively stable characteristics of the patients and their baseline condition, 6 patient factors (mental health status, chronic pain, preoperative opioid use, smoking status, employment status, and workers’ compensation status) are more evidently subject to shorter-term influences of each other and the condition motivating the RCR (as reflected in the baseline PSS). In such circumstances, a mutual adjustment model may over-match and obscure strong relationships by analytically mistaking causal mediators for confounders. Given this concern, specifically regarding mental health status but in principle relevant for all these variables, we assessed the effect of their mutual adjustment by fitting 6 additional separate models, each including 1 of these 6 variables in turn and examining, in each model, the change in the retained variable’s effect.
The eligible cohort of 1497 patients in the OME database included 55 patients (3.7%) missing 1 or more PSS components and, among those with complete PSS data, 124 (8.6%) missing data on race, 19 (1.2%) on employment status, 2 (0.14%) on CCI, and 1 (0.07%) on education; data on all other predictors were complete. With multiple outcomes to model, with few missing data, and without reason to expect informative missingness, we addressed missing data by the ad hoc, simplified approach of restricting analysis to the 96.7% of patients with completed PROMs and singly imputing predictors from each other using multivariate imputation by chained equations, an iterative fully conditional approach (mice R package31). The imputation portion of this strategy was expected to slightly attenuate estimated relative to true relationships and slightly understate variability, but with few missing data these effects on analyses should be small relative to other sources of error.
All statistical analyses were performed by use of R software (R version 3.2.3). All testing was 2-sided and considered significant at the 5% level (P < .05).
RESULTS
A total of 2040 patients undergoing surgery for RC tear at Cleveland Clinic facilities between February 2015 and February 2018 were captured in the OME database (Figure 1). Of these, 543 patients were excluded because they either had a superior-posterior RC tear that was not repaired (n = 440; 298 low-grade partial-thickness tears and 142 irreparable tears) or had isolated subscapularis tendon repairs (n = 103). Another 55 patients were excluded because they had incomplete baseline PROM data. Ultimately 1442 patients undergoing superior-posterior RC tendon repair performed by 23 surgeons met inclusion criteria and were available for investigation.
Figure 1.
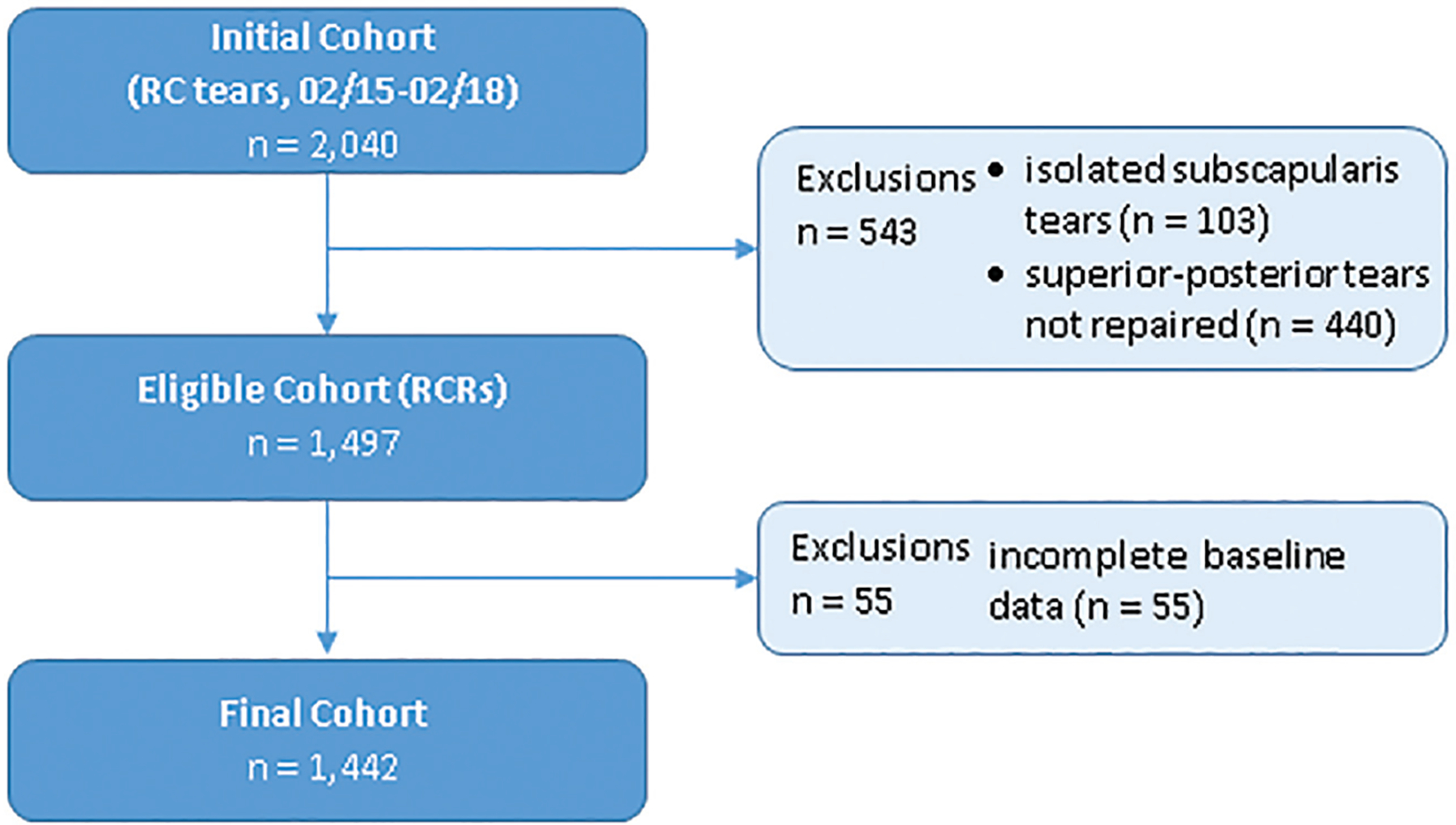
Flowchart of the inclusion and exclusion of patients with rotator cuff repair (RCR).
General Patient and Disease-Specific Characteristics
Table 1 presents the general patient and disease-specific characteristics of the 1442 patients included in this study. Patients had a median age of 58 years, BMI of 29.2, 14 years of education, VR-12 MCS of 52.9, and CCI of 1. Modal patients were white (77%), were male (61%), had primary repair (93%) of a full-thickness (76%) medium-sized (43%) tear, and had no prior shoulder surgery (88%). Further, 49% were current or former smokers, 36% had chronic pain, and 45% used opioids preoperatively. Most patients had a normal subscapularis tendon (79%), normal AC joint (91%), little or no arthritis on the glenoid (95%) or humeral head (94%), no adhesive capsulitis (97%), and no labral tear (81%). The long head of the biceps tendon was abnormal in 47% of patients and the acromion was abnormal in 38% of patients.
Baseline Penn Shoulder Scores
Table 2 presents the baseline PSS (the total score and the pain, function, and satisfaction subscale scores) in the 1442 patients. Patients had a median total PSS of 38.5, pain score of 12, function score of 24.2, and satisfaction score of 2.
TABLE 2.
Baseline Penn Shoulder Scores (Total Score and Pain, Function, and Satisfaction Subscale Scores) in the 1442 Patients Undergoing Superior-Posterior Rotator Cuff Tendon Repair
| Median (Interquartile Range) | Possible Range | |
|---|---|---|
| Total | 38.5 (28–51) | 0–100 |
| Pain | 12 (8–17) | 0–30 |
| Function | 24.2 (16.8–33) | 0–60 |
| Satisfaction | 2 (0–3) | 0–10 |
Multivariable Analysis
Table 3 and Figure 2 display the estimated effects and odds ratios of predictors for baseline PSS and subscale scores in patients undergoing RCR, with 95% confidence intervals and P values for each predictor in the full and partial models. Adjusted R2 in full models demonstrated that the 24 general patient and disease-specific factors accounted for 22% to 24% of the variability in the 3 outcome variables (total PSS and the pain and function scores). We found that 15 of the 24 predictors showed statistically significant associations with at least 1 PSS subscale score when controlling for the other predictors. Among general patient factors, lower VR-12 MCS and preoperative opioid use were significantly associated with lower values of all 3 subscale scores, and employment status was significantly associated with function and satisfaction scores (not employed status with lower function scores, and retired status with lower satisfaction scores than among the employed). Female sex, black race, and higher BMI were significantly associated with both lower pain scores and function scores. All 6 of these factors were associated with lower total PSS. Greater age and workers’ compensation were associated with lower function score. Also, higher CCI and less education were associated with lower pain score and total PSS, and smoking was associated with lower pain score. Among disease-specific factors, adhesive capsulitis was significantly associated with lower function, satisfaction, and total scores; large/massive RC tear, with lower function and total scores; and prior surgery and abnormal acromion status, with lower satisfaction scores.
TABLE 3.
Estimated Effects and Odds Ratios of General Patient Factors and Disease-Specific Factors for Baseline Penn Shoulder Scores, 95% CIs, and P Values for Each Predictor in Patients Undergoing Rotator Cuff Repaira
| PSS Pain | PSS Function | PSS Satisfaction | Total PSS | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Level | Model | Estimated Effect | P | Estimated Effect | P | Odds Ratio | P | Estimated Effect | P | |
| General Patient Factors | ||||||||||
| Age | 0.28 (−0.18, 0.74) | .23 | −1.2 (−1.85, −0.20) | .02 | 1.06 (0.92, 1.23) | .40 | −0.62 (−1.84, 0.60) | .32 | ||
| Body mass index | −0.42 (−0.77, −0.06) | .02 | −1.02 (−1.66, −0.39) | .002 | 1.08 (0.96, 1.21) | .19 | −1.31 (−2.25, −0.38) | .006 | ||
| Charlson comorbidity index | −0.58 (−0.98, −0.17) | .005 | −0.62 (−1.35, 0.11) | .10 | 0.99 (0.87, 1.13) | .88 | −1.16 (−2.24, −0.08) | .03 | ||
| Education, y | 1.05 (0.61, 1.48) | <.001 | 0.53 (−0.25, 1.31) | .18 | 0.93 (0.81, 1.07) | .32 | 1.40 (0.25, 2.54) | .02 | ||
| VR-12 MCS | Full | 1.94 (1.49, 2.39) | <.001 | 3.65 (2.84, 4.46) | <.001 | 1.25 (1.08, 1.45) | .003 | 5.78 (4.58, 6.98) | <.001 | |
| Partial | 2.24 (1.79, 2.68) | <.001 | 4.34 (3.54, 5.15) | <.001 | 1.28 (1.11, 1.48) | .001 | 6.80 (5.61, 7.98) | <.001 | ||
| Sex | Female | — | — | — | — | |||||
| Male | 1.69 (1.06, 2.32) | <.001 | 2.41 (1.27, 3.55) | <.001 | 1.16 (0.95, 1.42) | .14 | 4.14 (2.47, 5.82) | <.001 | ||
| Raceb | White | — | — | — | — | |||||
| Black | −1.78 (−2.70, −0.87) | <.001 | −2.54 (−4.19, −0.90) | .002 | 0.68 (0.50, 0.93) | .02 | −4.49 (−6.92, −2.07) | <.001 | ||
| Other | −0.53 (−2.42, 1.36) | .59 | −3.32 (−6.72, 0.08) | .06 | 0.85 (0.46, 1.56) | .59 | −4.03 (−9.04, 0.99) | .12 | ||
| Smoking statusc | Never | — | — | — | — | |||||
| Quit | Full | −0.19 (−0.86, 0.48) | .57 | −0.03 (−1.23, 1.18) | .97 | 0.89 (0.72, 1.10) | .29 | −0.38 (−2.16, 1.40) | .67 | |
| Partial | −0.2 (−0.9, 0.49) | .56 | −0.13 (−1.4, 1.13) | .84 | 0.88 (0.72, 1.09) | .24 | −0.52 (−2.39, 1.35) | .59 | ||
| Current | Full | −1.41 (−2.33, −0.50) | .002 | −1.28 (−2.92, 0.36) | .13 | 0.81 (0.60, 1.08) | .16 | −2.84 (−5.26, −0.42) | .02 | |
| Partial | −2.24 (−3.16, −1.32) | <.001 | −3.24 (−4.92, −1.55) | <.001 | 0.76 (0.57, 1.01) | .06 | −5.68 (−8.17, −3.19) | <.001 | ||
| Preoperative opioid use | No | — | — | — | — | |||||
| Yes | Full | −1.26 (−1.88, −0.64) | <.001 | −3.66 (−4.78, −2.54) | <.001 | 0.76 (0.63, 0.93) | .007 | −5.29 (−6.94, −3.64) | <.001 | |
| Partial | −1.84 (−2.47, −1.21) | <.001 | −4.64 (−5.78, −3.5) | <.001 | 0.74 (0.61, 0.89) | .002 | −6.88 (−8.56, −5.19) | <.001 | ||
| Chronic pain | No | — | — | — | — | |||||
| Yes | Full | −0.05 (−0.69, 0.59) | .88 | −0.16 (−1.31, 0.99) | .79 | 0.97 (0.79, 1.18) | .74 | −0.30 (−2.00, 1.40) | .73 | |
| Partial | −0.45 (−1.11, 0.2) | .177 | −0.84 (−2.05, 0.36) | .168 | 0.96 (0.79, 1.18) | .723 | −1.37 (−3.15, 0.41) | .131 | ||
| Employment statusd | Employed | — | — | — | — | |||||
| Retired | Full | −0.57 (−1.49, 0.34) | .22 | −1.51 (−3.15, 0.14) | .07 | 0.72 (0.54, 0.96) | .02 | −2.44 (−4.87, −0.01) | .05 | |
| Partial | −0.77 (−1.72, 0.17) | .109 | −1.69 (−3.41, 0.03) | .054 | 0.71 (0.53, 0.94) | .018 | −2.84 (−5.39, −0.29) | .029 | ||
| Not employed | Full | −0.81 (−1.57, −0.05) | .04 | −2.06 (−3.43, −0.69) | .003 | 1.17 (0.92, 1.50) | .20 | −2.56 (−4.58, −0.54) | .01 | |
| Partial | −1.55 (−2.31, −0.79) | <.001 | −3.23 (−4.62, −1.84) | <.001 | 1.07 (0.84, 1.35) | .575 | −4.55 (−6.61, −2.49) | <.001 | ||
| Workers’ compensation | No | — | — | — | — | |||||
| Yes | Full | −0.24 (−1.39, 0.91) | .68 | −2.56 (−4.63, −0.49) | .02 | 0.87 (0.60, 1.26) | .46 | −2.99 (−6.04, 0.07) | .06 | |
| Partial | −0.12 (−1.3, 1.06) | .847 | −2.04 (−4.19, 0.12) | .064 | 0.86 (0.6, 1.24) | .417 | −2.36 (−5.55, 0.83) | .147 | ||
| Disease-Specific Factors | ||||||||||
| Prior surgery | No | — | — | — | — | |||||
| Yes | −0.05 (−1.42, 1.31) | .94 | −1.67 (−4.13, 0.78) | .18 | 0.63 (0.41, 0.97) | .04 | −2.39 (−6.02, 1.23) | .20 | ||
| Rotator cuff tear type | Partial | — | — | — | — | |||||
| Full | 0.26 (−0.53, 1.06) | .51 | 0.86 (−0.56, 2.28) | .23 | 1.02 (0.80, 1.31) | .88 | 1.20 (−0.90, 3.29) | .26 | ||
| Rotator cuff tear sizee | Small | — | — | — | — | |||||
| Medium | −0.19 (−1.08, 0.70) | .68 | −0.51 (−2.10, 1.09) | .54 | 0.85 (0.64, 1.12) | .24 | −0.93 (−3.29, 1.43) | .44 | ||
| Large/massive | −0.09 (−1.06, 0.88) | .85 | −2.76 (−4.51, −1.01) | .002 | 0.72 (0.53, 0.98) | .04 | −3.15 (−5.73, −0.56) | .02 | ||
| Surgery type | Primary | — | — | — | — | |||||
| Revision | −0.45 (−2.13, 1.23) | .60 | 0.71 (−2.31, 3.74) | .64 | 1.48 (0.87, 2.51) | .15 | 0.89 (−3.57, 5.35) | .70 | ||
| Subscapularis tendon | Normal | — | — | — | — | |||||
| Torn | 0.35 (−0.41, 1.11) | .37 | −0.31 (−1.68, 1.06) | .66 | 0.98 (0.77, 1.24) | .85 | −0.01 (−2.03, 2.02) | .99 | ||
| Biceps tendon tear typef | Normal | — | — | — | — | |||||
| Partial | −0.05 (−0.74, 0.63) | .88 | 0.02 (−1.21, 1.25) | .97 | 1.10 (0.88, 1.36) | .41 | −0.00 (−1.82, 1.82) | >.999 | ||
| Full | −0.72 (−1.75, 0.31) | .17 | −1.22 (−3.08, 0.63) | .20 | 0.98 (0.71, 1.35) | .89 | −2.09 (−4.82, 0.65) | .13 | ||
| Acromioclavicular joint | Normal | — | — | — | — | |||||
| Abnormal | −0.69 (−1.77, 0.38) | .21 | 1.15 (−0.79, 3.08) | .25 | 0.90 (0.64, 1.25) | .52 | 0.14 (−2.71, 2.99) | .92 | ||
| Glenoid cartilage | Normal/G1/G2 | — | — | — | — | |||||
| G3/G4 | −0.49 (−2.19, 1.20) | .57 | −1.22 (−4.27, 1.83) | .43 | 0.64 (0.37, 1.11) | .11 | −2.44 (−6.94, 2.06) | .29 | ||
| Humeral head cartilage | Normal/G1/G2 | — | — | — | — | |||||
| G3/G4 | 1.26 (−0.24, 2.75) | .10 | 2.34 (−0.35, 5.03) | .09 | 1.03 (0.64, 1.67) | .90 | 3.72 (−0.25, 7.68) | .07 | ||
| Acromion | Normal | — | — | — | — | |||||
| Abnormal | −0.23 (−0.89, 0.42) | .49 | −0.37 (−1.56, 0.81) | .54 | 0.76 (0.61, 0.93) | .009 | −0.88 (−2.63, 0.86) | .32 | ||
| Adhesive capsulitis | No | — | — | — | — | |||||
| Yes | −1.04 (−2.80, 0.72) | .25 | −5.09 (−8.26, −1.92) | .002 | 0.50 (0.28, 0.87) | .01 | −6.91 (−11.59, −2.24) | .004 | ||
| Labral tear | No | — | — | — | — | |||||
| Yes | −0.31 (−1.10, 0.48) | .45 | 0.68 (−0.74, 2.10) | .35 | 1.02 (0.80, 1.31) | .87 | 0.50 (−1.60, 2.60) | .64 | ||
The effects for numeric variables (age, body mass index, education, VR-12 MCS, and Charlson comorbidity index) compare the 75th vs 25th percentiles shown in Table 1. For VR-12 MCS, smoking status, opioid use, chronic pain, employment status, and workers’ compensation, the effect estimates and odds ratios are shown for their simultaneous adjustment (full model) compared with their individual effects after adjustment for all other variables not in this sublist (partial model). Values in parentheses are 95% Cis. G, grade; PSS, Penn Shoulder Score; VR-12 MCS, Veterans RAND 12-Item Health Survey mental component score.
Overall (omnibus) P values for differences among any of the 3 race categories were .001 for pain score, .003 for function score, .05 for satisfaction score, and .001 for total PSS.
Overall (omnibus) P values for differences among any of the 3 smoking categories were .0096 and <.001 in the full and partially adjusted models for pain score, .285 and <.001 in the corresponding models for function score, .296 and .137 in the models for satisfaction score, and .069 and <.001 in the models for total PSS.
Full-time, part-time, and self-employed patients were grouped into a single category for statistical analysis. Overall (omnibus) P values for differences among any of the remaining 3 employment categories were .099 and <.001 in the full and partially adjusted models for pain score, .009 and <.001 in the corresponding models for function score, .007 and .021 in the models for satisfaction score, and .023 and <.001 in the models for total PSS.
Overall (omnibus) P values for differences among any of the 3 rotator cuff tear size categories were .899 for pain score, <.001 for function score, .098 for satisfaction score, and .021 for total PSS.
Overall (omnibus) P values for differences among any of the 3 biceps tendon tear type categories were .369 for pain score, .384 for function score, .641 for satisfaction score, and .285 for total PSS.
Examples of interpretation of total PSS and pain and function subscale scores (standard linear regression model):
• Preoperative opioid users have total PSS and pain and function subscale scores that are 5.29, 1.26, and 3.66 points lower on average, respectively, than patients who do not use opioids, after controlling for all other variables.
• A patient with VR-12 MCS of 60.5 (75th percentile) has a total PSS 5.78 points higher on average than a patient with VR-12 MCS of 43.1 (25th percentile), after controlling for all other variables.
Examples of interpretation of PSS satisfaction subscale score (proportional odds regression model):
• The odds that a preoperative opioid user has a PSS satisfaction score of at least x (eg, 5) are (1 – 0.76) × 100 = 24% lower than the odds that a non–opioid user has a PSS satisfaction score of at least 5, after adjustment for all other variables (this interpretation holds regardless of the number we put in for x: hence, proportional odds).
• The odds that a patient with VR-12 MCS of 60.5 (75th percentile) has a PSS satisfaction score of at least x are (1.25 – 1.00) × 100 = 25% higher than the odds of a patient with VR-12 MCS of 43.1 (25th percentile), after controlling for all other variables.
Figure 2.
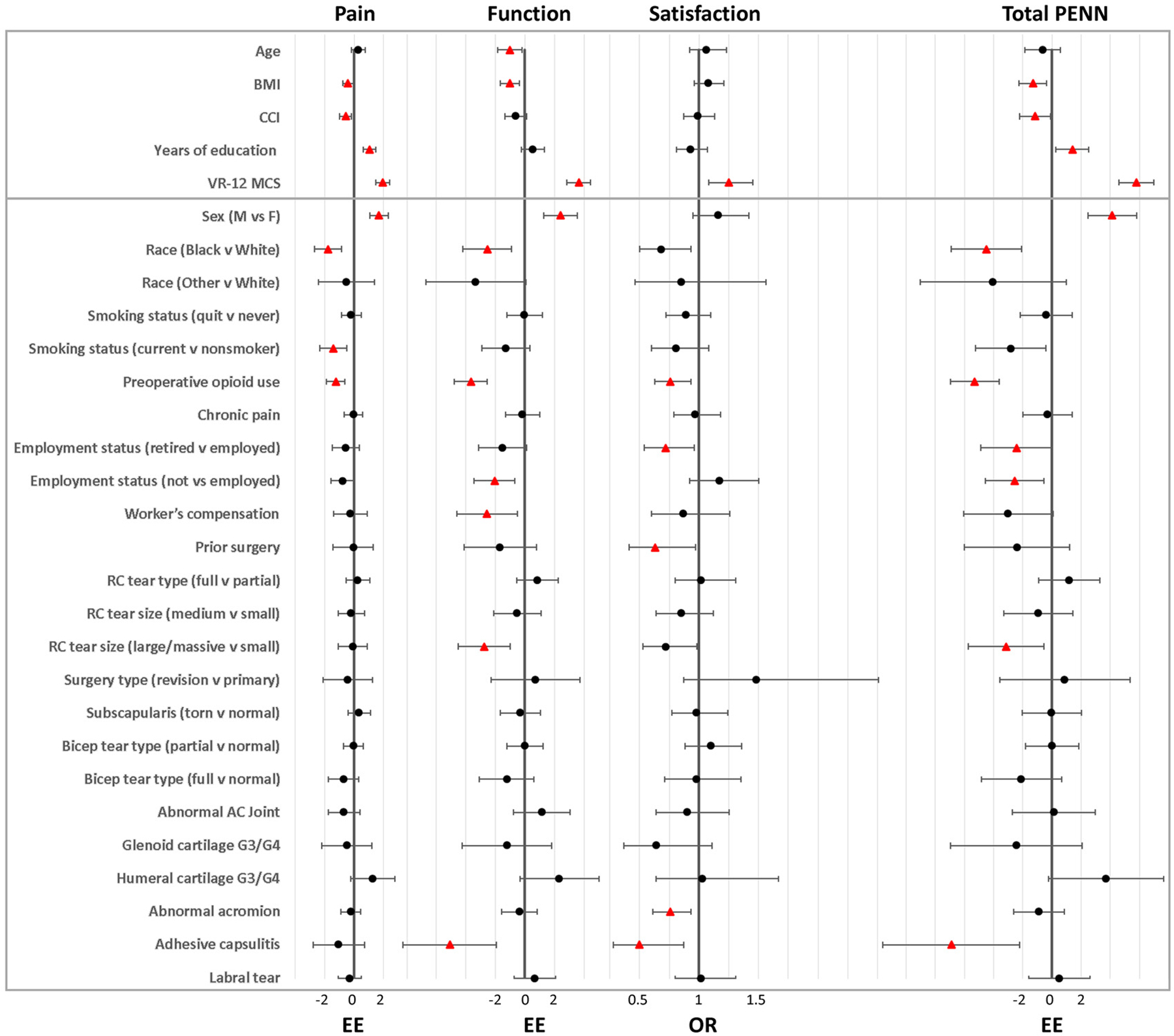
Forest plot showing the estimated regression coefficients for pain and function subscale scores and total Penn Shoulder Score and the odds ratios (ORs) for satisfaction subscale score, each with 95% CIs, for predictors in the full models of patients undergoing rotator cuff (RC) repair. The effects for numeric variables (age, BMI, education, VR-12 MCS, and CCI) compare the 75th vs 25th percentiles shown in Table 1. Predictors having statistically significant associations, both in omnibus tests and pairwise comparisons for trichotomous variables, with baseline PENN scores are marked as triangles and nonsignificant associations are marked as circles. AC, acromioclavicular; BMI, body mass index; CCI, Charlson comorbidity index; EE, estimated effect; F, female; G, grade; M, male; PENN, Penn Shoulder Score; VR-12 MCS, Veterans RAND 12-Item Health Survey mental component score.
Regarding sensitivity analyses, results of the Bonferroni-Holm multiple comparison adjustments are shown in Appendix Figure A1 (available in the online version of this article). Statistical significance (α = .05) was preserved for 36 of 44 (82%) significant results and, for at least 1 of the 4 scores, for 12 of 15 (80%) significant predictors in the original analysis, the exceptions being age, prior surgery, and workers’ compensation, each initially associated with a single subscale score. All interaction screening strategies identified the same 2 statistically significant interactions of VR-12 MCS with smoking status for function scores and with acromion status for satisfaction scores, both with .05 < P > .025. These 2 interactions, neither highly significant, compare with 4 false-positive interactions expected by chance among the 80 interactions tested, thus supporting adequacy of the additive regression models. Finally, after removal of possible causal mediators from the full model, the partial models showed that the significant associations of VR-12 MCS with PSS subscale scores and total PSS were essentially unchanged or slightly increased, and the associations of preoperative opioid use, not employed status, and smoking with pain and function scores and total PSS were increased (the association of smoking with function score was rendered significant). The association of workers’ compensation with function score decreased and lost statistical significance, whereas chronic pain remained not significant in both full and partial models.
Relative Importance of Predictors in Influencing Baseline Penn Shoulder Scores
Figure 3 compares the Akaike information criterion increases that resulted from removal of each variable from the full model as a gauge of relative importance of their contributions. In full linear models for total PSS and the pain and function scores, the top 5 variables by this measure accounted for 72.0% to 82.4% of the total variance explained by the 24 predictors, and the most important factor for total PSS and all subscale scores was VR-12 MCS, with lower values associated with poorer scores. Preoperative opioid use was also among the 5 top variables for PSS total and each subscale score, in each case associated with poorer scores, as were female sex and black race except for the satisfaction score. Other variables ranked among the top 5 were education for pain; tear size for function; employment, acromion, and adhesive capsulitis status for satisfaction; and adhesive capsulitis for total PSS.
Figure 3.
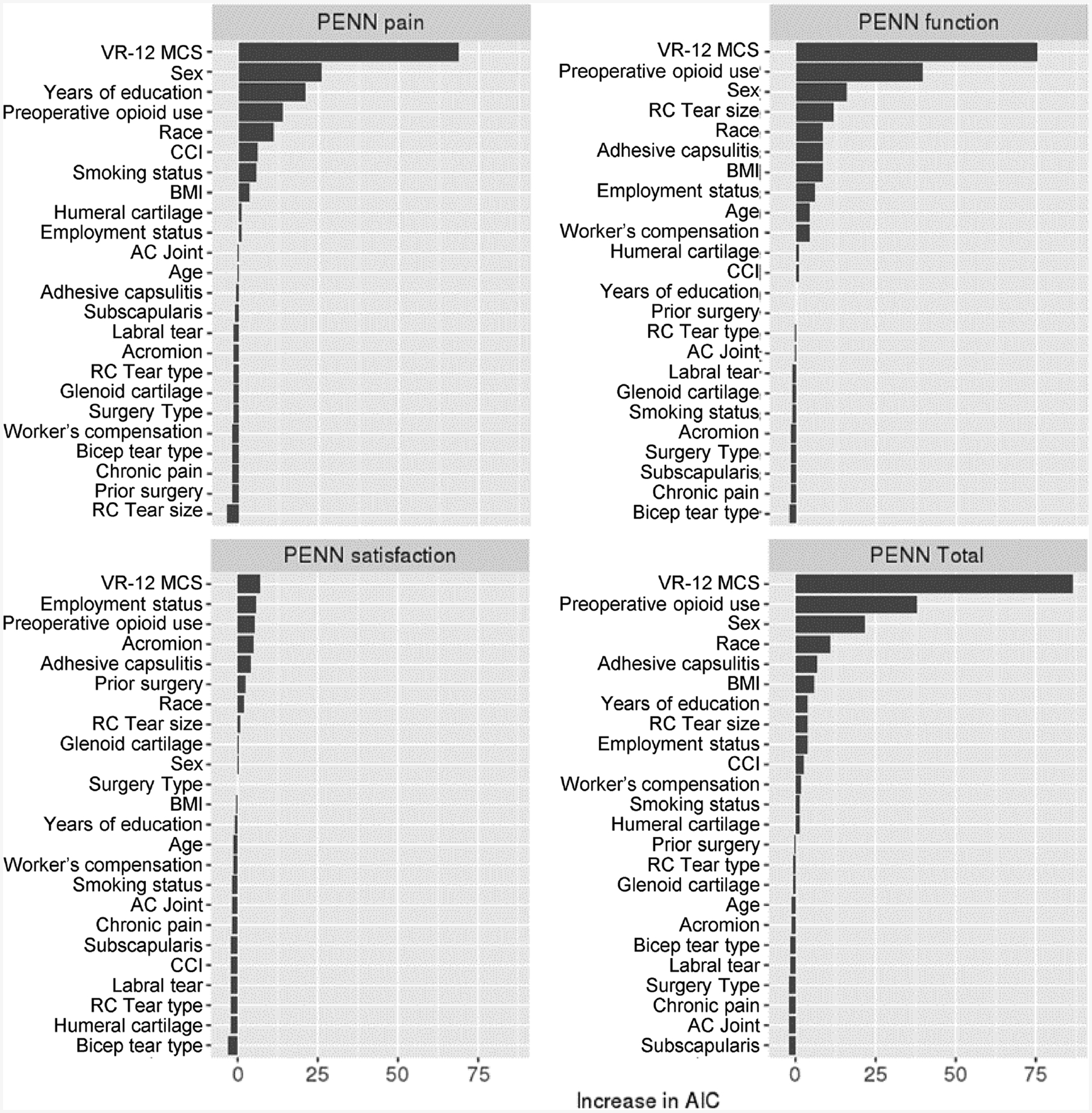
Relative variable importance of general patient and disease-specific factors on baseline Penn Shoulder Score, based on the increase in AIC upon removal from the full model. The most influential variables are listed on the top of the respective charts. AC, acromioclavicular; AIC, Akaike information criterion; BMI, body mass index; CCI, Charlson comorbidity index; PENN, Penn Shoulder Score; RC, rotator cuff; VR-12 MCS, Veterans RAND 12-Item Health Survey mental component score.
DISCUSSION
The purpose of this study was to investigate the extent to which general patient factors and disease-specific factors are associated with baseline PROMs in patients undergoing RCR. We hypothesized that both larger tear size and worse mental health status as assessed by VR-12 MCS would be associated with worse baseline total PSS and its pain, function, and satisfaction subscale scores. Using prospectively collected data on 24 potential general patient and disease-specific correlates of baseline symptoms, we performed multivariable analysis of 1442 patients undergoing RCR. As hypothesized, large/massive tear size was shown to be significantly associated with lower PSS (total score and function score but not pain or satisfaction scores), and lower VR-12 MCS was significantly associated with lower PSS (total score and all 3 subscale scores). Moreover, there was no compelling evidence that these relationships were modified by other factors studied.
The association between tear size or other measures of tear severity and shoulder PROMs is poorly understood. Our study showed that tear size was significantly and predominantly associated with PSS function subscale scores; patients with large/massive tears had PSS function scores that were 2.76 points lower on average than patients with small tears, after we controlled for all other variables. Our results are in agreement with several previous studies that have shown baseline shoulder pain to be largely associated with patient mental health status, sex, educational level, and race but not with tear size and thickness.6,9,11,18,36 Reports on associations between tear size and shoulder function have been conflicting; our study and another report found an association,36 whereas several other studies did not.6,9,11,18 The contradictory results from these previous studies may be due to a combination of narrower patient selection criteria (eg, inclusion of only patients with atraumatic full-thickness tears that were managed nonoperatively by physical therapy, or age >45 years), smaller cohort sizes, and limited number of variables collected and included in multivariable analyses to control for confounding. Our analysis showed that larger tear size was among the most prominent factors associated with lower shoulder function, along with lower mental health status, preoperative opioid use, female sex, and black race.
We found mental health status as measured by VR-12 MCS to be the most prominent factor associated with total PSS and all subscale scores in full models. Our study showed that compared with a patient with VR-12 MCS of 43.1 (25th percentile), a patient with VR-12 MCS of 60.5 (75th percentile) had a 1.94-point higher PSS pain score, 3.65-point higher PSS function score, and 5.78-point higher total PSS, as well as a 25% higher odds of achieving a certain PSS satisfaction score, after we controlled for all other variables. This is in agreement with several previous studies that have shown baseline mental health status to be closely associated with shoulder pain and disability at baseline,1–3,6,21,35,36 as well as with outcomes after repair10,23,30,34 in patients with RC tears. Although this finding is consistent, the reason that lower mental health status accompanies poorer total PSS and subscale scores remains unclear. Preexisting mental health issues may increase rumination or otherwise alter how patients perceive their shoulder pain and function, thereby reducing satisfaction. Alternatively, physical and functional limitations resulting from the torn RC may adversely affect work performance, social activities, and mood as reported on the VR-12,15,27 which asks about these items in the 4 weeks before testing (Appendix Table A1, available online) but does not address the primary cause, chronicity, or possible situational context of responses. The associations of VR-12 MCS with PSS total and subscale scores were essentially unaffected by adjustment for several variables that might in principle either confound or mediate a causal pathway in one direction or the other. The stability of these statistical associations was consistent with a causal relationship but, in such cross-sectional preoperative data, did not imply its direction.
However, although the relationship between mental health status and shoulder pain and function is likely complex,1 and causal relationships cannot be inferred from this cross-sectional study using self-rated subjective PROM tools,3 strong correlation of postrepair VR-12 MCS and PSS improvements would suggest that VR-12 MCS is more likely dependent on the preoperative RC tear disability than indicative of a true mental health condition. Indeed, in a small study of 47 patients, RCR was associated with improvements in mental status, and a poor preoperative mental status did not predict poor repair outcomes.4 Additional longitudinal studies with more rigorous psychological evaluations may be needed to fully understand these relationships.
Although we hypothesized that tear size and mental health status would be the 2 primary factors associated with baseline shoulder PROMs, 15 of the 24 variables we investigated were statistically significantly associated with 1 or more PSS results. We found that 12 (80%) of these variables and more than three-quarters of all statistically significant PSS results persisted after Bonferroni-Holm adjustment for simultaneous tests of the PSS total score and 3 subscale scores. These included factors such as sex, race, preoperative opioid use, years of education, employment status, acromion status, and adhesive capsulitis. Preoperative opioid use (5.29 points lower total PSS compared with nonusers), female sex (4.14 points lower total PSS compared with males), and black race (4.5 points lower total PSS compared with white race) were the factors that most influenced baseline PROMs.
The finding that general patient factors were substantially associated with baseline shoulder PROMs is consistent with results from previous studies, which have shown that older age, higher BMI, more comorbidities, lower level of education, lower mental health status, female sex, black/minority race, and smoking were significantly and negatively associated with baseline PROMs.6,9,11,18,36 In our data, employment status, receipt of workers’ compensation, and preoperative opioid use were also associated with lower baseline PROMs in patients undergoing RCR. In particular, preoperative use of opioids, which were prescribed to 45% of patients during the 3 months before surgery, similar to the 43% rate in the United States,32 was significantly associated with total PSS and all 3 subscale scores. Preoperative opioid use has been shown to be significantly associated with higher rates of certain comorbidities (including depression and chronic pain conditions), inferior postoperative outcomes, and continued postoperative opioid consumption after RCR.25,28,32,33 Taken together, these findings suggest that a patient’s preoperative opioid use may need to be considered when setting expectations with regard to RCR outcomes.
The present study has several strengths. The data were derived from a large prospective cohort (1442 patients) that captures a wide range of patient and surgical factors relevant to RCR surgery. The enrollment rate was nearly 100%, thereby avoiding patient selection bias in evaluating these factors in a cohort of patients undergoing RCR. Factors either cited or judged to influence baseline symptoms were prospectively chosen and used in multivariable models to identify statistically significant associations. This is the first study to our knowledge that identified correlates of baseline symptoms in a population of patients with RC injury while comprehensively controlling for patient and surgical factors. Furthermore, we used the PSS, which is unique among the various shoulder-specific PROMs as it measures patient satisfaction related to the shoulder on a 10-point scale, in addition to measuring shoulder pain and function.
This study is not without limitations. First, our database does not include all possible factors that might influence baseline symptoms, and some potentially important factors, such as hand dominance,3,16 tendon retraction,36 muscle fatty infiltration and atrophy,34,35 and socioeconomic status,8 were not investigated. The database was prospectively designed by specialty-specific orthopaedic surgeons at our institution to collect sociodemographic factors, joint-specific variables of disease severity and treatment, and joint-specific validated PROMs at baseline and 1 year after treatment for more than 30 elective orthopaedic procedures. The number of questions asked and the number of factors collected were carefully selected so as not to overburden the patient or the surgeon. Second, we limited our investigation to patients with RC tears undergoing surgical repair, and our study was performed in a single tertiary hospital network. Hence, our findings may not be generalizable to patients with RC tears not requiring repair or with irreparable tears, other patient populations, or surgical practice settings. Third, while we identified clinically relevant factors that were significantly associated with baseline symptoms, our cross-sectional analyses could not be used to adequately evaluate the causality or clinical significance of associations. In particular, we did not use more discriminating outcome tools to determine the cause of lower mental health status in this study, such as whether this was due to a mental health diagnosis or whether this was secondary to the disability caused by the RC tear, or some combination of both.
Our future work will investigate which patient demographic, disease, and treatment factors predict poor postoperative PROMs after RCR and, in particular, whether the predictors associated with poor baseline pain, function, and satisfaction before surgery identified in the current study will also be associated with poor postoperative PROMs.
ACKNOWLEDGMENT
The authors acknowledge the Orthopaedic and Rheumatologic Institute at Cleveland Clinic for support of the OME database and related infrastructure. The authors also thank Brittany Stojsavljevic, editor assistant, Cleveland Clinic, for editorial management.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes of Health (NIH) under award 5R01AR068342. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. S.S. has received research funding from NIH; holds personal stock in Becton Dickinson & Co, Johnson & Johnson, and Medtronic; and has received royalties from Viscus Biologics LLC. E.T.R. currently receives royalties and honoraria and/or consulting fees from DJO Surgical; has received honoraria, consulting income, research funding, and hospitality payments from DePuy Synthes; has received consulting fees from Encore Medical; and has received compensation for services other than consulting from Tornier. P.J.E. has received consulting fees from Axogen, Zimmer Biomet, Acumed, Extremity, Biomet Orthopedics, and Small Bone Innovations; royalties or license payments from Zimmer Biomet and Biomet Orthopedics; education payments from Arthrex; and hospitality payments from Exatech, Synthes GMBH, and Arthrosurface. L.D.F. has received consulting fees from Zimmer Biomet and hospitality payments from the Musculoskeletal Transplant Foundation. B.W.M. has received hospitality payments from Arthrex, Zimmer Biomet, and Ramsay Medical and education payments from Arthrex. A.A.M. has received royalties from Arthrosurface and Zimmer Biomet; is on the board of and holds stock in Arthrosurface and Trice; has received consulting fees from Arthrosuface, Amniox, Linvatec Corp, Stryker, and Trice; and has received hospitality payments from Arthrex, Rock Medical, DJO, and Smith & Nephew. V.J.S. has received research support from Arthrex, Orthofix, and Wright Medical Technology; consulting fees from Arthrex and CDC Medical; hospitality payments from Pacira Pharmaceuticals Inc, Zimmer Biomet, Encore Medical, Tornier, Stryker, and Depuy; honoraria from Encore Medical; and compensation for services other than consulting from Exactech. M.S.S. has received compensation for services other than consulting, hospitality payments, and consulting fees from Arthrex. W.H.S. has received consulting fees from Zimmer Biomet, Materialise USA, and Stryker. K.P.S. has received funding for research from NIH/NIAMS grant R01 AR053684, Smith & Nephew Endoscopy, and DonJoy Orthopaedics; consulting fees from the National Football League, Cytori, Mitek, Samumed, and Flexion Therapeutics; hospitality payments from DePuy and Biosense Webster; and commercial product nPhase royalties from Flexion Therapeutics. K.L.S. has received hospitality payments from Stryker, Horizon Pharma, Musculoskeletal Transplant Foundation, Biomet Orthopedics, Ramsay Medical, and Fidia Pharmacy; consulting fees from Molnlycke Health Care; and education payments from Arthrex and Biomet Orthopedics. V.E. has received consulting fees from DJ Orthopaedics; research support from OREF; and hospitality payments from Encore Medical, Integra Lifesciences Corporation, and Wright Medical Technology. J.P.I. has received royalties and consulting fees from Depuy, Encore Medical, Wright Medical, Arthrex, and Tornier; consulting fees from DJO; and compensation for services other than consulting from Zimmer Biomet. K.A.D. has received research funding from NIH and consulting fees from Orthofix. G.S. has received commercial product nPhase royalties. M.H.J. is on the Scientific Advisory Board for Samumed and receives salary support for research from NIH. P.B.I. has received consulting fees from GE Healthcare and Colgate-Palmolive. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Appendix Table A1. Questionnaire used to assess VR-12 MCS score (adapted from Kazis et al)15
Instructions: This questionnaire asks for your views about your health. This information will help keep track of how you feel and how well you are able to do your usual activities.
Answer every question by marking the answer as indicated. If you are unsure how to answer a question, please give the best answer you can.
4. During the past 4 weeks, have you had any of the following problems with your work or other regular daily activities as a result of any emotional problems (such as feeling depressed or anxious)?
| a. Accomplished less than you would like. | 1 | 2 | 3 | 4 | 5 |
| b. Didn’t do work or other activities as carefully as usual. | 1 | 2 | 3 | 4 | 5 |
These questions are about how you feel and how things have been with you during the past 4 weeks. For each question, please give the one answer that comes closest to the way you have been feeling.
6. How much of the time during the past 4 weeks:
| ALL OF THE TIME | MOST OF THE TIME | A GOOD BIT OF THE TIME | SOME OF THE TIME | A LITTLE OF THE TIME | NONE OF THE TIME | |
|---|---|---|---|---|---|---|
| a. Have you felt calm and peaceful? | 1 | 2 | 3 | 4 | 5 | 6 |
| b. Did you have a lot of energy? | 1 | 2 | 3 | 4 | 5 | 6 |
| c. Have you felt downhearted and blue? | 1 | 2 | 3 | 4 | 5 | 6 |
7. During the past 4 weeks, how much of the time has your physical health or emotional problems interfered with your social activities (like visiting with friends, relatives, etc.)?
| 1 | 2 | 3 | 4 | 5 |
Score calculation: Responses to each item are used to create a raw MCS summary score which is then standardized using a tscore transformation and normed to a general US population (based on a 1990 norm)/2000–2002 US Medical Expenditure Panel Survey population of a score of 50 and a standard deviation of 10. The scoring algorithm can impute missing responses using a modified regression estimate, and is able to compute MCS with as few as three available responses
Appendix Figure A1.
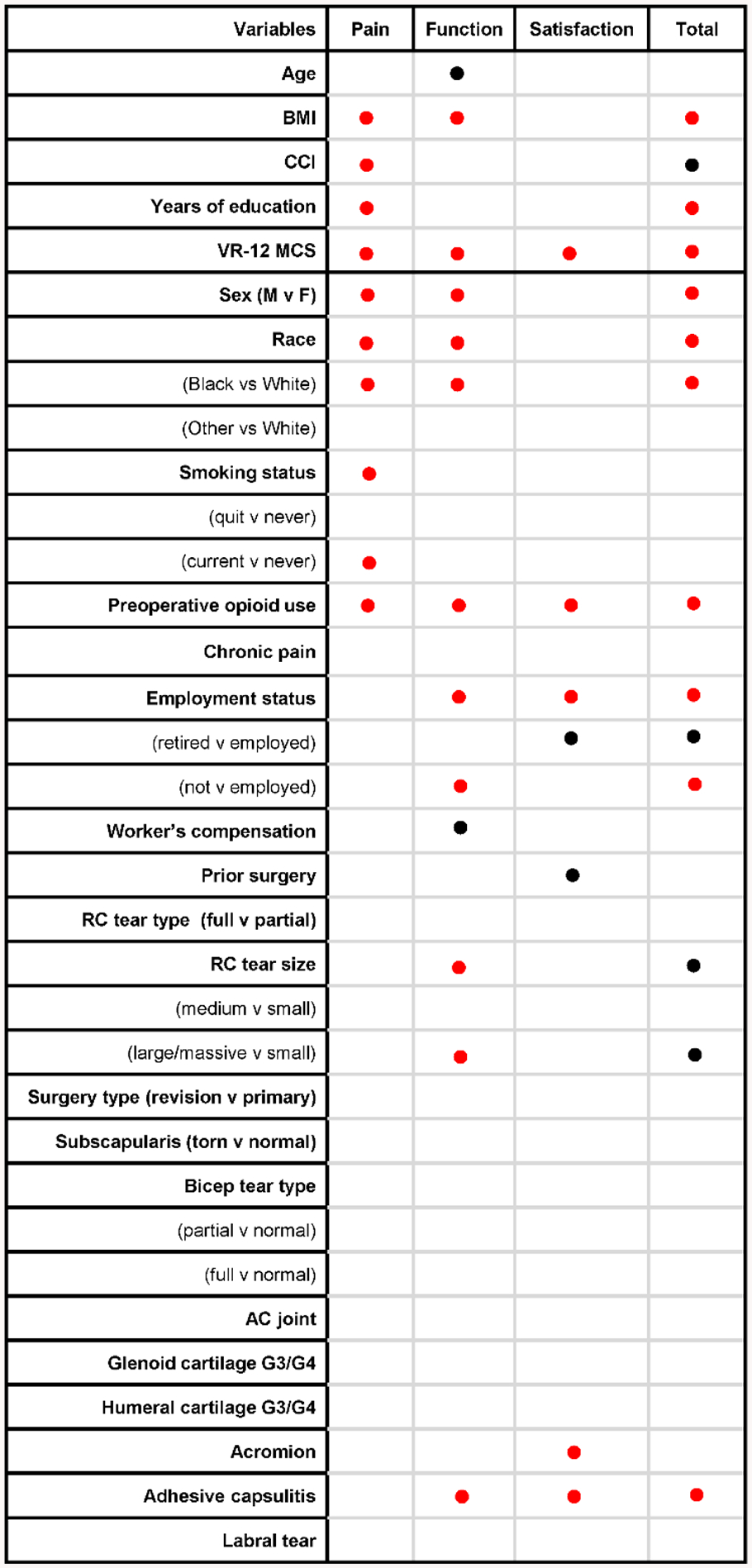
Sensitivity analysis showing statistical significance (α=0.05) of relationships of putative factors to baseline PSS total score and subscores, with and without Bonferroni-Holm adjustment for simultaneous testing of the four scores. Red dots represent significant relationship after adjustment, and black dots represent significant relationships before but not after adjustment. Statistical significance was preserved for 36/44 (82%) of significant results after adjustment.
REFERENCES
- 1.Barlow JD, Bishop JY, Dunn WR, Kuhn JE, Group MS. What factors are predictors of emotional health in patients with full-thickness rotator cuff tears? J Shoulder Elbow Surg. 2016;25(11):1769–1773. [DOI] [PubMed] [Google Scholar]
- 2.Cho CH, Jung SW, Park JY, Song KS, Yu KI. Is shoulder pain for three months or longer correlated with depression, anxiety, and sleep disturbance? J Shoulder Elbow Surg. 2013;22(2):222–228. [DOI] [PubMed] [Google Scholar]
- 3.Cho CH, Seo HJ, Bae KC, Lee KJ, Hwang I, Warner JJ. The impact of depression and anxiety on self-assessed pain, disability, and quality of life in patients scheduled for rotator cuff repair. J Shoulder Elbow Surg. 2013;22(9):1160–1166. [DOI] [PubMed] [Google Scholar]
- 4.Cho CH, Song KS, Hwang I, Warner JJ. Does rotator cuff repair improve psychologic status and quality of life in patients with rotator cuff tear? Clin Orthop Relat Res. 2015;473(11):3494–3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cleveland O, Piuzzi NS, Strnad G, et al. Implementing a scientifically valid, cost-effective, and scalable data collection system at point of care: the Cleveland Clinic OME cohort. J Bone Joint Surg Am. 2019;101(5):458–464. [DOI] [PubMed] [Google Scholar]
- 6.Curry EJ, Matzkin EE, Dong Y, Higgins LD, Katz JN, Jain NB. Structural characteristics are not associated with pain and function in rotator cuff tears: the ROW cohort study. Orthop J Sports Med. 2015;3(5):2325967115584596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Derwin KA, Sahoo S, Zajichek A, et al. Tear characteristics and surgeon influence repair technique and suture anchor use in repair of superior-posterior rotator cuff tendon tears. J Shoulder Elbow Surg. 2019;28(2):227–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dorner TE, Muckenhuber J, Stronegger WJ, Ràsky É, Gustorff B, Freidl W. The impact of socio-economic status on pain and the perception of disability due to pain. Eur J Pain. 2011;15(1):103–109. [DOI] [PubMed] [Google Scholar]
- 9.Dunn WR, Kuhn JE, Sanders R, et al. Symptoms of pain do not correlate with rotator cuff tear severity: a cross-sectional study of 393 patients with a symptomatic atraumatic full-thickness rotator cuff tear. J Bone Joint Surg Am. 2014;96(10):793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gil JA, Goodman AD, Mulcahey MK. Psychological factors affecting outcomes after elective shoulder surgery. J Am Acad Orthop Surg. 2018;26(5):e98–e104. [DOI] [PubMed] [Google Scholar]
- 11.Harris JD, Pedroza A, Jones GL, Group MS. Predictors of pain and function in patients with symptomatic, atraumatic full-thickness rotator cuff tears: a time-zero analysis of a prospective patient cohort enrolled in a structured physical therapy program. Am J Sports Med. 2012;40(2):359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hawkins RJ, Thigpen CA. Selection, implementation, and interpretation of patient-centered shoulder and elbow outcomes. J Shoulder Elbow Surg. 2018;27(2):357–362. [DOI] [PubMed] [Google Scholar]
- 14.James G, Witten D, Hastie T, Tibshirani RJ. Linear model selection and regularization In: Casella G, Fienberg S, Olkin I, eds. An Introduction to Statistical Learning. New York: Springer; 2013:203–264. [Google Scholar]
- 15.Kazis LE, Selim A, Rogers W, Ren XS, Lee A, Miller DR. Dissemination of methods and results from the Veterans Health Study: final comments and implications for future monitoring strategies within and outside the Veterans healthcare system. J Ambul Care Manage. 2006;29(4):310–319. [DOI] [PubMed] [Google Scholar]
- 16.Keener JD, Steger-May K, Stobbs G, Yamaguchi K. Asymptomatic rotator cuff tears: patient demographics and baseline shoulder function. J Shoulder Elbow Surg. 2010;19(8):1191–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR Jr. The Penn shoulder score: reliability and validity. J Orthop Sports Phys Ther. 2006;36(3):138–151. [DOI] [PubMed] [Google Scholar]
- 18.Maher A, Leigh W, Brick M, et al. Gender, ethnicity and smoking affect pain and function in patients with rotator cuff tears. ANZ J Surg. 2017;87(9):704–708. [DOI] [PubMed] [Google Scholar]
- 19.Mall NA, Kim HM, Keener JD, et al. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010;92(16):2623–2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752–757. [DOI] [PubMed] [Google Scholar]
- 21.Potter MQ, Wylie JD, Greis PE, Burks RT, Tashjian RZ. Psychological distress negatively affects self-assessment of shoulder function in patients with rotator cuff tears. Clin Orthop Relat Res. 2014;472(12): 3926–3932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. [DOI] [PubMed] [Google Scholar]
- 23.Ravindra A, Barlow JD, Jones GL, Bishop JY. A prospective evaluation of predictors of pain after arthroscopic rotator cuff repair: psychosocial factors have a stronger association than structural factors. J Shoulder Elbow Surg. 2018;27(10):1824–1829. [DOI] [PubMed] [Google Scholar]
- 24.Reilly P, Macleod I, Macfarlane R, Windley J, Emery RJ. Dead men and radiologists don’t lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl. 2006;88(2): 116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sabesan VJ, Petersen-Fitts GR, Sweet MC, Katz DL, Lima DJ, Whaley JD. The impact of preoperative opioid use on outcomes after arthroscopic rotator cuff repair. JSES Open Access. 2018;2(3):155–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sahoo S, Mohr J, Strnad G, et al. Validity and efficiency of a smartphone-based electronic data collection tool for operative data in rotator cuff repair. J Shoulder Elbow Surg. 2019;28(7):1249–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schalet BD, Rothrock NE, Hays RD, et al. Linking physical and mental health summary scores from the Veterans RAND 12-Item Health Survey (VR-12) to the PROMIS((R)) Global Health Scale. J Gen Intern Med. 2015;30(10):1524–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Syed UAM, Aleem AW, Wowkanech C, et al. Neer Award 2018: the effect of preoperative education on opioid consumption in patients undergoing arthroscopic rotator cuff repair: a prospective, randomized clinical trial. J Shoulder Elbow Surg. 2018;27(6):962–967. [DOI] [PubMed] [Google Scholar]
- 29.Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604. [DOI] [PubMed] [Google Scholar]
- 30.Thorpe AM, O’Sullivan PB, Mitchell T, et al. Are psychologic factors associated with shoulder scores after rotator cuff surgery? Clin Orthop Relat Res. 2018;476(10):2062–2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Buuren S, Groothuis-Oudshoorn K. MICE: multivariate imputation by chained equations in R. J Stat Soft. 2011;45(3):1–67. [Google Scholar]
- 32.Westermann RW, Anthony CA, Bedard N, et al. Opioid consumption after rotator cuff repair. Arthroscopy. 2017;33(8):1467–1472. [DOI] [PubMed] [Google Scholar]
- 33.Williams BT, Redlich NJ, Mickschl DJ, Grindel SI. Influence of preoperative opioid use on postoperative outcomes and opioid use after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28(3): 453–460. [DOI] [PubMed] [Google Scholar]
- 34.Wylie JD, Baran S, Granger EK, Tashjian RZ. A comprehensive evaluation of factors affecting healing, range of motion, strength, and patient-reported outcomes after arthroscopic rotator cuff repair. Orthop J Sports Med. 2018;6(1):2325967117750104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wylie JD, Bershadsky B, Iannotti JP. The effect of medical comorbidity on self-reported shoulder-specific health related quality of life in patients with shoulder disease. J Shoulder Elbow Surg. 2010;19(6): 823–828. [DOI] [PubMed] [Google Scholar]
- 36.Wylie JD, Suter T, Potter MQ, Granger EK, Tashjian RZ. Mental health has a stronger association with patient-reported shoulder pain and function than tear size in patients with full-thickness rotator cuff tears. J Bone Joint Surg Am. 2016;98(4):251–256. [DOI] [PubMed] [Google Scholar]
- 37.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease: a comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699–1704. [DOI] [PubMed] [Google Scholar]


