This review summarizes the steps from basic research on IL-17 family cytokines to understanding their role in psoriasis pathogenesis to the approval of a number of monoclonal antibodies targeting IL-17 pathways as first line treatment of psoriasis and psoriatic arthritis.
Abstract
The IL-17 cytokine family comprising IL-17A to IL-17F and receptor subunits IL-17RA to IL-17RE represents a genetically ancient intercellular network regulating local tissue homeostasis. Its pivotal role in antifungal defense and its central position in the pathogenesis of inflammatory diseases including psoriasis were discovered only relatively late in the early 2000s. Since the connection of dysregulated IL-17 and psoriasis pathogenesis turned out to be particularly evident, a number of monoclonal antibodies targeting IL-17 pathways have been approved and are used as first line treatment of moderate-to-severe plaque psoriasis and psoriatic arthritis, and further agents are currently in clinical development.
IL-17 and its pivotal role in psoriasis
Over the last few years, we have witnessed a remarkably fast and very successful translation of basic IL-17 biology research to the development of efficient drugs targeting IL-17. Most prominently, mAb designed to neutralize IL-17A, IL-17F, or IL-17RA are either already approved or in clinical trials to treat psoriasis, psoriatic arthritis (PsA), and other chronic inflammatory diseases (Kurschus and Moos, 2017; McGeachy et al., 2019), as summarized in Table 1 and Table 2. In this review, we will focus on the role of IL-17 cytokines as effectors and targets in psoriasis, where dysregulated local IL-17 levels are clearly the key effector mechanism driving the pathophysiology of psoriasis, i.e., neutrophil influx and keratinocyte hyperproliferation. Accordingly, novel biologics targeting IL-17 pathways have been shown to be highly efficacious in moderate-to-severe plaque psoriasis and PsA. As compared with other inflammatory cytokines such as IL-6 or TNF-α, IL-17 cytokines are rather acting locally, particularly at mucosal surfaces and in the skin.
Table 1. Biological drugs targeting IL-17 or IL-23 approved for psoriasis, PsA, and/or AS.
| INN | Target | Construct | Labeled indication |
|---|---|---|---|
| Brodalumab | IL-17RA | Fully human mAb | Pso, PsA (Japan only) |
| Ixekizumab | IL-17A | Humanized mAb | Pso, PsA, AS |
| Secukinumab | IL-17A | Fully human mAb | Pso, PsA, AS |
| Guselkumab | IL-23p19 | Fully human mAb | Pso |
| Risankizumab | IL-23p19 | Humanized mAb | Pso |
| Tildrakizumab | IL-23p19 | Humanized mAb | Pso |
| Ustekinumab | IL-12/23p40 | Fully human mAb | Pso, PsA |
INN, international nonproprietary names; Pso, psoriasis.
Table 2. Investigational drugs targeting IL-17 in indications of interest.
| INN/Code | Target | Construct | Indicationa |
|---|---|---|---|
| Bimekizumab | IL-17A/F | Humanized mAb | Pso, PsA, AS |
| M1095 | IL-17A/F | Nanobody | Pso, PsA |
| ALX-0761 | IL-17A/F | Nanobody | Pso, PsA |
| BCD-085 | IL-17A | mAb | Pso, PsA |
| COVA322 | IL-17A/TNF | Bispecific mAb | Pso, PsA |
INN, international nonproprietary names; Pso, psoriasis.
In clinical trials/planned.
Before we summarize the present clinical data and therapies targeting IL-17 cytokines and its upstream “master cytokine” IL-23, we will review the current understanding of IL-17’s physiological role in establishing local homeostasis with skin microbiota and subsequently discuss the mechanisms that can lead to a pathogenic dysregulation of the IL-23/IL-17 axis.
IL-17 immunity
In the search for cytotoxic lymphocyte–specific genes in mice, Pierre Golstein found the gene Ctla-8 that was 57% homologous to the putative protein encoded by the ORF13 gene of T lymphotropic herpesvirus Saimiri (Rouvier et al., 1993). In the meantime, CTLA-8 is known as IL-17A, the prototype of the IL-17 cytokine family comprising six related proteins from IL-17A to IL-17F (Gaffen, 2009; Moseley et al., 2003; Weaver et al., 2007), recently reviewed in Monin and Gaffen (2018). Members of the IL-17 family are relatively “local cytokines,” acting mainly on nonclassical immune cells such as epithelial, endothelial, and fibroblastic cells (Fossiez et al., 1996; Moseley et al., 2003; Yao et al., 1995). Those cells express IL-17 receptors that are heterodimers composed of the subunit IL-17RA associated with either IL-17RC, IL-17RE, or IL-17RB, giving combinations specific for IL-17A and F, IL-17C, and IL-17E (IL-25), respectively. Cytokine binding to IL-17 receptors recruits and activates the kinase Akt1 (Chang et al., 2006; Qian et al., 2007), which transduces signals via TNF receptor–associated factor 6–mediated pathways (Schwandner et al., 2000) and ultimately leads to activation of canonical NF-κB as well as the ERK pathway in a cell context–dependent manner (Gaffen et al., 2014). While these transcriptional activations are key components of the IL-17 pathway, more recent studies collectively point to a crucial aspect of IL-17 signaling, namely its ability to stabilize transcripts of cytokines and chemokines (Amatya et al., 2018; Herjan et al., 2018; Tanaka et al., 2019). In fact, in most cell culture models, IL-17 is a weak transcriptional activator. Thus, the impact of IL-17 on post-transcriptional regulation of gene expression is fundamental to its pro-inflammatory activity. In response to IL-17 signaling, keratinocytes produce antimicrobial peptides (AMP) and chemokines, which together induce local inflammation and neutrophil influx (Ivanov and Lindén, 2009). In line with the prominent local action of IL-17, it has been shown that IL-17 rather sticks with the extracellular matrix and can be detected even on the producing cells themselves (Brucklacher-Waldert et al., 2009). IL-17 signaling induces different outcomes in different target cells ranging from receptor activator of NF-κB ligand production in osteoclasts leading to bone remodeling (Noack et al., 2019) to production of IL-6 and IL-8 (CXCL8) in fibroblasts, leading to local inflammation and neutrophil influx (Noack et al., 2019). In experimental psoriasis, current data suggest that keratinocytes are the cells that are primarily involved in IL-17–driven pathogenesis of psoriasis (Garzorz-Stark and Eyerich, 2019). In the Aldara model of psoriasiform skin inflammation, Moos et al. (2019) showed that epidermal hyperplasia was only seen in mice expressing IL-17RA in keratinocytes. As demonstrated by Ha et al. (2014), IL-17A can increase the number of human keratinocytes in S-phase dependent on calcium concentration. A very recent study found that IL-17 and IL-22 promote keratinocyte stemness (Ekman et al., 2019). In two studies, it was shown that mice with a gain-of-function mutation of the card14 gene, a known risk locus for human psoriasis, developed spontaneous psoriasis-like skin inflammation triggered by IL-17 mostly derived from αβ T cells acting on keratinocytes (Mellett et al., 2018; Wang et al., 2018). This was mediated by intracellular CARMA2 accumulation and activation. Anti–IL-23p19 antibodies could significantly reduce inflammation by blocking IL-17–mediated effects on keratinocytes. These findings argue for a direct effect of IL-17 on keratinocyte proliferation and activation that contributes to the increased epidermal turnover, and AMP and chemokine overexpression in psoriasis.
Within the IL-17 family, the leading member in tissue inflammation, autoimmunity, and host defense is IL-17A. Its relative IL-17F shares the highest homology with IL-17A (Kawaguchi et al., 2001; Starnes et al., 2001), and the genes encoding IL-17F and IL-17A are actually syntenic, located on chromosome 6 in humans and on chromosome 1 in mice. Mouse studies of either single or double knockout mice suggested an important contribution of both cytokines to the defense against mucoepithelial infection, while only IL-17A– but not IL-17F–deficient mice were protected in inflammatory disease models (Ishigame et al., 2009). IL-17A and IL-17F can act as homo- or heterodimers (Liang et al., 2007), binding and signaling through the IL-17RA/IL-17RC receptor expressed on a variety of stroma and tissue cells including keratinocytes.
The finding that retinoic acid receptor–related orphan receptor γ isoform t was promoting differentiation of naive CD4+ T cells into IL-17–producing pro-inflammatory T helper 17 (Th17) cells initiated a bonanza of studies elucidating Th17 differentiation (Harrington et al., 2005; Ivanov et al., 2006), Th17 plasticity (Lee et al., 2009), and Th17 balance with Foxp3+ regulatory T cells (Bettelli et al., 2006). However, as suggested by its original name, Ctla-8, the Il17a gene was originally cloned from activated cytotoxic lymphocytes, and therefore it is not surprising that CD8+ T cells can also be an important source of IL-17 in mice (He et al., 2006) and humans (Singh et al., 2008). At the same time, it emerged that not Th17 cells, but rather γδ T cells, innate T cells, and innate lymphoid cells (ILCs), are the main sources of IL-17 in tissues (Awasthi et al., 2009; Roark et al., 2008). In mouse skin, a self-renewing population of dermal γδ T cells was identified as the major source of IL-17 in steady state (Gray et al., 2011; Sumaria et al., 2011). These IL-17–producing γδ T cells (γδ17 cells) in the dermis are chronically activated by local signals and fairly tissue-resident (Laidlaw et al., 2019; Tan et al., 2019). In human skin, the contribution of γδ17 cells and other innate lymphocytes to steady state IL-17 production is currently less clear (Brüggen et al., 2016).
IL-17 balancing microbiota and pathogens
The skin is the body’s most exposed barrier. It maintains and tolerates its own commensal microbiome, which is layered according to anatomical site and age to the environment (Belkaid and Segre, 2014; Gerstel et al., 2018; Sanford and Gallo, 2013). Interestingly, a number of recent experimental studies revealed how specific members of the skin microbiota, e.g., Staphylococcus epidermidis and Corynebacterium accolens, train and support the immune response to pathogens such as Staphylococcus aureus, the parasite Leishmania major, and invasive fungi (Naik et al., 2015; Ridaura et al., 2018). In those and other examples, the protective role of commensal colonization relied on the induction of local IL-17–mediated immunity in the skin (Linehan et al., 2018).
Likewise, absence or impaired IL-17 immunity predisposes patients to chronic mucocutaneous candidiasis disease caused by Candida albicans and, to a lesser extent, S. aureus (Boisson et al., 2013; Eyerich et al., 2008; Ling et al., 2015; Puel et al., 2011). Importantly, a single human null mutation of the IL17F gene was sufficient to cause an inherited susceptibility to mucocutaneous infections (Puel et al., 2011). Those findings highlight the central role of the cytokines IL-17A and IL-17F in establishing skin-commensal homeostasis and in protective immune responses to pathogens and opportunistic infections, in particular to fungi. Along these lines, the single or double knockout mice for Il17a and/or Il17f can be kept with no signs of pathology under specific pathogen–free conditions (Haas et al., 2012; Ishigame et al., 2009), but otherwise mouse lines with defective IL-17 signaling collectively show profoundly increased susceptibility to chronic infection with C. albicans and to a lesser extent S. aureus (Cho et al., 2010; Conti et al., 2009; Saijo et al., 2010). Experimental models indicated that IL-17 contributes to protection from fungi other than C. albicans (Burstein et al., 2018; Hernández-Santos et al., 2019; Sparber et al., 2019; Sparber and LeibundGut-Landmann, 2019; Wüthrich et al., 2011). A recent human study showed that Th17 cells directed against other fungi are induced by cross-reactivity to C. albicans (Bacher et al., 2019).
Dysregulation of IL-17
Experimental models of IL-17–driven psoriasis
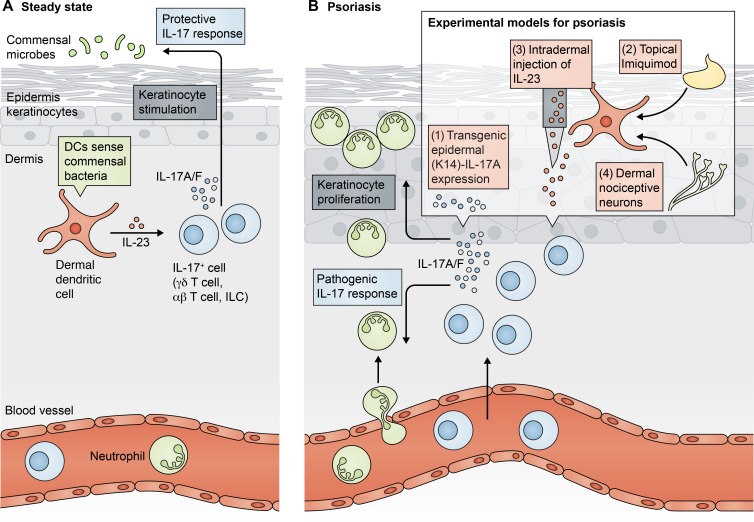
In skin, invasive infections and disturbances in barrier function induce profound effects. Subsequent activation of keratinocytes and dendritic cells (DCs) as sentinels of danger signals due to barrier disruption leads to the activation of innate and adaptive immunity. Recruitment of neutrophils and increased production of AMP in psoriasis are induced at least in a major part through the activity of IL-17 cytokine family members. It follows that mouse models for human psoriasiform skin inflammation depend on the overabundance of IL-17 in the skin (Fig. 1). However, as discussed previously, none of the current models is perfectly representing human psoriasis (Bocheńska et al., 2017; Chuang et al., 2018; Hawkes et al., 2018; Swindell et al., 2011). In steady state, direct and indirect sensing (via nociceptive sensory fibers; Cohen et al., 2019; Kashem et al., 2015; Riol-Blanco et al., 2014) of skin microbiota induce dermal DCs to produce basal levels of IL-23, which activates IL-17A and IL-17F secretion of tissue-resident lymphocytes. IL-17A and IL-17F in turn are essential to limit microbial invasion and to ensure skin integrity. Direct overexpression of IL-17A under the control of a keratinocyte-specific K14 Cre recombinase in mice induced a pathology resembling human psoriasis including dermal infiltration of effector T cells, formation of neutrophil microabscesses, and hyperkeratosis (Croxford et al., 2014). Similarly, keratinocyte-specific overexpression of IL-17C also promoted psoriasiform skin inflammation (Johnston et al., 2013). Other experimental models function via induction of elevated levels of dermal IL-23, which in turn activates IL-23R–expressing dermal lymphocytes including γδ17 cells, αβ T cells, and ILCs. This may be achieved directly by intradermal injection of IL-23 (Gauld et al., 2018; Rizzo et al., 2011), or via increased systemic levels of IL-23 (Leys et al., 2019), although human psoriasis is not usually accompanied by increased serum levels of IL-23 (Bai et al., 2017). The most widely used experimental model is topical application of the TLR7/8 agonist imiquimod (Aldara; Gilliet et al., 2004; van der Fits et al., 2009), which induces the innate activation of dermal DCs (van der Fits et al., 2009). This leads to locally increased IL-23 production, activating downstream IL-23R–expressing dermal lymphocytes that in turn respond by augmented IL-17 secretion (Gladiator et al., 2013; Pantelyushin et al., 2012). Among those IL-23–responsive skin-resident effector lymphocytes, γδ17 cells seem to be the most important population, because their conditional depletion protected from imiquimod-induced psoriasis-like inflammation (Sandrock et al., 2018). Together, all IL-23/IL-17–dependent models ultimately induce skin inflammation characterized by keratinocyte hyperproliferation and neutrophil influx resembling human psoriasis.
Figure 1.
IL-17 immunity and experimental psoriasis in mouse skin. (A) Healthy mouse skin is composed of a thin epidermal layer and the subjacent dermis. At steady state, dermal DCs sense the presence of commensal bacteria and secrete basal levels of IL-23 acting on local IL-17 producing lymphocytes including γδ T cells, αβ T cells, and ILC3s. In turn, dermal lymphocyte–derived IL-17 induces a protective IL-17 response that stimulates keratinocytes and ensures epithelial barrier integrity and homeostasis with commensal microbes. (B) Different experimental models for psoriasis induce a pathogenic IL-17 response that results in release of chemokines and cytokines attracting neutrophils from the circulation and aberrant proliferation of keratinocytes leading to acanthosis with hyper- and parakeratosis. (1) Genetic overexpression of IL-17A by K14+ keratinocytes, (2) topical application of imiquimod resulting in local secretion of IL-23 by dermal DC, and (3) intradermal injection of IL-23. Further, (4) activation of dermal nociceptive neurons results in pathogenic IL-17 response and proliferation of keratinocytes.
IL-17 in the pathogenesis of human psoriasis
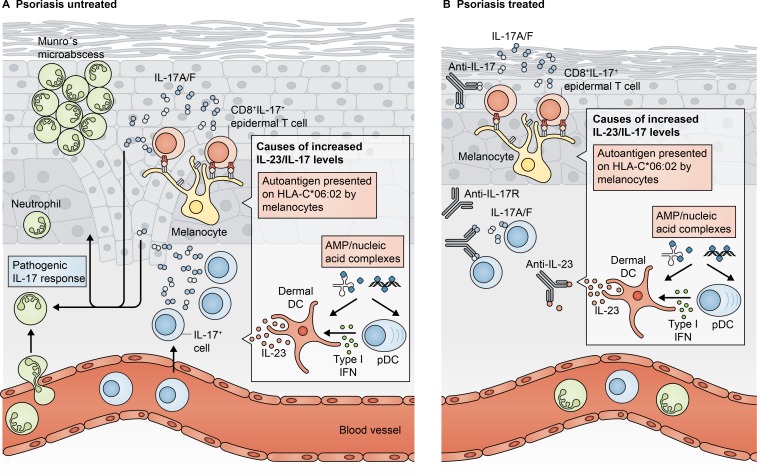
Accumulating evidence suggests that a dysregulated IL-23/IL-17 cytokine axis is at the heart of the pathogenesis of human psoriasis, further supported by the high efficacy of drugs targeting this pathway (see below). The data that initially pointed toward these cytokines as pathogenic suspects and thus prime targets for therapy were describing their increased expression in psoriatic lesions (Lee et al., 2004; Teunissen et al., 1998), as well as accumulations of IL-17–producing T cells (Lowes et al., 2008), suggesting key roles for IL-17A and IL-23 in the treatment of psoriasis (Lowes et al., 2007; Nickoloff, 2007). Accordingly, human psoriasis and related mouse models are considerably similar, i.e., dermal DCs produce IL-23, which activates tissue-resident lymphocytes to secrete IL-17A and IL-17F leading to recruitment of neutrophils, increased production of AMP and chemokines, and epidermal changes (Fig. 2). However, the factors that drive human psoriasis are certainly different and depend on genetic susceptibility and environmental factors.
Figure 2.
IL-17 immunity in human psoriasis. (A) Psoriasis pathogenesis is induced by increased levels of IL-17 that stimulate keratinocyte proliferation resulting in acanthosis, para- and hyperkeratosis, and release of AMP and chemokines that recruit neutrophils from the circulation, leading to formation of Munro’s microabscesses within the stratum corneum. Increased IL-23/IL-17 levels can be caused by presentation of autoantigens by melanocytes to autoreactive epidermal CD8+ T cells resulting in IL-17 secretion and by plasmacytoid DCs (pDCs) activated by antimicrobial peptide (AMP)–nucleic acid complexes to secrete type I interferons that in turn induce secretion of IL-23 by dermal DCs subsequently stimulating and recruiting IL-17 producing lymphoid cells. (B) Targeting IL-23, IL-17, and/or IL-17R by specific mAb leads to less stimulation of keratinocytes and IL-17–secreting cells. This results in reduced acanthosis, inhibits infiltration of neutrophils, and thus ameliorates psoriasis pathology.
In humans, the observation that topical imiquimod (Aldara) application led to exacerbation of psoriasis together with further investigations contributed to the elucidation of the role of IL-17 cytokines in psoriasis (Gilliet et al., 2004). However, there is considerable difference between natural psoriasis and Aldara-induced lesions in humans (Vinter et al., 2015). Along these lines, what drives the initial activation of the IL-23/IL-17 axis? Initial events might be the TLR9-dependent recognition of self-DNA complexed with the cationic AMP LL37 by plasmacytoid DCs, which subsequently activate dermal DCs via type I interferons (Lande et al., 2007). Self-RNA-LL37 complexes might in addition trigger IL-23 production by dermal myeloid DCs directly via TLR8 (Ganguly et al., 2009). This may induce a vicious circle, as IL-23 drives proliferation and accumulation of IL-23R–expressing innate lymphocytes; however, in human dermis, the majority of these may be ILC3s instead of γδ17 cells (Dyring-Andersen et al., 2014; Villanova et al., 2014). Their augmented secretion of IL-17A and IL-17F next acts on nearby keratinocytes, which in turn produce more AMP and chemokines and thereby perpetuate the dysregulated IL-23/IL-17 axis. Further support for an autoimmune cause of psoriatic skin inflammation comes from two reports identifying (1) LL37 peptides as direct targets of CD4+ and CD8+ T cells (Lande et al., 2014) and (2) a strong linkage of many clinical forms of psoriasis with HLA-C*06:02 mediating antigen-specific responses to melanocyte antigen ADAMTS-like protein 5 (Arakawa et al., 2015).
There is good evidence that the IL-23/IL-17 axis is at least in part responsible for the inflammation at the enthesis, the hallmark of PsA that develops in ∼20% of patients with plaque psoriasis (Ritchlin et al., 2017). Biomechanical stress and microbiome alterations are discussed as trigger factors for PsA leading to an IL-17–mediated bone and joint inflammation (McGonagle et al., 2019). A link between inflammation of skin, joints, and blood vessels related to IL-17 was provided by using the model of keratinocyte-specific K14 Cre recombinase (see above). The phenotype of mice showed psoriasis-like flaky skin and histological features of psoriasis-like inflammation, thinning of bone cortex and trabecular structure, and endothelial cell dysfunction (Karbach et al., 2014; Uluçkan et al., 2016).
Together, although the final common pathways of experimental psoriasis-like dermatitis and human psoriasis are sharing features such as increased numbers of dermal IL-23R–positive lymphocytes, keratinocyte hyperproliferation, and formation of neutrophil microabscesses, a number of autoimmune or cross-recognition events accidentally trigger and propagate the local production of IL-17 in the pathogenesis of the human disease, which are not covered by the experimental models.
Current therapies targeting IL-17 cytokines
Targeting IL-17 in psoriasis—A perfect match?
Excitement about the potential of anti–IL-17–based therapies for pathologies with an IL-17 signature was first generated by the work of Hueber et al. (2010), investigating the effect of secukinumab/AIN457, a fully human mAb against IL-17A, in a proof-of-concept setting in plaque psoriasis, rheumatoid arthritis, and uveitis. In patients with plaque psoriasis, secukinumab was given as single intravenous infusion (3 mg/kg), and disease severity was assessed in short intervals until week 12 using the psoriasis area and severity index (PASI). In >40% of patients, a reduction of PASI of >75% (PASI75) was achieved at week 12 in comparison to placebo (4%). Secukinumab was fast-acting and already achieved the maximum efficacy at week 6. Efficacy was also shown in rheumatoid arthritis and uveitis. Subsequently, a large clinical trial program was started, leading to the registration of secukinumab for plaque psoriasis in 2015 with a dose of 300 mg subcutaneously given every 4 wk in maintenance therapy after an updosing in weekly intervals in the initial 4 wk of therapy (Langley et al., 2014). Because of efficacy, speed of onset of activity, and a favorable benefit–risk profile, secukinumab was the first biological given a first-line label for plaque psoriasis.
Subsequently the anti–IL-17A humanized mAb ixekizumab (Griffiths et al., 2015) and a mAb against the IL-17 receptor A, brodalumab (Lebwohl et al., 2015), have been registered first-line for plaque psoriasis. The efficacy of anti–IL-17RA brodalumab is very high, possibly because IL-17RA neutralization blocks binding to all known heterodimeric receptors for IL-17A/F, but also IL-17C and IL-17E. However, because of the continued presence of active IL-17 cytokines, there is a rather quick relapse after stopping treatment with brodalumab (Masson Regnault et al., 2017). Three individual cases of suicide occurred connected to a brodalumab trial, and therefore the US Food and Drug Administration and Health Canada approval of this drug carries a suicide warning (Mullard, 2017). Although there are some recent data connecting deficient IL-17 signaling to impaired short-term memory (Ribeiro et al., 2019) a potential casual connection of psychiatric disease and blocking IL-17RA is regarded as controversial (Beck and Koo, 2019; Rodriguez-Bolanos et al., 2019).
A puzzling clinical observation is that there is primary and secondary nonresponse to anti–IL-17 drugs in a subgroup of patients. It cannot be explained today why a patient showing secondary nonresponse to secukinumab can successfully be switched to ixekizumab and vice versa (Gasslitter et al., 2019).
In a first randomized trial in palmoplantar pustulosis characterized by a prominent infiltrate of neutrophils, secukinumab showed improvement over placebo. However, given the hypothesis that IL-17A is an important cytokine mediating neutrophil recruitment, the estimate of a high efficacy was not met (Mrowietz et al., 2019).
Based on data about a pathophysiological role of IL-17 family members in PsA, clinical trial programs were launched leading to registration of ixekizumab (Mease et al., 2017; Nash et al., 2017) and secukinumab (McInnes et al., 2015) for this indication (brodalumab got a PsA indication only in Japan). As the pathophysiology of axial PsA has a number of similarities to ankylosing spondylitis (AS), anti–IL-17 drugs have been investigated for that indication. Because of the high efficacy, ixekizumab (van der Heijde et al., 2018) and secukinumab (Baeten et al., 2015) were further registered for treatment of AS. In clinical practice, anti–IL-17 drugs are now preferred over anti–TNF-targeted therapies for plaque psoriasis and for patients with concomitant PsA.
Related to their mode of action, two main safety signals became known when using anti–IL-17 drugs: candidiasis including rare cases of chronic mucocutaneous candidiasis disease and induction or exacerbation of Crohn’s disease. As mentioned above, IL-17 is a key cytokine required for antifungal defense, and known genetic deficiencies in IL-17 signaling or function lead to severe Candida infections (Lévy et al., 2016; Puel et al., 2011). In patients treated with anti–IL-17 drugs, candidiasis develops in up to 4% of patients (Saunte et al., 2017). Clinical trials to treat Crohn’s disease or other forms of inflammatory bowel disease with anti–IL-17A drugs turned out to be ineffective, and higher rates of adverse events were noted compared with placebo (Hueber et al., 2012). Although there is a low rate of anti–IL-17–induced Crohn’s disease according to a recent analysis using all clinical data of the secukinumab trial program, there are individual cases of new-onset Crohn’s or exacerbation of known disease (Schreiber et al., 2019). This suggests that IL-17 plays a different pathophysiological role in psoriasis and PsA versus inflammatory bowel disease, where the function in intestinal tissue repair and epithelial barrier function is pivotal (Lee et al., 2015; Maxwell et al., 2015; O’Connor et al., 2009; Zepp et al., 2017).
New data provided evidence that apart from IL-17A, other family members such as IL-17F and E may play an equally important role in plaque psoriasis and even in PsA (Bertelsen et al., 2018; Senra et al., 2016). A new dual antagonist antibody in phase 3 clinical trial development, bimekizumab (UCB4940), targeting IL-17A and F, showed PASI90 improvement in 79% of plaque psoriasis patients after 12 wk (Papp et al., 2018b). In a proof-of-concept trial in PsA, bimekizumab showed an ARC50 response (American College of Rheumatology 50% response criteria) in 57% of patients at week 12, suggesting a very high efficacy and a very fast onset of activity (Glatt et al., 2018). In a recent proof-of-concept trial, a new anti–IL-17A/F nanobody (M1095) given subcutaneously showed a PASI90 response at day 85 in up to 100% of patients, representing a level of efficacy among the highest known so far (Svecova et al., 2019).
Apart from therapeutics with a direct effect on IL-17 family members, there is accumulating evidence for a reduction of lesional IL-17 levels with known systemic drugs for plaque psoriasis including methotrexate (Furiati et al., 2019; Reich et al., 2019a).
Plaque psoriasis is associated with vascular inflammation and among key cytokines involved IL-17A plays a pivotal role. In the KC-Tie2 mouse model, animals develop psoriasis-like skin inflammation along with increased IL-17, IL-23, and increased occlusive thrombus formation. Treatment with mAbs against IL-17A or IL-17RA was able to lengthen the time to thrombus formation (Li et al., 2018). In recent studies in mice presenting either with IL-17RA or IL-17A deficiency, a clear link between the promotion of endothelial cell activation, vascular inflammation, and leukocyte infiltration mediated by IL-17 was demonstrated that could be inhibited by using an anti–IL-17A antibody (Nordlohne et al., 2018). The circulating IL-17 level correlates positively with the severity and progression of carotid artery plaques in patients with atherosclerosis, and there is a correlation of peripheral Th17 cells and Th17 cell–associated cytokines to the severity of carotid artery plaque (Liu et al., 2012). In a 52-wk randomized, placebo-controlled trial with secukinumab in plaque psoriasis, flow-mediated dilation was continuously measured as a surrogate marker for vascular inflammation (von Stebut et al., 2019). In the secukinumab group, flow-mediated dilation was higher but did not reach significance against placebo at the primary endpoint at week 12 but after 52 wk in the open phase.
Periodontitis, an inflammation of the gingival tissue surrounding the gingival crevice, is characterized by a prominent infiltration of neutrophils and excessive levels of IL-17 cytokines, namely IL-17A and F (Apatzidou et al., 2018; Hajishengallis, 2014). There is a significant association between periodontitis and plaque psoriasis and an even stronger link to PsA (Egeberg et al., 2017). Experimental models pointed toward a contribution of mechanical stress, i.e., mastication, as well as involvement of dysbiotic oral microbiota to the activation of inflammatory gingival Th17 cells and γδ17 cells (Dutzan et al., 2017, 2018; Krishnan et al., 2018; Wilharm et al., 2019). The concept that mechanical signals can trigger innate IL-17 production, while shown in periodontal inflammation, have also been discussed for AS (Reinhardt et al., 2016; Sherlock et al., 2012) and may also be applicable to psoriasis.
Psoriasis as a systemic disorder comprises a complex pathology that affects not only the skin. Comorbidity including joint and vascular manifestations varies among patients, respective triggers, and risk factors. Thus, the aim of disease management is to improve the main symptoms and comorbidity at the same time (Mrowietz et al., 2014). With therapeutics targeting IL-17–dependent pathways/events, this strategy seems to work well.
Targeting the master cytokine IL-23
A pivotal question about the pathophysiological relevance of IL-17 and its role as therapeutic target in psoriasis still remains open: Is the master cytokine IL-23 a better choice for treatment? It has long been known that IL-23 stimulates the differentiation of Th17 cells and subsequently the production of IL-17 (McGeachy et al., 2009). Very recently a group 2 ILC subpopulation was described that can convert into IL-17–producing NKp44− ILC3-like cells under the control of IL-1β and IL-23 and that can home into skin through CCR6 expression (Bernink et al., 2019; Bielecki et al., 2018 Preprint). These studies are reminiscent of earlier reports describing the innate activation of γδ T cells by IL-1β and IL-23 (Haas et al., 2009; Martin et al., 2009; Sutton et al., 2009).
The latest registered IL-23p19 therapeutic antibody risankizumab is able to improve psoriasis to clear or almost clear skin in >80% of patients after a year of therapy (Gordon et al., 2018). Even more intriguing data were generated in the early development program of risankizumab. After having received a single subcutaneous dose of risankizumab (0.25 mg/kg and 1 mg/kg), six of eight patients (of a total of 13 enrolled) with moderate to severe psoriasis maintained clear skin for at least 41–66 wk (Krueger et al., 2015). Data from a randomized withdrawal setting with the IL-23p19 inhibitor guselkumab shows maintenance of clear or almost clear skin in >40% of patients after 20 wk following the last dose (Reich et al., 2017). In this group of patients, serum levels of IL-17A and F remained low as compared with those not maintaining this level of efficacy (Gordon et al., 2019). As the pharmacological half-life of therapeutic IgG antibodies is about 3 wk, the very long disease-free time after IL-23p19 inhibition must be caused by lasting immunomodulatory effects. So far, known the high efficacy of IL-23 inhibitors is not associated with adverse events such as Candida infections seen when using IL-17A/IL-17RA antagonists, as exemplified by first long-term data on the IL-23p19 antagonist tildrakizumab (Reich et al., 2019b).
Concluding remarks
A balanced signaling along the IL-23/IL-17 cytokine axis is an important mechanism to ensure skin–microbial homeostasis. Experimental and clinical evidence suggest that its dysregulation induces psoriasis. Thus, targeting the IL-23/IL-17 cytokine axis is a straightforward approach to treat psoriasis, as demonstrated in clinical trials as well as in real-world data (Rompoti et al., 2019). Nevertheless, the universe of treatment options in psoriasis is expanding, and manifold new targets are evolving. JAK inhibitors were effective for moderate to severe plaque psoriasis in randomized trials (Bachelez et al., 2015; Papp et al., 2016). Specific inhibitors for tyrosine kinase 2 downstream of the IL-23 receptor resulted in improvement of psoriasis in clinical trials (Papp et al., 2018a). Furthermore, psoriasis is the lead indication for small molecule inhibitors antagonizing the activity of Th17 cell differentiation determining transcription factor retinoic acid receptor–related orphan receptor γ isoform t (Bronner et al., 2017; Ecoeur et al., 2019). However, IL-17A and IL-17F are the central effector cytokines, and their neutralization or blocking of their interaction with specific cytokine receptors turned out to be a game changer for patients suffering from psoriasis or PsA.
Some caution is necessary because rare congenital defects in the IL-17 pathway exemplify the relevance of IL-17 in protective immunity (Sparber and LeibundGut-Landmann, 2019) as genetic defects in IL-17 signaling displayed strong phenotypes characterized by susceptibility to fungal infection (Lévy et al., 2016; Okada et al., 2016; Puel et al., 2011). Therefore, it is somewhat surprising that the side effects of anti–IL-17 therapies are relatively mild. One theory is that targeting IL-17A inhibits IL-17A homodimers and A/F heterodimers but spares IL-17F homodimers (Kurschus and Moos, 2017). In addition, neutralizing cytokines with mAb depends on dosage, timing, and tissue penetration. A nonquantitative antagonism of IL-17 in the epidermis probably spares sufficient cytokine molecules required for antimicrobial defense. Neutralizing the upstream master cytokine IL-23 and not IL-17 cytokines directly spares IL-23–independent IL-17 production and thus should leave the required amount for local antimicrobial responses. In this context, targeting IL-23 still seems to be able to induce long-term remissions of the disease severity in psoriasis. Such long-lasting effects may be explained by a negative impact on the homeostasis and survival of IL-23R–dependent skin-resident lymphocytes, i.e., γδ T cells, αβ T cells, and ILCs, all of which may take some considerable time to recover in numbers once IL-23 blockade is discontinued. Monitoring the major cellular sources of IL-17 in a large number of patients treated with anti–IL-17 versus anti–IL-23 mAb will in turn be very instructive for understanding human IL-17 biology.
Acknowledgments
We thank the Deutsche Forschungsgemeinschaft for funding under Germany’s Excellence Strategy—EXC 2155 “RESIST”—Project ID 39087428.
I. Prinz has been an advisor and/or received speaker’s honoraria from Novartis and Bayer. U. Mrowietz has been an advisor and/or received speaker’s honoraria and/or received grants and/or participated in clinical trials of the following companies with interest in compounds mentioned in the manuscript: AbbVie, Almirall, Boehringer-Ingelheim, Eli Lilly, Formycon, Janssen, Leo Pharma, Medac, Novartis, and UCB. I. Sandrock declares no competing financial interests.
Author contributions: I. Prinz, I. Sandrock, and U. Mrowietz searched the literature, wrote, and edited the manuscript.
References
- Amatya N., Childs E.E., Cruz J.A., Aggor F.E.Y., Garg A.V., Berman A.J., Gudjonsson J.E., Atasoy U., and Gaffen S.L.. 2018. IL-17 integrates multiple self-reinforcing, feed-forward mechanisms through the RNA binding protein Arid5a. Sci. Signal. 11:eaat4617 10.1126/scisignal.aat4617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apatzidou D.A., Iskas A., Konstantinidis A., Alghamdi A.M., Tumelty M., Lappin D.F., and Nile C.J.. 2018. Clinical associations between acetylcholine levels and cholinesterase activity in saliva and gingival crevicular fluid and periodontal diseases. J. Clin. Periodontol. 45:1173–1183. 10.1111/jcpe.12989 [DOI] [PubMed] [Google Scholar]
- Arakawa A., Siewert K., Stöhr J., Besgen P., Kim S.M., Rühl G., Nickel J., Vollmer S., Thomas P., Krebs S., et al. . 2015. Melanocyte antigen triggers autoimmunity in human psoriasis. J. Exp. Med. 212:2203–2212. 10.1084/jem.20151093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awasthi A., Riol-Blanco L., Jäger A., Korn T., Pot C., Galileos G., Bettelli E., Kuchroo V.K., and Oukka M.. 2009. Cutting edge: IL-23 receptor gfp reporter mice reveal distinct populations of IL-17-producing cells. J. Immunol. 182:5904–5908. 10.4049/jimmunol.0900732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachelez H., van de Kerkhof P.C., Strohal R., Kubanov A., Valenzuela F., Lee J.H., Yakusevich V., Chimenti S., Papacharalambous J., Proulx J., et al. OPT Compare Investigators . 2015. Tofacitinib versus etanercept or placebo in moderate-to-severe chronic plaque psoriasis: a phase 3 randomised non-inferiority trial. Lancet. 386:552–561. 10.1016/S0140-6736(14)62113-9 [DOI] [PubMed] [Google Scholar]
- Bacher P., Hohnstein T., Beerbaum E., Röcker M., Blango M.G., Kaufmann S., Röhmel J., Eschenhagen P., Grehn C., Seidel K., et al. . 2019. Human Anti-fungal Th17 Immunity and Pathology Rely on Cross-Reactivity against Candida albicans. Cell. 176:1340–1355.e15. 10.1016/j.cell.2019.01.041 [DOI] [PubMed] [Google Scholar]
- Baeten D., Sieper J., Braun J., Baraliakos X., Dougados M., Emery P., Deodhar A., Porter B., Martin R., Andersson M., et al. MEASURE 2 Study Group . 2015. Secukinumab, an Interleukin-17A Inhibitor, in Ankylosing Spondylitis. N. Engl. J. Med. 373:2534–2548. 10.1056/NEJMoa1505066 [DOI] [PubMed] [Google Scholar]
- Bai F., Zheng W., Dong Y., Wang J., Garstka M.A., Li R., An J., and Ma H.. 2017. Serum levels of adipokines and cytokines in psoriasis patients: a systematic review and meta-analysis. Oncotarget. 9:1266–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bielecki P., Riesenfeld S.J., Kowalczyk M.S., Amezcua Vesely M.C., Kroehling L., Yaghoubi P., Dionne D., Jarret A., Steach H.R., McGee H.M., et al. . 2018. Skin inflammation driven by differentiation of quiescent tissue-resident ILCs into a spectrum of pathogenic effectors. bioRxiv. 10.1101/461228 (Preprint posted November 12, 2018) [DOI]
- Beck K.M., and Koo J.. 2019. Brodalumab for the treatment of plaque psoriasis: up-to-date. Expert Opin. Biol. Ther. 19:287–292. 10.1080/14712598.2019.1579794 [DOI] [PubMed] [Google Scholar]
- Belkaid Y., and Segre J.A.. 2014. Dialogue between skin microbiota and immunity. Science. 346:954–959. 10.1126/science.1260144 [DOI] [PubMed] [Google Scholar]
- Bernink J.H., Ohne Y., Teunissen M.B.M., Wang J., Wu J., Krabbendam L., Guntermann C., Volckmann R., Koster J., van Tol S., et al. . 2019. c-Kit-positive ILC2s exhibit an ILC3-like signature that may contribute to IL-17-mediated pathologies. Nat. Immunol. 20:992–1003. 10.1038/s41590-019-0423-0 [DOI] [PubMed] [Google Scholar]
- Bertelsen T., Iversen L., and Johansen C.. 2018. The human IL-17A/F heterodimer regulates psoriasis-associated genes through IκBζ. Exp. Dermatol. 27:1048–1052. 10.1111/exd.13722 [DOI] [PubMed] [Google Scholar]
- Bettelli E., Carrier Y., Gao W., Korn T., Strom T.B., Oukka M., Weiner H.L., and Kuchroo V.K.. 2006. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 441:235–238. 10.1038/nature04753 [DOI] [PubMed] [Google Scholar]
- Bocheńska K., Smolińska E., Moskot M., Jakóbkiewicz-Banecka J., and Gabig-Cimińska M.. 2017. Models in the Research Process of Psoriasis. Int. J. Mol. Sci. 18:2514 10.3390/ijms18122514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boisson B., Wang C., Pedergnana V., Wu L., Cypowyj S., Rybojad M., Belkadi A., Picard C., Abel L., Fieschi C., et al. . 2013. An ACT1 mutation selectively abolishes interleukin-17 responses in humans with chronic mucocutaneous candidiasis. Immunity. 39:676–686. 10.1016/j.immuni.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronner S.M., Zbieg J.R., and Crawford J.J.. 2017. RORγ antagonists and inverse agonists: a patent review. Expert Opin. Ther. Pat. 27:101–112. 10.1080/13543776.2017.1236918 [DOI] [PubMed] [Google Scholar]
- Brucklacher-Waldert V., Steinbach K., Lioznov M., Kolster M., Hölscher C., and Tolosa E.. 2009. Phenotypical characterization of human Th17 cells unambiguously identified by surface IL-17A expression. J. Immunol. 183:5494–5501. 10.4049/jimmunol.0901000 [DOI] [PubMed] [Google Scholar]
- Brüggen M.C., Bauer W.M., Reininger B., Clim E., Captarencu C., Steiner G.E., Brunner P.M., Meier B., French L.E., and Stingl G.. 2016. In Situ Mapping of Innate Lymphoid Cells in Human Skin: Evidence for Remarkable Differences between Normal and Inflamed Skin. J. Invest. Dermatol. 136:2396–2405. 10.1016/j.jid.2016.07.017 [DOI] [PubMed] [Google Scholar]
- Burstein V.L., Guasconi L., Beccacece I., Theumer M.G., Mena C., Prinz I., Cervi L., Herrero M., Masih D.T., and Chiapello L.S.. 2018. IL-17-Mediated Immunity Controls Skin Infection and T Helper 1 Response during Experimental Microsporum canis Dermatophytosis. J. Invest. Dermatol. 138:1744–1753. 10.1016/j.jid.2018.02.042 [DOI] [PubMed] [Google Scholar]
- Chang S.H., Park H., and Dong C.. 2006. Act1 adaptor protein is an immediate and essential signaling component of interleukin-17 receptor. J. Biol. Chem. 281:35603–35607. 10.1074/jbc.C600256200 [DOI] [PubMed] [Google Scholar]
- Cho J.S., Pietras E.M., Garcia N.C., Ramos R.I., Farzam D.M., Monroe H.R., Magorien J.E., Blauvelt A., Kolls J.K., Cheung A.L., et al. . 2010. IL-17 is essential for host defense against cutaneous Staphylococcus aureus infection in mice. J. Clin. Invest. 120:1762–1773. 10.1172/JCI40891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang S.Y., Lin C.H., Sung C.T., and Fang J.Y.. 2018. Murine models of psoriasis and their usefulness for drug discovery. Expert Opin. Drug Discov. 13:551–562. 10.1080/17460441.2018.1463214 [DOI] [PubMed] [Google Scholar]
- Cohen J.A., Edwards T.N., Liu A.W., Hirai T., Jones M.R., Wu J., Li Y., Zhang S., Ho J., Davis B.M., et al. . 2019. Cutaneous TRPV1+ Neurons Trigger Protective Innate Type 17 Anticipatory Immunity. Cell. 178:919–932.e14. 10.1016/j.cell.2019.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti H.R., Shen F., Nayyar N., Stocum E., Sun J.N., Lindemann M.J., Ho A.W., Hai J.H., Yu J.J., Jung J.W., et al. . 2009. Th17 cells and IL-17 receptor signaling are essential for mucosal host defense against oral candidiasis. J. Exp. Med. 206:299–311. 10.1084/jem.20081463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croxford A.L., Karbach S., Kurschus F.C., Wörtge S., Nikolaev A., Yogev N., Klebow S., Schüler R., Reissig S., Piotrowski C., et al. . 2014. IL-6 regulates neutrophil microabscess formation in IL-17A-driven psoriasiform lesions. J. Invest. Dermatol. 134:728–735. 10.1038/jid.2013.404 [DOI] [PubMed] [Google Scholar]
- Dutzan N., Abusleme L., Bridgeman H., Greenwell-Wild T., Zangerle-Murray T., Fife M.E., Bouladoux N., Linley H., Brenchley L., Wemyss K., et al. . 2017. On-going Mechanical Damage from Mastication Drives Homeostatic Th17 Cell Responses at the Oral Barrier. Immunity. 46:133–147. 10.1016/j.immuni.2016.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutzan N., Kajikawa T., Abusleme L., Greenwell-Wild T., Zuazo C.E., Ikeuchi T., Brenchley L., Abe T., Hurabielle C., Martin D., et al. . 2018. A dysbiotic microbiome triggers TH17 cells to mediate oral mucosal immunopathology in mice and humans. Sci. Transl. Med. 10:eaat0797 10.1126/scitranslmed.aat0797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyring-Andersen B., Geisler C., Agerbeck C., Lauritsen J.P., Gúdjonsdottir S.D., Skov L., and Bonefeld C.M.. 2014. Increased number and frequency of group 3 innate lymphoid cells in nonlesional psoriatic skin. Br. J. Dermatol. 170:609–616. 10.1111/bjd.12658 [DOI] [PubMed] [Google Scholar]
- Ecoeur F., Weiss J., Kaupmann K., Hintermann S., Orain D., and Guntermann C.. 2019. Antagonizing Retinoic Acid-Related-Orphan Receptor Gamma Activity Blocks the T Helper 17/Interleukin-17 Pathway Leading to Attenuated Pro-inflammatory Human Keratinocyte and Skin Responses. Front. Immunol. 10:577 10.3389/fimmu.2019.00577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egeberg A., Mallbris L., Gislason G., Hansen P.R., and Mrowietz U.. 2017. Risk of periodontitis in patients with psoriasis and psoriatic arthritis. J. Eur. Acad. Dermatol. Venereol. 31:288–293. 10.1111/jdv.13814 [DOI] [PubMed] [Google Scholar]
- Ekman A.K., Bivik Eding C., Rundquist I., and Enerbäck C.. 2019. IL-17 and IL-22 Promote Keratinocyte Stemness in the Germinative Compartment in Psoriasis. J. Invest. Dermatol. 139:1564–1573.e8. 10.1016/j.jid.2019.01.014 [DOI] [PubMed] [Google Scholar]
- Eyerich K., Foerster S., Rombold S., Seidl H.P., Behrendt H., Hofmann H., Ring J., and Traidl-Hoffmann C.. 2008. Patients with chronic mucocutaneous candidiasis exhibit reduced production of Th17-associated cytokines IL-17 and IL-22. J. Invest. Dermatol. 128:2640–2645. 10.1038/jid.2008.139 [DOI] [PubMed] [Google Scholar]
- Fossiez F., Djossou O., Chomarat P., Flores-Romo L., Ait-Yahia S., Maat C., Pin J.J., Garrone P., Garcia E., Saeland S., et al. . 1996. T cell interleukin-17 induces stromal cells to produce proinflammatory and hematopoietic cytokines. J. Exp. Med. 183:2593–2603. 10.1084/jem.183.6.2593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furiati S.C., Catarino J.S., Silva M.V., Silva R.F., Estevam R.B., Teodoro R.B., Pereira S.L., Ataide M., Rodrigues V. Jr., and Rodrigues D.B.R.. 2019. Th1, Th17, and Treg Responses are Differently Modulated by TNF-α Inhibitors and Methotrexate in Psoriasis Patients. Sci. Rep. 9:7526 10.1038/s41598-019-43899-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaffen S.L. 2009. Structure and signalling in the IL-17 receptor family. Nat. Rev. Immunol. 9:556–567. 10.1038/nri2586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaffen S.L., Jain R., Garg A.V., and Cua D.J.. 2014. The IL-23-IL-17 immune axis: from mechanisms to therapeutic testing. Nat. Rev. Immunol. 14:585–600. 10.1038/nri3707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganguly D., Chamilos G., Lande R., Gregorio J., Meller S., Facchinetti V., Homey B., Barrat F.J., Zal T., and Gilliet M.. 2009. Self-RNA-antimicrobial peptide complexes activate human dendritic cells through TLR7 and TLR8. J. Exp. Med. 206:1983–1994. 10.1084/jem.20090480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garzorz-Stark N., and Eyerich K.. 2019. Psoriasis Pathogenesis: Keratinocytes Are Back in the Spotlight. J. Invest. Dermatol. 139:995–996. 10.1016/j.jid.2019.01.026 [DOI] [PubMed] [Google Scholar]
- Gasslitter I., Kirsten N., Augustin M., Torz K., Mrowietz U., Eyerich K., Puig L., Hoetzenecker W., Schütz-Bergmayr M., Weger W., et al. . 2019. Successful intra-class switching among IL-17 antagonists: a multicentre, multinational, retrospective study. Arch. Dermatol. Res. 311:421–424. 10.1007/s00403-019-01907-y [DOI] [PubMed] [Google Scholar]
- Gauld S.B., Gauvin D., Olson L., Leys L., Paulsboe S., Liu Z., Edelmayer R.M., Wetter J., Salte K., Wang Y., et al. . 2018. Mechanistic and pharmacological assessment of murine IL-23 mediated psoriasiform dermatitis; implications for drug discovery. J. Dermatol. Sci. 92:45–53. 10.1016/j.jdermsci.2018.08.001 [DOI] [PubMed] [Google Scholar]
- Gerstel U., Latendorf T., Bartels J., Becker A., Tholey A., and Schröder J.M.. 2018. Hornerin contains a Linked Series of Ribosome-Targeting Peptide Antibiotics. Sci. Rep. 8:16158 10.1038/s41598-018-34467-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliet M., Conrad C., Geiges M., Cozzio A., Thürlimann W., Burg G., Nestle F.O., and Dummer R.. 2004. Psoriasis triggered by toll-like receptor 7 agonist imiquimod in the presence of dermal plasmacytoid dendritic cell precursors. Arch. Dermatol. 140:1490–1495. 10.1001/archderm.140.12.1490 [DOI] [PubMed] [Google Scholar]
- Gladiator A., Wangler N., Trautwein-Weidner K., and LeibundGut-Landmann S.. 2013. Cutting edge: IL-17-secreting innate lymphoid cells are essential for host defense against fungal infection. J. Immunol. 190:521–525. 10.4049/jimmunol.1202924 [DOI] [PubMed] [Google Scholar]
- Glatt S., Baeten D., Baker T., Griffiths M., Ionescu L., Lawson A.D.G., Maroof A., Oliver R., Popa S., Strimenopoulou F., et al. . 2018. Dual IL-17A and IL-17F neutralisation by bimekizumab in psoriatic arthritis: evidence from preclinical experiments and a randomised placebo-controlled clinical trial that IL-17F contributes to human chronic tissue inflammation. Ann. Rheum. Dis. 77:523–532. 10.1136/annrheumdis-2017-212127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon K.B., Strober B., Lebwohl M., Augustin M., Blauvelt A., Poulin Y., Papp K.A., Sofen H., Puig L., Foley P., et al. . 2018. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 392:650–661. 10.1016/S0140-6736(18)31713-6 [DOI] [PubMed] [Google Scholar]
- Gordon K.B., Armstrong A.W., Foley P., Song M., Shen Y.K., Li S., Muñoz-Elías E.J., Branigan P., Liu X., and Reich K.. 2019. Guselkumab efficacy after withdrawal is associated with suppression of serum IL-23-regulated IL-17 and IL-22 in psoriasis: VOYAGE 2 study. J. Invest. Dermatol.:S0022-202X(19)31755-5. [DOI] [PubMed] [Google Scholar]
- Gray E.E., Suzuki K., and Cyster J.G.. 2011. Cutting edge: Identification of a motile IL-17-producing gammadelta T cell population in the dermis. J. Immunol. 186:6091–6095. 10.4049/jimmunol.1100427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths C.E., Reich K., Lebwohl M., van de Kerkhof P., Paul C., Menter A., Cameron G.S., Erickson J., Zhang L., Secrest R.J., et al. UNCOVER-2 and UNCOVER-3 investigators . 2015. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. Lancet. 386:541–551. 10.1016/S0140-6736(15)60125-8 [DOI] [PubMed] [Google Scholar]
- Ha H.L., Wang H., Pisitkun P., Kim J.C., Tassi I., Tang W., Morasso M.I., Udey M.C., and Siebenlist U.. 2014. IL-17 drives psoriatic inflammation via distinct, target cell-specific mechanisms. Proc. Natl. Acad. Sci. USA. 111:E3422–E3431. 10.1073/pnas.1400513111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas J.D., González F.H., Schmitz S., Chennupati V., Föhse L., Kremmer E., Förster R., and Prinz I.. 2009. CCR6 and NK1.1 distinguish between IL-17A and IFN-gamma-producing gammadelta effector T cells. Eur. J. Immunol. 39:3488–3497. 10.1002/eji.200939922 [DOI] [PubMed] [Google Scholar]
- Haas J.D., Ravens S., Düber S., Sandrock I., Oberdörfer L., Kashani E., Chennupati V., Föhse L., Naumann R., Weiss S., et al. . 2012. Development of interleukin-17-producing γδ T cells is restricted to a functional embryonic wave. Immunity. 37:48–59. 10.1016/j.immuni.2012.06.003 [DOI] [PubMed] [Google Scholar]
- Hajishengallis G. 2014. Immunomicrobial pathogenesis of periodontitis: keystones, pathobionts, and host response. Trends Immunol. 35:3–11. 10.1016/j.it.2013.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington L.E., Hatton R.D., Mangan P.R., Turner H., Murphy T.L., Murphy K.M., and Weaver C.T.. 2005. Interleukin 17-producing CD4+ effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nat. Immunol. 6:1123–1132. 10.1038/ni1254 [DOI] [PubMed] [Google Scholar]
- Hawkes J.E., Adalsteinsson J.A., Gudjonsson J.E., and Ward N.L.. 2018. Research Techniques Made Simple: Murine Models of Human Psoriasis. J. Invest. Dermatol. 138:e1–e8. 10.1016/j.jid.2017.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He D., Wu L., Kim H.K., Li H., Elmets C.A., and Xu H.. 2006. CD8+ IL-17-producing T cells are important in effector functions for the elicitation of contact hypersensitivity responses. J. Immunol. 177:6852–6858. 10.4049/jimmunol.177.10.6852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herjan T., Hong L., Bubenik J., Bulek K., Qian W., Liu C., Li X., Chen X., Yang H., Ouyang S., et al. . 2018. IL-17-receptor-associated adaptor Act1 directly stabilizes mRNAs to mediate IL-17 inflammatory signaling. Nat. Immunol. 19:354–365. 10.1038/s41590-018-0071-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Santos N., Wiesner D.L., Fites J.S., McDermott A.J., Warner T., Wüthrich M., and Klein B.S.. 2019. Lung Epithelial Cells Coordinate Innate Lymphocytes and Immunity against Pulmonary Fungal Infection. Cell Host Microbe. 25:630 10.1016/j.chom.2019.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hueber W., Patel D.D., Dryja T., Wright A.M., Koroleva I., Bruin G., Antoni C., Draelos Z., Gold M.H., Durez P., et al. Uveitis Study Group . 2010. Effects of AIN457, a fully human antibody to interleukin-17A, on psoriasis, rheumatoid arthritis, and uveitis. Sci. Transl. Med. 2:52ra72 10.1126/scitranslmed.3001107 [DOI] [PubMed] [Google Scholar]
- Hueber W., Sands B.E., Lewitzky S., Vandemeulebroecke M., Reinisch W., Higgins P.D., Wehkamp J., Feagan B.G., Yao M.D., Karczewski M., et al. Secukinumab in Crohn’s Disease Study Group . 2012. Secukinumab, a human anti-IL-17A monoclonal antibody, for moderate to severe Crohn’s disease: unexpected results of a randomised, double-blind placebo-controlled trial. Gut. 61:1693–1700. 10.1136/gutjnl-2011-301668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishigame H., Kakuta S., Nagai T., Kadoki M., Nambu A., Komiyama Y., Fujikado N., Tanahashi Y., Akitsu A., Kotaki H., et al. . 2009. Differential roles of interleukin-17A and -17F in host defense against mucoepithelial bacterial infection and allergic responses. Immunity. 30:108–119. 10.1016/j.immuni.2008.11.009 [DOI] [PubMed] [Google Scholar]
- Ivanov S., and Lindén A.. 2009. Interleukin-17 as a drug target in human disease. Trends Pharmacol. Sci. 30:95–103. 10.1016/j.tips.2008.11.004 [DOI] [PubMed] [Google Scholar]
- Ivanov I.I., McKenzie B.S., Zhou L., Tadokoro C.E., Lepelley A., Lafaille J.J., Cua D.J., and Littman D.R.. 2006. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell. 126:1121–1133. 10.1016/j.cell.2006.07.035 [DOI] [PubMed] [Google Scholar]
- Johnston A., Fritz Y., Dawes S.M., Diaconu D., Al-Attar P.M., Guzman A.M., Chen C.S., Fu W., Gudjonsson J.E., McCormick T.S., and Ward N.L.. 2013. Keratinocyte overexpression of IL-17C promotes psoriasiform skin inflammation. J. Immunol. 190:2252–2262. 10.4049/jimmunol.1201505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karbach S., Croxford A.L., Oelze M., Schüler R., Minwegen D., Wegner J., Koukes L., Yogev N., Nikolaev A., Reißig S., et al. . 2014. Interleukin 17 drives vascular inflammation, endothelial dysfunction, and arterial hypertension in psoriasis-like skin disease. Arterioscler. Thromb. Vasc. Biol. 34:2658–2668. 10.1161/ATVBAHA.114.304108 [DOI] [PubMed] [Google Scholar]
- Kashem S.W., Riedl M.S., Yao C., Honda C.N., Vulchanova L., and Kaplan D.H.. 2015. Nociceptive Sensory Fibers Drive Interleukin-23 Production from CD301b+ Dermal Dendritic Cells and Drive Protective Cutaneous Immunity. Immunity. 43:515–526. 10.1016/j.immuni.2015.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawaguchi M., Onuchic L.F., Li X.D., Essayan D.M., Schroeder J., Xiao H.Q., Liu M.C., Krishnaswamy G., Germino G., and Huang S.K.. 2001. Identification of a novel cytokine, ML-1, and its expression in subjects with asthma. J. Immunol. 167:4430–4435. 10.4049/jimmunol.167.8.4430 [DOI] [PubMed] [Google Scholar]
- Krishnan S., Prise I.E., Wemyss K., Schenck L.P., Bridgeman H.M., McClure F.A., Zangerle-Murray T., O’Boyle C., Barbera T.A., Mahmood F., et al. . 2018. Amphiregulin-producing γδ T cells are vital for safeguarding oral barrier immune homeostasis. Proc. Natl. Acad. Sci. USA. 115:10738–10743. 10.1073/pnas.1802320115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger J.G., Ferris L.K., Menter A., Wagner F., White A., Visvanathan S., Lalovic B., Aslanyan S., Wang E.E., Hall D., et al. . 2015. Anti-IL-23A mAb BI 655066 for treatment of moderate-to-severe psoriasis: Safety, efficacy, pharmacokinetics, and biomarker results of a single-rising-dose, randomized, double-blind, placebo-controlled trial. J. Allergy Clin. Immunol. 136:116–124.e7. 10.1016/j.jaci.2015.01.018 [DOI] [PubMed] [Google Scholar]
- Kurschus F.C., and Moos S.. 2017. IL-17 for therapy. J. Dermatol. Sci. 87:221–227. 10.1016/j.jdermsci.2017.06.010 [DOI] [PubMed] [Google Scholar]
- Laidlaw B.J., Gray E.E., Zhang Y., Ramírez-Valle F., and Cyster J.G.. 2019. Sphingosine-1-phosphate receptor 2 restrains egress of γδ T cells from the skin. J. Exp. Med. 216:1487–1496. 10.1084/jem.20190114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lande R., Gregorio J., Facchinetti V., Chatterjee B., Wang Y.H., Homey B., Cao W., Wang Y.H., Su B., Nestle F.O., et al. . 2007. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature. 449:564–569. 10.1038/nature06116 [DOI] [PubMed] [Google Scholar]
- Lande R., Botti E., Jandus C., Dojcinovic D., Fanelli G., Conrad C., Chamilos G., Feldmeyer L., Marinari B., Chon S., et al. . 2014. The antimicrobial peptide LL37 is a T-cell autoantigen in psoriasis. Nat. Commun. 5:5621 10.1038/ncomms6621 [DOI] [PubMed] [Google Scholar]
- Langley R.G., Elewski B.E., Lebwohl M., Reich K., Griffiths C.E., Papp K., Puig L., Nakagawa H., Spelman L., Sigurgeirsson B., et al. FIXTURE Study Group . 2014. Secukinumab in plaque psoriasis--results of two phase 3 trials. N. Engl. J. Med. 371:326–338. 10.1056/NEJMoa1314258 [DOI] [PubMed] [Google Scholar]
- Lebwohl M., Strober B., Menter A., Gordon K., Weglowska J., Puig L., Papp K., Spelman L., Toth D., Kerdel F., et al. . 2015. Phase 3 Studies Comparing Brodalumab with Ustekinumab in Psoriasis. N. Engl. J. Med. 373:1318–1328. 10.1056/NEJMoa1503824 [DOI] [PubMed] [Google Scholar]
- Lee E., Trepicchio W.L., Oestreicher J.L., Pittman D., Wang F., Chamian F., Dhodapkar M., and Krueger J.G.. 2004. Increased expression of interleukin 23 p19 and p40 in lesional skin of patients with psoriasis vulgaris. J. Exp. Med. 199:125–130. 10.1084/jem.20030451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y.K., Turner H., Maynard C.L., Oliver J.R., Chen D., Elson C.O., and Weaver C.T.. 2009. Late developmental plasticity in the T helper 17 lineage. Immunity. 30:92–107. 10.1016/j.immuni.2008.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.S., Tato C.M., Joyce-Shaikh B., Gulen M.F., Cayatte C., Chen Y., Blumenschein W.M., Judo M., Ayanoglu G., McClanahan T.K., et al. . 2015. Interleukin-23-Independent IL-17 Production Regulates Intestinal Epithelial Permeability. Immunity. 43:727–738. 10.1016/j.immuni.2015.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lévy R., Okada S., Béziat V., Moriya K., Liu C., Chai L.Y., Migaud M., Hauck F., Al Ali A., Cyrus C., et al. . 2016. Genetic, immunological, and clinical features of patients with bacterial and fungal infections due to inherited IL-17RA deficiency. Proc. Natl. Acad. Sci. USA. 113:E8277–E8285. 10.1073/pnas.1618300114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leys L., Wang Y., Paulsboe S., Edelmayer R., Salte K., Wetter J., Namovic M., Phillips L., Dunstan R., Gauvin D., et al. . 2019. Characterization of psoriasiform dermatitis induced by systemic injection of interleukin-23 minicircles in mice. J. Dermatol. 46:482–497. 10.1111/1346-8138.14899 [DOI] [PubMed] [Google Scholar]
- Li Y., Golden J.B., Camhi M.I., Zhang X., Fritz Y., Diaconu D., Ivanco T.L., Simon D.I., Kikly K., McCormick T.S., et al. . 2018. Protection from Psoriasis-Related Thrombosis after Inhibition of IL-23 or IL-17A. J. Invest. Dermatol. 138:310–315. 10.1016/j.jid.2017.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang S.C., Long A.J., Bennett F., Whitters M.J., Karim R., Collins M., Goldman S.J., Dunussi-Joannopoulos K., Williams C.M., Wright J.F., and Fouser L.A.. 2007. An IL-17F/A heterodimer protein is produced by mouse Th17 cells and induces airway neutrophil recruitment. J. Immunol. 179:7791–7799. 10.4049/jimmunol.179.11.7791 [DOI] [PubMed] [Google Scholar]
- Linehan J.L., Harrison O.J., Han S.J., Byrd A.L., Vujkovic-Cvijin I., Villarino A.V., Sen S.K., Shaik J., Smelkinson M., Tamoutounour S., et al. . 2018. Non-classical Immunity Controls Microbiota Impact on Skin Immunity and Tissue Repair. Cell. 172:784–796.e18. 10.1016/j.cell.2017.12.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling Y., Cypowyj S., Aytekin C., Galicchio M., Camcioglu Y., Nepesov S., Ikinciogullari A., Dogu F., Belkadi A., Levy R., et al. . 2015. Inherited IL-17RC deficiency in patients with chronic mucocutaneous candidiasis. J. Exp. Med. 212:619–631. 10.1084/jem.20141065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Lu F., Pan H., Zhao Y., Wang S., Sun S., Li J., Hu X., and Wang L.. 2012. Correlation of peripheral Th17 cells and Th17-associated cytokines to the severity of carotid artery plaque and its clinical implication. Atherosclerosis. 221:232–241. 10.1016/j.atherosclerosis.2011.12.026 [DOI] [PubMed] [Google Scholar]
- Lowes M.A., Bowcock A.M., and Krueger J.G.. 2007. Pathogenesis and therapy of psoriasis. Nature. 445:866–873. 10.1038/nature05663 [DOI] [PubMed] [Google Scholar]
- Lowes M.A., Kikuchi T., Fuentes-Duculan J., Cardinale I., Zaba L.C., Haider A.S., Bowman E.P., and Krueger J.G.. 2008. Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. J. Invest. Dermatol. 128:1207–1211. 10.1038/sj.jid.5701213 [DOI] [PubMed] [Google Scholar]
- Martin B., Hirota K., Cua D.J., Stockinger B., and Veldhoen M.. 2009. Interleukin-17-producing gammadelta T cells selectively expand in response to pathogen products and environmental signals. Immunity. 31:321–330. 10.1016/j.immuni.2009.06.020 [DOI] [PubMed] [Google Scholar]
- Masson Regnault M., Konstantinou M.P., Khemis A., Poulin Y., Bourcier M., Amelot F., Bulaï Livideanu C., and Paul C.. 2017. Early relapse of psoriasis after stopping brodalumab: a retrospective cohort study in 77 patients. J. Eur. Acad. Dermatol. Venereol. 31:1491–1496. 10.1111/jdv.14387 [DOI] [PubMed] [Google Scholar]
- Maxwell J.R., Zhang Y., Brown W.A., Smith C.L., Byrne F.R., Fiorino M., Stevens E., Bigler J., Davis J.A., Rottman J.B., et al. . 2015. Differential Roles for Interleukin-23 and Interleukin-17 in Intestinal Immunoregulation. Immunity. 43:739–750. 10.1016/j.immuni.2015.08.019 [DOI] [PubMed] [Google Scholar]
- McGeachy M.J., Chen Y., Tato C.M., Laurence A., Joyce-Shaikh B., Blumenschein W.M., McClanahan T.K., O’Shea J.J., and Cua D.J.. 2009. The interleukin 23 receptor is essential for the terminal differentiation of interleukin 17-producing effector T helper cells in vivo. Nat. Immunol. 10:314–324. 10.1038/ni.1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGeachy M.J., Cua D.J., and Gaffen S.L.. 2019. The IL-17 Family of Cytokines in Health and Disease. Immunity. 50:892–906. 10.1016/j.immuni.2019.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGonagle D., Tan A.L., Watad A., and Helliwell P.. 2019. Pathophysiology, assessment and treatment of psoriatic dactylitis. Nat. Rev. Rheumatol. 15:113–122. 10.1038/s41584-018-0147-9 [DOI] [PubMed] [Google Scholar]
- McInnes I.B., Mease P.J., Kirkham B., Kavanaugh A., Ritchlin C.T., Rahman P., van der Heijde D., Landewé R., Conaghan P.G., Gottlieb A.B., et al. FUTURE 2 Study Group . 2015. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 386:1137–1146. 10.1016/S0140-6736(15)61134-5 [DOI] [PubMed] [Google Scholar]
- Mease P.J., van der Heijde D., Ritchlin C.T., Okada M., Cuchacovich R.S., Shuler C.L., Lin C.Y., Braun D.K., Lee C.H., and Gladman D.D.. SPIRIT-P1 Study Group . 2017. Ixekizumab, an interleukin-17A specific monoclonal antibody, for the treatment of biologic-naive patients with active psoriatic arthritis: results from the 24-week randomised, double-blind, placebo-controlled and active (adalimumab)-controlled period of the phase III trial SPIRIT-P1. Ann. Rheum. Dis. 76:79–87. 10.1136/annrheumdis-2016-209709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellett M., Meier B., Mohanan D., Schairer R., Cheng P., Satoh T.K., Kiefer B., Ospelt C., Nobbe S., Thome M., et al. . 2018. CARD14 Gain-of-Function Mutation Alone Is Sufficient to Drive IL-23/IL-17-Mediated Psoriasiform Skin Inflammation In Vivo. J. Invest. Dermatol. 138:2010–2023. 10.1016/j.jid.2018.03.1525 [DOI] [PubMed] [Google Scholar]
- Monin L., and Gaffen S.L.. 2018. Interleukin 17 Family Cytokines: Signaling Mechanisms, Biological Activities, and Therapeutic Implications. Cold Spring Harb. Perspect. Biol. 10:a028522 10.1101/cshperspect.a028522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos S., Mohebiany A.N., Waisman A., and Kurschus F.C.. 2019. Imiquimod-Induced Psoriasis in Mice Depends on the IL-17 Signaling of Keratinocytes. J. Invest. Dermatol. 139:1110–1117. 10.1016/j.jid.2019.01.006 [DOI] [PubMed] [Google Scholar]
- Moseley T.A., Haudenschild D.R., Rose L., and Reddi A.H.. 2003. Interleukin-17 family and IL-17 receptors. Cytokine Growth Factor Rev. 14:155–174. 10.1016/S1359-6101(03)00002-9 [DOI] [PubMed] [Google Scholar]
- Mrowietz U., Steinz K., and Gerdes S.. 2014. Psoriasis: to treat or to manage? Exp. Dermatol. 23:705–709. 10.1111/exd.12437 [DOI] [PubMed] [Google Scholar]
- Mrowietz U., Bachelez H., Burden A.D., Rissler M., Sieder C., Orsenigo R., and Chaouche-Teyara K.. 2019. Secukinumab for moderate-to-severe palmoplantar pustular psoriasis: Results of the 2PRECISE study. J. Am. Acad. Dermatol. 80:1344–1352. 10.1016/j.jaad.2019.01.066 [DOI] [PubMed] [Google Scholar]
- Mullard A. 2017. New plaque psoriasis approval carries suicide warning. Nat. Rev. Drug Discov. 16:155. [DOI] [PubMed] [Google Scholar]
- Naik S., Bouladoux N., Linehan J.L., Han S.J., Harrison O.J., Wilhelm C., Conlan S., Himmelfarb S., Byrd A.L., Deming C., et al. . 2015. Commensal-dendritic-cell interaction specifies a unique protective skin immune signature. Nature. 520:104–108. 10.1038/nature14052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash P., Kirkham B., Okada M., Rahman P., Combe B., Burmester G.R., Adams D.H., Kerr L., Lee C., Shuler C.L., and Genovese M.. SPIRIT-P2 Study Group . 2017. Ixekizumab for the treatment of patients with active psoriatic arthritis and an inadequate response to tumour necrosis factor inhibitors: results from the 24-week randomised, double-blind, placebo-controlled period of the SPIRIT-P2 phase 3 trial. Lancet. 389:2317–2327. 10.1016/S0140-6736(17)31429-0 [DOI] [PubMed] [Google Scholar]
- Nickoloff B.J. 2007. Cracking the cytokine code in psoriasis. Nat. Med. 13:242–244. 10.1038/nm0307-242 [DOI] [PubMed] [Google Scholar]
- Noack M., Beringer A., and Miossec P.. 2019. Additive or Synergistic Interactions Between IL-17A or IL-17F and TNF or IL-1β Depend on the Cell Type. Front. Immunol. 10:1726 10.3389/fimmu.2019.01726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordlohne J., Helmke A., Ge S., Rong S., Chen R., Waisman A., Haller H., and von Vietinghoff S.. 2018. Aggravated Atherosclerosis and Vascular Inflammation With Reduced Kidney Function Depend on Interleukin-17 Receptor A and Are Normalized by Inhibition of Interleukin-17A. JACC Basic Transl. Sci. 3:54–66. 10.1016/j.jacbts.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor W. Jr., Kamanaka M., Booth C.J., Town T., Nakae S., Iwakura Y., Kolls J.K., and Flavell R.A.. 2009. A protective function for interleukin 17A in T cell-mediated intestinal inflammation. Nat. Immunol. 10:603–609. 10.1038/ni.1736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okada S., Puel A., Casanova J.L., and Kobayashi M.. 2016. Chronic mucocutaneous candidiasis disease associated with inborn errors of IL-17 immunity. Clin. Transl. Immunology. 5:e114 10.1038/cti.2016.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantelyushin S., Haak S., Ingold B., Kulig P., Heppner F.L., Navarini A.A., and Becher B.. 2012. Rorγt+ innate lymphocytes and γδ T cells initiate psoriasiform plaque formation in mice. J. Clin. Invest. 122:2252–2256. 10.1172/JCI61862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papp K.A., Menter M.A., Raman M., Disch D., Schlichting D.E., Gaich C., Macias W., Zhang X., and Janes J.M.. 2016. A randomized phase 2b trial of baricitinib, an oral Janus kinase (JAK) 1/JAK2 inhibitor, in patients with moderate-to-severe psoriasis. Br. J. Dermatol. 174:1266–1276. 10.1111/bjd.14403 [DOI] [PubMed] [Google Scholar]
- Papp K., Gordon K., Thaçi D., Morita A., Gooderham M., Foley P., Girgis I.G., Kundu S., and Banerjee S.. 2018a Phase 2 Trial of Selective Tyrosine Kinase 2 Inhibition in Psoriasis. N. Engl. J. Med. 379:1313–1321. 10.1056/NEJMoa1806382 [DOI] [PubMed] [Google Scholar]
- Papp K.A., Merola J.F., Gottlieb A.B., Griffiths C.E.M., Cross N., Peterson L., Cioffi C., and Blauvelt A.. 2018b Dual neutralization of both interleukin 17A and interleukin 17F with bimekizumab in patients with psoriasis: Results from BE ABLE 1, a 12-week randomized, double-blinded, placebo-controlled phase 2b trial. J. Am. Acad. Dermatol. 79:277–286.e10. 10.1016/j.jaad.2018.03.037 [DOI] [PubMed] [Google Scholar]
- Puel A., Cypowyj S., Bustamante J., Wright J.F., Liu L., Lim H.K., Migaud M., Israel L., Chrabieh M., Audry M., et al. . 2011. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 332:65–68. 10.1126/science.1200439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian Y., Liu C., Hartupee J., Altuntas C.Z., Gulen M.F., Jane-Wit D., Xiao J., Lu Y., Giltiay N., Liu J., et al. . 2007. The adaptor Act1 is required for interleukin 17-dependent signaling associated with autoimmune and inflammatory disease. Nat. Immunol. 8:247–256. 10.1038/ni1439 [DOI] [PubMed] [Google Scholar]
- Reich K., Armstrong A.W., Foley P., Song M., Wasfi Y., Randazzo B., Li S., Shen Y.K., and Gordon K.B.. 2017. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the treatment of patients with moderate to severe psoriasis with randomized withdrawal and retreatment: Results from the phase III, double-blind, placebo- and active comparator-controlled VOYAGE 2 trial. J. Am. Acad. Dermatol. 76:418–431. 10.1016/j.jaad.2016.11.042 [DOI] [PubMed] [Google Scholar]
- Reich K., Reich J.L.K., Falk T.M., Blödorn-Schlicht N., Mrowietz U., von Kiedrowski R., Pfeiffer C., Niesmann J., Frambach Y., and Warren R.B.. 2019a Clinical response of psoriasis to subcutaneous methotrexate correlates with inhibition of cutaneous T helper 1 and 17 inflammatory pathways. Br. J. Dermatol. 181:859–862. 10.1111/bjd.18001 [DOI] [PubMed] [Google Scholar]
- Reich K., Warren R.B., Iversen L., Puig L., Pau-Charles I., Igarashi A., Ohtsuki M., Falqués M., Harmut M., Rozzo S., et al. . 2019b Long-term efficacy and safety of tildrakizumab for moderate-to-severe psoriasis: pooled analyses of two randomized phase III clinical trials (reSURFACE 1 and reSURFACE 2) through 148 weeks. Br. J. Dermatol.:bjd.18232 10.1111/bjd.18232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhardt A., Yevsa T., Worbs T., Lienenklaus S., Sandrock I., Oberdörfer L., Korn T., Weiss S., Förster R., and Prinz I.. 2016. Interleukin-23-Dependent γ/δ T Cells Produce Interleukin-17 and Accumulate in the Enthesis, Aortic Valve, and Ciliary Body in Mice. Arthritis Rheumatol. 68:2476–2486. 10.1002/art.39732 [DOI] [PubMed] [Google Scholar]
- Ribeiro M., Brigas H.C., Temido-Ferreira M., Pousinha P.A., Regen T., Santa C., Coelho J.E., Marques-Morgado I., Valente C.A., Omenetti S., et al. . 2019. Meningeal γδ T cell-derived IL-17 controls synaptic plasticity and short-term memory. Sci. Immunol. 4:eaay5199 10.1126/sciimmunol.aay5199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridaura V.K., Bouladoux N., Claesen J., Chen Y.E., Byrd A.L., Constantinides M.G., Merrill E.D., Tamoutounour S., Fischbach M.A., and Belkaid Y.. 2018. Contextual control of skin immunity and inflammation by Corynebacterium. J. Exp. Med. 215:785–799. 10.1084/jem.20171079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riol-Blanco L., Ordovas-Montanes J., Perro M., Naval E., Thiriot A., Alvarez D., Paust S., Wood J.N., and von Andrian U.H.. 2014. Nociceptive sensory neurons drive interleukin-23-mediated psoriasiform skin inflammation. Nature. 510:157–161. 10.1038/nature13199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchlin C.T., Colbert R.A., and Gladman D.D.. 2017. Psoriatic Arthritis. N. Engl. J. Med. 376:2095–2096. 10.1056/NEJMra1505557 [DOI] [PubMed] [Google Scholar]
- Rizzo H.L., Kagami S., Phillips K.G., Kurtz S.E., Jacques S.L., and Blauvelt A.. 2011. IL-23-mediated psoriasis-like epidermal hyperplasia is dependent on IL-17A. J. Immunol. 186:1495–1502. 10.4049/jimmunol.1001001 [DOI] [PubMed] [Google Scholar]
- Roark C.L., Simonian P.L., Fontenot A.P., Born W.K., and O’Brien R.L.. 2008. gammadelta T cells: an important source of IL-17. Curr. Opin. Immunol. 20:353–357. 10.1016/j.coi.2008.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Bolanos F., Gooderham M., and Papp K.. 2019. A Closer Look at the Data Regarding Suicidal Ideation and Behavior in Psoriasis Patients: The Case of Brodalumab. Skin Therapy Lett. 24:1–4. [PubMed] [Google Scholar]
- Rompoti N., Katsimbri P., Kokkalis G., Boumpas D., Ikonomidis I., Theodoropoulos K., Rigopoulos D., and Papadavid E.. 2019. Real world data from the use of secukinumab in the treatment of moderate-to-severe psoriasis, including scalp and palmoplantar psoriasis: A 104-week clinical study. Dermatol. Ther. (Heidelb.). 32:e13006. [DOI] [PubMed] [Google Scholar]
- Rouvier E., Luciani M.F., Mattéi M.G., Denizot F., and Golstein P.. 1993. CTLA-8, cloned from an activated T cell, bearing AU-rich messenger RNA instability sequences, and homologous to a herpesvirus saimiri gene. J. Immunol. 150:5445–5456. [PubMed] [Google Scholar]
- Saijo S., Ikeda S., Yamabe K., Kakuta S., Ishigame H., Akitsu A., Fujikado N., Kusaka T., Kubo S., Chung S.H., et al. . 2010. Dectin-2 recognition of alpha-mannans and induction of Th17 cell differentiation is essential for host defense against Candida albicans. Immunity. 32:681–691. 10.1016/j.immuni.2010.05.001 [DOI] [PubMed] [Google Scholar]
- Sandrock I., Reinhardt A., Ravens S., Binz C., Wilharm A., Martins J., Oberdörfer L., Tan L., Lienenklaus S., Zhang B., et al. . 2018. Genetic models reveal origin, persistence and non-redundant functions of IL-17-producing γδ T cells. J. Exp. Med. 215:3006–3018. 10.1084/jem.20181439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanford J.A., and Gallo R.L.. 2013. Functions of the skin microbiota in health and disease. Semin. Immunol. 25:370–377. 10.1016/j.smim.2013.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunte D.M., Mrowietz U., Puig L., and Zachariae C.. 2017. Candida infections in patients with psoriasis and psoriatic arthritis treated with interleukin-17 inhibitors and their practical management. Br. J. Dermatol. 177:47–62. 10.1111/bjd.15015 [DOI] [PubMed] [Google Scholar]
- Schreiber S., Colombel J.F., Feagan B.G., Reich K., Deodhar A.A., McInnes I.B., Porter B., Das Gupta A., Pricop L., and Fox T.. 2019. Incidence rates of inflammatory bowel disease in patients with psoriasis, psoriatic arthritis and ankylosing spondylitis treated with secukinumab: a retrospective analysis of pooled data from 21 clinical trials. Ann. Rheum. Dis. 78:473–479. 10.1136/annrheumdis-2018-214273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwandner R., Yamaguchi K., and Cao Z.. 2000. Requirement of tumor necrosis factor receptor-associated factor (TRAF)6 in interleukin 17 signal transduction. J. Exp. Med. 191:1233–1240. 10.1084/jem.191.7.1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senra L., Stalder R., Alvarez Martinez D., Chizzolini C., Boehncke W.H., and Brembilla N.C.. 2016. Keratinocyte-Derived IL-17E Contributes to Inflammation in Psoriasis. J. Invest. Dermatol. 136:1970–1980. 10.1016/j.jid.2016.06.009 [DOI] [PubMed] [Google Scholar]
- Sherlock J.P., Joyce-Shaikh B., Turner S.P., Chao C.C., Sathe M., Grein J., Gorman D.M., Bowman E.P., McClanahan T.K., Yearley J.H., et al. . 2012. IL-23 induces spondyloarthropathy by acting on ROR-γt+ CD3+CD4-CD8- entheseal resident T cells. Nat. Med. 18:1069–1076. 10.1038/nm.2817 [DOI] [PubMed] [Google Scholar]
- Singh S.P., Zhang H.H., Foley J.F., Hedrick M.N., and Farber J.M.. 2008. Human T cells that are able to produce IL-17 express the chemokine receptor CCR6. J. Immunol. 180:214–221. 10.4049/jimmunol.180.1.214 [DOI] [PubMed] [Google Scholar]
- Sparber F., and LeibundGut-Landmann S.. 2019. Interleukin-17 in Antifungal Immunity. Pathogens. 8:54 10.3390/pathogens8020054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparber F., De Gregorio C., Steckholzer S., Ferreira F.M., Dolowschiak T., Ruchti F., Kirchner F.R., Mertens S., Prinz I., Joller N., et al. . 2019. The Skin Commensal Yeast Malassezia Triggers a Type 17 Response that Coordinates Anti-fungal Immunity and Exacerbates Skin Inflammation. Cell Host Microbe. 25:389–403.e6. 10.1016/j.chom.2019.02.002 [DOI] [PubMed] [Google Scholar]
- Starnes T., Robertson M.J., Sledge G., Kelich S., Nakshatri H., Broxmeyer H.E., and Hromas R.. 2001. Cutting edge: IL-17F, a novel cytokine selectively expressed in activated T cells and monocytes, regulates angiogenesis and endothelial cell cytokine production. J. Immunol. 167:4137–4140. 10.4049/jimmunol.167.8.4137 [DOI] [PubMed] [Google Scholar]
- Sumaria N., Roediger B., Ng L.G., Qin J., Pinto R., Cavanagh L.L., Shklovskaya E., Fazekas de St Groth B., Triccas J.A., and Weninger W.. 2011. Cutaneous immunosurveillance by self-renewing dermal gammadelta T cells. J. Exp. Med. 208:505–518. 10.1084/jem.20101824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton C.E., Lalor S.J., Sweeney C.M., Brereton C.F., Lavelle E.C., and Mills K.H.. 2009. Interleukin-1 and IL-23 induce innate IL-17 production from gammadelta T cells, amplifying Th17 responses and autoimmunity. Immunity. 31:331–341. 10.1016/j.immuni.2009.08.001 [DOI] [PubMed] [Google Scholar]
- Svecova D., Lubell M.W., Casset-Semanaz F., Mackenzie H., Grenningloh R., and Krueger J.G.. 2019. A randomized, double-blind, placebo-controlled phase 1 study of multiple ascending doses of subcutaneous M1095, an anti-interleukin 17A/F nanobody, in moderate-to-severe psoriasis. J. Am. Acad. Dermatol. 81:196–203. 10.1016/j.jaad.2019.03.056 [DOI] [PubMed] [Google Scholar]
- Swindell W.R., Johnston A., Carbajal S., Han G., Wohn C., Lu J., Xing X., Nair R.P., Voorhees J.J., Elder J.T., et al. . 2011. Genome-wide expression profiling of five mouse models identifies similarities and differences with human psoriasis. PLoS One. 6:e18266 10.1371/journal.pone.0018266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan L., Sandrock I., Odak I., Aizenbud Y., Wilharm A., Barros-Martins J., Tabib Y., Borchers A., Amado T., Gangoda L., et al. . 2019. Single-Cell Transcriptomics Identifies the Adaptation of Scart1+ Vγ6+ T Cells to Skin Residency as Activated Effector Cells. Cell Reports. 27:3657–3671.e4. 10.1016/j.celrep.2019.05.064 [DOI] [PubMed] [Google Scholar]
- Tanaka H., Arima Y., Kamimura D., Tanaka Y., Takahashi N., Uehata T., Maeda K., Satoh T., Murakami M., and Akira S.. 2019. Phosphorylation-dependent Regnase-1 release from endoplasmic reticulum is critical in IL-17 response. J. Exp. Med. 216:1431–1449. 10.1084/jem.20181078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teunissen M.B., Koomen C.W., de Waal Malefyt R., Wierenga E.A., and Bos J.D.. 1998. Interleukin-17 and interferon-gamma synergize in the enhancement of proinflammatory cytokine production by human keratinocytes. J. Invest. Dermatol. 111:645–649. 10.1046/j.1523-1747.1998.00347.x [DOI] [PubMed] [Google Scholar]
- Uluçkan Ö., Jimenez M., Karbach S., Jeschke A., Graña O., Keller J., Busse B., Croxford A.L., Finzel S., Koenders M., et al. . 2016. Chronic skin inflammation leads to bone loss by IL-17-mediated inhibition of Wnt signaling in osteoblasts. Sci. Transl. Med. 8:330ra37 10.1126/scitranslmed.aad8996 [DOI] [PubMed] [Google Scholar]
- van der Fits L., Mourits S., Voerman J.S., Kant M., Boon L., Laman J.D., Cornelissen F., Mus A.M., Florencia E., Prens E.P., and Lubberts E.. 2009. Imiquimod-induced psoriasis-like skin inflammation in mice is mediated via the IL-23/IL-17 axis. J. Immunol. 182:5836–5845. 10.4049/jimmunol.0802999 [DOI] [PubMed] [Google Scholar]
- van der Heijde D., Cheng-Chung Wei J., Dougados M., Mease P., Deodhar A., Maksymowych W.P., Van den Bosch F., Sieper J., Tomita T., Landewé R., et al. COAST-V study group . 2018. Ixekizumab, an interleukin-17A antagonist in the treatment of ankylosing spondylitis or radiographic axial spondyloarthritis in patients previously untreated with biological disease-modifying anti-rheumatic drugs (COAST-V): 16 week results of a phase 3 randomised, double-blind, active-controlled and placebo-controlled trial. Lancet. 392:2441–2451. 10.1016/S0140-6736(18)31946-9 [DOI] [PubMed] [Google Scholar]
- Villanova F., Flutter B., Tosi I., Grys K., Sreeneebus H., Perera G.K., Chapman A., Smith C.H., Di Meglio P., and Nestle F.O.. 2014. Characterization of innate lymphoid cells in human skin and blood demonstrates increase of NKp44+ ILC3 in psoriasis. J. Invest. Dermatol. 134:984–991. 10.1038/jid.2013.477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinter H., Iversen L., Steiniche T., Kragballe K., and Johansen C.. 2015. Aldara®-induced skin inflammation: studies of patients with psoriasis. Br. J. Dermatol. 172:345–353. 10.1111/bjd.13236 [DOI] [PubMed] [Google Scholar]
- von Stebut E., Reich K., Thaçi D., Koenig W., Pinter A., Körber A., Rassaf T., Waisman A., Mani V., Yates D., et al. . 2019. Impact of Secukinumab on Endothelial Dysfunction and Other Cardiovascular Disease Parameters in Psoriasis Patients over 52 Weeks. J. Invest. Dermatol. 139:1054–1062. 10.1016/j.jid.2018.10.042 [DOI] [PubMed] [Google Scholar]
- Wang M., Zhang S., Zheng G., Huang J., Songyang Z., Zhao X., and Lin X.. 2018. Gain-of-Function Mutation of Card14 Leads to Spontaneous Psoriasis-like Skin Inflammation through Enhanced Keratinocyte Response to IL-17A. Immunity. 49:66–79.e5. 10.1016/j.immuni.2018.05.012 [DOI] [PubMed] [Google Scholar]
- Weaver C.T., Hatton R.D., Mangan P.R., and Harrington L.E.. 2007. IL-17 family cytokines and the expanding diversity of effector T cell lineages. Annu. Rev. Immunol. 25:821–852. 10.1146/annurev.immunol.25.022106.141557 [DOI] [PubMed] [Google Scholar]
- Wilharm A., Tabib Y., Nassar M., Reinhardt A., Mizraji G., Sandrock I., Heyman O., Barros-Martins J., Aizenbud Y., Khalaileh A., et al. . 2019. Mutual interplay between IL-17-producing γδT cells and microbiota orchestrates oral mucosal homeostasis. Proc. Natl. Acad. Sci. USA. 116:2652–2661. 10.1073/pnas.1818812116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wüthrich M., Gern B., Hung C.Y., Ersland K., Rocco N., Pick-Jacobs J., Galles K., Filutowicz H., Warner T., Evans M., et al. . 2011. Vaccine-induced protection against 3 systemic mycoses endemic to North America requires Th17 cells in mice. J. Clin. Invest. 121:554–568. 10.1172/JCI43984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Z., Painter S.L., Fanslow W.C., Ulrich D., Macduff B.M., Spriggs M.K., and Armitage R.J.. 1995. Human IL-17: a novel cytokine derived from T cells. J. Immunol. 155:5483–5486. [PubMed] [Google Scholar]
- Zepp J.A., Zhao J., Liu C., Bulek K., Wu L., Chen X., Hao Y., Wang Z., Wang X., Ouyang W., et al. . 2017. IL-17A-Induced PLET1 Expression Contributes to Tissue Repair and Colon Tumorigenesis. J. Immunol. 199:3849–3857. 10.4049/jimmunol.1601540 [DOI] [PMC free article] [PubMed] [Google Scholar]