Abstract
Purpose
Hip dislocation and scoliosis are common in children with cerebral palsy (CP). Hip dislocation develops in 15% and 20% of children with CP, mainly between three and six years of age and especially in the spastic and dyskinetic subtypes. The risk of scoliosis increases with age and increasing disability as expressed by the Gross Motor Function Score.
Methods
A hip surveillance programme and early surgical treatment have been shown to reduce the hip dislocation, but it remains unclear if a similar programme could reduce the need for neuromuscular scoliosis. When hip dislocation and neuromuscular scoliosis are co-existent, there appears to be no clear guidelines as to which of these deformities should be addressed first: hip or spine.
Results
Hip dislocation or windswept deformity may cause pelvic obliquity and initiate scoliosis, while neuromuscular scoliosis itself leads to pelvic obliquity and may increase the risk of hip dislocation especially on the high side. It remains unclear if treating imminent hip dislocation can prevent development of scoliosis and vice versa, but they may present at the same time for surgery. Current expert opinion suggests that when hip dislocation and scoliosis present at the same time, scoliosis associated pelvic obliquity should be corrected before hip reconstruction. If the patient is not presenting with pelvic obliquity the more symptomatic condition should be addressed first.
Conclusion
Early identification of hip displacement and neuromuscular scoliosis appears to be important for better surgical outcomes.
Keywords: cerebral palsy, hip dislocation, neuromuscular scoliosis, CP surveillance, hip reconstruction, spinal fusion surgery
Introduction
Hip dislocation develops in 15% and 20% of children with cerebral palsy (CP), mainly between three and six years of age, and especially in the spastic dyskinetic subtypes.1 Children with Gross Motor Function Classification System (GMFCS) level V demonstrate an incidence of hip displacement up to 90%.2 The risk of scoliosis increases with age and increasing disability (increasing GMFCS level).3 The risk of scoliosis is 1% for GMFCS level I at ten years of age and 5% at 20 years, but 30% for GMFCS V at ten years and 80% at 20 years. Hip dislocation may cause pelvic obliquity and initiate scoliosis, usually with the side of the adducted dislocated hip corresponding to the high hemi-pelvis (windswept deformity), while neuromuscular scoliosis itself can lead to pelvic obliquity and may increase the risk of hip dislocation especially on the high side4,5 (Fig. 1a). It remains unclear if treating imminent hip dislocation can prevent development of scoliosis and vice versa, but they may present at the same time for surgery. There appears to be no clear guidelines as to which of these deformities should be addressed first: hip or spine.
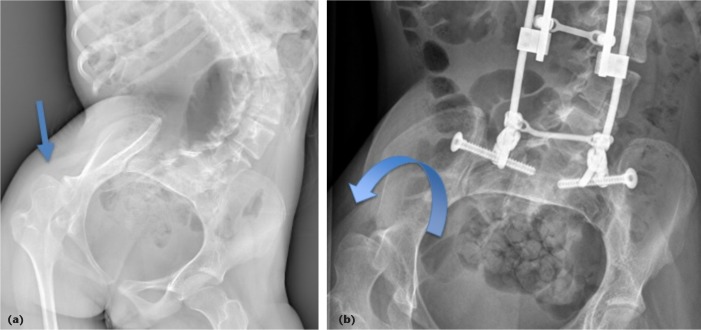
Fig. 1.
a) Hip subluxation before spine surgery on the high side; b) improvement of hip subluxation after spine surgery.
This article was conceived by the neuromuscular and spine study groups of the European Paediatric Orthopaedic Society based on the presentations of the authors given at the society’s 37th annual meeting in Tel Aviv, Israel (05 April 2019) in a two-hour focus session on CP and associated spine deformities.
Hip dislocation
A hip surveillance programme and early surgical treatment have been shown to reduce the risk of hip dislocation.6 In a Swedish hip surveillance programme,6 every child with suspected CP is evaluated by a neuropaediatrician at the age of four years and receives a pelvic radiograph. Thereafter, the child is followed up twice annually by a physiotherapist and receives pelvic radiographs annually until the age of eight years. Hips demonstrating a migration percentage of 33% (the percentage of the ossified femoral head outside of the lateral margin of the ossified acetabum7) are referred to an orthopaedic surgeon.
Conservative treatment methods include better position of the hips into abduction and external rotation as well as regular physiotherapy. Better position of the hips can be promoted by using a wedge between the legs or intermittent serial plaster. Hips presenting with a migration percentage of 40% or more receive early surgery including adductor and ileopsoas tenotomies or proximal femoral and pelvic osteotomies.6 Using early surgery, the risk of hip dislocation (defined as migration percentage of 100% or more) has decreased from 9.2% to 0.6% in Southern Sweden during the last two decades, while the percentage of children undergoing hip surgery has remained at 13%. Similar findings have been obtained in Australia as well.8
Hip reconstruction surgery using femoral and/or pelvic osteotomies has improved the health-related quality of life even in non-ambulatory children with CP.9 Children with a lower migration precentage (< 50%) had a higher preoperative Caregiver Priorities and Child Health Index of Life with Disabilities (CPCHILD) total score than those with a larger migration percentage (> 50%), but improvements in the CPCHILD were similar in both groups resulting in higher health-related quality of life in children with < 50% migration percentage preoperatively.
Based on a daily living point of view it is most important to keep the hips well centred with a level pelvis in order to achieve good sitting comfort, prevent pain and avoid biomechanical conditions that can allow scoliosis to evolve.10 Surgery of a dislocated hip may not cure sitting and positioning asymmetry, and may even worsen it when performed unilaterally. Bilateral surgery may, therefore, be needed to correct a pelvic imbalance that would hinder activities of daily living.11
Reconstructive hip surgery in severely dysplastic hips or in the presence of osteoarthritis should be first weighed against its potential complications and the need for a complete preoperative work-up in the severely involved CP patient to decrease complications. Considering daily life activities, reducing spasticity using focal hip objective-based toxin injections to improve comfort and maintain symmetric movement for daily care may be more useful than having a located hip as documented on a radiograph.12 For reliable orthopaedic management of hip problems in CP patients, it is most important to be aware of long-term issues of daily living. It’s essential to ask ‘good’ questions to be able to propose a daily living objective-based therapy programme. Good questions can be for example: is the hip deformity or asymmetry annoying more the child, the parents, or the physiotherapist? Are there any objective findings to support more active conservative or surgical management for the hip dislocation?
Scoliosis
In a population based study on 962 children with CP, the risk of scoliosis was closely associated with disability i.e. increasing GMFCS score and age.3 Of these children with GMFCS I, 1% presented with scoliosis at ten years of age and 5% at 20 years, but 30% had scoliosis with GMFCS V at ten years and 80% at 20 years. The risk of scoliosis > 40° was 0% in the GMFCS 1, but 75% in GMFCS V at the age of 20 years. The risk factors for progressive neuromuscular scoliosis include scoliosis of 40° or more, thoracolumbar curves and total body involvement.13 The progression of scoliosis does not stop at skeletal maturity in curves 40° or more. In children with CP associated scoliosis the internal rotation and reduced range of flexion on the high side hip may result into sitting problems.14
Senaran et al5 evaluated the effect of unilateral hip dislocation on the CP scoliosis. They followed up 23 spastic tetraplegic CP children with untreated unilateral hip dislocation and scoliosis and compared their outcomes with 83 spastic tetraplegic CP with well-located hips and scoliosis. The progression of scoliosis was similar in both groups (12.9°versus 12.2°per year), while the incidence of pelvic obliquity was higher in the group with hip dislocation (74% versus 63%). Pelvic obliquity was corrected after posterior spinal fusion to the pelvis without reducing the hip at the same surgery.
The issues associated with CP scoliosis include poor sitting balance, abdominal and thoracic crowding leading to smaller lung volumes and increased risk of pneumonia when curves exceed 70°,15 impingement between thoracic cage and pelvis. The conservative treatment methods of CP scoliosis include annual observation, bracing, but also seating modification and medical management (bisphosphonates).16 There is limited evidence that bracing can reduce the risk of progression of CP scoliosis, but it remains unclear if bracing can reduce the risk of spinal fusion.16,17
Instrumented spinal fusion for neuromuscular scoliosis has been recommended when curves exceed 40° as these are regarded as highly progressive.18,19 Spinal fusion has improved health-related quality of life even in the non-ambulatory CP children.18,19 It remains unclear if juvenile children with CP scoliosis benefit from growing rod surgery, as it is associated with high risk of complications, especially deep surgical site infection.20 Yaszay et al21 reported stable outcomes in this age group using a definitive spinal fusion. They also postulated that the pulmonary function requirements of non-ambulatory CP children may not be equal to idiopathic or congenital scoliosis children in whom the T1-T12 length of 22 cm or more has been recommended to achieve normal lung function.22
Coexistent hip dislocation and scoliosis
When hip surveillance methods fail, hip displacement and scoliosis may present at the same age (typically after eight years of age). There are no widely accepted clinical guidelines as to which of the conditions should be addressed first. Daily living has to be the basis for long-term decision-making regarding the concommitent orthopaedic problems and good and painless sitting posture and daily care are the principal objectives to obtain.23Table 1 gives a summary of how the authors decide which of the condition should be treated first.
Table 1.
Factors affecting decision making as to whether to perform spine or hip reconstruction first on a cerebral palsy child with both scoliosis and hip dislocation
| Factors |
|---|
| Symptoms |
| The more symptomatic (hip or spine) should be addressed first |
| Mobile and pain-free dislocated hip => Scoliosis surgery first |
| Fixed, non-mobile, painful hip => Consider hip salvage or reconstruction first |
| Type of scoliosis |
| Early-onset scoliosis ≥ 60° => Growing rods (age < 8 yrs) or spinal fusion (age > 8 yrs) |
| Flexible adolescent neuromuscular scoliosis < 60° => Hip surgery can be performed first |
| Rigid or more severe neuromuscular scoliosis ≥ 60° => Spinal fusion (age > 8 yrs) |
| Pelvic obliquity |
| < 10° and flexible scoliosis < 60° => Hip reconstruction can be performed first |
| ≥ 10° => Spinal fusion first to level the pelvis |
In general, the presence of symptoms will help dictate the order in which procedures are performed. Furthermore, more aggressive surveillance of ‘hips at risk’ has led to a dramatic reduction in dislocated hips. If the dislocated hip is relatively mobile and pain free, spine surgery should be performed before the hip is treated. In these cases, unilateral subluxation of the hip may improve after spine surgery and secondary hip surgery may not be necessary (Fig. 1).
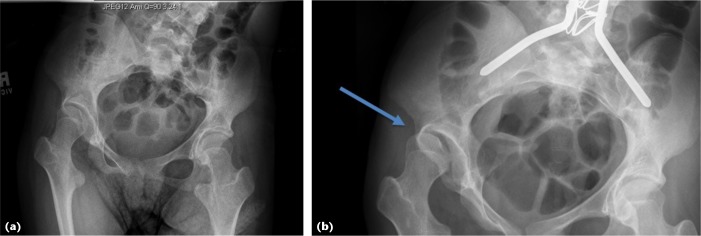
In mobile but unilateral high dislocated hips levelling the pelvis by spine surgery may increase the constraint on the hip. Especially following correction of severe pelvic obliquity associated with lumbar spine rotation, muscular tone in the ipsilateral lower limb may increase with decrease of hip mobility and increase hip pain and daily care difficulties (Fig. 2). In these cases, families and peers should be aware of the need for close hip surveillance after spine surgery and the possible need for combined tone treatment, soft-tissue loosening around the hip or conservative or hip reconstruction.
Fig. 2.
An 11-year-old cerebral palsy patient: a) before spine surgery no hip related pain, but hip migration; b) two years after spine surgery developed painful hip subluxation.
In the adolescent or adult patient with a symptomatic dislocated hip in combination with pelvic obliquity and a scoliosis, scoliosis surgery is usually performed first, to horizontalize the pelvis. Care should be taken to leave iliac screws rather short on the side of the dislocated hip to allow for later pelvic osteotomy.
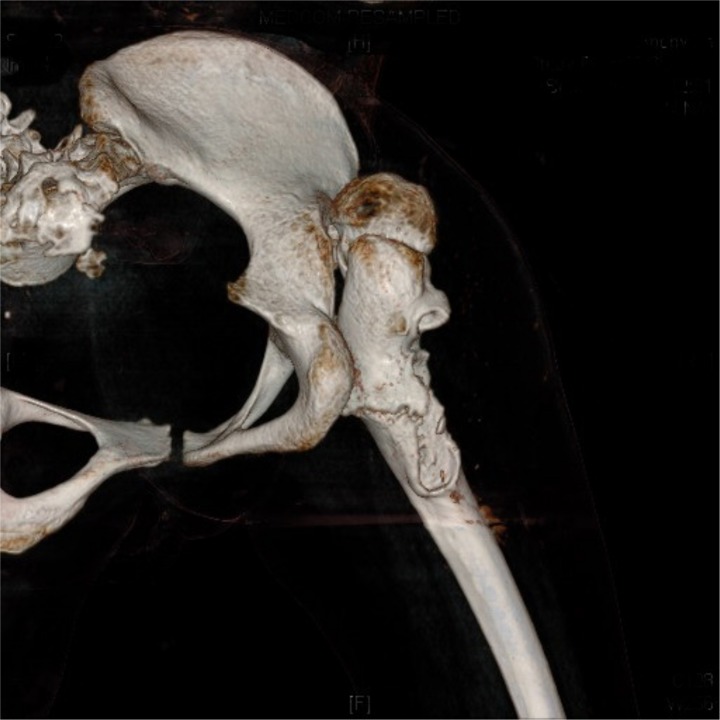
Careful preoperative testing and simulation of the postoperative sitting possibilities are essential. In the case of a fixed, non-mobile hip dislocation (Fig. 3), scoliosis surgery levelling the pelvis may prevent sitting. Therefore, a reconstruction or hip salvage procedure should be considered first, before scoliosis surgery.
Fig. 3.
Fixed dislocated hip.
Since hip problems often arise before the onset or rapid progression of the scoliosis, in the younger child treating the hip first and trying to control the spine by bracing, seating orthoses or growing implants may be indicated. In any case, hip and spine surgery should not be undertaken at the same time. This would result in long anaesthesia, risk of major blood loss, increased risk of deep wound infection, pressure sores, increased postoperative pain and risk of prolonged intensive care management. This may also lead to a severely disbalanced situation whereas staged procedures allow for intermittent evaluation of hip function and requirements for comfortable seating. Furthermore, some children require a relative or absolute lumbar kyphosis for adequate and comfortable seating; drastic restoration of lumbar lordosis may seriously disturb their sitting balance. Painful hips tend to become more painful once the spine is fixed.
In children with neuromuscular type of early onset scoliosis, delaying surgery with bracing or other conservative methods can be applied if the curves are < 60° and the dislocated hip can be addressed first. General health of the patient has to be taken into consideration and application of conservative methods should not delay surgery until severe curvatures with increase of pulmonary and gastrointestinal problems which will increase the risk of scoliosis surgery and the postoperative complications. In larger curves (major curve 60° or more), scoliosis surgery either with growing rods (before eight years of age) or definitive spinal fusion (after the age of eight years) should be carried out first. If the pelvic instrumentation (iliac or S2 alar iliac (S2AI) screws) is needed, it is worth considering if the screw on the high side (displaced hip side) should be left short to facilitate later pelvic osteotomy.
On an adolescent patient with horizontal pelvis, the more clinically relevant issue (spine or hip) should be addressed first, unless the patient is presenting with a larger curve (major curve > 60°), which has been identified as an independent risk factor for pneumonia.15 When the patient is presenting with pelvic obliquity, it is difficult to reconstruct the pelvis without first correcting the pelvic obliquity using spinal fusion. In a flexible scoliosis, presumably more pelvic obliquity may be acceptable, when addressing the hip first. It is also important to bear in mind that CP children may have stiff hips, and part of the ‘hip flexion’ may actually result from kyphosing of the lumbar spine. Careful clinical evaluation is mandatory to assess the hips as spinal fusion to the pelvis with full restoration of lumbar lordosis may result into painful hips as the hips do not have enough flexion mobility for a good sitting position.
Conclusion
Hip surveillance programmes have decreased the incidence of dislocated hips in children with CP. Risk of scoliosis increases with increasing disability and age. Surgery for early onset scoliosis should be given a priority due to high risk of rapid progression. In an adolescent patient with horizontal pelvis and scoliosis, hip reconstruction before spinal fusion is acceptable if the hips are painful or without mobility to allow sitting after spine surgery and the scoliosis is moderate. In children with larger curves or with pelvic obliquity spinal fusion to level the pelvis should be addressed first. It still remains unclear if treating the hip well prevents scoliosis and vice versa.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with Ethical Standards
Funding statement
Although none of the authors has received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but will be directed solely to a research fund, foundation, educational institution, or other non-profit organization with which one or more of the authors are associated.
Ethical statement
Ethical approval: This review did not include original scientific evaluation of patient data and therefore no informed consent or ethical committee approval was requested by the institution where the writing of this review was conducted.
ICMJE Conflict of interest statement
IJH reports grants from Medtronic and from K2M via Innosurge during the conduct of the study; grants and personal fees from Medtronic, and grants and personal fees from K2M, outside the submitted work.
The other authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Dr. Paul Sponseller, Baltimore and Dr. Suken Shah, Wilmington, for valuable comments.
Author Contributions
IJH: Literature review, writing of the manuscript
EV: Literature review, critical revision of the manuscript
RMC: Literature review, critical revision of the manuscript
References
- 1.Hägglund G, Andersson S, Düppe H, et al. . Prevention of dislocation of the hip in children with cerebral palsy. The first ten years of a population-based prevention programme. J Bone Joint Surg [Br] 2005;87-B:95-101. [PubMed] [Google Scholar]
- 2.Soo B, Howard JJ, Boyd RN, et al. . Hip displacement in cerebral palsy. J Bone Joint Surg [Am] 2006;88-A:121-129. [DOI] [PubMed] [Google Scholar]
- 3.Hägglund G, Pettersson K, Czuba T, Persson-Bunke M, Rodby-Bousquet E. Incidence of scoliosis in cerebral palsy. Acta Orthop 2018;89:443-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Letts M, Shapiro L, Mulder K, Klassen O. The windblown hip syndrome in total body cerebral palsy. J Pediatr Orthop 1984;4:55-62. [DOI] [PubMed] [Google Scholar]
- 5.Senaran H, Shah SA, Glutting JJ, Dabney KW, Miller F. The associated effects of untreated unilateral hip dislocation in cerebral palsy scoliosis. J Pediatr Orthop 2006;26:769-772. [DOI] [PubMed] [Google Scholar]
- 6.Hägglund G, Alriksson-Schmidt A, Lauge-Pedersen H, et al. . Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint J 2014;96-B:1546-1552. [DOI] [PubMed] [Google Scholar]
- 7.Reimers J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 1980;184:1-100. [DOI] [PubMed] [Google Scholar]
- 8.Wynter M, Gibson N, Willoughby KL, et al. . Australian hip surveillance guidelines for children with cerebral palsy: 5-year review. Dev Med Child Neurol 2015;57:808-820. [DOI] [PubMed] [Google Scholar]
- 9.DiFazio R, Shore B, Vessey JA, Miller PE, Snyder BD. Effect of hip reconstructive surgery on health-related quality of life of non-ambulatory children with cerebral palsy. J Bone Joint Surg [Am] 2016;98:1190-1198. [DOI] [PubMed] [Google Scholar]
- 10.Viehweger E. Importance of hip problems in daily activities for cerebral palsy patients. J Child Orthop 2013;7:401-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans GA. The lower limb in cerebral palsy. Curr Orthop 1995;9:156-163. [Google Scholar]
- 12.Noonan KJ, Jones J, Pierson J, Honkamp NJ, Leverson G. Hip function in adults with severe cerebral palsy. J Bone Joint Surg [Am] 2004;86-A:2607-2613. [DOI] [PubMed] [Google Scholar]
- 13.Saito N, Ebara S, Ohotsuka K, Kumeta H, Takaoka K. Natural history of scoliosis in spastic cerebral palsy. Lancet 1998;351:1687-1692. [DOI] [PubMed] [Google Scholar]
- 14.Ágústsson A, Sveinsson Þ, Rodby-Bousquet E. The effect of asymmetrical limited hip flexion on seating posture, scoliosis and windswept hip distortion. Res Dev Disabil 2017;71:18-23. [DOI] [PubMed] [Google Scholar]
- 15.Keskinen H, Lukkarinen H, Korhonen K, et al. . The lifetime risk of pneumonia in patients with neuromuscular scoliosis at a mean age of 21 years: the role of spinal deformity surgery. J Child Orthop 2015;9:357-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rutz E, Brunner R. Management of spinal deformity in cerebral palsy: conservative treatment. J Child Orthop 2013;7:415-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Terjesen T, Lange JE, Steen H. Treatment of scoliosis with spinal bracing in quadriplegic cerebral palsy. Dev Med Child Neurol 2000;42:448-454. [DOI] [PubMed] [Google Scholar]
- 18.Sewell MD, Malagelada F, Wallace C, et al. . A preliminary study to assess whether spinal fusion for scoliosis improves carer-assessed quality of life for children with GMFCS level IV or V cerebral palsy. J Pediatr Orthop 2016;36:299-304. [DOI] [PubMed] [Google Scholar]
- 19.Miyanji F, Nasto LA, Sponseller PD, et al. . Assessing the risk-benefit ratio of scoliosis surgery in cerebral palsy: surgery is worth it. J Bone Joint Surg [Am] 2018;100:556-563. [DOI] [PubMed] [Google Scholar]
- 20.McElroy MJ, Sponseller PD, Dattilo JR, et al. . Growing rods for the treatment of scoliosis in children with cerebral palsy: a critical assessment. Spine (Phila Pa 1976) 2012;37:E1504-E1510. [DOI] [PubMed] [Google Scholar]
- 21.Yaszay B, Sponseller PD, Shah SA, et al. . Performing a definitive fusion in juvenile CP patients is a good surgical option. J Pediatr Orthop 2017;37:e488-e491. [DOI] [PubMed] [Google Scholar]
- 22.Karol LA, Johnston C, Mladenov K, et al. . Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis. J Bone Joint Surg [Am] 2008;90-A:1272-1281. [DOI] [PubMed] [Google Scholar]
- 23.Ramstad K, Jahnsen RB, Terjesen T. Severe hip displacement reduces health-related quality of life in children with cerebral palsy. Acta Orthop 2017;88:205-210. [DOI] [PMC free article] [PubMed] [Google Scholar]