Abstract
Background:
Professional treatment and non-professional mutual-help organizations (MHOs) play important roles in mitigating addiction relapse risk. More recently, a third tier of recovery support services has emerged that are neither treatment nor MHO that encompass an all-inclusive flexible approach combining professionals and volunteers. The most prominent of these is Recovery Community Centers (RCCs). RCC’s goal is to provide an attractive central recovery hub facilitating the accrual of recovery capital by providing a variety of services (e.g., recovery coaching; medication assisted treatment [MAT] support, employment/educational linkages). Despite their growth, little is known formally about their structure and function. Greater knowledge would inform the field about their potential clinical and public health utility.
Method:
On-site visits (2015–2016) to RCCs across the northeastern U.S. (K=32) with semi-structured interviews conducted with RCC directors and online surveys with staff assessing RCCs’: physicality and locality; operations and budgets; leadership and staffing; membership; and services.
Results:
Physicality and locality: RCCs were mostly in urban/suburban locations (90%) with very good to excellent Walk Scores reflecting easy accessibility. Ratings of environmental quality indicated neighborhood/grounds/buildings were moderate-good attractiveness and quality. Operations: RCCs had been operating for an average of 8.5 years (SD=6.2; range 1–33 years) with budgets (mostly state-funded) ranging from $17,000-$760,000/year, serving anywhere from a dozen to more than two thousand visitors/month. Leadership and Staffing: Center directors were mostly female (55%) with primary drug histories of alcohol (62%), cocaine (19%), or opioids (19%). Most, but not all, directors (90%) and staff (84%) were in recovery. Membership: A large proportion of RCC visitors were male (61%), White (72%), unemployed (50%), criminal-justice system-involved (43%) and reported opioids (35%) or alcohol (33%) as their primary substance. Roughly half were in their first year of recovery (49%), but about 20% had five or more years. Services: RCCs reported a range of services including social/recreational (100%), mutual-help (91%), recovery coaching (77%), and employment (83%) and education (63%) assistance. Medication-assisted treatment (MAT) support (43%) and overdose reversal training (57%) were less frequently offered, despite being rated as highly important by staff.
Conclusions:
RCCs are easily accessible, attractive, mostly state-funded, recovery support hubs providing an array of services to individuals in various recovery stages. They appear to play a valued role in facilitating the accrual of social, employment, housing, and other recovery capital. Research is needed to understand the relative lack of opioid-specific support and to determine their broader impact in initiating and sustaining remission and cost-effectiveness.
Keywords: recovery community centers, recovery, addiction, support services, recovery coaching, addiction, substance use disorder
Introduction
Substance use disorders (SUD) are among the most intransigent and pervasive public health problems in most middle- and high-income countries globally. Consequences transcend the health sector into the justice system, nations’ economies, and the safety and social fabric of communities (National Drug Intelligence Center, 2011; Savidge & Stein, 2012; World Health Organization. Management of Substance Abuse Team, 2011). While some suffering from these disorders are able to achieve remission without seeking help from formal treatment (Cunningham, 1999; Kelly, 2017), those with more severe and complex problems seek help through some combination of formal treatment and/or longer-term mutual help organization participation (Kelly & White, 2012). Research suggests that the majority of people with a substance use disorder (SUD) do in fact achieve full remission (Sheedy & Whitter, 2009; White, 2012), however, despite the use of both formal and informal intervention services, the road to long-term recovery is often oscillatory, characterized by periods of relapse, treatment, incarceration, and short-term remission (White, 2012), especially for those with greater addiction severity and fewer recovery resources (Kelly et al, 2019). In response to this, the field has developed, tested, and implemented service models that incorporate long-term continuing care elements often described as recovery support services (Kelly & White, 2011; Scott & Dennis, 2009).
Many of these recovery support services provide options beyond the medical stabilization of addiction to address the psychosocial barriers to sustained remission (White, 2009). The most prevalent of these recovery support services are residential recovery homes (e.g., Oxford Houses, (Jason & Ferrari, 2010)); however, more recently, recovery community centers (RCCs) have emerged as the second most common source of community recovery support and are growing rapidly (Cousins, Antonini, & Rawson, 2012). RCCs are literally and metaphorically, “new kids on the block”, as these novel entities are most often located on city blocks within the heart of communities and provide a variety of services including recovery coaching, medication assisted treatment (MAT) support, relapse prevention skills-building and mutual-help groups, employment linkages, and a host of other support programs intended for people in or seeking recovery. They are purported to be operated most often by peer volunteers and occasionally addiction professionals (Cousins et al., 2012).
Conceptually, RCCs are innovative in that they are founded on the principle that the achievement of sustained recovery from alcohol or other drug use disorders is not just a function of medical stabilization (e.g., detoxification) or addressing psychopathology, but also by providing and successfully mobilizing personal, social, environmental, and cultural resources that can be brought to bear on recovery. The total aggregate of these resources has been termed, “recovery capital” (Cloud & Granfield, 2008)”. From a stress and coping theoretical perspective (Lazarus & Folkman, 1984), the greater the availability of, and access to, recovery capital, the greater the likelihood individuals will be able to buffer stress associated with the adaptations needed to sustain stable remission (Kelly and Hoeppner, 2016).
RCCs play a unique role not played by professional care or mutual help organizations (MHOs), such as SMART Recovery, Alcoholics Anonymous (AA), or Narcotics Anonymous (NA), since RCCs provide different services than addiction treatment, and offer more formal and tangible linkages to social services, employment, training, and educational agencies than do mutual-help organizations (Valentine, 2011). Consequently, they are considered to be a “third tier” addition to the existing two-tier professional treatment and MHO entities. Importantly, one of the principles of RCCs is that there are many pathways to recovery; RCCs are not allied with any specific recovery philosophy or model (e.g., 12-step; cognitive-behavioral; religious; secular) and thus are all-inclusive and “agnostic” when it comes to recovery approaches (Valentine, 2011). This is a critically important aspect of these facilities in a field where partisan approaches can create unnecessary barriers to recovery for some (Kelly & White, 2012).
RCCs arise out of the recognition that individuals in, and seeking, recovery from chronically relapsing substance-related conditions, need ongoing support and recovery capital, and their broad recovery philosophy and growing presence and utilization would suggest many individuals may benefit from their presence in ways similar to other recovery support services, such as recovery housing and mutual-help organizations (Humphreys & Moos, 2001; Humphreys & Moos, 2007; Jason & Ferrari, 2010). Yet, despite their growth, RCCs have not been subjected to any systematic study. By characterizing RCCs and the individuals who use them, we may begin to identify components that might contribute to RCCs as viable and effective entities. Such evidence can begin to inform national efforts by providing a model or blueprint for further development of RCCs.
As a first step in this effort to gather more systematic research, the present investigation assessed the characteristics of RCCs across the northeastern region of the U.S. We sought to begin to answer several basic questions: what and where are they; how do they operate; who is running them; who is using them; and what are they providing. Toward this end, this study describes RCCs along five dimensions: 1. Physicality and locality – the structural characteristics of RCCs, attractiveness, and where they are located; 2. Operations and Budgets – years in operation, how they are funded and staffed; 3. Leadership and Staffing –who is running RCCs; 4. Membership –who is using RCCs; and, 5. Services Provided –what RCCs are providing and the perceived importance to recovery of services provided, as rated by center staff. Finally, some exploratory inferential correlational analyses were conducted to investigate the degree of association among RCC center variables (e.g., the rated attractiveness of centers) and the degree of member utilization (6. Correlational associations among center characteristics and usage of centers).
Methods
1.1. Participants
1.1.1. Centers
Our goal was to create a comprehensive listing of RCCs operating in the New England and New York state area. Centers were identified in two ways: in states which have state-level funding for RCCs (i.e., MA, CT, VT, NY), state agencies were contacted to provide a list of existing RCCs. In states without state-level funding (i.e., NH, ME), grass-root efforts were used to obtain a comprehensive list of RCCs (e.g., through “Faces and Voices”, known recovery leaders, other RCC directors). Thirty-eight centers were contacted, all of which agreed initially to participate. Once funded (a year later), centers were re-approached to launch the study, at which point 32 centers agreed to participate.
1.1.2. Directors
A total of 30 directors participated in in-person, on-site interviews with study staff. Two directors ran 2 centers each.
1.1.3. Staff
Of 108 staff members invited to participate, 59 (55%) RCC staff members from 22 of the 32 centers completed an online survey. Centers were not represented in these surveys if they did not have any staff besides the director (k=3) or if none of the staff members completed the survey (k=7)
1.2. Procedures
1.2.1. Directors
On-site, in-person interviews with RCC directors were conducted between April 2015 and May 2016. In advance of the meeting, directors were emailed a document spanning the questions that would be addressed in the interview. This form was then reviewed and completed together with study staff at the interview. Directors received $10 remuneration for completing the interview.
1.2.2. Staff
Center directors provided study staff with email addresses of all of their RCC staff members. Study staff then emailed invitations to RCC staff to complete an online survey using REDCap electronic data capture tools (Research Electronic Data Capture; project-redcap.org) hosted by Partners HealthCare Research Computing, Enterprise Research Infrastructure & Services (ERIS) group. REDCap is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources (P. A. Harris et al., 2019; Paul A Harris et al., 2009). Repeated outreach efforts were made to get staff to complete surveys, ending in September 2016. Staff received $10 for completing the online survey.
Human Subjects Research Ethics Approval:
The human subjects ethics approval for this study was obtained from the Partners Health Care organization internal review board.
1.3. Measures
1.3.1. Physicality and Locality.
Two study staff members conducted a walk around and walk-through of all RCCs and independently used the Environmental Rating Scale (Timko, 1996) to rate the overall site location attractiveness and the characteristics and attractiveness of the interior of each center. From this scale, 3 items assessed neighborhood, grounds and buildings. A “site location attractiveness” score was calculated by averaging across the 3 items on neighborhood, grounds and buildings, which were individually rated from 0 (unattractive/unpleasant) to 3 (very pleasant and attractive), and then averaging across raters. Eight items assessed interior characteristics. The interior space items were rated separately per room, with a maximum of five areas (reception area, common area, group rooms, hallways, and staff members’ offices) rated within each site (on a 0–3 scale). Items assessed noise level, odors, level of illumination, cleanliness, condition of walls and floors, condition of furniture, windows, and attractiveness of the view from windows. Ratings for each of the eight interior space ratings were averaged across the five areas scores, then across the two raters. Lastly, 1 item assessed referability (the extent to which a rater would refer a family member with an alcohol/drug problem to the center) and overall attractiveness of the center as a whole. This single item was averaged across raters. The interrater reliability across individual items was very good ranging from r=0.77 to 0.94 (M=.88).
1.3.1.1. Accessibility.
Each RCC’s physical address was entered by research staff into the publicly available website www.walkscore.com in 2018 to obtain a Walk Score® for each site. A Walk Score describes the walking distance to amenities and pedestrian friendliness based on population density and road metrics. Scores range from zero to one-hundred and describe the site location to be a ‘walker’s paradise’ (90–100), ‘very walkable’ (70–89), ‘somewhat walkable’ (50–69), or ‘car-dependent’ (0–49) (Carr, Dunsiger, & Marcus, 2011; Walk Score Inc). RCC directors self-reported the catchment area of their center.
1.3.2. Operations and Budget.
During the in-person interviews with RCC directors, directors reported on their operations using items from the Texas Christian University (TCU) Survey of Structure and Operations scale (SSO, (Institute of Behavioral Research, 2006); see Table 2). RCC directors typically based the provided information on a combination of actual, tracked data (e.g., service user visits ascertained through a formal check-in process, detailed budget and revenue reports and/or their best estimate of these figures in the absence of documented data. For k=3 centers, budget details were not provided by the director, however, because they were state-funded sites (i.e., received a fixed funding amount); study staff were able input the total budget, and whether or not they paid staff, but we did not have more detailed information.
Table 2.
Operations of Recovery Community Centers as Reported by Center Directors (n = 29)
| M (SD) / % (n) | median | range | |
|---|---|---|---|
| Operation | |||
| Years in Operation | 8.5 (6.2) | 9 | 1–33 |
| Open Weekends and Weekdays | 71.9% (23) | - | - |
| Hours of Operation Per Week | 54.1 (19.9) | 56.3 | 6–94 |
| Total Annual Budget (in $) a | $215,104 ($156,672) | $148,200 | $16,956-$760,591 |
| Personnel/salaries costs | |||
| % of centers covering personnel costs b | 93.1% (27) | - | - |
| if yes, average amount spent on salaries c | $129,288 ($112,697) | $88,032 | $15,000-$557,541 |
| Facilities costs | |||
| % of centers covering facilities costs c | 100% (24) | - | - |
| if yes, average amount spent c | $30,033 ($18,498) | $25,250 | $8,475-$96,217 |
| Staff d (in number of) | |||
| Paid Staff | 3.9 (2.7) | 3 | 0–12 |
| Volunteer Staff | 3.0 (5.8) | 0 | 0–19 |
| Full Time Staff | 2.4 (2) | 2 | 0–8 |
| Part Time Staff | 3.4 (4.8) | 2 | 0–20 |
| Staff hired in the last 6 months e | 1.1 (1.2) | 1 | 0–4 |
| Staff who left the center in the last 6 months e | 0.6 (0.9) | 0 | 0–3 |
| Staff who have less than 2 years with center e | 2.7 (2.8) | 1.5 | 0–12 |
| Staff who have 2–5 years with center e | 1.6 (1.7) | 1 | 0–7 |
| Staff who have more than 5 years with center e | 1.1 (2.2) | 0 | 0–11 |
| Service User Visits f | |||
| Monthly Visits from Unique Service Users | 252.6 (416.0) | 125 | 13–2,200 |
| Monthly Visits from Service Users in Total | 1366.2 (1127.3) | 1050 | 113–5,250 |
| Hours a Service User Spends at Center Per Visit | 2.4 (1.1) | 2 | 1–5 |
| Service Users Per Day | 46 (37.1) | 34 | 6–175 |
| New Service Users Per Month | 26.5 (33.0) | 16.5 | 3–150 |
Note: M = mean, SD = standard deviation of the mean, n = number of centers who endorsed “yes”;
based on n=28, because 1 center did not provide any budget information;
based on n=29, using director reports on having paid staff;
based on n=24, as 4 centers did not provide breakdown of total budget;
reported by 29 directors, as 3 center dyads existed, which shared staff between centers;
one center did not report these breakdowns;
14 centers reported service users visits from enrollment records and others were estimates.
1.3.3. Leadership and Staffing
1.3.3.1. Demographics.
Directors and staff were asked to report their age, race, ethnicity, and education using items from the TCU SSO (Institute of Behavioral Research, 2006).
1.3.3.2. Substance use history.
Given the peer-support emphasis of RCCs, directors and staff were asked about their own substance use history. Directors and staff were asked if they considered themselves to be in recovery (yes/no). Directors were asked about their substance use in an open-ended fashion, while staff were provided with a multiple-choice survey item.
1.3.3.3. Employment history.
Using items from the TCU SSO (Institute of Behavioral Research, 2006), directors and staff indicated the number of years employed at their current position, at the center, and in the addiction field. Staff were also asked to provide the number of hours worked per week, and whether they were paid or unpaid.
1.3.4. Member Characteristics.
RCC directors reported on the characteristics of the members they served using items from the TCU SSO regarding demographics, legal status, and substance use history.
1.3.4.1. Referral source.
Directors were asked to estimate through which referral pathways RCC members came to the center. This included referral sources such as, treatment settings, the criminal justice system, shelters, self-referrals, or another referral source.
1.3.5. Services Provided.
Starting with a list of services from the TCU SSO (Institute of Behavioral Research, 2006), study staff asked directors to indicate which listed services, and what additional services, if any, were offered at their RCC. As the original list of services was pre-populated based mostly on clinical treatment services outlined in the TCU SSO, the list was modified, and services were added and removed to reflect the nature of RCCs. Following the completion of all center visits, a revised list of services offered was compiled based on the director reports and center materials provided (i.e., meeting/event calendars; brochures), which removed any formal services originally listed that were not reported to have been provided at any center (e.g., individual or group treatment/counseling, biological testing), and instead added the emergent informal center services (e.g., recovery coaching, Medication Assisted Treatment [MAT] support groups). This list was included also in the staff survey, in which RCC staff were asked, “Of the services offered at [your RCC], how important do you believe each service is for your members’ recovery?”, which they answered on a 1–7 scale, with anchored values at 1 (not at all important), 4 (moderately important), and 7 (extremely important).
Results
1.4. Physicality and Locality
The visited RCCs were diverse in size, appearance and setting (Table 1). Based on the environmental ratings scale, the outward appearance of the centers ranged from fairly unattractive to very attractive, but on average were rated on the slightly higher end of the spectrum by the two study staff members, who independently rated overall site location with an average rating of 1.7 (SD=0.6; “somewhat pleasant”). RCCs typically consisted of 3 rooms, with an average of 4.4 (SD=0.7) types of rooms. On average the indoor appearance of the centers was rated as “quiet”, “clean”, “good”, and free of odors. Lowest ratings were given for access to windows and view from the windows. The vast majority of the 32 centers were easily accessible (81.3%), with walk-scores of “very walkable” (62.5%) and “extremely walkable” (18.8%). RCCs were typically reported as being located in urban population centers (63.3%).
Table 1.
Physicality and locality of Recovery Community Centers (N = 32)
| Observation | mean/% | (SD)/(n) | range |
|---|---|---|---|
| Site Location Attractiveness (neighborhood, grounds, buildings) a | 1.5 | (0.6) | 0.3–2.5 |
| Number of types of rooms (i.e., 1–5, reception, common, group, hallways, staff office) b | 4.5 | (0.7) | 3–5 |
| Quality of the RCC interior space c | |||
| Noise Level | 2.2 | (0.6) | 1–3 |
| Odors | 2.1 | (0.5) | 0.8–3 |
| Illumination | 2.4 | (0.4) | 1.8–3 |
| Cleanliness of Walls and Floors | 2.1 | (0.6) | 1–3 |
| Condition of Walls and Floors | 2.0 | (0.6) | 0.8–3 |
| Condition of Furniture | 1.9 | (0.6) | 0.8–3 |
| Window Area | 1.5 | (0.6) | 0–3 |
| View from Windows (Attractiveness) | 1.2 | (0.6) | 0–2.8 |
| Total score for the quality of the RCC interior space | 1.9 | (0.4) | 1.3–2.8 |
| Overall study-staff rated appeal | |||
| Recommendability / Referrability | 2.5 | (0.5) | 1.5–3 |
| Attractiveness of the Program | 2.3 | (0.7) | 1–3 |
| Accessibility (in Walk Scores, %) | |||
| Extremely Walkable | 18.8 | (6) | |
| Very Walkable | 62.5 | (20) | |
| Somewhat Walkable | 6.3 | (2) | |
| Car-Dependent | 12.5 | (4) | |
| Catchment Area (in %) d | |||
| Rural | 26.7 | (8) | |
| Suburban | 26.7 | (8) | |
| Urban | 63.3 | (19) |
Note:
average of 3 items, where two study staff independently rated neighborhood, grounds and building on a 0–3 scale, ranging from 0 (unattractive/unpleasant) to 3 (very pleasant and attractive);
counted by study staff;
rated independently by 2 study staff members on a 0–3 scale, where 0 represented poor quality (e.g., moderately objectionable odor; inadequate lighting) and 3 represented excellent quality (e.g., very quiet;, very attractive); displayed scores were first averaged across types of rooms within center, then averaged across two independent research staff raters (average r between raters = 0.88, ranging from 0.77 for ‘odor’ to 0.94 for ‘window area’);
as reported by RCC directors.
1.5. Operations and Budget.
Centers also differed widely in indices capturing their operation (Table 2). Some centers had been in operation for several years; others had just opened. The median number of years in operation was 9 (range = 1–33 years). On average, centers were open for 54.1 (SD=19.9) hours per week, with some centers only open for a select few hours during the week, for specific group meetings, and others providing services up to 94 hours per week. Center budgets differed widely, from $17,000 to $761,000 per year. A relatively small portion of these budgets were spent on facilities (i.e., rent, heat, utilities, insurance), on average $30,000, though some centers did not provide detailed budgets, and thus it is difficult to compare the relative allocation of resources. Surprisingly, most directors reported that their centers operated without any formal volunteer staff (69%), though those centers who did use volunteer staff, did so extensively, with an average of 9.6 (7.0) volunteer staff per center. Paid staff, overall, were more common with 93.1% of centers having at least 1 paid staff member, with an average of 4.2 (2.6) paid staff members per center. Many centers had full-time staff (79.3%), with on average 3.0 (1.7) full-time staff members per center. Staff turn-over was common, with 42.8% of centers reporting a staff member had left within the past 6 months.
The median number of unique individuals who visited a center in a month was 125; the range was very wide, from 13 unique individuals per month utilizing a center to 2,200 (this upper limit was not an estimate but documented by swipe-in ID cards). On average, visitors spent 2.4 (1.1) hours at the center per visit.
1.6. Leadership and Staffing
Approximately just over half to two-thirds of RCC staff (including directors) were women and most were middle-aged; the vast majority were White. Most, but not all, directors (90%) and staff (84%) themselves were in recovery from an alcohol or other drug problem, with directors having longer recovery histories than their staffs, and more commonly having had alcohol as their primary substance (Table 3). As would be expected, center directors had longer employment histories at their centers than their staff. Center directors and staff were similar on demographics, with directors tending to be a little bit older, more educated, and more commonly certified or licensed to provide addiction support (Table 3).
Table 3.
Director and Staff Characteristics of Recovery Community Centers: Demographics, Substance Use History, and Employment History
| Directors n=30 a |
Staff n=59 b |
|
|---|---|---|
| Characteristic | M (SD) / % (n) | M (SD) / % (n) |
| Demographics | ||
| Age | 55.1 (8.7) | 48.7 (13.8) |
| Female c | 53.3% (16) | 69.0% (40) |
| Race | ||
| White | 86.7% (26) | 86.4% (51) |
| Black or African American | 13.3% (4) | 10.2% (6) |
| Other | 0% (0) | 3.4% (2) |
| Ethnicity Latino or Hispanic (% yes) | 3.3% (1) | 10.71% (6) |
| Education | ||
| High school diploma/GED or less | 6.7% (2) | 8.5% (5) |
| Any college (bachelors or some college) | 26.7% (8) | 49.2% (29) |
| Graduate degree (e.g., masters, doctorate) | 33.3% (10) | 16.9% (10) |
| Other professional degree (e.g., LADC) / Associates | 33.3% (10) | 25.4% (15) |
| Certification in Addiction Field | ||
| Currently certified or licensed | 40% (12) | 19.0% (11) |
| Not certified or licensed in addiction | 50% (15) | 75.9% (44) |
| Previously certified or licensed, not current | 10% (3) | 5.1% (3) |
| Substance Use History | ||
| In Recovery | 90.0% (27) | 84.2% (48) |
| Years in Recovery c | 18.6 (10) | 10.2 (8.3) |
| Primary Substance | ||
| Alcohol | 61.6% (16) | 39.1% (18) |
| Opioids | 19.2% (5) | 37.0% (17) |
| Cocaine | 19.2% (5) | 19.6% (9) |
| Amphetamines & Methamphetamines | 0% (0) | 0% (0) |
| Cannabis | 0% (0) | 2.2% (1) |
| Other | 0% (0) | 2.2% (1) |
| Secondary Substance | ||
| Alcohol | 27.2% (6) | 27.8% (10) |
| Opioids | 0% (0) | 22.2% (8) |
| Cocaine | 22.7% (5) | 22.2% (8) |
| Amphetamines & Methamphetamines | 4.6% (1) | 0% (0) |
| Cannabis | 36.4% (8) | 19.4% (7) |
| Other | 9.1% (2) | 8.3% (3) |
| Employment History | ||
| Years Worked at Current Position d | 3.8 (4.3) | 1.9 (1.7) |
| Years Worked at Center e | 5.2 (4.9) | 3 (2.1) |
| Years Worked in Addiction Treatment and Recovery Field f | 13.5 (8.4) | 6.9 (7.7) |
| Specialist in Addictions (% yes) | - | 69.5% (41) |
| Employment | ||
| Paid, full-time (35+ hrs weekly) | - | 39.3% (22) |
| Paid, part-time (under 35 hrs weekly) | - | 33.9% (19) |
| Unpaid, full-time (35+ hrs weekly) | - | 0% (0) |
| Unpaid, part-time (under 35 hours weekly) | - | 26.8% (15) |
Note: M = mean, SD = standard deviation of the mean;
2 directors managed 2 centers each;
from 21 centers;
1 staff identified as transgender.
1.7. Membership
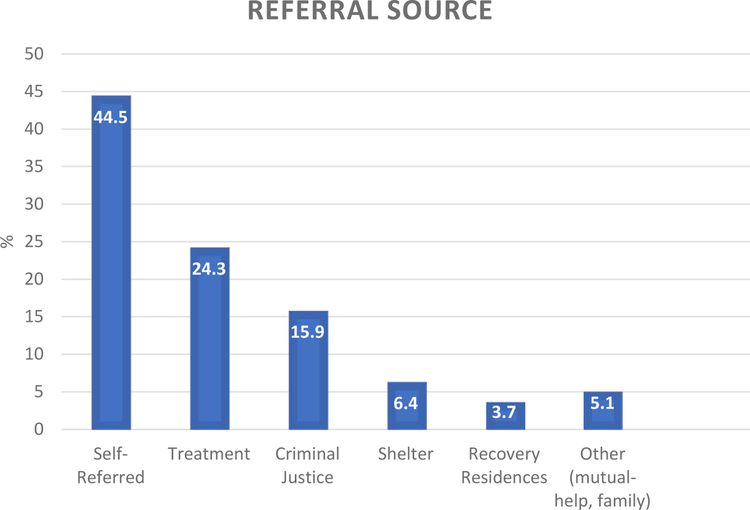
Whereas RCC staff tended to be comprised of more women (53% of directors, 69% of staff), only a minority of center visitors were women (39.3% ± 13.4). Roughly one in four RCC members were in the emerging adult age range (22.6%; i.e., under age 25 years old), though the majority were estimated to be between 25–59 years of age (65%). Most RCC members were estimated to have no more than a high school degree or less (76%), and half were unemployed (50%). Almost half (42.7%) had some kind of current legal system involvement. Despite this however, the biggest referral sources were estimated to be self-referral (e.g., word-of-mouth, 45%), and treatment programs (24.3%), with criminal justice playing a comparatively smaller referral role (15.9%) (Figure 1). In terms of the substances that RCC members used, the majority reported either alcohol (33%) or opioids (35%) as their primary substance (see Figure 2). In terms of time in recovery, the modal length of time was between 0–6 months (31.4%) but nearly half of RCC service users (48.9%) were in their first year of recovery. Also, RCCs were being used by many in the early phases of recovery beyond the first year (years 1–5; 27.1%) and roughly an additional one in five were using the centers despite longer-term stable recovery of greater than 5 years (19.8%). Of note, approximately 5% were still actively using substances but accessing centers.
Figure 1.
Reported Referral Source for Centers
Figure 2.
Years in Recovery and Primary Substance by Center Service Users
1.8. Services Provided
The most common services centers offered (Table 5) were substance-free social events (100%), meetings for known mutual-help organizations such as AA (97%), family support services (87%), employment assistance (83%), health-behavior programs (83%), and organically grown, center-specific, peer-facilitated support groups (77%) and recovery coaching (77%). Very few centers offered child care services (10%), legal support (17%) or financial services (23%). Importance ratings, as rated by staff, matched up with availability of services to quite a large degree (r=.74, p<.05) with some notable exceptions. Staff felt that the most important services to aid addiction recovery for RCC participants were meetings for known mutual-help groups (rated on average as 6.6 on a 1–7 scale of importance), other peer facilitated groups (6.6), and substance-free recreational activities (6.3). These services were both most common and judged to be most important. By contrast, NARCAN training was rated as very important by staff (6.3±1.2) but was comparatively infrequently offered (by 57% of centers), as was medication-assisted treatment (MAT) support (5.9±1.6), but again was less frequently offered (43.3% of centers). Similarly, mental health support (e.g., dual-diagnosis support groups) was rated as important by staff (6.1±1.0), but infrequently offered (only 37% of centers). Conversely, employment assistance was rated relatively lower in importance by staff (5.9±1.2), but very frequently offered (83%). Health behavior support (e.g., physical fitness; yoga etc.) as well was frequently offered (83%), but not as valued by staff (5.7±1.3). Lowest importance ratings (though still above 4 (moderately important)), were ascribed to child care services, legal assistance and smoking cessation support.
Table 5.
Services offered by RCCs and their perceived importance rated by RCC staff
| % offered (30 centers)a |
perceived importanceb (55 staff) |
|||
|---|---|---|---|---|
| Service | % | (n) | mean | (SD) |
| Support Group Meetings | ||||
| “All Recovery” meetings | 60.0 | (18) | 6.3 | (1.3) |
| Mutual-help groups by known organizations (e.g., Alcoholics Anonymous) | 96.7 | (29) | 6.6 | (0.7) |
| Other peer-facilitated recovery support groups (e.g., relapse prevention groups) | 76.7 | (23) | 6.6 | (0.7) |
| Mental health support (e.g., dual diagnosis support groups) | 36.7 | (11) | 6.1 | (1.0) |
| Recovery coaching (and/or case management) | 76.7 | (23) | 6.2 | (1.4) |
| Opioid and/or Harm Reduction Services | ||||
| Medication-assisted treatment (MAT) support (e.g., Pathway Guide, MARS group) | 43.3 | (13) | 5.9 | (1.6) |
| NARCAN training and/or distribution | 56.7 | (17) | 6.3 | (1.2) |
| Provision of Access to Technology/Internet (e.g., use of center computers, printers, fax) | 46.7 | (14) | 5.6 | (1.4) |
| Assistance with Basic Needs and Social Services | ||||
| Basic needs assistance (e.g., access to food, clothing, transportation) | 43.3 | (13) | 5.8 | (1.2) |
| Childcare services | 10.0 | (3) | 4.8 | (1.6) |
| Education assistance | 63.3 | (19) | 5.6 | (1.3) |
| Employment assistance (e.g., job or computer skills, resume writing, CORI support) | 83.3 | (25) | 5.9 | (1.2) |
| Family support services (e.g., family/parent education or support groups) | 86.7 | (26) | 6.1 | (1.1) |
| Financial services | 23.3 | (7) | 5.1 | (1.6) |
| Health insurance education | 36.7 | (11) | 5.2 | (1.4) |
| Housing assistance | 70.0 | (21) | 5.9 | (1.3) |
| Legal assistance | 16.7 | (5) | 5.0 | (1.8) |
| Assistance with Health Behaviors | ||||
| Health, exercise, and nutrition programs (e.g., yoga, meditation, fitness classes) | 83.3 | (25) | 5.7 | (1.3) |
| Smoking cessation support | 53.3 | (16) | 5.0 | (1.7) |
| Facilitation of Substance-free Recreational Activities | ||||
| Recreational/social activities (e.g., substance free social events) | 100.0 | (30) | 6.3 | (1.0) |
| Expressive arts (e.g., arts/craft groups, music, poetry) | 53.3 | (16) | 5.4 | (1.3) |
Note.
as reported by directors, where 2 directors managed 2 centers each
importance was rated on a 1 (not important at all) to 7 (extremely important) scale, where staff from 21 centers provided ratings, with 1 to 9 staff members completing surveys per RCC; n=4 staff members did not complete this part of the survey, others indicated “not applicable” instead of rating the importance of a particular service, resulting in importance ratings from n=38 staff members for “child care services” to n=55 staff members for “mutual-help groups” and “recreational activities”, respectively.
1.9. Correlational associations among Center Characteristics and Usage of Centers
Spearman correlations among indices capturing RCC attractiveness, fiscal appropriation, and member utilization indices indicated that higher total budgets were positively related to accessibility of centers in terms of higher walk scores (r=.54), and the amount of time RCC members spend at the center (r=.47). Of note, the attractiveness of the site location where the RCC was situated was related to the attractiveness of the program itself (r=.41), but negatively associated with new service users per month (Table 6).
Table 6.
Spearman correlations between center characteristics and use of center (K=32)
| Variables | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | |
|---|---|---|---|---|---|---|---|---|---|---|
| Center Characteristic | ||||||||||
| 1. | Site Location Attractiveness | 1.00 | ||||||||
| 2. | Quality of the RCC interior space | 0.51 | * 1.00 | |||||||
| 3. | Walk Score | −0.16 | 0.03 | 1.00 | ||||||
| 4. | Total budget | −0.08 | 0.15 | 0.54 | * 1.00 | |||||
| 5. | Hours of Operation Per Week | −0.28 | −0.18 | 0.04 | 0.13 | 1.00 | ||||
| 6. | Recommendability / Referability | 0.10 | 0.15 | 0.34 | 0.24 | 0.33 | 1.00 | |||
| 7. | Attractiveness of the Program | 0.41 | * 0.61 | * 0.24 | 0.27 | 0.21 | 0.60 | * 1.00 | ||
| Use of center | ||||||||||
| 8. | Monthly Visits from Unique Service Users | −0.21 | −0.20 | −0.05 | 0.03 | 0.29 | 0.30 | 0.21 | 1.00 | |
| 9. | Hours a Service User Spends at Center Per Visit | −0.15 | −0.27 | 0.37 | * 0.47 | * 0.30 | 0.09 | −0.13 | −0.20 | 1.00 |
| 10. | New Service Users Per Month | −0.41 | * −0.21 | −0.09 | 0.20 | 0.20 | 0.06 | −0.07 | 0.30 | −0.30 |
Note: To account for center dyads that shared budget and/or staff, we excluded satellite centers from analysis;
p < 0.05
Discussion
Findings represent the first systematic aggregated summary of the broad characteristics of U.S. recovery community centers. RCCs across the northeastern region of the U.S. were found to vary somewhat in physicality and urbanicity, but more so in terms of allocated budgets, staffing composition, number and characteristics of RCC service users, and the number and types of services provided. RCCs were found to be, in general, moderately physically attractive, mostly easily accessible and located close to population centers, operated mostly by paid staff but with some relying heavily on volunteer staff, and with most (but not all) staff in recovery themselves. Centers on average served several hundred individual service users per month, who visited approximately 1400 times per month. In keeping with their overall mission, centers were found to be centrally located in dense population areas, and provided a broad range of socially-based recovery support infrastructure and technical assistance to visitors who were typically White, unemployed men, with a history of a primary opioid or alcohol problem, in the early stages of recovery stabilization, and largely involved in the criminal justice system. Importantly, however, a large proportion of RCC participants were in stable long-term recovery of several years or more, indicating RCCs’ potential to provide services that may be of continued value long-after initial sustained remission. The longevity and continuing growth of RCCs, and the fact they appear to offer a variety of services deemed important to sustaining recovery to high numbers of individuals across a broad range of recovery stages, suggest RCCs play a valued community role that may facilitate the accrual of social, employment, housing, and other recovery capital.
Centers were mostly located according to population density with most situated in highly populated urban areas within walkable distances from parts of the city. This central location appears to fit well with the RCC mission, which is to be located in the “hearts of communities”. This visible central positioning is intended to provide accessibility to large numbers of affected individuals but also as a way to serve as a visible beacon of hope and help destigmatize addiction and recovery from it by serving as a safe and helpful community resource (Valentine, 2011). There was widespread variability among RCCs in the physical size, staffing, budgets, technological sophistication, service capacity and scope of provided services. The degree of emphasis on the RCC model also appeared to vary by state with MA and CT appropriating much higher annual fiscal budgets than smaller population states such as VT and ME. There appeared to be philosophical differences too that may well be associated with the degree of rigorous record keeping and documentation and the desire to keep the same, as well as the degree of technological adoption. Some RCC Directors, for instance, lamented the fact that they were often asked by state agencies and bodies to provide numerous details and numbers of RCC clientele, which seemed to go against their more grass-roots volunteer orientation and the overarching philosophy that had initially driven the formation of RCCs and the broader recovery movement (e.g., informal peer-to-peer volunteer helping). Many of these centers tended to oppose keeping membership records or even asking people to sign in to the facility at all. Other RCCs appeared to embrace and rely more heavily on sophisticated technology requiring membership registration, and even issuing scannable membership cards with computerized tracking and monitoring. The ultimate question of course, is the degree to which such tracking and technological variation may be associated with derived recovery benefits for those seeking help at RCCs. This will be a focus of future research.
Somewhat surprising was the finding that the majority of centers functioned with only minimal use of volunteer staff. The centers that did use more volunteers tended to rely much more heavily on volunteers with almost 10 volunteer staff in each of those centers. Again, this tended to be in those RCCs with the lowest budgets. Staff turnover was relatively high but similar to that of addiction treatment settings. One treatment center study, for example, that examined turnover among addiction treatment counselors and clinical supervisors at 27 geographically dispersed public and private addiction treatment organizations over a 2-year period (2008–2009), found an annual turnover rate of 33% for counselors and 23% for supervisors (Eby, Burk, & Maher, 2010). Also, in a national study of 175 addiction treatment programs, McLellan and colleagues (2003) found past-year turnover rates among staff and directors was 53% (McLellan et al., 2003). The failure to keep paid staff long-term in RCCs and addiction treatment settings may be indicative of lower pay rates, and limited opportunity for promotion to higher levels within such organizations.
Utilization of RCCs by those in or seeking recovery varied considerably from a handful to more than two thousand per month and an average center visit lasted about two and a half hours. Centers varied too in the degree of services provided with RCCs which had larger censuses tending to offer more recovery support services. It is currently unclear whether a certain census or capacity threshold (quorum) may be needed, or specific types or a certain number of specific services provided, for positive therapeutic benefits to be realized. Future research should examine this.
In terms of leadership and staffing, a slightly higher proportion of RCC Directors were women whereas almost 70% of staff were women; most were of White race. Somewhat surprisingly, about one in ten directors were not in recovery, as were approximately one in seven staff. This is noteworthy given that the “wounded healer” model (Jackson, 2001) is deemed to be a cornerstone of the recovery movement and considered to convey at least some unique therapeutic value to the recipient (as well as to the helper; (Zemore, 2007). Understanding how such individuals are perceived and welcomed by the majority recovering staff community and how the inclusion of non-recovering Directors and/or staff may affect the social climate and therapeutic gains should be a focus of future investigation.
In terms of who is using RCCs, findings here suggest that the largest proportion are unemployed men with primary opioid or alcohol histories, involved in the criminal justice system, and in their first year of recovery. For such individuals, RCCs may play a particularly valuable role in finding social support, increasing a sense of belonging and instilling hope for a better future, as well as providing help in dealing with legal issues in early recovery and finding a job, stable housing, and educational access. The fact that all of these elements may be attainable within a single RCC suggests RCCs represent a kind of “recovery department store” that facilitates one stop shopping in the accrual of recovery capital.
As expected, a large proportion of RCC users (about 50%) were in their first year of recovery, but it is noteworthy that just over one in five RCC users had between one and five years in recovery and an additional, roughly 20%, had five or more years in recovery. The fact that, in total, almost half of RCC participants are individuals with more stable remission and long-term recovery suggests potential value far beyond initial stabilization and even the early phases of recovery. Understanding more about this specific group of individuals and what value they appear to obtain from RCC involvement at these longer recovery milestones could inform the broader field about the perceived needs of those in longer-term recovery.
The types and number of services provided varied across RCCs and centered on expected broad dimensions of recovery peer support (e.g., mutual-help meetings/recovery coaching), technical assistance (e.g., employment, housing, education assistance), and recreational and self-care activities (e.g., substance-free social events, meditation/yoga, physical fitness). Centers with greater funding and serving higher numbers of individuals tended to offer more services whereas smaller, lower budget, centers tended to offer fewer services, with a few being mostly a venue for mutual-help organization meetings and peer support. Of note, the only thing offered universally by every RCC was substance-free social and recreational activities. Researchers have noted the need to make recovery more attractive and rewarding (McKay, 2017) and RCCs may serve as a valuable hub in this regard facilitating and providing such substance-free activities. Peer-led mutual-help meetings were another, almost universally provided and highly rated, recovery support service and were rated the highest by staff in terms of their importance to recovery. This central valued role of groups like AA for recovery is supported also by strong empirical evidence (Kelly, Humphreys, & Ferri, In press).
Whereas, in general, there was a high correlation between services provided and their perceived importance to recovery, there were some notable exceptions particularly relating to opioid use disorders. Specifically, NARCAN overdose reversal training was rated as very important by staff, but less frequently offered by RCCs (57% of centers). The same pattern was evident for medication-assisted treatment (MAT) support, which was again less frequently provided (43.3% of centers) but rated as very important to recovery. This indicates an important discrepancy may be occurring with many RCCs failing to offer support for MAT and overdose reversal despite it being rated as highly important. In light of the current opioid crisis, and the noteworthy fact that one of the main constituencies of RCC participants are those with a primary opioid problem who could stand to benefit from greater support for MAT and overdose reversal training, there is potential for expanded provision of such services within RCCs.
Additionally, mental health support was rated as important, but offered only by about one-third of centers, again indicating a discrepancy between the perceived importance of a service to recovery and its availability. Finally, some of the lowest importance ratings (though still above 4 (moderately important)), were ascribed to smoking cessation support, which was offered by only about half of centers. Although it appears that more people in recovery that smoke cigarettes are quitting and quitting sooner in more recent times (Kelly et al, 2019), there remains an important need to address smoking cessation given its deleterious impact on health and longevity. Given the fact that many smokers with SUD prefer to stop smoking sequentially after stabilizing in SUD recovery, rather than at the same time (Kodl, Fu, & Joseph, 2006), RCCs could be an ideal venue to offer smoking cessation services.
Exploratory inter-relationships among center characteristics and use of RCCs suggest that centers that have attractive locations also tend to have better interior space and overall are more attractive programs, but this did not relate to greater recommendability/referability to centers. Recommendability/referability (the likelihood that you would refer a family member to the program) appeared to be more related to the warmth of the social climate than on physicality and locality per se. This observation suggests that while RCC’s physical appearance may be important, the degree to which raters would recommend a family member to attend a center was largely independent of this, and more about the social climate (i.e., was perceived as emotionally warm and had a good “vibe”) and the number and types of services provided within a center. The amount of time a service user spent at a center was associated positively with greater ease of accessibility (Walk Score) and a higher budget. It may be that centers with higher budgets have more offerings that keep people at the center longer. Somewhat unexpected was the negative relationship between RCC site location attractiveness and fewer new service users per month. This may be explained by the observation that the more attractively located centers were relatively new and were yet to become known, established, entities in the community.
1.10. Limitations
Conclusions and generalizations from the current study should be made cautiously in light of several limitations. The study findings reported herein relied largely on self-reported estimations by directors and only rarely through objective and systematically kept records. Also, the accuracy and allocation of budgets varied greatly, with some being objectively verifiable and others estimated by directors. Given this study’s regional sampling of RCCs from the northeastern U.S., generalizability of findings to other U.S. regions is unknown. Also, a goal of the current exploratory/developmental investigation was to help uncover and characterize the nature of these novel recovery support services; thus, several measures were constructed in the process of conducting the study, with obtained RCC elements subsequently recorded and categorized into broad domains. These measures may well hold value for future work, but their reliability needs confirmation in the process of further investigation.
Conclusions
It has long been recognized that for at least some individuals suffering from alcohol or other drug use disorders, there is a need for ongoing support to address clinical relapse vulnerability as well psychosocial deficits not addressed by more acute formal treatment services. Recovery community centers have emerged across the U.S. during the past 15 years in order to provide different elements of social recovery support as well as to facilitate the accrual of recovery capital (e.g., in areas of employment, housing, and education) that can provide income, safety, enhanced self-esteem and quality of life, and instill hope for a better future that are locally available in the communities in which people live. This study suggests that RCCs vary greatly in their financial resources, degree of professional vs volunteer staff, size, number and scope of services, degree of technological adoption and sophistication, and systematic record-keeping. Although utilized to a large degree by individuals both seeking and in their first year of recovery, their perceived value extends to those in the early years of recovery and even to those who have achieved longer-term stable recovery of five or more years. The use of such services among individuals that have achieved longer-term recovery suggests valuable offerings at such facilities about which much is to be learned.
Table 4.
Service User Characteristics of Recovery Community Centers: Demographics, Substance Use History, and Referral Source as Reported by Directors
| Characteristic of RCC Service User | Reported by RCC Directors n=30 |
||
|---|---|---|---|
| M % (SD) | range of % | ||
| Demographics | |||
| Age | |||
| Under 18 | 2.3 (4.5) | 0–20 | |
| 18–24 | 20.3 (13.4) | 0–50 | |
| 25–59 | 65.0 (16.3) | 40–99 | |
| 60+ | 12.3 (11.3) | 0–50 | |
| Not reported | 0.2 (0.9) | 0–5 | |
| Female a | 39.3 (13.4) | 3–70 | |
| Race | |||
| White | 72.0 (30.7) | 10–100 | |
| Black or African American | 15.8 (22.9) | 0–80 | |
| More than one race | 7.2 (10.7) | 0–41 | |
| Other | 2.0 (2.6) | 0–10 | |
| Not reported | 3.0 (11.2) | 0–58 | |
| Hispanic or Latino | 8.4 (11.5) | 0–58 | |
| Education b | |||
| High school diploma/GED or less | 75.8 (16.5) | 1–95 | |
| Bachelor’s | 9.8 (10.7) | 0–50 | |
| Graduate degree | 3.1 (5.3) | 0–18 | |
| Other professional degree (e.g., technical, associates) | 10.7 (11.7) | 0–56 | |
| no reported | 0.6 (2.1) | ||
| Employment | |||
| Employed or student, full time | 29.5 (21.9) | 0–75 | |
| Employed, part time | 20.5 (15.2) | 0–80 | |
| Unemployed | 50.0 (26.2) | 10–100 | |
| Current Legal Involvement | |||
| Not currently involved | 56.6 (24.1) | 15–96 | |
| Currently involved | 42.7 (24.1) | 4–85 | |
| Substance Use History c | |||
| Years in Recovery | |||
| 0–6 months | 31.4 (21.5) | 4–99 | |
| 6 months - 1 year | 17.5 (9.3) | 1–40 | |
| 1–5 years | 27.1 (15.2) | 0–50 | |
| 5+ years | 19.8 (18.9) | 0–61 | |
| Actively using | 4.5 (7.9) | 0–27 | |
| Primary Substance | |||
| Alcohol | 32.9 (20.3) | 2–80 | |
| Opioids | 35.4 (30.8) | 0–92 | |
| Cocaine/crack | 7.9 (12.2) | 0–60 | |
| Amphetamines & Methamphetamines | 0.6 (1.7) | 0–8 | |
| Cannabis | 4.8 (7.9) | 0–30 | |
| Other | 3.1 (4.7) | 0–17 | |
| No drug problem | 2.0 (3.0) | 0–10 | |
| Referral Source | |||
| Treatment | 24.3 (17.6) | 0–75 | |
| Criminal Justice | 15.9 (14.2) | 0–60 | |
| Shelters | 6.4 (8.5) | 0–36 | |
| Self-Referred (e.g., word of mouth, walk-in) | 44.5 (26.1) | 0–100 | |
| Recovery Residences | 3.7 (11.1) | 0–50 | |
| Other (e.g., mutual help organization, family, college) | 5.1 (7.7) | 0–28 | |
| Not reported | 0.1 (0.8) | 0–4 | |
Note. M% = mean percent. SD = standard deviation of the mean percent.
60.5% male, 0.2% other gender.
reported by directors for 31 centers;
= reported by directors for 30 centers.
JSAT Highlights.
RCCs were mostly state-funded with budgets ranging from $17,000-$760,000/year
RCCs served anywhere from a dozen to more than two thousand clients/month.
Clients were mostly unemployed, justice-system involved; opioid/alcohol histories.
Services included recreational, mutual-help/recovery coaching, employment, education.
Medication treatment (MAT) support, OD-reversal training, was offered less often.
Acknowledgments
Funding: The study was supported by the National Institute of Alcohol Abuse and Alcoholism (NIAAA) under grant R21AA022693 to the Massachusetts General Hospital (PI: John F. Kelly). Authors are also supported by K24AA022136 (JFK), F32AA025823 (CLV).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Carr LJ, Dunsiger SI, & Marcus BH. (2011). Validation of Walk Score for estimating access to walkable amenities. British Journal of Sports Medicine, 45(14), 1144–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloud W, & Granfield R. (2008). Conceptualizing recovery capital: expansion of a theoretical construct. Substance Use and Misuse, 43(12–13), 1971–1986. [DOI] [PubMed] [Google Scholar]
- Cousins SJ, Antonini VP, & Rawson RA. (2012). Utilization, measurement, and funding of recovery supports and services. Journal of Psychoactive Drugs, 44(4), 325–333. [DOI] [PubMed] [Google Scholar]
- Cunningham JA. (1999). Untreated remissions from drug use: the predominant pathway. Addictive Behaviors, 24(2), 267–270. [DOI] [PubMed] [Google Scholar]
- Eby LT, Burk H, & Maher CP. (2010). How serious of a problem is staff turnover in substance abuse treatment? A longitudinal study of actual turnover. Journal of Subs Abuse Treatment, 39(3), 264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, … Consortium, R. E. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG. (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K, & Moos R. (2001). Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study. Alcoholism: Clinical and Experimental Research, 25(5), 711–716. [PubMed] [Google Scholar]
- Humphreys K, & Moos RH. (2007). Encouraging posttreatment self-help group involvement to reduce demand for continuing care services: two-year clinical and utilization outcomes. Alcoholism: Clinical and Experimental Research, 31(1), 64–68. [DOI] [PubMed] [Google Scholar]
- Institute of Behavioral Research. (2006). TCU Survey of Structure and Operations (TCU SSO). Fort Worth: Texas Christian University, Institute of Behavioral Research. [Google Scholar]
- Jackson SW. (2001). The wounded healer. Bulletin of the History of Medicine, 75(1), 1–36. [DOI] [PubMed] [Google Scholar]
- Jason LA, & Ferrari JR. (2010). Oxford House Recovery Homes: Characteristics and Effectiveness. Psychological Services, 7(2), 92–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF. (2017). Are societies paying unnecessarily for an otherwise free lunch? Final musings on the research on Alcoholics Anonymous and its mechanisms of behavior change. Addiction, 112(6), 943–945. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Hoeppner B. A biaxial formulation of the recovery construct. Addict Res Theory 2015; 23(1):5–9. [Google Scholar]
- Kelly JF, Humphreys KN, & Ferri M. (In press). Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database of Systematic Reviews. [DOI] [PMC free article] [PubMed]
- Kelly JF, & White WL. (2012). Broadening the Base of Addiction Mutual-Help Organizations. Journal of Groups in Addiction & Recovery, 7(2–4), 82–101. [Google Scholar]
- Kelly JF, & White WL. (2011). Addiction Recovery Management: Theory, Research and Practice In Rosenbaum JF. (Ed.), Current Clinical Psychiatry (p. 326). New York: Humana Press. [Google Scholar]
- Kelly JF, Greene MC, Bergman BG, Hoeppner BB. Smoking cessation in the context of recovery from drug and alcohol problems: Prevalence, predictors, and cohort effects in a national US sample. Drug and Alc Dep. 2018; 195:6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodl M, Fu SS, & Joseph AM. (2006). Tobacco cessation treatment for alcohol-dependent smokers: when is the best time? Alcohol Research and Health, 29(3), 203–207. [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S. (1984). Stress, Appraisal, and Coping. New York: Springer Publishing Company. [Google Scholar]
- McKay JR. (2017). Making recovery more rewarding: difficult with possible unintended consequences, but successful examples are out there. Addiction, 112(5), 763–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Carise D, & Kleber HD. (2003). Can the national addiction treatment infrastructure support the public’s demand for quality care? Journal of Substance Abuse Treatment, 25(2), 117–121. [PubMed] [Google Scholar]
- National Drug Intelligence Center. (2011). The Economic Impact of Illicit Drug Use on American Society. Washington, D.C.: United States Department of Justice. [Google Scholar]
- Savidge TO, & Stein F. (2012). Prevention, treatment, and recovery supports for those with substance use problems: opportunities for enhanced access quality of care. North Carolina Med Jnl, 73(3), 209–211. [PubMed] [Google Scholar]
- Scott CK, & Dennis ML. (2009). Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction, 104(6), 959–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheedy CK, & Whitter M. (2009). Guiding principles and elements of recovery-oriented systems of care: What do we know from the research? (Vol. HHS Publication No. (SMA) 09–4439). Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Timko C. (1996). Physical characteristics of residential psychiatric and substance abuse programs: organizational determinants and patients outcomes. American Journal of Community Psychology, 24(1), 173–192. [DOI] [PubMed] [Google Scholar]
- Valentine P. (2011). Peer-based recovery support services within a recovery community organization: The CCAR experience In Kelly JF & White WL. (Eds.), Addiction Recovery Management: Theory, research and practice (pp. 259–279). New York, NY: Springer [Google Scholar]
- Walk Score Inc. Walk Score Methodology. Retrieved from: www.walkscore.com (Accessed August 3 2019).
- White WL. (2009). The mobilization of community resources to support long-term addiction recovery. Journal of Substance Abuse Treatment, 36(2), 146–158. [DOI] [PubMed] [Google Scholar]
- White WL. (2012). Recovery/remission from substance use disorders: An analysis of reported outcomes in 415 scientific reports, 1868–2011. Philadelphia Department of Behavioral Health and Intellectual Disability Services.
- World Health Organization. Management of Substance Abuse Team. (2011). Global status report on alcohol and health. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Zemore SE. (2007). A role for spiritual change in the benefits of 12-step involvement. Alcoholism: Clinical and Experimental Research, 31(10 Suppl), 76s–79s. [DOI] [PubMed] [Google Scholar]