Abstract
Objectives:
To compare the therapeutic effect of 6 SSRIs among the Chinese senile depression patients. And drug-induced nausea leads to low compliance in elderly depression patients in China, it is urgent to assess the safety of 6 SSRIs with respect to induced-nausea among the Chinese senile depression patients.
Method:
In the present study, a network of meta-analysis was conducted to assess the efficacy of 6 SSRIs among the Chinese senile depression patients, in addition, the safety of 6 SSRIs with respect to induced-nausea among the Chinese senile depression patients was also evaluated. PubMed, Embase databases, WanFang, CNKI, ChongqingWeiPu were searched for the related articles. The primary outcome of this study were the number of effective cases of SSRIs and the number of cases of nausea caused by SSRIs in Chinese elderly depressed patients. Odds ratios (ORs) and corresponding 95% confidence intervals(95%CIs) were calculated within pairwise and network meta-analysis.
Results:
Twenty eight trials were identified, including 2246 patients, the network meta-analysis indicated that Escitalopram was associated with a lower risk of nausea compared Paroxetine (odds ratios 0.49, 95%CI = 0.34–0.69) when they were used in Chinese elderly depressed patients. Escitalopram also exhibited distinct advantages compared other SSRIs.
In terms of drug efficacy, Escitalopram was significantly superior to Paroxetine (OR = 2.26, 95%CI = 1.55–3.37).
Conclusion:
The rank of SSRIs with respect to induced-nausea was: Combination of EP > Fluoxetine > Paroxetine > Citalopram > Sertraline > Fluvoxamine > Escitalopram, respectively.
Keywords: nausea, network of meta analysis, Selective Serotonin Reuptake Inhibitors, senile depression patients
1. Introduction
Depression has become an important risk factor affecting the health of the elderly and seriously reduces the quality of life of the elderly.[1] Depression is common among the elderly worldwide, however, given the rapid urbanization and accompanying social changes, the situation may be even worse in China.[2] For example, a previous study indicated that the prevalence of depression among the general group in China is 15%, while the prevalence of geriatric depression is 17.3%.[3] Thus far, at least 15% of the total population in China is elderly.[4] It has been predicted that by the middle of the 22nd century, 25% of the worlds elderly population will be Chinese citizens.[5] Also, the aged population of China has a high prevalence of pre-existing diseases,[6] and much important is the fact that the drug tolerance of the elderly decreases as a result of lower metabolic and degradation of organs.[7]
Without appropriate treatment, depression in the elderly can easily lead to or aggravate some serious diseases such as: coronary heart disease,[8] hypertension,[9] diabetes,[10] and tumors.[11] In addition, severe depression even results in suicide.[12]
Previous studies have shown that drug compliance is low among elderly depressed patients in China, partly because of dissatisfaction with the efficacy of the drugs, and also because some drugs can cause side effects, such as nausea.[13–16]
Therefore, in order to improve the medication compliance of elderly depressed patients in China, this study evaluated the efficacy of SSRIs. At the same time, we evaluated the gastrointestinal side effects (nausea) associated with the use of this drug in elderly Chinese, hoping to improve valuable information for reducing the burden of mental illness in China.
Currently, selective serotonin reuptake inhibitors (SSRIs) are recommended by the National Institute for Health and Care Excellence (NICE) as the first-line treatment of depression,[17] and have been the most prescribed antidepressants in many countries, including China.[18]
SSRIs, including Citalopram, Fluvoxamine, Fluvoxamine, Sertraline, Paxil, and Escitalopram, have been approved in many countries for different age groups. Although western countries have carried out the evaluation of efficacy and side effects of these drugs in the elderly population,[19] the health status of the elderly in China is different from that of their peers in foreign countries and their tolerance to the drugs is also different.[20] Therefore, it is necessary to evaluate the use of these drugs in elderly Chinese population. A large number of studies reported the side effects of SSRIs,[21–23] and most of them indicated nausea as a common side effect of SSRIs.[21] Although several studies of meta-analysis have compared the risk of nausea between SSRIs and other antidepressants,[21,24,25] there has not been any comparative analysis about the incidence of SSRIs-induced nausea. Besides, most of the preceding studies did not focus on the elderly population with depression. Therefore, it was necessary to conduct a comparative analysis of the most widely used antidepressant with respect to their incidence of nausea among the senile depression patients in China. In the present study, a network meta-analysis (NMA) was conducted to combine both direct and indirect published evidence in order to provide ranking of the incidence of SSRIs-induced nausea, in addition, a NMA to compare the efficacy of SSRIs among the aged group was also conducted. so as to provide clear evidence for clinicians to make the best choice for elderly depressed patients in China.
2. Methods
2.1. Search strategy
Six electronic databases: Embase, Web of science, Pubmed, WanFang, CNKI, ChongqingWeiPu were searched for related studies from the inception of the databases up until September 2018.
Studies published only in English or Chinese language were considered. Search terms including SSRIs or Citalopram, Fluvoxamine, Floxetine, Sertraline, Paroxetine, Escitalopram, “effeacy”, “nausea”, “old patients with depression”, “depression of elder”, “depression of the elderly”, “randomized, controlled, trials”, and “China”. And the search sterms in PubMed was: “((((efficacy[MeSH Terms]) AND ((((((((Selective Serotonin Reuptake Inhibitors[Title/Abstract]) OR SSRIs[Title/Abstract]) OR Fluoxetine[Title/Abstract]) OR Paroxetine[Title/Abstract]) OR Citalopram[Title/Abstract]) OR Sertraline[Title/Abstract]) OR Fluvoxamine[Title/Abstract]) OR Escitalopram[Title/Abstract])) OR nausea) AND senile depression patients AND randomized controlled trials[MeSH Terms]”
2.2. Study selection
Studies were included in the analyses if they met the following criteria:
-
1.
randomized controlled trials (RCT), which compared induced nausea among Citalopram, Fluoxetine, Fluvoxamine, Sertraline, Paroxetine, and Escitalopram, on individuals with depression in China of age ≥60; and
-
2.
studies assessed depression using DSM-IV or DSM-V or ICD-10 or CCMD-3.
-
3.
In this research, nausea was defined an unpleasant, diffuse sensation of unease and discomfort, often perceived as an urge to vomit.
We excluded such studies that samples have been diagnosed as Peptic ulcer, stomach disease, or other associated comorbidities, because these factors can interfere with the results.
2.3. Data extraction
Two authors independently extracted relevant data from the included studies. These data consisted of name of first author, year of publication, study design, duration of treatment, number of patients, average age, and medications.
2.4. Outcome
The number of the cases treated effectively cases by SSRIs and the number of the SSRIs-induced nausea cases were considered as the outcome variable of this study.
2.5. Risk of bias assessment
Risk of bias was assessed according to the guidelines of the Cochrane reviews.[26] Two authors conducted the assessment independently on the following information: blinding, randomization, and definition of outcome. These were described as “low risk of bias”, “unclear risk of bias”, or “high risk of bias”, with respect to the degree of information integrity.
2.6. Statistical analysis
The safety of SSRI drugs were compared by means of NMA. This involved conducting a Bayesian model network meta-analysis to combine both direct and indirect evidence into 1 single comparison. Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were calculated. The heterogeneity was assessed with I2 test, with an I2 > 50% indicating the existence of heterogeneity. In addition, publication bias of articles involved was evaluated by funnel plot and confirmed using Egger test. All statistical analyses were conducted using R version 3.4.4 (R Project for Statistical Computing, Vienna, Austria). Statistical tests were considered significant when P < .05.
3. Result
3.1. Ethical approval
In this study, relevant data were extracted from previously published literatures and relevant research was carried out, which was not applicable to the provisions of ethical consent.
3.2. Study selection
The search strategy yielded a total of 645 potentially eligible RCTs. Of the 645 RCTs, 107 duplicates were removed. In addition, 464 studies were excluded after screening titles and abstracts. Then among the 79 full text studies left, 51 were ruled out for not providing the outcome of interest for this study. Finally, a total of 28[27–54] articles comprising 2246 patients were included in the analyses.
The flow chart depicting the study selection process is schematically shown in Figure 1.
Figure 1.
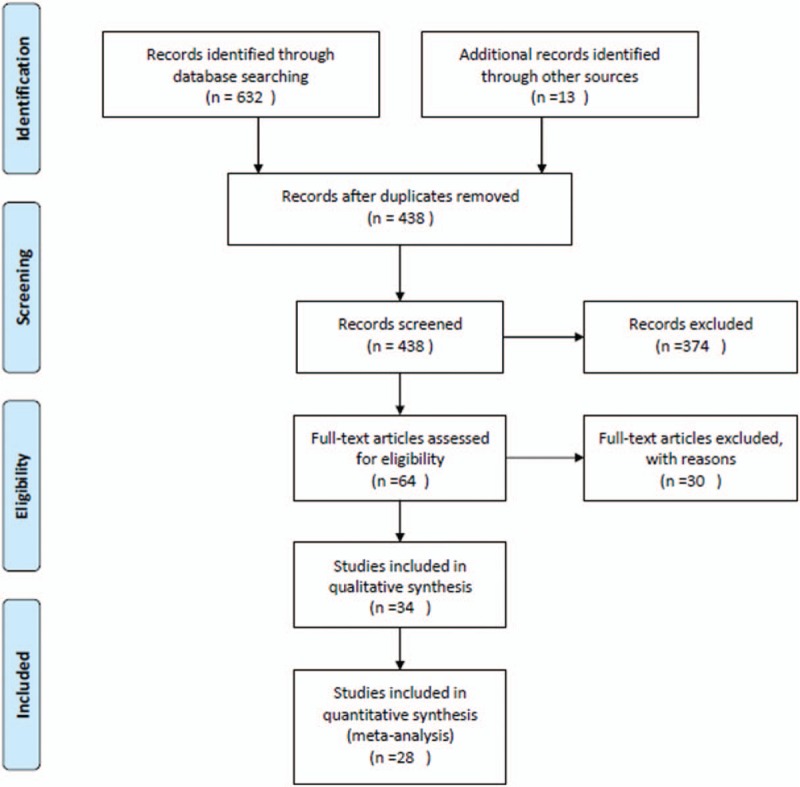
Flowchart presenting the steps of the literature search and selection.
3.3. Study characteristics
Table 1 shows a summary of study characteristics. There were 27 two-arm studies, and 1 three-arm study. Sixteen studies compared the probability of induced nausea by Paroxetine and Escitalopram, and these studies consisted of 1349 patients. Also, 3 studies compared the side effect of nausea between Escitalopram and Sertraline; whereas other 2 studies compared the same between Paroxetine and Citalopram; 1 study between Sertraline and Fluoxetine; and 1 study between Fluoxetine and Fluvoxamine. Collectively, the included studies comprised 2246 elderly depression patients from China, among whom, 920(40.96%) received treatment of Escitalopram, 193 (8.59%) received Citalopram, 151(6.72%) received Fluoxetine, 823(36.64%) received Paroxetine, and 198 (8.82%) received the treatment of Sertraline. The risk of bias assessment of included studies were shown in Table 2. Network plots of effect was shown in Figure 2, network plots of caused-nausea was shown in Figure 3.
Table 1.
The basic information and data of all included studies in the meta-analysis.
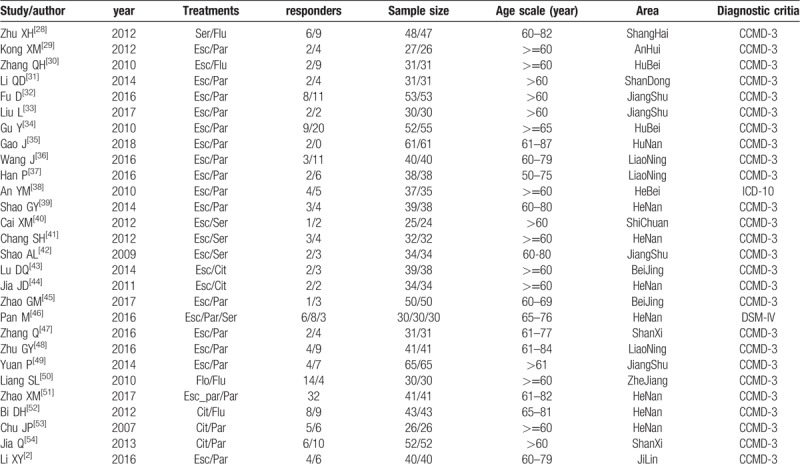
Table 2.
Risk of bias assessment. L indicated low risk, H: high risk, U: unclear risk.
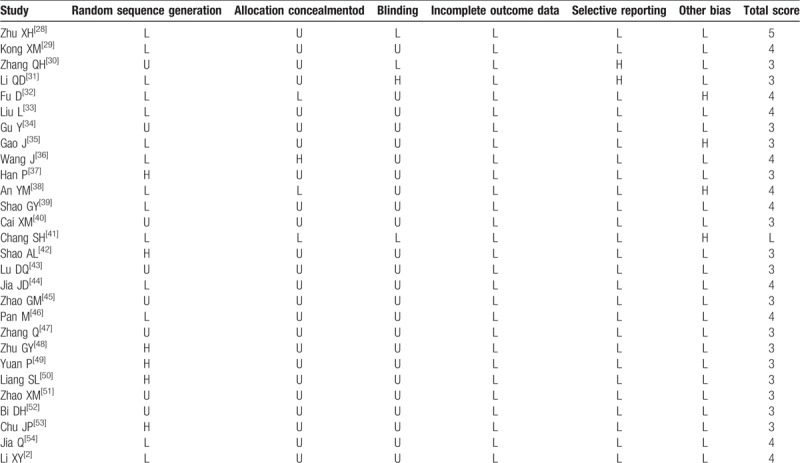
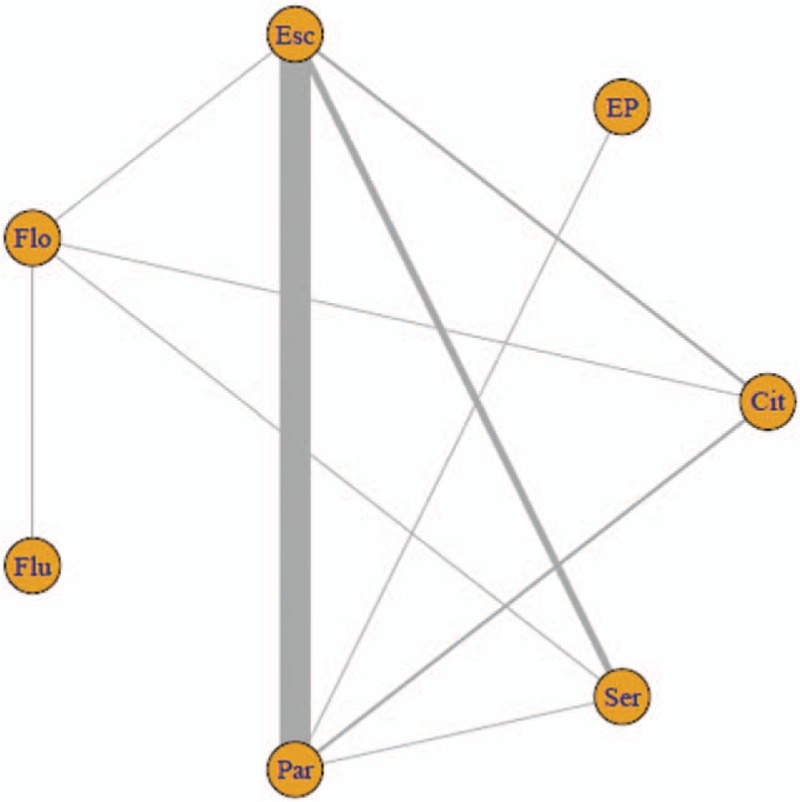
Figure 2.
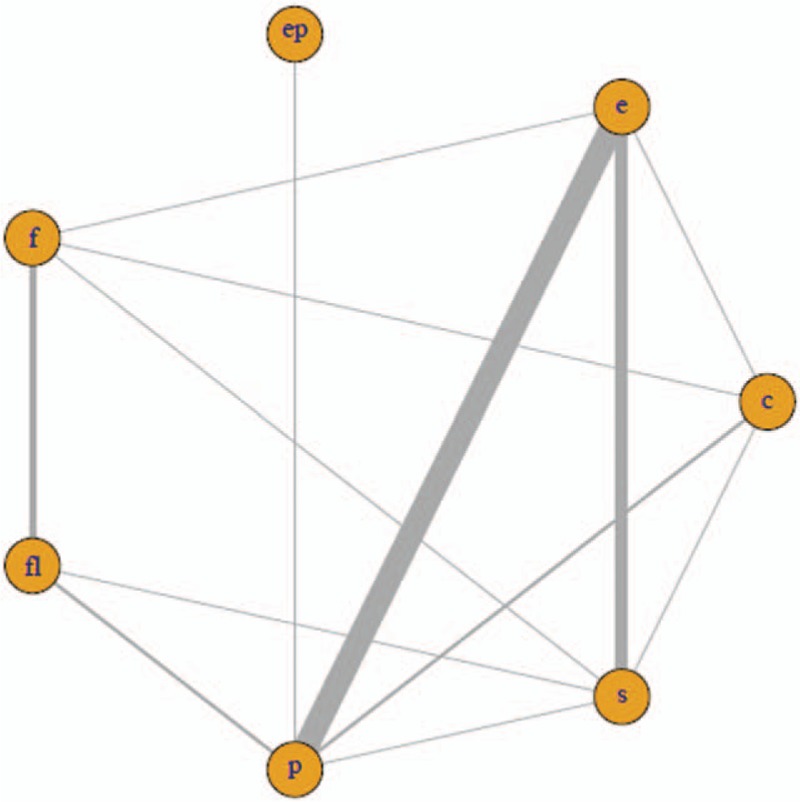
Network plots of SSRIs. The width of the lines represents the total number of trials for each comparison. C indicated Citalopram, F: Fluoxetine, S: Sertraline, P: Paroxetine, E: Escitalopram.
Figure 3.
Network plots of SSRIs. The width of the lines represents the total number of trials for each comparison. Cit indicated Citalopram, Flo: Fluvoxamine, Ser: Sertraline, Par: Paroxetine, Esc: Escitalopram, Flu: Fluvoxamine. EP: combination of Escitalopram and Paroxetine.
3.4. Efficacy of SSRIs
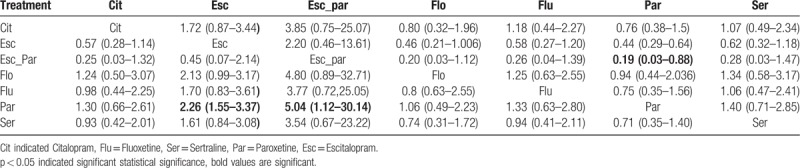
As shown in Table 3, the efficacy (response rate) of combined of Escitalopram and Paroxetine has significant superiority over Paroxetine alone, the OR and 95% CI were 5.04 (1.12–30.14), On the other hand, Escitalopram was also associated with a higher response rate compared with Paroxetine (OR = 2.26, 95%CI = 1.55–3.37). Among other comparisons, the alternative hypothesis can not be accepted duo to the confidence intervals of the OR include the 1.
Table 3.
Results of effcacy among SSRIs from network meta-analysis.
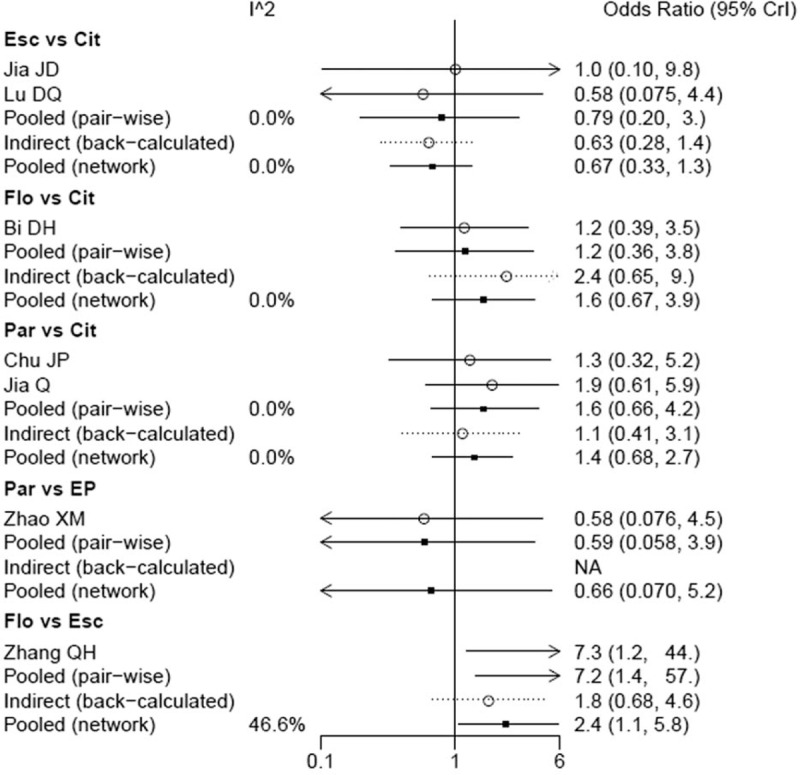
3.5. Incidence of induced nausea
As shown in Table 4, Escitalopram showed a significant decline in the incidence of caused nausea compared to Paroxetine (OR = 0.49, 95%CI = 0.34–0.69). And Escitalopram also showed a significant decline in the incidence of nausea reaction compared to Fluoxetine (OR = 0.42, 95%CI = 0.18–0.96); On the other hand, Fluvoxamine was associated with a lower risk of nausea reaction compared with Fluoxetine (OR = 0.16, 95%CI = 0.03–0.62). Among other comparisons, the alternative hypothesis can not be accepted duo to the confidence intervals of the OR include the 1. The forest plot of network results were illustrated in Figure 4.
Table 4.
Results of SSRIs for the incidence of induced-nausea from network meta-analysis.
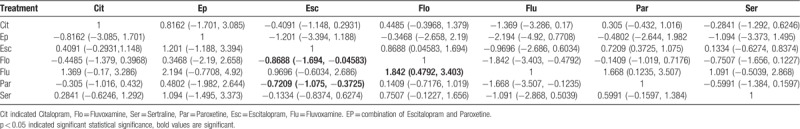
Figure 4.
The forest plot of network results on the incidence of nausea. Cit indicated Citalopram, Flo: Fluvoxamine, Ser: Sertraline, Par: Paroxetine, Esc: Escitalopram, Flu: Fluvoxamine. EP: combination of Escitalopram and Paroxetine.
3.6. The ranks of SSRIs-induced nausea
The Bayes model was used in this study, which has an advantage of providing ranks for the different drugs analyzed in terms of their severity as regards to the number of nausea cases caused. The ranking diagram and rank probability were shown in Table 5 and Figure 5. The drugs were ranked according to the number of induced-nausea cases from more to less, and the larger the number was, the safety of the drug indicated poor.
Table 5.
Rank probability of caused nausea among SSRIs.
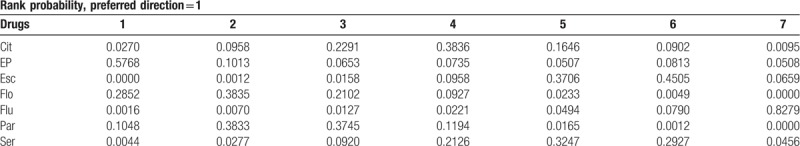
Figure 5.
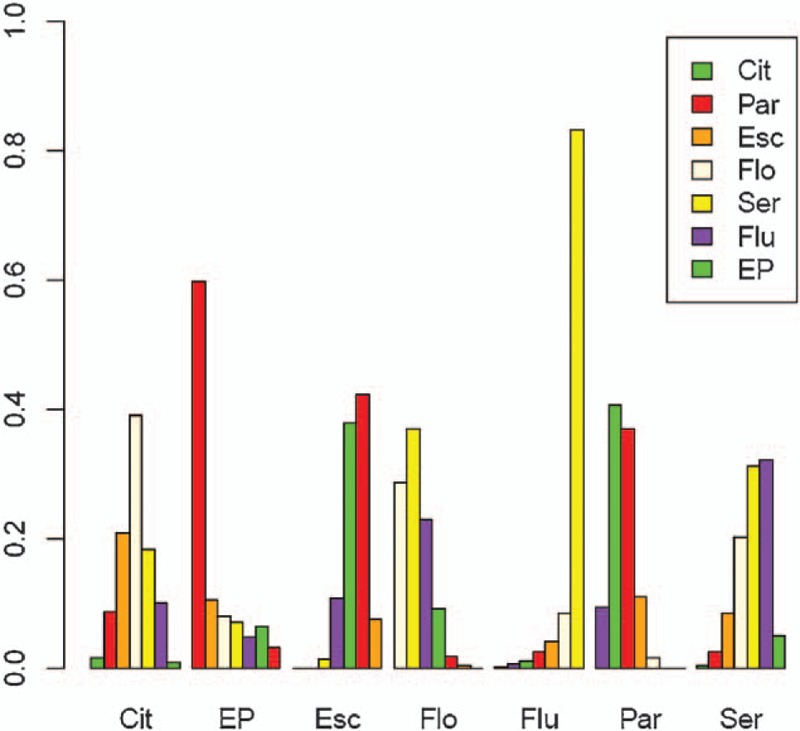
Probabilistic ranking of induced nausea among Chinese senile depression patients, Cit indicated Citalopram, Flo: Fluvoxamine, Ser: Sertraline, Par: Paroxetine, Esc: Escitalopram, Flu: Fluvoxamine. EP: combination of Escitalopram and Paroxetine.
Thus, the descending order, with respect to the probability of inducing nausea, is given as follows: Paroxetine and Escitalopram (probability = 0.58), Fluoxetine (probability = 0.29), Paroxetine (probability = 0.1), and Escitalopram (probability = 0.00). So, Escitalopram exhibited the best reliable performance in comparison with other medications.
3.7. Heterogeneity, consistency, and publication bias
According to the result which displayed in Figure 6, there was no significant heterogeneity among the included studies.
Figure 6.
The heterogeneity of the included studies, Cit indicated Citalopram, Flo: Fluvoxamine, Ser: Sertraline, Par: Paroxetine, Esc: Escitalopram, Flu: Fluvoxamine. EP: combination of Escitalopram and Paroxetine.
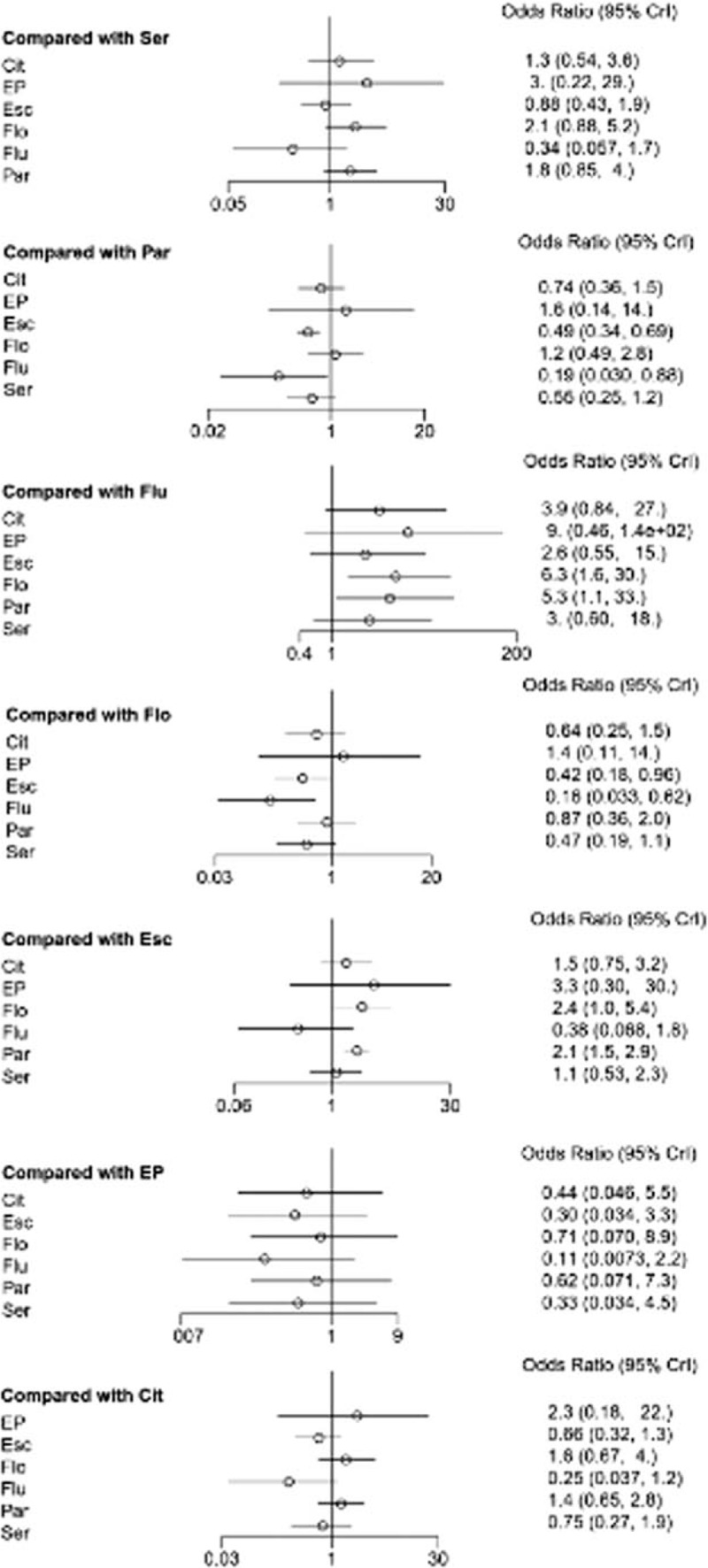
The node-splitting method was used to assess the consistency of direct and indirect evidences, the forest plots was shown in Figure 7. A P value of less than .05 suggests potentially significant inconsistency, the detail result also could be seen in Table 6, there were no significant difference was observed in the present study. The results of publication bias analyses are presented in Figure 8. There was no significant publication bias among the included studies. Thus, the validity and credibility of this meta-analysis was confirmed.
Figure 7.
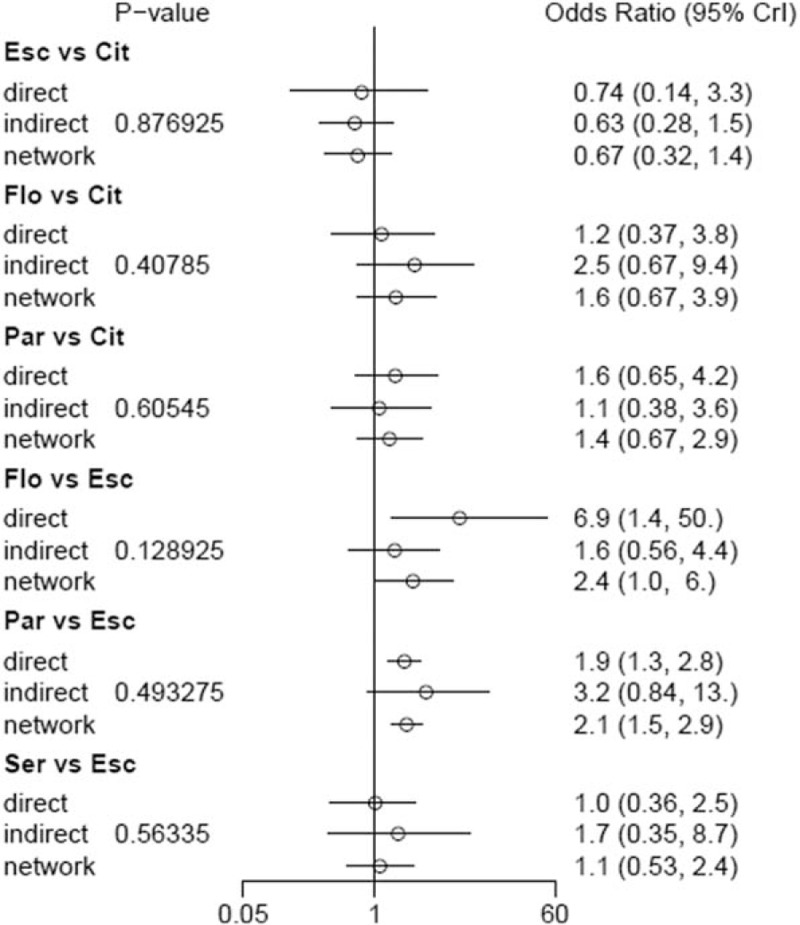
Summarized results of direct and indirect comparisons between different SSRIs. Cit indicated Citalopram, Flo: Fluvoxamine, Ser: Sertraline, Par: Paroxetine, Esc: Escitalopram, Flu: Fluvoxamine. EP: combination of Escitalopram and Paroxetine.
Table 6.
Results of consistency analysis by node-splitting plot.
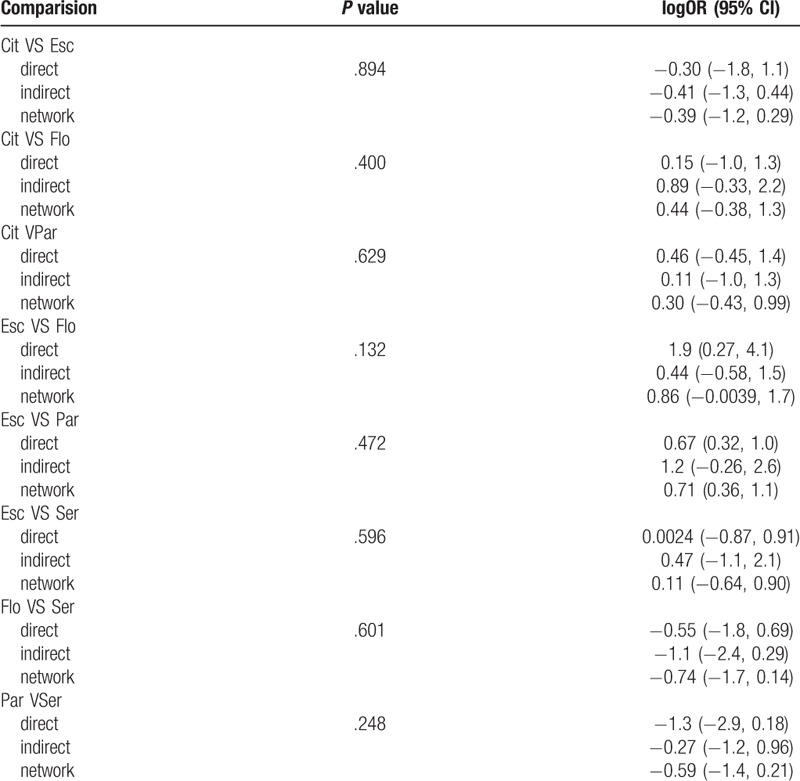
Figure 8.
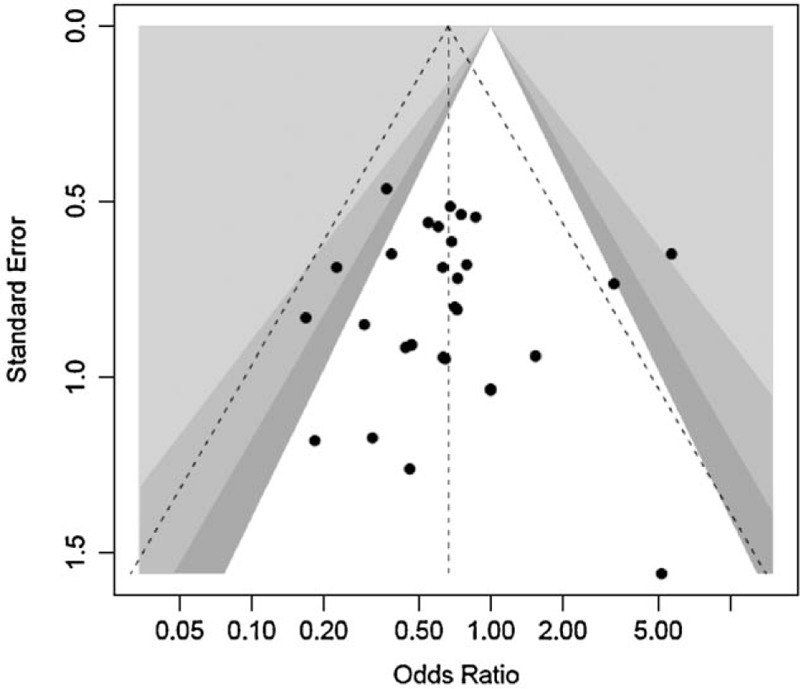
Funnel plot of publication bias.
4. Discussion
In China, depression has become the third leading cause of disease burden,[15] and some studies indicated that the prevalence of depression among the elderly in this country will keep increasing rapidly in the future.[2]
However, drug adherence of senile depression patients in China was very low.[55] The effectiveness and side effects of antidepressants can affect compliance, a previous study has analyzed the cardiovascular side effects of these drugs on depressed elderly people in China,[56] however, nausea was also a common side effect of antidepressants, which could be among the leading causes of poor compliance to medications.[57] SSRIs have a high risk of nausea in older people.[58,59] Taking Fluvoxamine, for example, the drug causes nausea more than 49% of the time.[60] Although a previous review concluded that second-generation antidepressants are equally effective, however, their side effects may vary differently.[61]
The mechanism of SSRIs-induced nausea is very complicated. Uda et al[62] suggested that SSRI-induced nausea may be associated with Serotonergic hyperactivity, while Yoshida et al[63] suggested that the genetic polymorphism of MAOA-VNTR might play an important role in the process of inducing nausea. However, the mechanisms described by the preceding studies need to be further validated.
Preventing antidepressants’ side effects among senile depression patients in China has been considered as an important task by clinicians.
For a long time, SSRIs have been the most prescribed antidepressants in China to different groups. In this study, pairwise meta-analysis and network meta-analysis showed that, compared with other SSRI drugs, Escitalopram was associated with a reduced risk of nausea. With respect to drug safety, a previous study held the viewpoint that there was no significant difference between Escitalopram and Citalopram,[61] while another study[64] proved that Escitalopram was better in terms of safety when compared with Citalopram, which is also consistent with the present study.
In addition, this study showed that the combination of EP has the highest risk of nausea, and the rank probability of drugs was successively Escitalopram, Sertraline, Fluvoxamine, Citalopram, Fluvoxamine, and Paroxetine.
This is the first comparative study on the efficacy and gastrointestinal side effects (nausea) of SSRIs in depressed elderly people in China. The findings of the present study may provide valuable information for enhancing the mental health status of the elderly who have depression. Besides, they may be beneficial to interventions aimed at reducing the burden of depression among the elderly in this country. However, some limitations need to be considered when interpreting the results of this study. First, though we had conducted a thorough literature search, all included studies still were published in Chinese, which may be exist public bias. Second, drug safety was not a predefined outcome, and therefore may not have been accurately evaluated, and among the included studies, some of them used 2 diagnostic criteria, ICD-10 and CCMD-3, which may influence the results. Third, significant variations existed with respect to the number of studies for each comparison. For example, 9 studies compared the efficacy of Paroxetine and Escitalopram, only 1 compared Paroxetine and Fluoxetine, and only 1 compared Escitalopram and Sertraline. So, this may result in wide confidence intervals for summary statistics.
In summary, the combination of Escitalopram and Paroxetine had the biggest efficacy probability, Escitalopram was also associated with a better efficacy compared with Paroxetine, and the efficacy (response rate) of combined of Escitalopram and Paroxetine has significant superiority over Paroxetine alone.
In terms of efficacy safety, Escitalopram exhibited the least probability of inducing nausea when used in the Chinese senile depression patients. Additionally, Sertraline showed the second least probability of caused nausea, while Fluoxetine exhibited the highest probability of inducing nausea among the Chinese senile depression patients.
Acknowledgments
The authors thank all the reviewers for their helpful comments.
Author contributions
Conceptualization: Shengyu Guo.
Funding acquisition: Shengyu Guo, Xi jun Pei.
Methodology: Shengyu Guo, Yan Yang.
Software: Yan Yang.
Supervision: Feiyue Liu.
Writing – original draft: Shengyu Guo.
Writing – review & editing: Feiyue Liu, Xi jun Pei.
Footnotes
Abbreviations: CIs = confidence intervals, CNKI = China National Knowledge infrastructure, DSM = Diagnostic and Statistical Manual of Mental Disorders, ICD = international classification of diseases, NICE = National Institute for Health and Care Excellence, NMA = network meta-analysis, ORs = odds ratios, SSRIs = Selective Serotonin Reuptake Inhibitors.
How to cite this article: Guo S, Yang Y, Pei Xj, Liu Fy. Comparative risk of Selective Serotonin Reuptake Inhibitors (SSRIs)-induced nausea among Chinese senile depression patients: A network meta-analysis of randomized-controlled trials. Medicine. 2020;99:7(e19133).
This work was supported by China social science fund (Number: 17BSH059); Education fund of Hunan Province (Number:18B409, http://jyt.hunan.gov.cn/sjyt/xxgk/tzgg/201903/t20190318_5297301.html).
The authors have declared that no competing interests exist.
References
- [1].Chan SW, Chiu HF, Chien WT, et al. Quality of life in Chinese elderly people with depression. Int J Geriatr Psychiatry 2010;21:312–8. [DOI] [PubMed] [Google Scholar]
- [2].Chen R, Wei L, Hu Z, et al. Depression in older people in rural China. Arch Intern Med 2005;165:2019–25. [DOI] [PubMed] [Google Scholar]
- [3].Chen R, Hu Z, Qin X, et al. A community-based study of depression in older people in Hefei, China--the GMS-AGECAT prevalence, case validation and socio-economic correlates. Int J Geriatr Psychiatry 2010;19:407. [DOI] [PubMed] [Google Scholar]
- [4].Zhibao W, Tieshan S, Guoping L. Regional differences and evolutions of population aging in China. Popul Res 2013;37–42. [Google Scholar]
- [5].Liu L. China's population trends and their implications for fertility policy. Asian Popul Stud 2010;6:289–305. [Google Scholar]
- [6].Wang XZ, Zhang P, Wang YS, et al. Clinical effect and safety of carvedilol in elderly patients with diabetes mellitus and chronic heart failure. J Guangdong Med Coll 2008;9:135–6. [Google Scholar]
- [7].Gorp FV, Whyte IM, Isbister GK. Clinical and ECG effects of escitalopram overdose. Ann Emerg Med 2009;54:404–8. [DOI] [PubMed] [Google Scholar]
- [8].Jan Sundquist. Depression and your heart link between depression, coronary heart disease mental health and psychiatry news. Depression and your heart: link between depression, coronary heart disease. Cancer 2005;11: [Google Scholar]
- [9].Bogner HR, de Vries HF. depression, hypertension. Ann Fam Med 2008;6:295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Prestele S, Aldenhoff J, Reiff J. The HPA-axis as a possible link between depression, diabetes mellitus and cognitive dysfunction. Fortschritte der Neurologie-Psychiatrie 2003;71:24–36. [DOI] [PubMed] [Google Scholar]
- [11].Spiegel D, Giese-Davis J. Depression and cancer: mechanisms and disease progression. Biol Psychiatry 2003;54:269–82. [DOI] [PubMed] [Google Scholar]
- [12].Clark L, Dombrovski AY, Siegle GJ, et al. Impairment in risk-sensitive decision-making in older suicide attempters with depression. Psychol Aging 2011;26:321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ms RBS, Caranasos GJ. Medication compliance in the elderly. Med Clin North Am 1989;73:1551. [DOI] [PubMed] [Google Scholar]
- [14].Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Therapeut 2001;23:1296–310. [DOI] [PubMed] [Google Scholar]
- [15].Li M, Cai J, Zhang P, et al. Drug brand response and its impact on compliance and efficacy in depression patients. Front Pharmacol 2016;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Fincke BG, Miller DR, Rd SA. The Interaction of patient perception of overmedication with drug compliance and side effects. J Gen Intern Med 2010;13:182–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Veale D. National Collaborating Centre for Mental Health. Br Psychol Soc 2006;9:35–7. [Google Scholar]
- [18].Geddes JR, Cipriani A. Selective serotonin reuptake inhibitors. BMJ Br Med J 2004;329:809–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet 2018;391:1357–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Jakobsen JC, Katakam KK, Schou A, et al. Selective serotonin reuptake inhibitors versus placebo in patients with major depressive disorder. A systematic review with meta-analysis and Trial Sequential Analysis. Bmc Psychiatry 2017;17:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Brambilla P, Cipriani A, Hotopf M, et al. Side-effect profile ofFluvoxamine in comparison with other SSRIs, tricyclic and newer antidepressants: a meta-analysis of clinical trial data. Pharmacopsychiatry 2005;38:69–77. [DOI] [PubMed] [Google Scholar]
- [22].Takahashi H, Yoshida K, Ito K, et al. No association between the serotonergic polymorphisms and incidence of nausea induced by fluvoxamine treatment. Eur Neuropsychopharmacol 2002;12:477–81. [DOI] [PubMed] [Google Scholar]
- [23].Ueda N, Yoshimura R, Shinkai K, et al. Higher plasma 5-hydroxyindoleacetic acid levels are associated with SSRI-induced nausea. Neuropsychobiology 2003;48:31–4. [DOI] [PubMed] [Google Scholar]
- [24].Trindade E, Menon D, Topfer LA, et al. Adverse effects associated with selective serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis. Can Med Assoc J 1998;17:1245. [PMC free article] [PubMed] [Google Scholar]
- [25].Wilson K, Mottram P. A comparison of side effects of selective serotonin reuptake inhibitors and tricyclic antidepressants in older depressed patients: a meta-analysis. Int J Geriatr Psychiatry 2004;19:754–62. [DOI] [PubMed] [Google Scholar]
- [26].Furlan AD, Malmivaara A, Chou R, et al. 2015 updated method guideline for systematic reviews in the cochrane back and neck group. Spine 2015;40:1660–73. [DOI] [PubMed] [Google Scholar]
- [27].Zhu XH. Clinical study of sertraline andFluvoxamine in the treatment of depression in elderly patients. World Health Digestmed Periodieal 2012;9:215–1215. [Google Scholar]
- [28].Kong XM, Zhu DF, Zhang Xl, et al. The effect of escitalopram in the treatment of geriatric depression. Chin J Clin Health 2012;15:123–4. [Google Scholar]
- [29].Zhang QH, Qin S. Esdtalopram and Fluoxeline in the treatment of geriatric depression. Med Innov China 2010;7:49–51. [Google Scholar]
- [30].Li QD. A comparative study of escitalopram and Paroxetine in the treatment of geriatric depression. Guide China Med 2014;12:138–9. [Google Scholar]
- [31].Fu D. Comparison of effect and safety between escitalopram and Paroxetine among elder in China. Chin J Clin Ration Drug Use 2016;9:67–8. [Google Scholar]
- [32].Liu L. Comparative analysis of escitalopram and paroxetine in treatment of senile depression. J Syst Med 2017;8:1–3. [Google Scholar]
- [33].Gu Y, Jiang T, Guo JB, et al. Efficacy and safety of escitalopram in elderly patients with major depression: a randomized and control study. Chin Mental Health J 2010;24:445–9. [Google Scholar]
- [34].Gao J. Comparison of the efficacy of escitalopram and paroxetine in the treatment of senile depression. Chin J Clin Ration Drug Use 2018;11:67–8. [Google Scholar]
- [35].Wang J. Treatment with escitalopram and Paroxetine in the elderly: a controlled study. Chin J Mod Drug Appl 2015;12:101–2. [Google Scholar]
- [36].Han P. Effect of escitalopram and Paroxetine in the treatment of senile depression. Chin J Trauma Disab Med 2016;24:102–3. [Google Scholar]
- [37].An YM, Zhao HF, Liu YL, et al. A comparative study of escitalopram and Paroxetine in the treatment of senile depression. HeBei Med J 2011;33:711–3. [Google Scholar]
- [38].Shao GY, Liu J. Efficacy and safety of escitalopram and paroxetine in the treatment of senile patients with depression. Chin J Health Psychol 2014;22:19–20. [Google Scholar]
- [39].Cai XM, Ruan HM, Ren JD. A research of the curative effectof escitalopram and sertraline for the physical disease associated with depression in elderly. Chin J Aesth Med 2012;21:51–2. [Google Scholar]
- [40].Chang SH. Efficacy and safety of escitalopram and sertraline in the treatment of senile patients with depression. China J Health Psychol 2012;20:1296–7. [Google Scholar]
- [41].Shao AL, Liu JJ, Wu B, et al. Study of efficacy and safety of escitalopram and sertraline in the teatment of senile patients with depression. Pract Geriatr 2009;23:467–9. [Google Scholar]
- [42].Lu DQ, Xiao G, Jiang BS. Escitalopram and citalopram for female patients with geriatric depression and anxiety a razed controlled trial. China J Health Psychol 2014;22:656–8. [Google Scholar]
- [43].Jia JD, Yang JZ, Yu X, et al. Clinical study on efficacy and safety of escitalopramvs citalopram in the treatment of first-episode geriatric depression. Med J Chin People's Health 2011;23:2112–6. [Google Scholar]
- [44].Zhao GM, Lu B, Diao JH. To compare the clinical application of escitalopram and paroxetine in the treatment of senile depression with anxiety. Guide China Med 2017;15:172–3. [Google Scholar]
- [45].Pan M, Zhang SQ, Lv LX, et al. Effects of different antidepressant drug interventions on the half-year outcome of first-episode elderly patients with depression. Chin J Gerontol 2016;36:2640–3. [Google Scholar]
- [46].Zhang Q. Comparison of escitalopram and paroxetine for the treatment of senility patients. Med J Chin People's Health 2016;28:45–6. [Google Scholar]
- [47].Zhu GY. Comparison of efficacy between escitalopram and paroxetine in the senility patients. Pharmacoecon China 2016;11:45–7. [Google Scholar]
- [48].Yuan P, zhang LH, Li RH. Analysis and comparison of curative effect of escitalopram and paroxetine in the treatment of senile depression patients. China Prac Med 2014;27:11–2. [Google Scholar]
- [49].Liang SL, Cao SL, Xie WG. A comparative study of fluvoxamine andFluvoxamine in the treatment of senile depression. J Pract Med 2010;26:1620–2. [Google Scholar]
- [50].Zhao XM. To investigate the effect of escitalopram combined with Paroxetine in the treatment of senile depression. Clin J Integr Tradition Chin Western Med 2017;17:135–6. [Google Scholar]
- [51].Bi DH. Comparison of the efficacy of citalopram and fluvoxamine in the treatment of depression in elderly women. Chin J Gerontol 2012;22:5012–3. [Google Scholar]
- [52].Chu JP. Comparison of citalopram and Paroxetine in elder. China J Health Psychol 2007;15:582–3. [Google Scholar]
- [53].Jia Q. A comparative study of citalopram and Paroxetine in the treatment of senile depressive disorder. Chin Remed Clin 2013;13:914–5. [Google Scholar]
- [54].Li XY. To study the application of escitalopram and paroxetine in the treatment of senile depression. Clin Psychosom Disord 2016;5:178–9. [Google Scholar]
- [55].Mjeldemossey LA, Chi I, Lou VW. Relationship between adherence to tradition and depression in Chinese elders in China. Aging Mental Health 2006;10:19–26. s. [DOI] [PubMed] [Google Scholar]
- [56].Guo S, Chen L, Cheng S, et al. Comparative cardiovascular safety of selective serotonin reuptake inhibitors (SSRIs) among Chinese senile depression patients: a network meta-analysis of randomized controlled trials. Medicine 2019;98:e15786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Devane CL. Immediate-release versus controlled-release formulations: pharmacokinetics of newer antidepressants in relation to nausea. J Clin Psychiatry 2003;64:14–9. [PubMed] [Google Scholar]
- [58].Spigset DO. Adverse reactions of selective serotonin reuptake inhibitors. Drug Saf 1999;20:277–87. [DOI] [PubMed] [Google Scholar]
- [59].Thomas KLH, Ellingrod VL. Pharmacogenetics of selective serotonin reuptake inhibitors and associated adverse drug reactions. Pharmacoth J Hum Pharmacol Drug Ther 2012;29:822–31. [DOI] [PubMed] [Google Scholar]
- [60].Wilde MI, Plosker GL, Benfield P. Fluvoxamine. An updated review of its pharmacology, and therapeutic use in depressive illness. Drugs 1993;46:895–924. [DOI] [PubMed] [Google Scholar]
- [61].Morgan LC, Gartlehner G, Nussbaumer B, et al. Comparative benefits and harms of second-generation antidepressants in the pharmacologic treatment of depression in older adults: systematic revview and network meta-analysis. Eur Psychiatry 2015;30:774–1774. [Google Scholar]
- [62].Ueda N, Yoshimura R, Shinkai K, et al. Higher plasma 5-hydroxyindoleacetic acid levels are associated with SSRI-Induced Nausea. Neuropsychobiology 2003;48:31–4. [DOI] [PubMed] [Google Scholar]
- [63].Yoshida K, Naito S, Takahashi H, et al. Monoamine oxidase A gene polymorphism, 5-HT2A receptor gene polymorphism and incidence of nausea induced by fluvoxamine. Neuropsychobiology 2003;48:10–3. [DOI] [PubMed] [Google Scholar]
- [64].Ramsberg J, Asseburg C, Henriksson M. Effectiveness and cost-effectiveness of antidepressants in primary care: a multiple treatment comparison meta-analysis and cost-effectiveness model. Plos One 2012;7:e42003. [DOI] [PMC free article] [PubMed] [Google Scholar]


