Abstract
INTRODUCTION
Contextual factors representing chronic stressors, such as neighborhood crime characteristics, have been repeatedly linked to compromised mental and physical health, and may contribute to the pathologizing of normative/non-clinical experiences. However, the impact of such structural factors has seldom been incorporated in Clinical High Risk (CHR) for psychosis research. Understanding how context can influence the presence or severity of symptoms such as suspiciousness/paranoia may have important relevance for promoting valid and reliable assessment, as well as for understanding ways in which environment may be related to illness development and expression.
METHODS
A total of 126 adolescents and young adults (nCHR = 63, ncontrol= 63) underwent clinical interviews for Clinical High-Risk syndromes. Neighborhood crime indices and socioeconomic status were calculated through geocoding and extracting of publicly available Census and Federal Bureau of Investigation (FBI) data. Analyses examined presence of associations between neighborhood crime indices, socioeconomic status, suspiciousness and total symptoms.
RESULTS
Greater neighborhood crime was related to increased suspiciousness in CHR individuals, even after controlling for neighborhood socioeconomic status, r = 0.27, p = 0.03. Neighborhood crime was not related to total symptoms, and neither was neighborhood socioeconomic status.
DISCUSSION
Results suggest neighborhood crime uniquely related to suspiciousness symptoms in CHR individuals, while this was not the case for healthy volunteers (HV). Future work will be critical for determining the extent to which assessors are pathologizing experiences that are normative for a particular context, or rather, if a stressful context is serving as a sufficient environmental stressor to unmask emerging psychosis.
Keywords: neighborhood crime, crime, socioeconomic status, neighborhood income, clinical high risk, psychosis, suspiciousness, paranoia, schizophrenia, neighborhood, contextual factors
Introduction
Inclusion of contextual or structural factors (such as socioeconomic status, neighborhood characteristics, policy or educational structures) in models of psychopathology allows for a richer understanding of mental illness that goes beyond individual level determinants (Evans et al., 2013). Structural components such as crime in an individual’s neighborhood are relatively unexplored vulnerability factors for developing psychopathology, particularly in those fields of study where evidence is newly emerging. This is the case for research on youth at Clinical High Risk (CHR) of developing a psychotic disorder, who experience attenuated positive symptoms of psychosis and accompanying functional decline or distress (Cannon et al., 2008). A CHR symptom domain that could be particularly sensitive to these contextual factors is suspiciousness/paranoid thinking and ideation (e.g. living in a dangerous neighborhood could lead to wariness and maybe even suspicious thinking). Current research requires replication in differing samples and geographic settings, as well as case-control comparisons. Further, it is unclear whether the effects of neighborhood crime characteristics are distinguishable from other structural vulnerability factors such as socioeconomic status (Smith and Jarjoura, 1988). Identifying specific contextual factors such as neighborhood crime, which could impact symptom presentation and assessment, is critical for informing preventive and intervention efforts, as well as for understanding the etiological underpinnings of psychotic disorders.
Research on predictors of risk for developing psychosis has often emphasized individual level factors such as genetic risk, cognitive function, and premorbid functioning (Ciarleglio et al., 2018; Nelson et al., 2018). With some exceptions, structural level factors such as crime exposure at the neighborhood level have gone relatively unexplored, despite compelling evidence suggesting that these factors have an impactful influence on both physical and mental illness (Draine et al., 2002; Miller et al., 2018; Theall, 2017). A neural-diathesis conceptualization of psychosis posits that a predisposing biological or genetic vulnerability can be exacerbated by one or multiple “hits” in the form of acute or chronic stressors, thus triggering the onset of psychopathology (Corcoran et al., 2003; Jones and Fernyhough, 2006; Walker et al., 2008; Walker and Diforio, 1997). Among structural-level factors that could constitute “hits”, research has linked exposure to crime, income inequality, and neighborhood deprivation to increased risk of developing a psychotic disorder (Bhavsar et al., 2014; Boydell et al., 2004; Burns et al., 2014; Lasalvia et al., 2014; Miller et al., 1999; van Os et al., 2010; Zammit et al., 2010). Specifically, living in a high crime environment could instill exposure to multiple risk factors, which could accumulate as chronic and acute stressors, eventually affecting an individual’s physical and mental health (Bauman et al., 2006; Brody et al., 2013; Evans and Cassells, 2014; Evans et al., 2013). Thus, incorporating the contextual perspective could likely be essential for informing neural-diathesis predictive models of psychosis in CHR individuals.
It is estimated that at least 10–15% of the general population regularly experiences paranoid, suspicious or persecutory thoughts (Freeman, 2007). Suspiciousness has also been found to be the most commonly reported psychotic-like experience (PLE) (Morgan et al., 2009). There is evidence that suggests exposure to crime could particularly relate to the suspiciousness/paranoid CHR symptom domain (Freeman, 2007; Morgan et al., 2009; Wilson et al., 2016). Living in a high crime neighborhood could be associated with suspiciousness and paranoia (Brody et al., 2013; Evans and Cassells, 2014; Wilson et al., 2016). Further, studies have found that exposure to crime can predict occurrence of psychosis (Bhavsar et al., 2014). Proposed mechanisms include experiences of threat (Bebbington et al., 2004) or social defeat (Selten and Cantor-Graae, 2007) increasing likelihood of paranoia (Bhavsar et al., 2014; Boydell et al., 2004; Zammit et al., 2010).
It is not clear if the link between exposure to crime and suspiciousness is strictly a contextual response, if crime exposure can be an environmental trigger increasing susceptibility towards psychosis, or both. One could argue that adaptiveness and effect on functioning is most important when conceptualizing whether suspiciousness is reaching significant levels of clinical symptomatology. However, assessing for suspiciousness/paranoid symptoms in CHR individuals without taking factors such as neighborhood crime levels into proper account could also easily lead to mis-diagnosis in a field already plagued by high false-positive rates of prediction to transition to a psychotic disorder (Fusar-Poli et al., 2012; Yung et al., 2007). To our knowledge, only one investigation has explored neighborhood crime and suspiciousness/paranoia in CHR individuals (Wilson et al., 2016). This study recruited a majority African American CHR sample in the Baltimore area to examine the relations between crime and suspiciousness, finding greater neighborhood crime predicted greater suspiciousness symptoms in CHR individuals over and above other psychosis risk symptoms.
While these results are highly informative, it is unclear whether this association is geographically specific, or sample-specific. Replication is needed in regions with varying average crime levels, as well as in differing populations, which was this study’s first aim. Further, while Wilson et al. brought to light an important association between suspiciousness and neighborhood crime, specificity was not established with regards to other neighborhood level factors that could be highly related to crime levels, such as socioeconomic status (Evans and Kim, 2010). While factors such as socioeconomic status at the neighborhood level are also hypothesized to be sources of chronic stress, one could expect crime specifically to relate to suspiciousness/paranoia, given the nature of the symptom cluster (e.g. “do you often feel that you have to pay close attention to what’s going on around you in order to feel safe?” (Miller et al., 1999; Nelson et al., 2018). However, this has not been investigated, and is an important point given that different contextual considerations could be indicated if these relations are not specific to crime; thus, this is the present study’s second aim. Lastly, comparisons with healthy volunteers (HV) have not been undertaken, and would be informative with regards to whether an effect is observable beyond clinical groups; this is the third aim of the investigation. It was hypothesized that results would mirror those found by Wilson et al. 2016, and that the association would remain after controlling for neighborhood socioeconomic status (despite an expected strong association between neighborhood crime and socioeconomic status). Further, it was hypothesized that neighborhood socioeconomic status would be associated with total positive symptoms, and not with suspiciousness symptoms, lending evidence for specificity of the association. Lastly, it was hypothesized that the association would be observable in both healthy and CHR individuals.
Method
Participants
The sample comprised 126 participants (n = 63 CHR, n = 63 HV) who were adolescents and young adults recruited from 2012–2016 to the University of Colorado Boulder’s Adolescent Development and Preventive Treatment (ADAPT) program (Table 1). CHR and HV individuals 16–24 years of age were recruited through newspaper ads, Craigslist, e-mail postings, and community professional referrals. CHR participant inclusion required meeting the Structured interview for Psychosis-Risk syndromes (SIPS) criteria for a clinical high-risk syndrome (Miller et al., 1999). Criteria for a psychosis risk syndrome included one or more of the following: progression of recent onset of attenuated positive symptoms, presence of a first-degree relative with a psychotic disorder along with a recent decline in global functioning, or a decline in global functioning with the presence of schizotypal personality disorder. HV were included given they did not meet criteria for a psychosis risk syndrome, and given that they did not endorse presence of a psychotic disorder in a first degree relative. In addition, exclusion criteria for both groups included head injury, presence of a neurological disorder, lifetime substance dependence, and presence or lifetime history of an Axis I psychotic disorder. Informed consent was given by all adult participants. In the case that a participant was younger than 18 years old, the parent gave written informed consent in addition to the participant. Study procedures were approved by Institutional Review Boards of the University of Colorado Boulder and Northwestern University.
Table 1.
Demographic Characteristics.
| HV n = 63 (1) | CHR n = 63 (2) | Group Diff. | |
|---|---|---|---|
| Demographics | |||
| Sex (Female/Male) | 35/28 | 25/38 | 1 = 2 |
| Age Mean (SD) | 18.14 (2.71) | 18.56 (1.81) | 1 = 2 |
| Race | 1 = 2 | ||
| First Nations Count (%) | 2 (3.2%) | 5 (7.9%) | |
| East Asian Count (%) | 4 (6.3%) | 2 (3.2%) | |
| Southeast Asian Count (%) | 1 (1.6%) | ||
| Black Count (%) | 2 (3.2%) | 1 (1.6%) | |
| Central/South American Count (%) | 14 (22.2%) | 11 (17.5%) | |
| West/Central Asia, Middle East Count (%) | 2 (3.2%) | 1 (1.6%) | |
| White Count (%) | 38 (60.3%) | 43 (68.3%) | |
| Hispanic (no/yes) | 47/16 | 48/15 |
Clinical Interviews
The SIPS was administered to generate attenuated positive symptom scores, diagnose psychosis and psychosis-risk syndromes, and designate CHR status (McGlashan et al., 2010; Miller et al., 1999). The SIPS rates severity of symptoms on a 7-point Likert-type scale. Positive symptoms are rated absent (0) to psychotic (6). Positive symptoms include Unusual Thought Content/Delusional Ideas, Suspiciousness/Persecutory Ideas, Grandiose Ideas, Perceptual Abnormalities/Hallucinations, and Disorganized Communication. Sum scores were used to quantify positive and negative symptoms (see Table 2, Supplementary Tables 1, 2). Participants were also administered the Structured Clinical Interview for DSM-IV Axis I disorders (SCID) (First and Gibbon, 2004). The SCID was used to rule out a psychosis diagnosis for CHR individuals, as well as to assess history of mood and anxiety disorders. Interviews were conducted by trained clinical psychology doctoral students; Kappas of at least .8 for SIPS and .9 for psychosis-risk and psychiatric diagnoses were obtained.
Table 2.
Positive Symptoms and Crime Characteristics.
| CHR | ||||
|---|---|---|---|---|
| Variable | Range | Mean (SD) | Skew (SE = 0.30) | Kurtosis (SE = 0.60) |
| P1: Unusual Thought Content | 0–5 | 3.37 (1.20) | −0.99 | 0.86 |
| P2: Suspiciousness/Paranoia | 0–5 | 2.65 (1.60) | −0.11 | −1.19 |
| P3: Grandiosity | 0–5 | 1.62 (1.58) | 0.46 | −1.03 |
| P4: Perceptual Abnormalities | 0–5 | 2.67 (1.39) | −0.71 | −0.47 |
| P5: Disorganized Thinking | 0–5 | 1.83 (1.50) | 0.37 | −0.87 |
| Sum P (minus P2) | 0–17 | 9.48 (3.83) | −0.24 | 0.13 |
| Neighborhood Total Crimea | 10–201 | 74.94 (43.02) | 0.64 | 0.23 |
| Neighborhood Median Family Incomeb | 40,250–181,250 | 111,993.35 (27,718.77) | −0.48 | 0.30 |
| Healthy volunteers | ||||
| Variable | Range | Mean (SD) | Skew (SE = 0.30) | Kurtosis (SE = 0.60) |
| P1: Unusual Thought Content | 0–2 | 0.11 (0.41) | 3.86 | 14.72 |
| P2: Suspiciousness/Paranoia | 0–1 | 0.14 (0.35) | 2.09 | 2.45 |
| P3: Grandiosity | 0–2 | 0.11 (0.36) | 3.51 | 12.87 |
| P4: Perceptual Abnormalities | 0–2 | 0.13 (0.46) | 3.64 | 12.29 |
| P5: Disorganized Thinking | 0–1 | 0.06 (0.25) | 3.67 | 11.83 |
| Sum P (minus P2) | 0–5 | 0.41 (1.03) | 2.70 | 7.16 |
| Neighborhood Total Crimea | 8–208 | 100.62 (51.18) | 0.46 | −0.72 |
| Neighborhood Median Family Incomeb | 40,250–154,453 | 106,103.16 (32,414.53) | −0.44 | −0.94 |
Standardized such that a score of 100 indicates crime levels are at the U.S national average level.
In the past 12 months, in 2016 inflation-adjusted dollars.
Neighborhood Variables
Participant addresses were collected and geo-coded into X and Y coordinates on a private server using ArcGIS software. The geocoded locations were then used to extract variables at the tract level for each individual. Applied Geographic Solutions computes a Total Crime Index (TCI) using yearly crime data that local police departments supply to the Federal Bureau of Investigation (FBI). This index is current and calculated at the tract level, which comprises 2500–8000 individuals (average of 4000) defined by the U.S. Census. The validity of crime indices calculated in this manner has been demonstrated in studies of violence and health in adults (Miller et al., 2018; Theall, 2017; Theall et al., 2012). The total crime index includes murder, personal crime, rape, assault, property crime, burglary, larceny, and motor vehicle theft. The TCI is scaled such that a value of 100 represents a neighborhood with crime rates at the national average. In order to test specificity of the effect of crime controlling for socioeconomic variables (Smith and Jarjoura, 1988), median family income at the tract level was also extracted, derived from publicly available U.S. Census data averaged from 2012 to 2016 using IPUMS NHGIS (https://www.nhgis.org), which publishes averages from 2012 to 2016.
Statistical Analyses
All analyses were estimated using SPSS version 25. Independent samples t tests and chi-square tests of independence, where appropriate, were used to examine differences in demographic characteristics (age, gender, race) between CHR and HV groups. Z tests were used (Skewness/SEskewness and Kurtosis/ SEkurtosis) to evaluate normality of continuous variables, with z values of > |1.99| considered to be evidence of non-normal distributions, given current sample size (Kim, 2013). Given evidence of non-normality in TCI for CHR individuals, and in symptoms for HV (see Table 2), non-parametric tests were used. Spearman correlations were run between outcome variables and predictor variables (including TCI, median family income at the neighborhood level, P2 symptoms, and total symptoms excluding P2; see Table 3). Partial correlations were also run between symptoms (P2 and total symptoms excluding P2) and TCI controlling for median family income at the neighborhood level. These analyses were run separately for CHR individuals and HV. Due to missing data, neighborhood crime and symptom analyses in healthy control participants contained 60 individuals.
Table 3.
Spearman correlations between symptoms, outcome and control variables.
| CHR | 1 | 2 | 3 |
|---|---|---|---|
| 1. Neighborhood crime | |||
| 2. Neighborhood Median Family Income | −0.46** | ||
| 3. P2 | 0.25* | −0.02 | |
| 4. Sum P minus P2 | 0.12 | −0.15 | 0.22 |
| Healthy Volunteer | 1 | 2 | 3 |
| 1. Neighborhood crime | |||
| 2. Neighborhood Median Family Income | −0.58** | ||
| 3. P2 | 0.01 | −0.04 | |
| 4. Sum P minus P2 | −0.06 | 0.06 | 0.53** |
Significant at p < 0.05
Significant at p < 0.01
Replication of previous findings
Aiming to replicate findings by Wilson et al. 2016, a step-wise linear regression was conducted with 3 models, to tease apart the contributions of neighborhood socioeconomic status, total symptoms excluding suspiciousness, and neighborhood crime in predicting suspiciousness symptoms. Wilson et al. 2016 had not included neighborhood socioeconomic status in their model, and so this portion was an extension of their work. Otherwise, analyses were the same. To account for skew in neighborhood crime, a natural log transformation was applied to this variable. Model 1 included neighborhood crime predicting P2, Model 2 included neighborhood crime and symptoms (excluding suspiciousness) predicting P2, and Model 3 included neighborhood crime, symptoms (excluding suspiciousness), and neighborhood socioeconomic status predicting P2.
Results
There were no significant differences between CHR and HV groups on demographic characteristics such as age (t = −1.0, p = 0.32), binary gender (X2 = 3.18, p = 0.07), and race (dichotomized as Caucasian/non-Caucasian given the Caucasian majority sample; X2 = 0.86, p = 0.35).
CHR group
The neighborhood crime mean value in the CHR group indicates that on average, crime was 25.06% less common in CHR participant neighborhoods compared to the United States as a whole. The sample’s distribution was skewed to the left however, and so the median of 69 is a better indication of central tendency. This indicates that half of participants lived in neighborhoods in which crime was at least 31% less common compared to the United States as a whole. Neighborhood crime score was associated with suspiciousness symptoms, and not related to the sum of other positive symptoms excluding suspiciousness. Neighborhood socioeconomic status was not related to suspiciousness symptoms, or to total positive symptoms excluding suspiciousness (see Table 3, Supplementary Table 3). Partial correlations controlling for median neighborhood income did not change the direction, magnitude, or significance of the results: greater neighborhood crime predicted greater suspiciousness symptoms, controlling for neighborhood socioeconomic status (r = 0.27, p = 0.03). Likewise, neighborhood crime and total positive symptoms excluding suspiciousness were not significantly related when controlling for neighborhood socioeconomic status (r = 0.06, p = 0.66).
HV group
The neighborhood crime mean value in the HV group indicates that on average, crime was 0.62% more common in HV neighborhoods compared to the United States average. Neighborhood crime was not significantly associated with suspiciousness symptoms, or total positive symptoms minus suspiciousness. Neighborhood median family income was likewise not related to suspiciousness symptoms or total positive symptoms minus suspiciousness. Lastly, controlling for neighborhood median family income, neighborhood crime was not related to suspiciousness symptoms (r = −0.01, p = 0.93), or total positive symptoms minus suspiciousness (r = −0.03, p = 0.81).
Replication of previous findings
Neighborhood crime remained a significant predictor for all 3 models in CHR individuals, suggesting that crime remains a predictor of suspiciousness over and above other symptoms and neighborhood median family income (see Table 4). Even when both total symptoms and neighborhood median family income are both put into the model, neighborhood crime remains the sole significant predictor.
Table 4.
Step-wise linear regression testing the predictive value of neighborhood crime on suspiciousness symptoms in CHR individuals over and above total symptoms (Model 2) and neighborhood socioeconomic status (Model 3).
| Std. beta | t | p value | |
|---|---|---|---|
| Model 1 | |||
| Neighborhood crime | 0.33 | 2.75 | 0.008** |
| Model 2 | |||
| Neighborhood crime | 0.30 | 2.49 | 0.016* |
| Total symptoms | 0.20 | 1.67 | 0.10 |
| Model 3 | |||
| Neighborhood crime | 0.34 | 2.64 | 0.011* |
| Total symptoms | 0.20 | 1.66 | 0.103 |
| Neighborhood socioeconomic status | 0.11 | 0.89 | 0.377 |
Significant at p < 0.05
Significant at p < 0.01
Discussion
As in an earlier study exploring this question (Wilson et al., 2016), greater neighborhood crime was associated with greater suspiciousness symptoms in CHR. This is largely consistent with the broader literature linking exposure to crime to adverse health outcomes (Aneshensel and Sucoff, 1996; Draine et al., 2002; Ellen et al., 2001; Leventhal and Brooks-Gunn, 2003; Miller et al., 2018; Stockdale et al., 2007; Theall, 2017; Wilson et al., 2016; Zammit et al., 2010). Moreover, neighborhood crime was not significantly related to total symptoms excluding suspiciousness in CHR, which lends support to specificity of the relation between suspiciousness/paranoid symptoms and neighborhood crime. Further, a control variable of neighborhood socioeconomic status was included in order to rule out the possibility of the effects being a function of income/socioeconomic status at the neighborhood level. Interestingly, the relation between neighborhood crime and suspiciousness in CHR remained statistically significant after controlling for neighborhood socioeconomic status, lending further evidence to specificity of crime beyond neighborhood income. Finally, neighborhood socioeconomic status was not significantly related to positive symptoms (both total and suspiciousness individually) in either CHR individuals or HV. This is not fully consistent with the literature, though sample characteristics may have driven the lack of association. Significant associations were not observed in HV participants for any analyses of interest, suggesting the association of neighborhood crime and suspiciousness may be particularly relevant to CHR. Taken together, results lend support to the broader notion that taking context into account is key for conceptualizations of psychosis risk, and has poignant ramifications for both assessment, treatment and intervention efforts.
As noted, despite key differences in demographic and geographic sample characteristics, results replicated a previous study of neighborhood crime and suspiciousness symptoms (Wilson et al., 2016). Greater neighborhood crime predicted greater suspiciousness symptoms in CHR, which was not the case in HV. Notably, the current CHR sample resided in Colorado neighborhoods that were, on average, at least 25.06 % below the national average for total crimes per neighborhood. On the other hand, Baltimore, where the other study sample was from, is known to have very high crime rates relative to the national average (Fenton, 2014). Thus, results suggest that the link between suspiciousness and neighborhood crime is present across varying geographic settings and degrees of severity of neighborhood crime. Similarly, the majority of the Baltimore sample self-identified as African American, while the current sample primarily self-identified as Caucasian. Despite these racial differences, results for primary analyses were similar, lending evidence to generalizability of this effect to racial majority group members. Similar to the approach applied in the Baltimore study, the geocoding technique allows us to obtain an objective gauge of crime exposure, providing an incrementally valuable measure of crime beyond that of self-reported experiences or perception of neighborhood crime (Junger-Tas and Marshall, 1999; Thornberry and Krohn, 2000). Differences in self-reported perception of crime could be particularly relevant in CHR groups, since increased suspiciousness could lead to heightened perception of crime occurrence.
As hypothesized, a significant relation was not observed between neighborhood crime and total symptoms (excluding suspiciousness). These results suggest that SIPS measures of suspiciousness and paranoia may relate to neighborhood crime in a specific, meaningful manner. Findings are particularly impactful given that suspiciousness and paranoia are among the most common sub-threshold psychotic symptoms (Freeman, 2007; Morgan et al., 2009). It is possible that at this stage of illness progression, neighborhood crime constitutes an all-encompassing stressful environment comprising “multiple hits”, which interacting with predisposed biological or genetic vulnerability, could ultimately lead to the onset of a psychotic disorder (Jones and Fernyhough, 2006; Walker and Diforio, 1997). This is partially supported by the literature linking exposure to crime among other structural/contextual factors to increased risk of developing psychosis (Bhavsar et al., 2014; Boydell et al., 2004; Burns et al., 2014; Lasalvia et al., 2014; Miller et al., 1999; van Os et al., 2010; Zammit et al., 2010). This neural-diathesis stress conceptualization is also supported by the notion that associations were not detected in HV.
Further, despite the fact that, as expected, neighborhood socioeconomic status was highly correlated with neighborhood crime (r = −0.46), controlling for neighborhood socioeconomic status did not alter the magnitude or significance of the relation between neighborhood crime and suspiciousness symptoms in CHR individuals. In addition, a replication and extension of analyses done by Wilson et al. 2016 demonstrated that adding total symptoms and neighborhood socioeconomic status as predictors did not decrease the predictive value of neighborhood crime for suspiciousness symptoms. This lends evidence to a distinct effect of crime in the current results beyond that of neighborhood socioeconomic status and other psychotic symptoms. The SIPS suspiciousness and paranoid thinking items probe for vigilance and concerns of safety. As Wilson and colleagues posed, rather than a dysfunctional behavior, this could be a normative response to an unsafe environment (Wilson et al., 2016). This fact, however, would not necessarily preclude such heightened suspiciousness from being taxing, or a source of chronic stress in an individual. Nonetheless, this highlights the need for careful assessment of contextual factors while administering the SIPS and labeling individuals with CHR diagnoses.
SIPS ratings, when not fully informed of relevant contextual factors, may over-pathologize participants, or misattribute the nature of distressing or pathological symptoms. Of note, none of our study participants met criteria for a CHR syndrome based on suspiciousness alone, suggesting that participants in the present sample may not be misdiagnosed at high rates due to this phenomenon. Alternatively, hesitance to label individuals living in high-crime contexts with a CHR diagnosis may also lead to missed opportunity for early intervention for those individuals at-risk for developing psychosis. It is crucial to keep in mind that regardless of the reason for the suspiciousness, if it compromises functioning and becomes maladaptive, it remains pertinent as a clinical symptom. It will be paramount for prospective CHR research therefore to incorporate measures of contextual factors into clinical assessment in a manner balancing risk of over-pathologizing with that of under-identifying (Draine et al., 2002; Miller et al., 2018; Wilson et al., 2016). Effective training for assessors (already emphasized in the existing SIPS training protocol) around these issues will only increase in importance as CHR assessment moves from specialty research centers to community mental health (e.g., SAMHSA’s CHRP grants in the U.S). Alternatively, to more directly test these issues, future work could attempt revising SIPS questions to specifically probe about whether the endorsed item is true for the participant in their neighborhood. Nonetheless, independent of context, the field would benefit from conceptualizing suspiciousness symptoms on a spectrum based on level of adaptiveness and influences on functioning.
Contrary to our expectations, neighborhood socioeconomic status was not related to total positive symptoms, for both CHR and HV groups. This is somewhat surprising, considering the wide body of literature linking neighborhood socioeconomic status to both mental and physical health outcomes (Aneshensel and Sucoff, 1996; Bosma et al., 2001; Evans and Kim, 2010; Pickett and Pearl, 2001; Steptoe and Feldman, 2001). The fact that our sample had a rather high average neighborhood median household income ($111,993.35 for CHR individuals and $106,103.16 for HV) could have played a role. Indeed, the lowest value in our sample for neighborhood median household income was $40,250. Perhaps a greater range of socioeconomic conditions are needed in order to detect this effect. There are studies that suggest, for example, that increased risk for psychosis only emerges for those in the lowest social classes (Corcoran et al., 2009). Nonetheless, future studies will be needed to reach a definitive conclusion.
Finally, associations observed in CHR individuals between suspiciousness symptoms and neighborhood crime were not observable in HV. As mentioned above, there is some reason to believe (with caution) that this could strengthen support for the theory that in individuals with pre-existing vulnerability (such as CHR individuals), environmental risk factors may interact to compound risk for development of serious psychopathology (Brody et al., 2013; Evans and Cassells, 2014; Evans and Kim, 2010; Evans et al., 2013; Jones and Fernyhough, 2006; Miller et al., 2018; Walker and Diforio, 1997). Nonetheless, it is important to point out that in a cross-sectional sample, these interpretations are tentative, and future longitudinal investigations are needed before forming conclusions regarding disorder etiology. In addition, restriction of range may have substantially compromised our ability to detect an existing effect in HV. Whereas suspiciousness symptoms ranged from 0–5 in CHR individuals, non-help seeking HV were necessarily constrained to sub-clinical scores (in this case ranging from 0–1, see Table 2, Supplementary Table 2), which considerably restricts variability. Despite this notion, results are useful in lending a comparison point and control group, which was lacking in the literature in the context of neighborhood crime and suspiciousness in CHR.
There are several limitations to consider when interpreting the results of the present investigation. First, it will be paramount to further explore neuroendocrine mechanisms underlying this observed association, given our diathesis-stress conceptualization of the results. Basal cortisol or glucocorticoid resistance could serve as candidate mechanisms through which stress effects the association between suspiciousness and neighborhood crime (Corcoran et al., 2003; Flinn and England, 1997; Lupien et al., 2000; Miller et al., 2002). Though there are benefits to using objective measures of neighborhood characteristics, collecting complementary self-report measures could allow for a fuller understanding of a participant’s perception of the neighborhood context (Cantor and Lynch, 2000). Incorporating qualitative research would also afford a valuable mixed-methods approach to understanding the association between neighborhood crime and suspiciousness in CHR individuals. Adding a qualitative dimension would allow for answering questions such as, do family beliefs affect this association? Further, it will be greatly informative for future investigations to collect specific information about how long the participant lived at each address, and to match these time periods with historical data. This approach would allow for exploring degree of exposure to the neighborhood context.
Relatedly, investigations would benefit from examining the effect of different types of crime on suspiciousness, to identify if this relation is specific to crime type. In a more ethnically diverse sample, it will also be informative to relate ethnic congruence to risk for psychosis, given previous studies have found that it is protective for ethnic minority individuals to live among other ethnic minority groups (Veling et al., 2008). Conversely, seeing whether suspiciousness mediates the association between ethnic density and psychosis risk. Cumulative indices of neighborhood environmental risk will also be important, as many neighborhood factors, such as socioeconomic status, ethnic diversity, and population density, may have additive effects on psychosis risk (Veling et al., 2015). Importantly, limited range in HV precludes us from reaching definitive conclusions from those analyses. In addition, ideally data would be aggregated across different geographic sites, in order to gain a nationally representative distribution of neighborhood crime. Larger, more well-powered samples would also benefit from undertaking analyses at differing geographic levels (e.g. tracts nested within zip codes or states, and so on). This approach would allow for a greater understanding of precise degrees of risk based on distance and severity of exposure. Lifetime substance dependence was an exclusion criterion for the present study; a possible future direction could be to recruit and compare groups based on CHR with history of substance dependence and without. Such studies will likely add generalizability to this work. Despite these limitations, this study builds on previous research to support the notion that context is critical, especially in the case of neighborhood crime and suspiciousness in CHR individuals. It will be key for future investigations to adopt multimodal approaches such as community ecological momentary assessments, and physiological measures of arousal (i.e. heart rate variability) (McDevitt-Murphy et al., 2018). Prevention and intervention efforts could also build on this research by incorporating techniques such as virtual reality, as previous landmark studies have done (Pot-Kolder et al., 2018; Veling et al., 2016). Thus, it is clear that future research may greatly benefit from incorporating contextual factors into assessment, risk models, preventive and intervention treatments.
Supplementary Material
Figure 1.
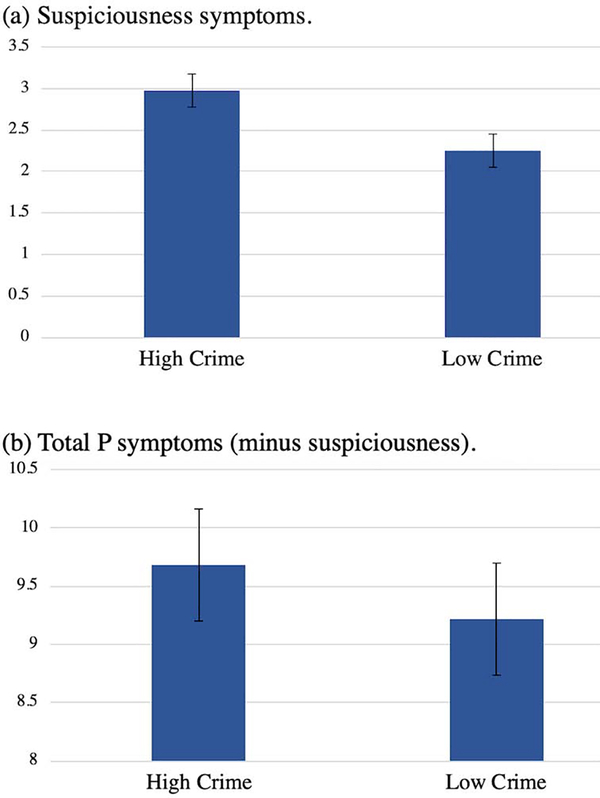
Suspiciousness/P2 symptoms (a) and total P symptoms (b) by neighborhood total crime in CHR individuals. High/Low cutoff is based on the median TCI score (below median = low crime, above or at median = high crime). Mean and standard error are illustrated.
Acknowledgments
We would like to thank the individuals who participated in the study, and the ADAPT research team for their help with data collection and entry.
Role of the Funding Source
This work was supported by a Northwestern University Society Biology and Health Cluster fellowship (T.V.), and by grants R01MH112545, R21/R33MH103231 and R21MH110374 (V.A.M).
Footnotes
Conflicts of Interest
The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aneshensel CS, Sucoff CA, 1996. The neighborhood context of adolescent mental health. Journal of health and social behavior, 293–310. [PubMed] [Google Scholar]
- Bauman LJ, Silver EJ, Stein RE, 2006. Cumulative social disadvantage and child health. Pediatrics 117(4), 1321–1328. [DOI] [PubMed] [Google Scholar]
- Bebbington PE, Bhugra D, Brugha T, Singleton N, Farrell M, Jenkins R, Lewis G, Meltzer H, 2004. Psychosis, victimisation and childhood disadvantage: evidence from the second British National Survey of Psychiatric Morbidity. The British Journal of Psychiatry 185(3), 220–226. [DOI] [PubMed] [Google Scholar]
- Bhavsar V, Boydell J, Murray R, Power P, 2014. Identifying aspects of neighbourhood deprivation associated with increased incidence of schizophrenia. Schizophrenia research 156(1), 115–121. [DOI] [PubMed] [Google Scholar]
- Bosma H, Dike van de Mheen H, Borsboom GJ, Mackenbach JP, 2001. Neighborhood socioeconomic status and all-cause mortality. American Journal of Epidemiology 153(4), 363–371. [DOI] [PubMed] [Google Scholar]
- Boydell J, Van Os J, McKenzie K, Murray R, 2004. The association of inequality with the incidence of schizophrenia. Social Psychiatry and Psychiatric Epidemiology 39(8), 597–599. [DOI] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen Y. f., Kogan SM, Evans GW, Beach SR, Windle M, Simons RL, Gerrard M, Gibbons FX, 2013. Cumulative socioeconomic status risk, allostatic load, and adjustment: a prospective latent profile analysis with contextual and genetic protective factors. Developmental psychology 49(5), 913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns JK, Tomita A, Kapadia AS, 2014. Income inequality and schizophrenia: Increased schizophrenia incidence in countries with high levels of income inequality. International Journal of Social Psychiatry 60(2), 185–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, 2008. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Archives of general psychiatry 65(1), 28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor D, Lynch JP, 2000. Self-report surveys as measures of crime and criminal victimization. Criminal justice 4, 85–138. [Google Scholar]
- Ciarleglio AJ, Brucato G, Masucci MD, Altschuler R, Colibazzi T, Corcoran CM, Crump FM, Horga G, Lehembre-Shiah E, Leong W, Schobel SA, Wall MM, Yang LH, Lieberman JA, Girgis RR, 2018. A predictive model for conversion to psychosis in clinical high-risk patients. Psychol Med, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran C, Perrin M, Harlap S, Deutsch L, Fennig S, Manor O, Nahon D, Kimhy D, Malaspina D, Susser E, 2009. Effect of socioeconomic status and parents’ education at birth on risk of schizophrenia in offspring. Social psychiatry and psychiatric epidemiology 44(4), 265–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran C, Walker E, Huot R, Mittal V, Tessner K, Kestler L, Malaspina D, 2003. The stress cascade and schizophrenia: etiology and onset. Schizophrenia bulletin 29(4), 671–692. [DOI] [PubMed] [Google Scholar]
- Draine J, Salzer MS, Culhane DP, Hadley TR, 2002. Role of social disadvantage in crime, joblessness, and homelessness among persons with serious mental illness. Psychiatric Services 53(5), 565–573. [DOI] [PubMed] [Google Scholar]
- Ellen IG, Mijanovich T, Dillman K-N, 2001. Neighborhood effects on health: exploring the links and assessing the evidence. Journal of Urban Affairs 23(3–4), 391–408. [Google Scholar]
- Evans GW, Cassells RC, 2014. Childhood poverty, cumulative risk exposure, and mental health in emerging adults. Clinical Psychological Science 2(3), 287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Kim P, 2010. Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status–health gradient. Annals of the New York Academy of Sciences 1186(1), 174–189. [DOI] [PubMed] [Google Scholar]
- Evans GW, Li D, Whipple SS, 2013. Cumulative risk and child development. Psychological Bulletin 139(6), 1342. [DOI] [PubMed] [Google Scholar]
- Fenton J, 2014. New FBI statistics: Baltimore No. 5 in murder rate., The Baltimore Sun. [Google Scholar]
- First MB, Gibbon M, 2004. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). [Google Scholar]
- Flinn MV, England BG, 1997. Social economics of childhood glucocorticoid stress response and health. American Journal of Physical Anthropology: The Official Publication of the American Association of Physical Anthropologists 102(1), 33–53. [DOI] [PubMed] [Google Scholar]
- Freeman D, 2007. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev 27(4), 425–457. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P, 2012. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Archives of general psychiatry 69(3), 220–229. [DOI] [PubMed] [Google Scholar]
- Jones SR, Fernyhough C, 2006. A new look at the neural diathesis–stress model of schizophrenia: the primacy of social-evaluative and uncontrollable situations. Schizophrenia Bulletin 33(5), 1171–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junger-Tas J, Marshall IH, 1999. The self-report methodology in crime research. Crime and justice 25, 291–367. [Google Scholar]
- Kim H-Y, 2013. Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restorative dentistry & endodontics 38(1), 52–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia A, Bonetto C, Tosato S, Zanatta G, Cristofalo D, Salazzari D, Lazzarotto L, Bertani M, Bissoli S, De Santi K, 2014. First-contact incidence of psychosis in north-eastern Italy: influence of age, gender, immigration and socioeconomic deprivation. The British Journal of Psychiatry 205(2), 127–134. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J, 2003. Moving to opportunity: an experimental study of neighborhood effects on mental health. American journal of public health 93(9), 1576–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien SJ, King S, Meaney MJ, McEwen BS, 2000. Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biological psychiatry 48(10), 976–980. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Luciano MT, Zakarian RJ, 2018. Use of Ecological Momentary Assessment and Intervention in Treatment With Adults. Focus (Am Psychiatr Publ) 16(4), 370–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlashan TH, Walsh B, Woods S, 2010. The psychosis-risk syndrome : handbook for diagnosis and follow-up. Oxford University Press, New York. [Google Scholar]
- Miller GE, Chen E, Armstrong CC, Carroll AL, Ozturk S, Rydland KJ, Brody GH, Parrish TB, Nusslock R, 2018. Functional connectivity in central executive network protects youth against cardiometabolic risks linked with neighborhood violence. Proc Natl Acad Sci U S A 115(47), 12063–12068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Cohen S, Ritchey AK, 2002. Chronic psychological stress and the regulation of pro-inflammatory cytokines: a glucocorticoid-resistance model. Health psychology 21(6), 531. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Woods SW, Stein K, Driesen N, Corcoran CM, Hoffman R, Davidson L, 1999. Symptom assessment in schizophrenic prodromal states. Psychiatric Quarterly 70(4), 273–287. [DOI] [PubMed] [Google Scholar]
- Morgan C, Fisher H, Hutchinson G, Kirkbride J, Craig TK, Morgan K, Dazzan P, Boydell J, Doody GA, Jones PB, Murray RM, Leff J, Fearon P, 2009. Ethnicity, social disadvantage and psychotic-like experiences in a healthy population based sample. Acta Psychiatr Scand 119(3), 226–235. [DOI] [PubMed] [Google Scholar]
- Nelson B, Amminger GP, McGorry PD, 2018. Recent Meta-Analyses in the Clinical High Risk for Psychosis Population: Clinical Interpretation of Findings and Suggestions for Future Research. Front Psychiatry 9, 502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett KE, Pearl M, 2001. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. Journal of Epidemiology & Community Health 55(2), 111–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pot-Kolder RM, Geraets CN, Veling W, van Beilen M, Staring AB, Gijsman HJ, Delespaul PA, van der Gaag M, 2018. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. The Lancet Psychiatry 5(3), 217–226. [DOI] [PubMed] [Google Scholar]
- Selten J-P, Cantor-Graae E, 2007. Hypothesis: social defeat is a risk factor for schizophrenia? The British Journal of Psychiatry 191(S51), s9–s12. [DOI] [PubMed] [Google Scholar]
- Smith DA, Jarjoura GR, 1988. Social structure and criminal victimization. Journal of Research in crime and delinquency 25(1), 27–52. [Google Scholar]
- Steptoe A, Feldman PJ, 2001. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine 23(3), 177–185. [DOI] [PubMed] [Google Scholar]
- Stockdale SE, Wells KB, Tang L, Belin TR, Zhang L, Sherbourne CD, 2007. The importance of social context: Neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Social science & medicine 65(9), 1867–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theall KP, Drury SS, Shirtcliff EA, 2012. Cumulative neighborhood risk of psychosocial stress and allostatic load in adolescents. American journal of epidemiology 176(suppl_7), S164–S174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theall KP, Shirtcliff EA, Dismukes AR, Wallace M, Drury SS, 2017. Association between neighborhood violence and biological stress in children. JAMA Pediatrics 171, 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Krohn MD, 2000. The self-report method for measuring delinquency and crime. Criminal justice 4(1), 33–83. [Google Scholar]
- van Os J, Kenis G, Rutten BP, 2010. The environment and schizophrenia. Nature 468(7321), 203. [DOI] [PubMed] [Google Scholar]
- Veling W, Pot-Kolder R, Counotte J, van Os J, van der Gaag M, 2016. Environmental social stress, paranoia and psychosis liability: a virtual reality study. Schizophrenia bulletin 42(6), 1363–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veling W, Susser E, Selten J-P, Hoek H, 2015. Social disorganization of neighborhoods and incidence of psychotic disorders: a 7-year first-contact incidence study. Psychological medicine 45(9), 1789–1798. [DOI] [PubMed] [Google Scholar]
- Veling W, Susser E, Van Os J, Mackenbach JP, Selten J-P, Hoek HW, 2008. Ethnic density of neighborhoods and incidence of psychotic disorders among immigrants. American Journal of Psychiatry 165(1), 66–73. [DOI] [PubMed] [Google Scholar]
- Walker E, Mittal V, Tessner K, 2008. Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu. Rev. Clin. Psychol 4, 189–216. [DOI] [PubMed] [Google Scholar]
- Walker EF, Diforio D, 1997. Schizophrenia: a neural diathesis-stress model. Psychological review 104(4), 667. [DOI] [PubMed] [Google Scholar]
- Wilson C, Smith ME, Thompson E, Demro C, Kline E, Bussell K, Pitts SC, DeVylder J, Reeves G, Schiffman J, 2016. Context matters: The impact of neighborhood crime and paranoid symptoms on psychosis risk assessment. Schizophr Res 171(1–3), 56–61. [DOI] [PubMed] [Google Scholar]
- Yung AR, Yuen HP, Berger G, Francey S, Hung T-C, Nelson B, Phillips L, McGorry P, 2007. Declining transition rate in ultra high risk (prodromal) services: dilution or reduction of risk? Schizophrenia bulletin 33(3), 673–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zammit S, Lewis G, Rasbash J, Dalman C, Gustafsson J-E, Allebeck P, 2010. Individuals, schools, and neighborhood: a multilevel longitudinal study of variation in incidence of psychotic disorders. Archives of general psychiatry 67(9), 914–922. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.