Abstract
Objective
Examine the prevalence of sarcopenia (low muscle mass) and osteosarcopenia (low bone density and muscle mass) in older motor vehicle crash (MVC) occupants, and the relationship of these musculoskeletal conditions with age, sex, and injury.
Methods
Sarcopenia and osteopenia was assessed from abdominal computed tomography (CT) scans of 61 seriously injured MVC occupants over age 50 in the Crash Injury Research and Engineering Network (CIREN) database.
Results
The prevalence was 43% for sarcopenia, 25% for osteopenia, and 15% for osteosarcopenia in the CIREN occupants. The Injury Severity Score (ISS) was higher in those with only sarcopenia (mean ± standard error: 22.4 ± 2.3), followed by those with osteosarcopenia (17.9 ± 2.4) and only osteopenia (12.8 ± 1.5). More total fractures were observed in occupants with sarcopenia alone (7.6 ± 1.5) or osteosarcopenia (7.0 ± 2.1) compared to non-sarcopenic occupants with osteopenia (4.0 ± 2.5).
Conclusions
Sarcopenia and osteosarcopenia may be associated with more serious injuries and fractures in MVCs.
Keywords: osteopenia, muscle, computed tomography, fracture, atrophy, aging
INTRODUCTION
Sarcopenia, a geriatric syndrome characterized by progressive and generalized loss of skeletal muscle mass and strength (Cruz-Jentoft, et al., 2010), is expected to impact injury incidence and severity. The prevalence of sarcopenia over age 60 is 10%, and up to 50% over age 80 (Shefiee, et al., 2017). Since drivers age 50 and older comprise 45% of all licensed U.S. drivers (Office of Highway Policy Information, 2018), it is important to understand the effects of sarcopenia in older adult MVC trauma. Low bone mineral density (BMD) also commonly occurs with sarcopenia, termed “osteosarcopenia”, which intensifies the risk of fracture (Yu, et al., 2014). Sarcopenia and osteosarcopenia effects have not been studied specifically in MVC trauma, as previous studies have primarily focused on fall injuries. Though sarcopenia diagnosis can include loss of muscle mass, muscle strength, and/or physical function, many studies have diagnosed sarcopenia based on muscle size measured from CT (Lenchik, et al., 2018). The objective of this study is to analyze CT scans and crash, occupant, and injury data collected from seriously injured MVC occupants in the Crash Injury Research and Engineering Network (CIREN) database to examine the prevalence of sarcopenia and osteosarcopenia in MVC trauma, and the relationship of these musculoskeletal conditions with MVC occupant and injury attributes. CT assessment of sarcopenia and osteosarcopenia in MVC occupants may explain contributing factors to the causation and mechanisms of injury, and identify patients with a high risk of poor outcomes who may benefit from additional rehabilitation to preserve function.
METHODS
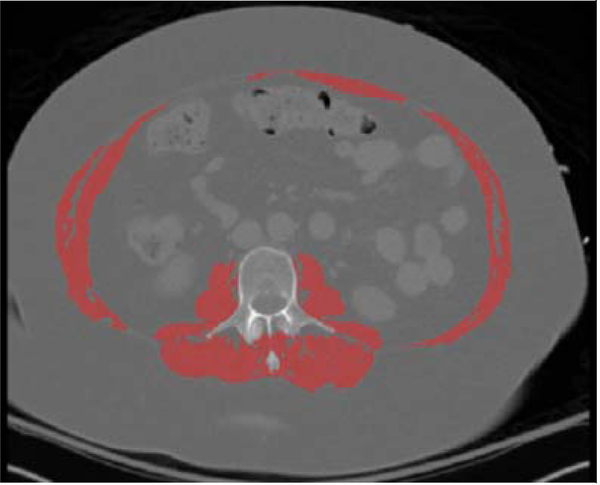
Eligibility for the CIREN study has been established as seriously injured MVC occupants of a modern vehicle (≤7 years old) who sustained at least one Abbreviated Injury Scale (AIS) 3+ or certain AIS 2+ injuries. Skeletal muscle cross-sectional area (CSA) and lumbar BMD was measured in abdominal CT scans of 61 CIREN occupants 50 years and older. All visualized muscles at the L3 vertebral level were segmented by thresholding muscle from -29 to +150 Hounsfield Units (HU) to compute the muscle CSA (Figure 1). The skeletal muscle index (SMI; Eq. 1) was used to determine the presence of sarcopenia, with thresholds defined as SMI < 52.4 cm2/m2 for men and SMI < 38.5 cm2/m2 for women (Prado, et al., 2008). A prior study obtained lumbar BMD from these CTs and established a 145 mg/cc threshold for osteopenia (Weaver, et al., 2015). Descriptive statistics, t-tests, and chi-squared tests were performed using JMP Pro 13 (SAS, Cary, NC).
Figure 1.
CT segmentation of all muscles at the L3 level for sarcopenic 69-year-old woman with 35.4 cm2/m2 SMI, below the 38.5 cm2/m2 sarcopenia cutpoint for women (Prado, et al., 2008).
| (1) |
RESULTS
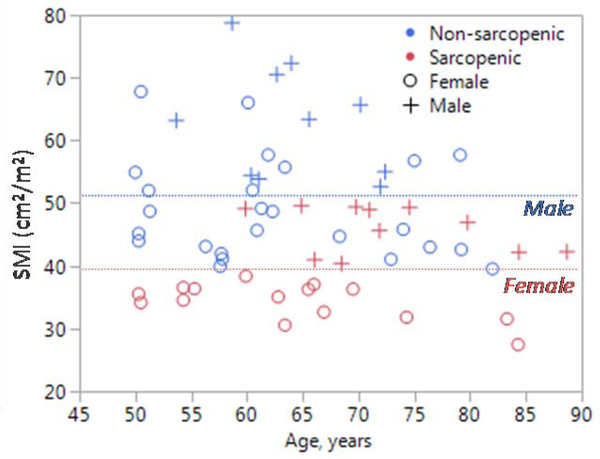
The prevalence of CT-indicated sarcopenia was 43% amongst the 61 CIREN occupants over the age of 50 (Figure 2), and increased to 45% for ages 60+ and 80% for ages 80+ (out of n=42 and n=5, respectively; Table 1). Sarcopenic occupants were slightly older, although this was not statistically significant. Sex, crash speed, crash mode, and ISS were similar between sarcopenic and non-sarcopenic occupants. On average, SMI was 17.1 cm2/m2 lower in sarcopenic males and 14.7 cm2/m2 lower in sarcopenic females, compared to their non-sarcopenic counterparts (p<0.001). Lumbar BMD was an average 20.6 mg/cc lower in sarcopenic occupants (p=0.049). Osteopenia was indicated based on CT-derived lumbar BMD for 35% of sarcopenic occupants compared to 17% of non-sarcopenic occupants, illustrating a 15% prevalence of osteosarcopenia within this CIREN cohort. A similar number of total, chest, spine, and upper extremity fractures were observed between sarcopenic and non-sarcopenic occupants; however, slightly more pelvis and lower extremity fractures were observed in non-sarcopenic occupants (p=0.027). Amongst occupants with CT-indicated sarcopenia and/or osteopenia, the average ISS was highest in those with only sarcopenia (mean ± standard error: 22.4 ± 2.3), followed by those with osteosarcopenia (17.9 ± 2.4) and only osteopenia (12.8 ± 1.5). More total fractures were observed in occupants with sarcopenia alone (7.6 ± 1.5) or osteosarcopenia (7.0 ± 2.1) in comparison to non-sarcopenic occupants with osteopenia (4.0 ± 2.5).
Figure 2.
SMI versus age for 61 CIREN occupants, with sarcopenia indicated by CT in 11 males and 15 females. Dashed lines illustrate the 52.4 and 38.5 cm2/m2 sarcopenia cutpoints for males and females (Prado, et al., 2008).
Table 1.
Characteristics of CIREN occupants with CT-indicated sarcopenia versus normal muscle mass (non-sarcopenic). Mean ± standard error is reported, unless otherwise noted. P-values were computed using t-tests for continuous variables and chi-squared tests for categorical variables.
| CT-indicated Sarcopenia | Non-sarcopenic | p-value | |
|---|---|---|---|
| N (%) | 26 (43%) | 35 (57%) | -- |
| Age, years | 68 ± 2 | 63 ± 9 | 0.088 |
| >60 years old, n (%) | 19 (45%) | 23 (55%) | -- |
| >80 years old, n (%) | 4 (80%) | 1 (20%) | -- |
| Female, n (%) | 15 (58%) | 25 (71%) | 0.265 |
| Crash speed, km/hr | 31.0 ± 2.3 | 35.7 ± 3.2 | 0.242 |
| Crash mode, n (%) Frontal | 15 (58%) | 21 (60%) | 0.857 |
| Near side | 7 (27%) | 11 (31%) | |
| Far side | 3 (12%) | 2 (6%) | |
| SMI (cm2/m2) Male | 46.0 ± 1.1 | 63.1 ± 2.8 | <0.001* |
| Female | 34.3 ± 0.8 | 49.0 ± 1.6 | <0.001* |
| Lumbar BMD, mg/cc | 163.7 ± 8.1 | 184.3 ± 6.2 | 0.049* |
| Osteopenic, n (%) | 9 (35%) | 6 (17%) | 0.118 |
| Injury Severity Score (ISS) | 20.8 ± 1.7 | 21.7 ± 1.8 | 0.730 |
| Number of Fractures | 7.4 ± 1.2 | 9.1 ± 1.1 | 0.281 |
| Chest | 4.4 ± 1.0 | 4.2 ± 0.8 | 0.878 |
| Spine | 1.2 ± 0.3 | 2.1 ± 0.6 | 0.176 |
| Upper Extremity | 0.5 ± 0.2 | 0.4 ± 0.1 | 0.629 |
| Pelvis/Lower Extremity | 1.1 ± 0.2 | 2.2 ± 0.4 | 0.027* |
DISCUSSION
The prevalence of sarcopenia amongst CIREN MVC occupants over age 60 was 45% compared to 10% for the general population (Shefiee, et al., 2017), which may suggest sarcopenic occupants are more likely to be seriously injured in a MVC. Sarcopenia and osteosarcopenia may be associated with more serious injuries and fractures in MVCs compared to osteopenia alone. This was supported by higher ISS and more total fractures in occupants with sarcopenia or osteosarcopenia, compared to those with osteopenia. However, when stratifying solely by sarcopenic status and not accounting for bone health, more pelvis and lower extremity fractures were seen in non-sarcopenic occupants. This may suggest that other risk factors in addition to sarcopenic status are needed predict injury severity and fracture incidence. Further analysis of the interplay of sarcopenia and osteopenia should be conducted in larger samples to determine if their effects on injury incidence are independent or mixed. Adjustment for potential confounders (e.g. delta-v, crash direction) may help explain these findings, but unfortunately, the small sample size of this study did not yield significant models when adjusting for these factors. The CIREN database is not nationally representative because it is limited to seriously injured MVC occupants; thus, sarcopenia and osteosarcopenia may be overrepresented in the CIREN population if these conditions predispose occupants to injury. Individuals with sarcopenia or osteosarcopenia may also have deteriorated health and greater likelihood of being admitted to a Level I trauma center, further elevating the prevalence of these disorders in CIREN MVC occupants. Larger and nationally representative samples including non-injured, minimally injured, and severely injured occupants are needed to fully explore the effects of these musculoskeletal conditions in MVC trauma. While such studies would provide more insight on the interplay between crash mechanics, sarcopenia, and osteopenia, the results of the current study suggest this may be an important area to investigate further given that the prevalence of sarcopenia in 60+ year olds is 4.5-fold higher in CIREN compared to the general population.
ACKNOWLEDGEMENTS
Funding was provided by NHTSA (DTNH2217R00069) and NIH (K25AG058804). Views expressed are those of the authors and do not represent the views of the sponsors.
REFERENCES
- 1.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis. Age and Ageing. 2010;39:412–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lenchik L, Boutin RD. Sarcopenia: Beyond Muscle Atrophy and into the New Frontiers of Opportunistic Imaging, Precision Medicine, and Machine Learning. Semin Musculoskelet Radiol. July 2018;22(3):307–322. [DOI] [PubMed] [Google Scholar]
- 3.Office of Highway Policy Information. Highway Statistics 2017. Washington, DC: Federal Highway Administration;2018. [Google Scholar]
- 4.Prado CMM, Lieffers JR, McCargar LJ, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. The Lancet Oncology. 2008;9:629–635. [DOI] [PubMed] [Google Scholar]
- 5.Shefiee G, Keshtkar A, Saoltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord. 2017;16(21). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weaver AA, Beavers KM, Hightower RC, Lynch SK, Miller AN, Stitzel JD. Lumbar Bone Mineral Density Phantomless Computed Tomography Measurements and Correlation with Age and Fracture Incidence. Traffic Inj Prev. 2015;16 Suppl 2(sup2):S153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu R, Leung J, Woo J. Incremental predictive value of sarcopenia for incident fracture in an elderly Chinese cohort: results from the Osteoporotic Fractures in Men (MrOs) Study. J Am Med Dir Assoc. 2014;15(8):551–558. [DOI] [PubMed] [Google Scholar]