Figure 1.
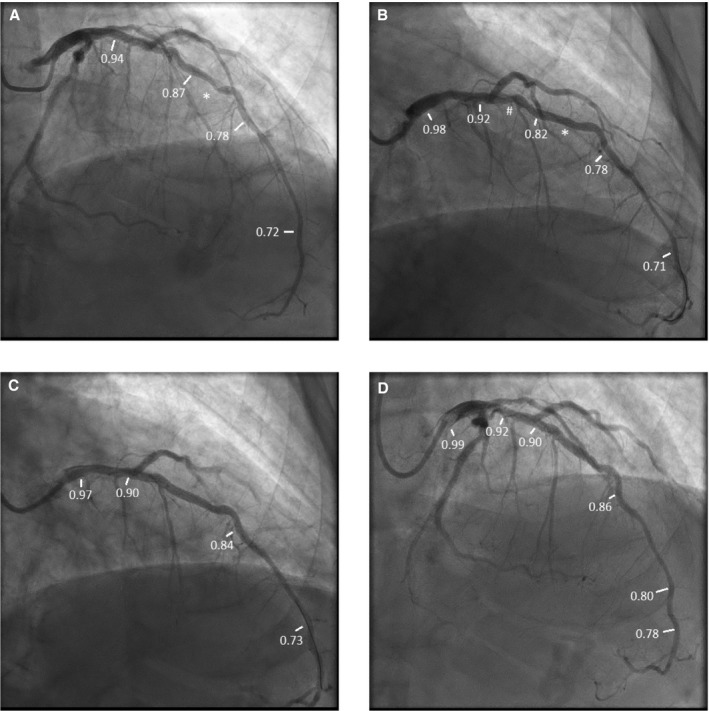
Patient example of the functionally optimized coronary intervention strategy. A, Angiogram before percutaneous coronary intervention (PCI). Fractional flow reserve (FFR) in the distal vessel was 0.72. On pullback, FFR distal to lesion (*) was 0.78, with step up to 0.87 across the lesion, then gradually to 0.94 in the proximal left anterior descending artery (LAD). B, Post‐PCI angiogram. FFR in the distal vessel after stent deployment across the lesion, denoted by (*). FFR in the distal vessel was 0.71. On pullback, FFR distal to stent was 0.78, proximal to stent was 0.82 (TSG 0.04) with step‐up across a less apparent lesion (#) to 0.92, then gradually to 0.98 in proximal LAD. C, Angiogram after stenting, less apparent lesion denoted by (#) and dilatation with noncompliant balloon of first stent (*). FFR after these interventions in the distal vessel was 0.73. On pullback, FFR distal to distal stent was 0.84, proximal to proximal stent 0.90 (TSG: 0.06), and then gradually rose to 0.97 in the proximal LAD. D, Intravascular ultrasound showed the distal stent was adequately expanded (90% of the target minimal luminal area [MLA]) but the proximal stent was underexpanded (74% of target MLA). Postdilation with a noncompliant balloon increased stent MLA to 86% of predicted stent area. FFR distally after postdilation was 0.78. On pullback, FFR in the distal vessel was 0.80, distal to distal stent was 0.86, proximal to proximal stent was 0.90 with a TSG of 0.04, and FFR was0.92 in the proximal LAD and 0.99 in the left main and guide. Thus, final drift was 0.01.
