Abstract
Purpose
The objective of this study was to estimate the prevalence of intimate partner violence (IPV) in an emergency department (ED) by sexual orientation and gender identification.
Methods
We conducted a cross-sectional survey of adult patients (n=1,136) presenting to a Level I Trauma Center ED from November 2015-November 2016. Multivariable logistic regression analysis was used to estimate the adjusted odds (aOR) of reporting any IPV or IPV subtypes (physical or sexual IPV or battering) by sexual orientation and gender identification, controlling for confounders.
Results
Overall, 11.6% (132/1136) of those surveyed were IPV positive. The prevalence of IPV was significantly higher in LGBTQ patients than in heterosexuals (18.3% vs 10.8%, p=0.0151); prevalence was highest among bisexuals (21.6%) and gay men (18.5%). IPV prevalence did not differ significantly in females versus males (13.5% vs 9.2%, p=0.0872). After controlling for age, the odds of reporting any IPV was highest among females (aOR=1.67 [1.10–2.53]); no significant differences were found by sexual orientation. Gay patients (aOR=5.50 [1.60–18.94]) and females (aOR=2.70 [1.46–9.99]) had significantly higher odds of reporting physical or sexual IPV than heterosexuals and males, respectively.
Conclusions
The study is among the first to report IPV prevalence by sexual orientation in an ED patient population. The reported IPV was higher among LGBTQ patients than heterosexual patients although this relationship diminished when controlling for covariates. These data begin to define the scope of IPV among LGBTQ ED patients and may be used to inform brief interventions to reduce the IPV-related morbidity experienced by ED patients.
INTRODUCTION
Intimate partner violence (IPV), defined as “physical violence, sexual violence, stalking and psychological aggression (including coercive tactics) by a current or former intimate partner (i.e., spouse, boyfriend/girlfriend, dating partner, or ongoing sexual partner)” (M. Breiding, Basile, Smith, Black, & Mahendra, 2015) poses a considerable health burden to men and women alike. Physical or sexual IPV in the United States affects an estimated three in ten women and one in ten men in their lifetime, with psychological aggression present in almost half of intimate relationships (Black et al., 2011). Reports of IPV among lesbians, gays and bisexuals exceed those of heterosexual populations: 44% of lesbian and 61% of bisexual women, and 26% of gay and 37% of bisexual men have reported rape, physical violence and/or stalking IPV in their lifetime compared to 35% and 29% of heterosexual women and men, respectively (Black et al., 2011).
Further examination of the high prevalence of IPV in the lesbian, gay, bisexual, transgender and questioning (LGBTQ) relationships can contribute to our understanding of IPV as a whole. Much of the work in IPV has focused on individual-level gender-based assumptions and examining IPV in the LGBTQ community allows for examination of cultural and systematic factors that may contribute to IPV (Baker, Buick, Kim, Moniz, & Nava, 2013). Further investigation into IPV in LGBTQ relationships will also increase understanding in how “internalized homophobia” or “stigma consciousness”, well known sexual minority stressors, are associated with IPV (Kimmes et al., 2017). Finally, asking those in LGBTQ communities about their experiences with IPV will lend them a voice to speak to their experiences and may reduce barriers to seeking help(Calton, Cattaneo, & Gebhard, 2015).
Many studies of IPV prevalence have not provided a definition of IPV or used measures to encompass all of the dynamics of IPV (Hamby, 2017). A widely used scale, the partner-spouse Conflict Tactics Scale (Straus, Hamby, Boney-McCoy, & Sugarman, 1996), has been be criticized as it does not differentiate between the impact of male-on-female versus female-on-male physical violence, fails to exclude play fighting compared to violence or distinguish between unhealthy conflict management versus “intentional, unwanted, nonessential, and harmful” behavior which defines violence (Hamby, 2017). This study works to address these weaknesses of previous prevalence studies by setting forth a clear definition of IPV using validated measurements specific to physical, sexual and psychological or emotional violence which capture the power imbalance necessary to define a behavior as IPV.
Emergency department (ED) estimates of IPV are almost solely based on heterosexual females, (Davidov, Larrabee, & Davis, 2014) administrative data discharge diagnoses (Datner et al., 2004; Davidov et al., 2014) or reports of physical and sexual violence only (Bazargan-Hejazi et al., 2014; Choo & Houry, 2014; Sutherland, Fantasia, & McClain, 2013). Many of these estimates do not take into account the prevalence of IPV among those presenting to the ED for non-IPV related conditions. Victims of IPV utilize the ED more than those not experiencing IPV for health conditions such as depression, pain syndromes, headaches, and digestive problems (Bonomi, Anderson, Rivara, & Thompson, 2007; J. Campbell et al., 2002; Coker et al., 2002). These disorders are not only associated with physical and sexual violence but also with battering and controlling behaviors (Bonomi et al., 2007). The prevalence of these various forms of IPV in association with sexual orientation and gender identification among an ED population is largely unknown.
The objectives of this study are 1) to estimate the prevalence of IPV among ED patients of both genders, considering their sexual orientation and gender identification, and 2) to examine the prevalence of IPV controlling behaviors in an ED population.
METHODS
This prospective cross-sectional survey was completed in a Level I Trauma Center Emergency Department with over 60,000 visits per year. Each patient who reported to the ED from November 2015 through November 2016 between 9am and midnight was screened for study eligibility. Eligible patients were 18 to 64 years of age, could read and write in English and presented to the ED without visitors, as documented in the electronic medical record by the triage nurse. Per requirements of the Institutional Review Board, only patients presenting alone were invited to participate to ensure patient safety and privacy while completing the study survey and to reduce the likelihood that the study survey would provoke an IPV incident. Patients were ineligible if they were unable to consent due to alcohol intoxication, had a developmental disability, or a durable power of attorney. This study was approved by the University of Iowa Institutional Review Board.
Patients were approached by the research team about the study following initial evaluation by the clinical care team. Each subject completed a written informed consent for the study. Following consent, subjects completed the paper and pencil survey in private with the research team returning after 10 minutes to retrieve the completed survey. Study data were entered into a REDCap electronic database hosted at The University of Iowa (Harris et al., 2009).
Violence experienced by a current or former intimate partner in the last 12 months was measured using validated scales for assessing heterosexual IPV, including a modified version of the Abuse Assessment Screen (AAS), (McFarlane, Parker, Soeken, & Bullock, 1992) and the Women’s Experience with Battering (WEB) Scale, which measures “battering” defined as chronic non-physical violence (Smith, Earp, & DeVellis, 1995). The AAS consisted of 3 questions: “Within the last year: 1) were you forced to have sex or engage in a sex act when you did not want to?”, 2) “... have you been hit, slapped, kicked, or otherwise physically hurt by anyone?”, and 3) …”have you been threatened with a weapon like a gun or a knife, or an object that can be used as a weapon?” Any affirmative responses were followed up with questions about who perpetrated the violence (i.e., current partner, former partner, or someone else). The AAS has high sensitivity (93–94%) and moderate specificity (55–99%) for detecting IPV (McFarlane et al., 1992). To date, no validated IPV screening questionnaire has been developed for populations of varying sexual orientations (Ard & Makadon, 2011; Brown & Herman, 2015). To accommodate men and same sex couples, the WEB scale was modified to use gender neutral language (i.e., “my partner”) as previous research has demonstrated that the role of power and control in same-sex relationships is similar to that in heterosexual relationships (Smith et al., 1995). Results from the AAS, which encompasses physical and sexual abuse, are referred to as “physical or sexual intimate partner violence (PS-IPV)” in further text. The WEB includes 10 items representing controlling or threatening behaviors. The WEB was modified to include both current and former partner perpetration of these behaviors. Each item is responded to on a six point Likert scale from strongly disagree (1 point) to strongly agree (6 points) with possible scores ranging 10–60 points. A score greater than 20 is considered positive for battering (Smith et al., 1995). Results from the WEB are referred to as battering in further text. A romantic or sexual partner was defined as “…anybody you have been involved with romantically or sexually, which might include current or former spouses, partners, boyfriends, girlfriends, people you have dated, people you were seeing, or people you hooked up with”.
Demographic information was collected on patient age, gender identity, race and ethnicity, sexual orientation and being in a current romantic or sexual relationship. Sexual orientation was assessed by the question:(Sexual Minority Assessment Research Team, 2009) How would you identify your sexual orientation? a) heterosexual or straight, b) gay c) lesbian, d) bisexual e) WSW (woman who has sex with women), f) MSM (man who has sex with men), g) questioning, h) asexual and i) other. Gender identity was measured with the following question:(Sexual Minority Assessment Research Team, 2009) “How do you identify your gender identity? a) female, b) male, c) transsexual, d) transgender, e) genderqueer, f) FTM (female-to-male), g) MTF (male-to-female), h) intersex, i) questioning, and j) other. For both sexual orientation and gender identity, subjects who identified as ‘other’ were asked to specify their orientation and/or identity in open text.
Data Analysis
The sexual orientation variable was categorized as heterosexual/straight, gay/MSM, lesbian/WSW, bisexual, and other LGBTQ orientation (questioning, asexual and other). The last category was created due to small numbers in the questioning, asexual and other orientation groups. Gender was coded as female, male, and non-binary.
To examine if subject demographics differed by presence of IPV or IPV subtype (PS-IPV or battering), comparisons of categorical variables were completed using the Pearson’s chi-square or Fisher’s exact test, and for continuous variables using the Student’s t-test. A subject was considered to be IPV positive for any type of IPV if they responded affirmatively to whether a current or former partner had perpetrated physical or sexual IPV (PS-IPV) on any of the AAS questions or if they screened positive (score >20) for battering on the WEB. Analyses are presented for the outcomes of any IPV, current partner PS-IPV, former partner PS-IPV and battering.
To estimate the odds of reporting any IPV and IPV subtype (PS-IPV or battering) while controlling for covariates, multivariable logistic regression was used to estimate odds ratios and 95% confidence intervals. Covariates were considered for inclusion in the model based on a priori knowledge including age, gender, race/ethnicity, and current relationship status. Multiplicative and additive interaction between gender and sexual orientation was tested and no interaction was found. All analyses were completed using SAS® software, version 9.4, Cary, NC, USA.
RESULTS
During the study period, 2,575 patients reported to the ED without visitors according to the electronic medical record (Figure 1). Among these, 127 could not be approached due to clinical care and 853 screened ineligible. Among those eligible (n=1595), 1145 (71.8%) consented to participate in the study and 1136 completed a survey (71.2%). The mean age of subjects was 37.3 years, 56.3% were female, 77.9% White, 10.6% reported being LGBTQ, and 1.5% reported their gender as non-binary. Overall, 11.6% of subjects reported IPV in the last year.
Figure 1.
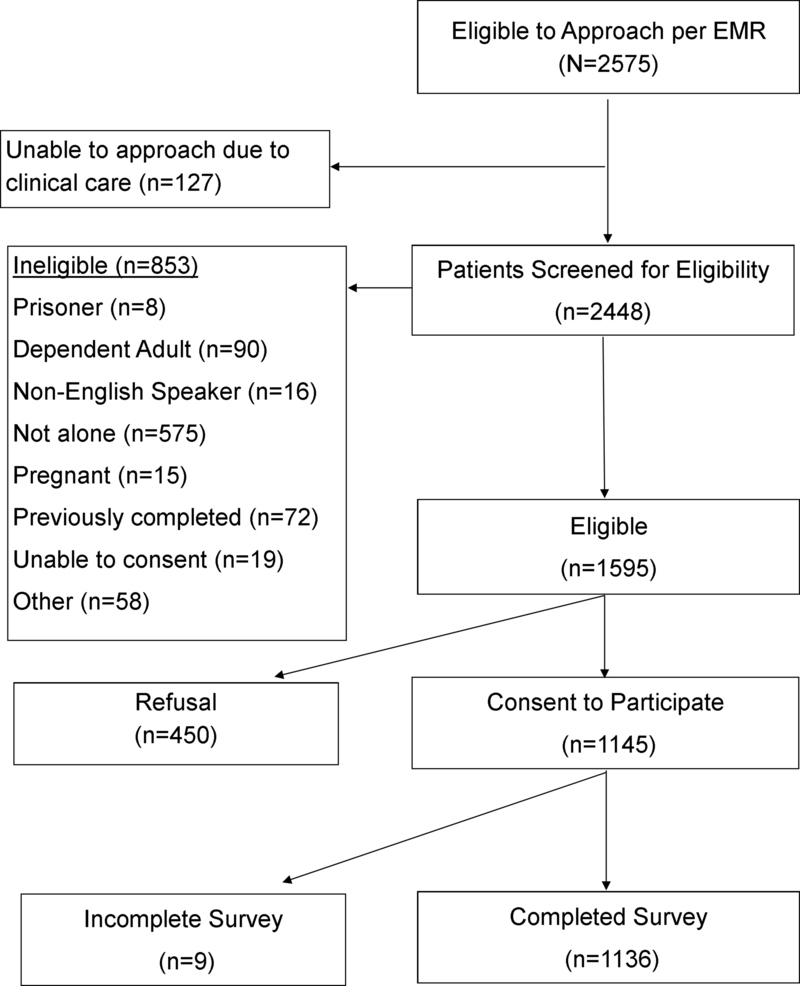
Study flow diagram
Reports of IPV did not differ significantly by gender as 9.2% (44 of 477) of males, 13.5% (86 of 636) of females, and 11.8% (2 of 17) of non-binary gender subjects reported IPV (p=0.0872) (Table 1). Younger subjects, on average, were more likely to report any IPV (35.2 vs 37.6 years, p=0.0459) and heterosexual subjects were less likely to report IPV than LGBTQ subjects (10.8% vs 18.3%, p=0.0151) (Table 1). Among all subjects, bisexuals reported the highest prevalence of IPV at 21.6%, followed by gay men at 18.5%. Bisexual females reported higher prevalence of IPV than bisexual males (24% versus 9% respectively, p=0.4, data not shown).
Table 1.
Subject Demographics by report of Intimate Partner Violence in the Last 12 months (N=1136)
| Total | IPV1 | ||||||
|---|---|---|---|---|---|---|---|
| No | Yes | ||||||
| N | (Col %) | n | (Row %) | n | (Row %) | p-value | |
| ALL | 1136 | 1004 | (88.4) | 132 | (11.6) | ||
| Age | |||||||
| Mean (SD) | 37.3 | (13.5) | 37.6 | (13.5) | 35.2 | (12.3) | 0.0459 |
| 18–24 | 255 | (22.5) | 225 | (88.2) | 30 | (11.8) | 0.0549 |
| 25–34 | 278 | (24.5) | 238 | (85.6) | 40 | (14.4) | |
| 35–44 | 229 | (20.2) | 196 | (85.6) | 33 | (14.4) | |
| 45–54 | 219 | (19.3) | 202 | (92.2) | 17 | (7.8) | |
| 55–64 | 155 | (13.7) | 143 | (92.3) | 12 | (7.7) | |
| Gender | |||||||
| Male | 477 | (42.2) | 433 | (90.8) | 44 | (9.2) | 0.0872 |
| Female | 636 | (56.3) | 550 | (86.5) | 86 | (13.5) | |
| Non-binary Identity | 17 | (1.5) | 15 | (88.2) | 2 | (11.8) | |
| Race | 0.6433 | ||||||
| Caucasian/White | 885 | (77.9) | 785 | (88.7) | 100 | (11.3) | |
| Black/African American | 135 | (11.9) | 117 | (86.7) | 18 | (13.3) | |
| Asian | 22 | (1.9) | 20 | (90.9) | 2 | (9.1) | |
| American Indian/Alaskan Native | 10 | (0.9) | 10 | (100.0) | 0 | ||
| Multiple Race | 84 | (7.4) | 72 | (85.7) | 12 | (14.3) | |
| Hispanic | 70 | (6.6) | 60 | (85.7) | 10 | (14.3) | 0.4724 |
| Sexual Orientation | |||||||
| Heterosexual/Straight | 1008 | (89.4) | 899 | (89.2) | 109 | (10.8) | 0.0151 |
| Non-Heterosexual | 120 | (10.6) | 98 | (81.7) | 22 | (18.3) | |
| Lesbian | 23 | (2.0) | 20 | (87.0) | 3 | (13.0) | 0.09192 |
| Gay | 27 | (2.4) | 22 | (81.5) | 5 | (18.5) | |
| Bisexual | 51 | (4.5) | 40 | (78.4) | 11 | (21.6) | |
| Other LGBTQ | 19 | (1.7) | 16 | (84.2) | 3 | (15.8) | |
| Current relationship | 0.0068 | ||||||
| Yes | 685 | (62.4) | 619 | (90.4) | 66 | (9.6) | |
| No | 412 | (37.6) | 350 | (85.0) | 62 | (15.0) | |
Any IPV classified as positive for physical or sexual violence (as measured by the abuse assessment screen) or positive for battering (as measured by the Women’s Experience with battering) by a current or former partner
Fisher exact text for Heterosexual/straight versus Non-heterosexual subgroups
Overall, the most common type of IPV reported was battering at 9.3%. Physical/sexual IPV (PS-IPV) was more frequently reported to be perpetrated by former partners (4.3%) than current partners (2.2%) (Table 2). Those whose gender identity was non-binary had the highest prevalence of current partner IPV (11.8%, 2 of 17), while females (2.8%) were more likely to report current partner IPV than males (1.0%; p=0.0036). The prevalence of PS-IPV by a current partner was highest among subjects identifying as other LGBTQ (5.3%), lesbian (4.3%), bisexual (3.9%), and gay (3.7%); all were greater than the prevalence among heterosexuals (2.0%).
Table 2.
Patient Characteristics by type of Intimate Partner Violence Experienced
| Current Partner PS-IPV | Former Partner PS-IPV | Battering1,2 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | ||||||||||
| n | (row%) | n | (row%) | p-value | n | (row%) | n | (row%) | p-value | n | (row%) | n | (row%) | p-value | |
| All | 1111 | (97.8) | 25 | (2.2) | 1087 | (95.7) | 49 | (4.3) | 891 | (90.7) | 91 | (9.3) | |||
| Age | |||||||||||||||
| Mean (SD) | 37.4 | (13.5) | 36.2 | (9.9) | 0.6675 | 37.6 | (13.5) | 30.7 | (9.7) | 0.0003 | 36.3 | (13.2) | 37.0 | (12.9) | 0.6068 |
| 18–24 | 253 | (99.2) | 2 | (0.8) | 0.0731 | 241 | (95.5) | 14 | (5.5) | 0.0016 | 216 | (91.9) | 19 | (8.1) | 0.8478 |
| 25–34 | 268 | (96.4) | 10 | (3.6) | 259 | (93.2) | 19 | (6.8) | 234 | (90.4) | 25 | (9.7) | |||
| 35–44 | 221 | (96.5) | 8 | (3.5) | 216 | (94.3) | 13 | (5.7) | 177 | (89.4) | 21 | (10.6) | |||
| 45–54 | 215 | (98.2) | 4 | (1.8) | 217 | (99.1) | 2 | (0.9) | 161 | (92.0) | 14 | (175.0) | |||
| 55–64 | 154 | (99.4) | 1 | (0.6) | 154 | (99.4) | 1 | (0.6) | 103 | (89.6) | 12 | (10.4) | |||
| Gender | 0.0036 | 0.0754 | 0.3440 | ||||||||||||
| Male | 472 | (99.0) | 5 | (1.0) | 464 | (97.3) | 13 | (2.7) | 378 | (92.2) | 32 | (7.8) | |||
| Female | 618 | (97.2) | 18 | (2.8) | 601 | (94.5) | 35 | (5.5) | 495 | (89.5) | 58 | (10.5) | |||
| Non-binary gender identity | 15 | (88.2) | 2 | (11.8) | 16 | (9.4) | 1 | (5.9) | 14 | (93.3) | 1 | (6.7) | |||
| Race | 0.40243 | 0.80462 | 0.4224 | ||||||||||||
| Caucasian/White | 868 | (98.1) | 17 | (1.9) | 847 | (95.7) | 38 | (4.3) | 695 | (90.6) | 72 | (9.4) | |||
| Black/African American | 131 | (97.0) | 4 | (3.0) | 127 | (94.1) | 8 | (5.9) | 106 | (93.0) | 8 | (7.0) | |||
| Asian | 21 | (95.5) | 1 | (4.6) | 22 | (100.0) | 0 | 19 | (95.0) | 1 | (5.0) | ||||
| American Indian/Alaskan Native | 10 | (100.0) | 0 | 10 | (100.0) | 0 | 9 | (100.0) | 0 | ||||||
| Multiple Race | 81 | (96.4) | 3 | (3.6) | 81 | (96.4) | 3 | (3.6) | 62 | (86.1) | 10 | (13.9) | |||
| Hispanic | 70 | (100.0) | 0 | 65 | (92.9) | 5 | (7.1) | 0.2292 | 53 | (89.8) | 6 | (10.2) | 0.8052 | ||
| Sexual Orientation | |||||||||||||||
| Heterosexual/Straight | 998 | (98.0) | 20 | (2.0) | 0.1247 | 969 | (96.1) | 39 | (3.9) | 0.0233 | 802 | (91.5) | 75 | (8.9) | 0.0381 |
| Non-Heterosexual | 115 | (95.8) | 5 | (4.2) | 110 | (91.7) | 10 | (8.4) | 86 | (85.2) | 15 | (14.2) | |||
| Lesbian | 22 | (96.7) | 1 | (4.3) | 0.18794 | 22 | (95.7) | 1 | (4.4) | 0.03113 | 14 | (82.4) | 3 | (17.6) | 0.17093 |
| Gay | 26 | (96.3) | 1 | (3.7) | 24 | (88.9) | 3 | (11.1) | 18 | (85.7) | 3 | (14.3) | |||
| Bisexual | 49 | (96.1) | 2 | (3.9) | 45 | (88.2) | 6 | (11.8) | 40 | (85.1) | 7 | (14.9) | |||
| Other LGBTQ | 18 | (94.7) | 1 | (5.3) | 19 | (100.0) | 0 | 14 | (87.5) | 2 | (12.5) | ||||
| Current Relationship | 0.00132 | 0.0687 | <.0001 | ||||||||||||
| Yes | 662 | (96.6) | 23 | (3.4) | 661 | (96.5) | 24 | (3.5) | 624 | (94.3) | 38 | (5.7) | |||
| No | 410 | (99.5) | 2 | (0.5) | 388 | (94.2) | 24 | (5.8) | 243 | (82.9) | 50 | (17.1) | |||
Among subjects with a current partner or a former partner within the last 12 months
Battering is defined as chronic non-physical violence and represents controlling and threating behaviors
Fisher exact test
Fisher exact text for Heterosexual/straight versus Non-heterosexual subgroup
Subjects who experienced former partner PS-IPV were significantly younger (30.7 years vs 37.6 years, p=0.0003) than those who had not experienced former partner PS-IPV. Heterosexuals were significantly less likely to report former partner PS-IPV (3.9%) than gay (11.1%) or bisexual subjects (11.8%) (p=0.031).
Over 14% of non-heterosexuals reported battering compared to 9% of heterosexuals (p=0.0381). The highest prevalence of battering was reported by lesbians (17.6%), bisexuals (14.9%) and gays (14.3%). Among those reporting battering, only 43.2% (38 of 88) reported being in a current relationship.
Odds of reporting IPV in the last 12 months was higher for females and LGBTQ patients, although confidence intervals were significant for gender but not for sexual orientation (Table 3). After controlling for age, subjects who identified as being female had an odds of any IPV of 1.67 (95% CI: 1.10–2.53) compared to males; those who were not in a current relationship had 2.01 odds of any IPV (95% CI: 1.36–2.99) compared to those in a current relationship. Bisexuals and gays had 1.66 (95% CI: 0.79–3.49) and 2.45 (95% CI: 0.86–7.02) the odds of reporting any IPV relative to heterosexuals, respectively. When sexual orientation was analyzed as a dichotomous variable after controlling for age, gender and being in a current relationship, the odds of any IPV in the last year was 63% higher among LGBTQ compared to heterosexuals (1.63 (95% CI: 0.94–2.80); data not shown). After controlling for age, female gender identification (aOR=2.70 (95% CI: 1.46–9.99)) and gay (aOR=5.50 (95% CI: 1.60–18.94)) sexual orientation were significantly associated with reporting PS-IPV. In multivariable analyses, not being in a current relationship was the only factor significantly associated with battering. (aOR=4.16 [2.58–6.71]).
Table 3.
Adjusted Odds of reporting intimate partner violence in the last 12 months
| IPV | PS-IPV1 | Battering2,3 | |
|---|---|---|---|
| (n=132) | (n=73) | (n=91) | |
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Age | |||
| 18–24 | 1.62 (0.92–2.88) | 2.82 (1.11–7.17) | 0.75 (0.39–1.45) |
| 25–34 | 2.54 (1.47–4.41) | 6.03 (2.54–14.29) | 1.41 (0.75–2.63) |
| 35–44 | 2.62 (1.49–4.62) | 5.35 (2.19–13.06) | 1.65 (0.86–3.16) |
| 45–64 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Gender | |||
| Female | 1.67 (1.10–2.53) | 2.70 (1.46–9.99) | 1.59 (0.97–2.62) |
| Non-binary identity | 0.96 (0.19–2.53) | 2.42 (0.44–13.48) | 0.74 (0.08–6.66) |
| Male | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Sexual Orientation | |||
| Bisexual | 1.66 (0.79–3.49) | 1.84 (0.77–4.41) | 1.45 (0.57–3.67) |
| Gay | 2.45 (0.86–7.02) | 5.50 (1.60–18.94) | 1.81 (0.48–6.95) |
| Lesbian | 1.15 (0.32–4.05) | 1.22 (0.27–5.54) | 2.74 (0.73–10.30) |
| Other LGBTQ | 1.22 (0.32–4.68) | 0.67 (0.08–5.87) | 1.08 (0.22–5.34) |
| Heterosexual | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Current Relationship | |||
| Yes | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| No | 2.01 (1.36–2.99) | 1.26 (0.74–2.14) | 4.16 (2.58–6.71) |
PS-IPV, physical or sexual intimate partner violence
Former or current partner physical or sexual violence
Among subjects with a current partner or a former partner within the last 12 months
Battering is defined as chronic non-physical violence and represents controlling and threating behaviors
DISCUSSION
In our study of ED patients, while not statistically significant, LGBTQ subjects had higher odds of any IPV than heterosexuals while gay subjects had significantly higher odds of physical or sexual IPV then heterosexuals. Over 18% of LGBTQ subjects reported IPV, and all IPV sub-types were reported more frequently among LGBTQ than heterosexual patients (current partner PS-IPV: 4.2% vs 2.0%; former partner PS-IPV: 8.4% vs 3.9%; battering 14.2% vs 8.9%). Females demonstrated a higher prevalence and odds of IPV than males overall and across all IPV sub-types. Of interest is the increased odds of reporting any IPV or battering in the last year by subjects who were not in a current relationship at the time of the survey. Continuation of violence following relationship separation is not unique to our study (Walker, Logan, Jordan, & Campbell, 2004). In an analysis of coercive control by an ex-spouse in the National Violence Against Women Survey, Johnson and Leone found that on the nine item Coercive Control Scale, the mean number of coercive controls used among ex-spouses was over seven (Johnson, Leone, & Xu, 2014). In a population of women seeking elective abortions, a similar association was found indicating former partners were more likely to perpetrate PS-IPV than current partners (8.3% vs 2.8%) (Saftlas et al., 2010). One pathway might be that subjects ended relationships that involved IPV, or, ending the relationship may spark or intensify incidents of IPV (J. C. Campbell et al., 2003; Walker et al., 2004). Given the cross-sectional design of the study, we are unable to support one hypothesis over another but this result warrants further investigation.
Previous research suggests the prevalence of IPV in the ED is higher than the prevalence of IPV in the general population (Bonomi et al., 2007; J. Campbell et al., 2002; Coker et al., 2002); however we found the prevalence of IPV in LGBTQ patients seen in the ED to be similar, albeit on the lower end, to that reported from LGBTQ community samples: 12–40% of gay men, (Balsam, Rothblum, & Beauchaine, 2005; Goldberg & Meyer, 2013; Taylor N.T. Brown & Herman, 2015) 7–27% of lesbians, (Goldberg & Meyer, 2013; Taylor N.T. Brown & Herman, 2015) 9–52% of bisexuals (Goldberg & Meyer, 2013; Taylor N.T. Brown & Herman, 2015) in community samples reported IPV compared to 18.5%, 13.0% and 21.6%, respectively, in our ED sample. In contrast, heterosexual ED patients had an IPV prevalence of 10.8%, which, as expected, is much higher than estimates of 1–4% (M. J. Breiding et al., 2014; Tjaden, 2000) in the general population. Our failure to observe a higher IPV prevalence among LGBTQ patients in the ED compared to LGBTQ community samples, as one might expect based on heterosexual IPV prevalence studies, may be explained by a number of factors. LGBTQ populations report decreased access to healthcare, increased un-met healthcare needs, and use healthcare less frequently than non-LGBTQ populations due to lack of insurance(Everett & Mollborn, 2014; Macapagal, Bhatia, & Greene, 2016) therefore the LGBTQ ED population may differ significantly from the LGBTQ community. In addition, LGBTQ may fear disclosing their orientation to their healthcare provider and discrimination upon disclosure (Baker et al., 2013; Macapagal et al., 2016) which may result in under reporting of sexual orientation in a healthcare based research study. It is also important to note that over time heterosexuals may have become accustomed to and more comfortable with reporting IPV to healthcare professionals because of increased screening traditionally focused on heterosexual relationships and supportive responses; the same may not yet be true of the LGBTQ community.
After controlling for age, gender and current relationship status, we found non-significant increased odds of IPV for non-heterosexuals compared with heterosexuals, and all LGBTQ groups reported a higher prevalence of IPV than heterosexuals across all IPV sub-types. Previous work in California found that bisexual women reported PS-IPV at 4 times the odds of heterosexual women; and gay men were at two-fold higher odds compared to heterosexual men (Goldberg & Meyer, 2013). In studies of late adolescence/early adulthood, the odds of PS-IPV among LGBTQ has been estimated to be 2 to 4 times that of heterosexual youth (Walters, 2013; Whitton, Newcomb, Messinger, Byck, & Mustanski, 2016). Our study found 1.5 to five times higher odds of IPV among LGBTQ subjects compared to heterosexuals, similar to previous research, but our study may have been under-powered to find statistically significant results among these groups. In addition, the discordance between our results and previous literature may be due to differences in the populations studied and lack of generalizable findings across studies of IPV in LGBTQ populations.
Battering is prevalent among ED patients. Almost 10% reported a partner exhibited controlling behaviors over them, and no differences in prevalence were found between females and males. The long-term health consequences of battering are well established in heterosexual females (Bonomi et al., 2007; Coker et al., 2002) but the consequences of battering violence among males and sexual minorities are largely unknown and require further study.
Our study suggests the odds of IPV among LGBTQ is similar, if not greater than, that of heterosexuals. This finding further stresses the need to develop LGBTQ resources and IPV policies that support victims beyond the traditional heterosexual female. Like heterosexual female IPV victims, patients identifying as LGBTQ are more likely to report adverse health outcomes including suicidal ideation (Remafedi, French, Story, Resnick, & Blum, 1998). Potential interventions are likely to differ for LGBTQ couples as they face additional barriers to services, such as men not being allowed in domestic violence shelters, and having a history of prior traumatic experiences if their sexual orientation was not accepted by their family and community (Ard & Makadon, 2011). In addition to IPV-related help seeking barriers experienced among heterosexual females, LGBTQ face additional barriers; for example, legal definitions of IPV may exclude LGBTQ relationships, the additional fear of being “outed” when they disclose the violence, and insensitivity of law enforcement and civil courts when adjudicating an IPV incident involving an LGBTQ couple (Calton et al., 2015).
In our sample, 10% of ED patients identified as being LGBTQ, an estimate higher than national estimates of 3.4% or reports in Iowa of 2.8% (Gary J. Gates & Frank Newport, 2013). Iowa does have a more inclusive LGBTQ culture that allows for LGBTQ marriage, medical decision making capacity and state leave for LGBTQ couples (Movement Advancement Project, 2015). Furthermore, the study was conducted in a tertiary care center located within a city with established LGBTQ inclusivity (Human Rights Campaign Foundation, 2016). This inclusivity may account for the higher prevalence of LGBTQ in the study population as those within the community may be more comfortable reporting their sexual orientation and gender identity than those in less inclusive communities. This result may also suggest a higher ED utilization among the LGBTQ population within the catchment area of the hospital, which is in contrast to previous reports of healthcare under-utilization in the general LGBTQ population (Everett & Mollborn, 2014; Macapagal et al., 2016). Given the health disparities experienced by LGBTQ, ED staff should consider collecting sexual orientation and gender identification data at intake. Previous work suggests LGBTQ patients are willing to disclose this information in a safe environment and ED staffs are comfortable collecting such data given the impact it has on health outcomes (German et al., 2016).
LIMITATIONS
This study has limitations. This is a single center study of a largely Caucasian English-speaking population in a rural state and the results may not be generalizable to other populations. Due to safety concerns expressed by the IRB, only patients alone at ED triage were eligible for the study. Previous research suggests patients experiencing IPV are less likely to present for healthcare by themselves (McCloskey et al., 2007) suggesting the prevalence estimated in our study may be lower than that in our general ED population. The AAS does not discriminate between being “hit, kicked, or slapped” as part of horseplay versus with intent to injury someone therefore the prevalence of physical IPV may be artificially inflated; on the contrary, the AAS does not account for choking or strangulation and therefore this type of physical IPV may not be reported resulting in artificially reduced physical IPV prevalence. In addition, if our measure of physical IPV had excluded horseplay, a greater difference in the odds of physical IPV among females compared to males may have been found. Lastly, subjects were not asked if the battering they reported was perpetrated by a current or former partner therefore we were unable to examine battering by this relationship characteristic.
CONCLUSION
Although we did not find statistically increased odds of IPV among LGBTQ ED patients, sexual minorities did report a higher prevalence of IPV by both current and former partners and of battering behavior. Given the barriers that LGBTQ patients may have in disclosing their sexual orientation to healthcare providers, they may also have barriers in reporting violent victimization by intimate partners. Following research that has identified the high prevalence of IPV victims in the ED, many ED environments have become far more receptive to identifying IPV victims through routine screening, and follow-up support services and referrals. However, these services have focused on heterosexual females. Broadening these changes to better incorporate sexual minorities can help expand the impact of ED response to patients experiencing IPV.
Acknowledgments:
The authors would like to thank Catherine Fairfield BSN, EM Research Coordinator, and Julie Amendola, Kimberly Meyer, Vaelen Molian, and Ashley Radig with the Emergency Department Research Enroller Program (ED-REP) for their essential role in enrolling patients and collecting data for this project.
Funding Sources/Disclosures:
This work was funded by University of Iowa, Injury Prevention Research Center pilot grant program (CDC/NCICP R49CE002108) and the Institute for Clinical and Translational Science grant support (NIH/CTSA grant #: U54TR001356)
Footnotes
Author Disclosure Statement
KKH, CPA and AFS report no conflicts of interest.
References
- Ard KL, & Makadon HJ (2011). Addressing intimate partner violence in lesbian, gay, bisexual, and transgender patients. J Gen Intern Med, 26(8), 930–933. doi: 10.1007/s11606-011-1697-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker NL, Buick JD, Kim SR, Moniz S, & Nava KL (2013). Lessons from examining same-sex intimate partner violence. Sex Roles, 69(3–4), 182–192. doi: 10.1007/s11199-012-0218-3 [DOI] [Google Scholar]
- Balsam KF, Rothblum ED, & Beauchaine TP (2005). Victimization over the life span: a comparison of lesbian, gay, bisexual, and heterosexual siblings. J Consult Clin Psychol, 73(3), 477–487. doi: 10.1037/0022-006x.73.3.477 [DOI] [PubMed] [Google Scholar]
- Bazargan-Hejazi S, Kim E, Lin J, Ahmadi A, Khamesi MT, & Teruya S (2014). Risk Factors Associated with Different Types of Intimate Partner Violence (IPV): An Emergency Department Study. J Emerg Med, 47(6), 710–720. doi: 10.1016/j.jemermed.2014.07.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, . . . Stevens MR (2011). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. . Retrieved from Atlanta, GA: [Google Scholar]
- Bonomi AE, Anderson ML, Rivara FP, & Thompson RS (2007). Health outcomes in women with physical and sexual intimate partner violence exposure. Journal of women’s health (2002), 16(7), 987–997. doi: 10.1089/jwh.2006.0239 [DOI] [PubMed] [Google Scholar]
- Breiding M, Basile K, Smith S, Black M, & Mahendra R (2015). Intimate Partner Violence Surveillance: Uniform Definitions and Recommended Data Elements, Version 2.0. Retrieved from Atlanta GA: https://www.cdc.gov/violenceprevention/pdf/ipv/intimatepartnerviolence.pdf
- Breiding MJ, Smith SG, Basile KC, Walters ML, Chen J, & Merrick MT (2014). Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization--national intimate partner and sexual violence survey, United States, 2011. MMWR Surveill Summ, 63(8), 1–18. [PMC free article] [PubMed] [Google Scholar]
- Brown TNT, & Herman JL (2015). Intimate Partner Violence and Sexual Abuse Among LGBT People: A Review of the Existing Literature. Retrieved from https://williamsinstitute.law.ucla.edu/wp-content/uploads/Intimate-Partner-Violence-and-Sexual-Abuse-among-LGBT-People.pdf
- Calton JM, Cattaneo LB, & Gebhard KT (2015). Barriers to Help Seeking for Lesbian, Gay, Bisexual, Transgender, and Queer Survivors of Intimate Partner Violence. Trauma Violence Abuse. doi: 10.1177/1524838015585318 [DOI] [PubMed] [Google Scholar]
- Campbell J, Jones AS, Dienemann J, Kub J, Schollenberger J, O’Campo P, . . . Wynne C (2002). Intimate partner violence and physical health consequences. Archives of Internal Medicine, 162(10), 1157–1163. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Webster D, Koziol-McLain J, Block C, Campbell D, Curry MA, . . . Laughon K (2003). Risk factors for femicide in abusive relationships: results from a multisite case control study. Am J Public Health, 93(7), 1089–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choo EK, & Houry DE (2014). Managing Intimate Partner Violence in the Emergency Department. Ann Emerg Med. doi: 10.1016/j.annemergmed.2014.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, & Smith PH (2002). Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine, 23(4), 260–268. [DOI] [PubMed] [Google Scholar]
- Datner EM, O’Malley M, Schears RM, Shofer FS, Baren J, & Hollander JE (2004). Universal screening for interpersonal violence: inability to prove universal screening improves provision of services. European journal of emergency medicine : official journal of the European Society for Emergency Medicine, 11(1), 35–38. [DOI] [PubMed] [Google Scholar]
- Davidov DM, Larrabee H, & Davis SM (2014). United States Emergency Department Visits Coded for Intimate Partner Violence. J Emerg Med. doi: 10.1016/j.jemermed.2014.07.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett BG, & Mollborn S (2014). Examining Sexual Orientation Disparities in Unmet Medical Needs among Men and Women. Popul Res Policy Rev, 33(4), 553–577. doi: 10.1007/s11113-013-9282-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates Gary J., & Newport Frank. (2013). LGBT Percentage Highest in D.C., Lowest in North Dakota. Retrieved from http://www.gallup.com/poll/160517/lgbt-percentage-highest-lowest-north-dakota.aspx?version=print [Google Scholar]
- German D, Kodadek L, Shields R, Peterson S, Snyder C, Schneider E, . . . Haider A (2016). Implementing Sexual Orientation and Gender Identity Data Collection in Emergency Departments: Patient and Staff Perspectives. LGBT Health. doi: 10.1089/lgbt.2016.0069 [DOI] [PubMed] [Google Scholar]
- Goldberg NG, & Meyer IH (2013). Sexual orientation disparities in history of intimate partner violence: results from the California health interview survey. J Interpers Violence, 28(5), 1109–1118. doi: 10.1177/0886260512459384 [DOI] [PubMed] [Google Scholar]
- Hamby S (2017). On defining violence and why it matters. Psychology of Violence, 7(2), 167–180. doi: 10.1037/vio0000117 [DOI] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 42(2), 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human Rights Campaign Foundation. (2016). 2016 Municipal Equality Index Scorecard: Iowa City IA. Retrieved from http://assets.hrc.org//files/assets/resources/Iowa-City-Iowa-2016.pdf?_ga=1.154992440.1650320592.1492458198
- Johnson MP, Leone JM, & Xu Y (2014). Intimate terrorism and situational couple violence in general surveys: ex-spouses required. Violence Against Women, 20(2), 186–207. doi: 10.1177/1077801214521324 [DOI] [PubMed] [Google Scholar]
- Kimmes JG, Mallory AB, Spencer C, Beck AR, Cafferky B, & Stith SM (2017). A Meta-Analysis of Risk Markers for Intimate Partner Violence in Same-Sex Relationships. Trauma Violence Abuse, 1524838017708784. doi: 10.1177/1524838017708784 [DOI] [PubMed] [Google Scholar]
- Macapagal K, Bhatia R, & Greene GJ (2016). Differences in Healthcare Access, Use, and Experiences Within a Community Sample of Racially Diverse Lesbian, Gay, Bisexual, Transgender, and Questioning Emerging Adults. LGBT Health, 3(6), 434–442. doi: 10.1089/lgbt.2015.0124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey LA, Williams CM, Lichter E, Gerber M, Ganz ML, & Sege R (2007). Abused women disclose partner interference with health care: an unrecognized form of battering. J Gen Intern Med, 22(8), 1067–1072. doi: 10.1007/s11606-007-0199-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane J, Parker B, Soeken K, & Bullock L (1992). Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA : the journal of the American Medical Association, 267(23), 3176–3178. [DOI] [PubMed] [Google Scholar]
- Movement Advancement Project. (2015). Iowa’s LGBT Laws and Policies. Retrieved from http://www.lgbtmap.org/equality_maps/profile_state/IA
- Remafedi G, French S, Story M, Resnick MD, & Blum R (1998). The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health, 88(1), 57–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saftlas AF, Wallis AB, Shochet T, Harland KK, Dickey P, & Peek-Asa C (2010). Prevalence of intimate partner violence among an abortion clinic population. American Journal of Public Health, 100(8), 1412–1415. doi: 10.2105/AJPH.2009.178947; 10.2105/AJPH.2009.178947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexual Minority Assessment Research Team. (2009). Best Practices for Asking Questions about Sexual Orientation on Surveys. Retrieved from http://williamsinstitute.law.ucla.edu/wp-content/uploads/SMART-FINAL-Nov-2009.pdf
- Smith PH, Earp JA, & DeVellis R (1995). Measuring battering: development of the Women’s Experience with Battering (WEB) Scale. Womens Health, 1(4), 273–288. [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised conflict tactics scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues, 17, 283–316. [Google Scholar]
- Sutherland MA, Fantasia HC, & McClain N (2013). Abuse experiences, substance use, and reproductive health in women seeking care at an emergency department. J Emerg Nurs, 39(4), 326–333. doi: 10.1016/j.jen.2011.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor NT Brown, & Herman JL (2015). Intimate Partner Violence and Sexual Abuse Among LGBT People: A Review of the Existing Literature. Retrieved from Los Angeles, CA: https://williamsinstitute.law.ucla.edu/wp-content/uploads/Intimate-Partner-Violence-and-Sexual-Abuse-among-LGBT-People.pdf
- Tjaden PTN (2000). Full Report of the Prevalence, Incidence and Consequences of Violence Against Women (NCJ 183781). Retrieved from Rockville, MD: [Google Scholar]
- Walker R, Logan TK, Jordan CE, & Campbell JC (2004). An integrative review of separation in the context of victimization: consequences and implications for women. Trauma, violence & abuse, 5(2), 143–193. doi: 10.1177/1524838003262333 [DOI] [PubMed] [Google Scholar]
- Walters ML, Chen J, & Breiding MJ,. (2013). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Findings on Victimization by Sexual Orientation. Retrieved from Atlanta, GA: [Google Scholar]
- Whitton SW, Newcomb ME, Messinger AM, Byck G, & Mustanski B (2016). A Longitudinal Study of IPV Victimization Among Sexual Minority Youth. J Interpers Violence. doi: 10.1177/0886260516646093 [DOI] [PMC free article] [PubMed] [Google Scholar]


